Professional Documents
Culture Documents
Vaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD May 2015
Uploaded by
denekeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD May 2015
Uploaded by
denekeCopyright:
Available Formats
Vaginal Birth after Caesarean
(VBAC)
Max Brinsmead MB BS PhD
May 2015
VBAC The Controversy
Once a Caesarean always a Caesarean
Edwin Cragin 1916
In an era of classical CS
Designed to prevent unnecessary primary CS
For 60 years Trial of (lower segment) scar
was standard British practice
But repeat CS more common in the US
Controversy broke out again in 2000
And it was all about fetal risks
VBAC The Controversy
Smith et al from Cambridge UK in JAMA 2002
Reviewed 313, 238 singleton births, 37 - 43w,
cephalic presentation in the Scottish Morbidity
Register 1992 -1997 excluding congenital
malformations and found
1. Rate of perinatal death 11 times higher for VBAC
compared to elective CS
2. This is 2 times higher than for multiparas having a
vaginal birth
VBAC The Controversy
Guise et al from Portland Oregan in BMJ July 2004
Reviewed 568 publications on VBAC vs elective
CS but found only 71 had useful data
Concluded that the additional risk of perinatal
death from attempted VBAC was 1.4 per 10,000
(95 percent confidence limits 0 - 9.8)
In only 5% of uterine ruptures did the baby die
This means that one has to perform 7142 elective
CS to prevent one baby death
This presentation will:
Examine the advantages and disadvantages
of VBAC
Evaluate the risks to mother & baby
Provide an evidence base for the safe
practice of VBAC...
Patient selection
Preparation of patients
Guidelines for intrapartum care
Advantages of VBAC
Greater maternal satisfaction
But its not all about me
Quicker recovery
But not always
Cheaper
But not much cheaper than elective CS and can
be much more costly
Less RDS for babies
But greater risk of death & disability
Less maternal morbidity and mortality
But these are rare with elective CS
Advantages of VBAC - 2
More vaginal births in the future
But whats the point if theres only to be two
kids!
Less maternal depression
But there is no evidence that this is so
Breast feeding more likely to succeed
Occurs in the delivery room
Easier for mothers without wound pain
Avoids risks unique to CS
But these are rare
Advantages of Elective CS
Certainty of timing
Thats the modern way!
Certainty of outcome
If I have a 30 50% chance of CS just do one!
Emergency CS more dangerous
Its Pain-free
More or less guaranteed!
Often preferred by fathers & obstetricians
Thats a male thing
Advantages of Elective CS
Protects the pelvic floor
Controversial because
Some risk arises from the pregnancy itself
And CS may not be protective
Safer for babies
But the absolute risk of VBAC is small
Avoids the risk of scar rupture
But there is much uncertainty about the
frequency of this
and the maternal and fetal risks
VBAC Risk to the Fetus
The rate of perinatal death is 11 x higher than
for elective CS
BUT
This risk is equivalent to that of being a fetus
to a Primigravida
The absolute risk is only 4.5 per 10,000 births
Confidence limits are wide
In the 2002 UK publication all emergency CS
were classified as attempted VBAC
Maternal Risk from VBAC
Meta analysis of risk of death
2.8 per 10,000 with trial of scar
2.4 per 10,000 for elective CS
No maternal death ever attributed to scar rupture
Scar rupture
Much confusion in the literature over the definition
Rate of asymptomatic scar rupture the same whether
VBAC or elect CS
Overall rate approx. 0.5% or 1:200
Was 0.35% in the largest combined contemporary study
Hysterectomy
Additional risk from trial of scar is 3.4 per 10,000
Requires 2941 elective CS to prevent one hysterectomy
Patient selection for VBAC
Type of previous CS
"10% " risk of rupture from classical and T incisions
Myomectomy and Hysterotomy
Indication for Previous CS
But 50-75% of patients can VBAC after previous CS for
CPD!
Previous obstetric history
VBAC success >90% if there has been prior vaginal birth
Dilatation at the time of previous CS
Gestation at previous CS was there a lower segment?
Number of previous CS
Increasing risk with increasing number
Patient selection for VBAC -2
Time since previous CS
Risk of scar rupture is 2 3x greater if <18m
Maternal weight
Miserable rates of VBAC for women >135 Kg
Lower uterine segment thickness
No uterine ruptures if >4.5 mm
Maternal Age
Clear evidence for declining uterine performance with age
at first labour
Family history of labour performance
A field ripe for study
Patient selection for VBAC - 3
Size of the mother and baby
But we are very bad at estimating this
Other pregnancy problems
Should be assessed according to obstetric principles
Engagement and cervical ripening
Best assessed at the onset of labour
Labour performance
Thats why its called trial of scar
Dilatation and descent
Progress rather than arbitrary time limits
Psychological Factors
The patients willingness and drive
The support provided
More than one previous CS?
Tahseen & Griffith BJOG Jan 2010 in a
systematic analysis of available data and
meta analysis concluded:
1.
2.
3.
4.
Overall success 71.1%
Risk of scar rupture 1.36% (this is 3x greater than
for one CS)
Perinatal risk is 0.09% (this is 3x greater than for
one CS)
The overall maternal morbidity was the same as
that for elective CS
Hysterectomy, transfusion, febrile morbidity etc
More than two previous CS?
Cahill et al BJOG 2010 in a retrospective
cohort study 89 women with >2 previous
CS concluded:
1.
2.
3.
Overall success 79.8%
No cases of uterine rupture
The overall maternal morbidity was the same as
that for elective CS
Hysterectomy, transfusion, febrile morbidity etc
Lower segment thickness and risk of scar rupture
Rozenberg et al Lancet 1996 studied 642 women with
ultrasound , measured the thinnest point of the lower
segment against a filled bladder, then attempted VBAC:
>4.5 mm - no ruptures or dehiscence (278)
3.6 - 4.5 mm 2% rate of scar rupture (177)
2.6 - 3.5 mm 10% rate of scar rupture (136)
<2.6 mm
16% rate of scar rupture (51)
Can be technically difficult particularly in obese woman
Vaginal and 3-dimensional measures promising
VBAC for the Obese?
Carrel et al (Am J OG in 2003) studied 70 women >200 lb,
70 who were 200-300 lb and 69 >300 lb
81.8% success for those <200 lb
57.1% success for those 200-300 lb
13.3% success for those >300 lb
Infection rate was:
5.7% group 1
11.4% group 2
39%
group 3
(Very similar results published in 2001)
VBAC for Older Women?
Byfield et al Am J OG in 2004 studied 659 women <30 years
age, 721 who were 30-35 years age and 370 >35 years age
72% success for those <30
71% success for those 30-35
65% success for those >35
Scar rupture rate was:
2.0% group 1
1.1% group 2
1.4% group 3
Pregnancy Interval and Risk of Scar Rupture
Byfield et al Am J OG in 2002 studied 1527 women who
attempted VBAC at <12 to >36 months after previous CS:
4.8% ruptured for those <12m
2.7% ruptured for those 13-24m
0.9% ruptured for those 25-36m
0.9% ruptured for those >36m
Pregnancy Interval and Risk of Scar Rupture
Bujold & Gauthier Obstet Gynec in 2010 studied 1768
women who attempted VBAC after one previous CS:
4.8% ruptured for those <18m
1.9% ruptured for those 18-24m
1.3% ruptured for those >24m
Also noted 7-fold increased rate of rupture
when the previous CS was a single layer
closure
Single vs Double-layer closure at prior CS
Blumenfeld et al BJOG in 2010 studied 127 women
undergoing primary CS.
At subsequent CS those who had a single
layer closure had a 7-fold increased risk of
bladder adhesions (RR=6.96, CI 1.72
28.1)
Regardless of any other variation in surgical
technique
Induction of Labour for VBAC?
Ravasia et al Am JOG 2000 studied 2119 women attempting
VBAC between 1992 and 1998 of whom 27% had an
induction of labour
Spontaneous labour
Induced labour
Cx ripening c PGs
Cx ripening c Foley
IOL not using PGs
0.45% scar rupture rate
1.4%
2.9%
0.7%
0.7%
Induction of Labour for VBAC -2?
Lyndan-Rochelle et al NEJM 2001 studied all women
attempting VBAC between 1987 and 1996 in Washington
state
Rate of Scar Rupture
No labour
1.6 per 1000
Spontaneous labour
5.2 "
"
Induced labour (not PGs) 7.7 "
"
Induced with PGs
24.5 " "
However this study used ICD9 codes for identifying scar
rupture and these are only 40% accurate
Induction of Labour for VBAC -3?
Lin & Rayner Am JOG 2004 studied 3533 women attempting
VBAC after one or more CS, 2523 in spontaneous labour,
438 by elective CS, 430 induced with oxytocin and 142
induced with Misoprostol
Rate of scar rupture was significantly higher
when labour was induced.
No significant difference between oxytocin
(0.8%) and Misoprostol (1.1%)
Induction of Labour for VBAC -4?
Dekkar et al studied 29,008 women attempting VBAC in
Australia 1998 2000 BJOG 117:1358 2010
Rate of scar rupture (complete & partial ) was:
No labour
Spontaneous labour with no augmentation
Labour augmented with oxytocin
Induced using oxytocin
Induced using prostaglandins (PGs)
Induced with PGs and oxytocin
Overall rate of successful VBAC
0.01%
0.15%
1.91%
0.54%
0.68%
0.88%
54.3%
Canadian College Surgeons & Physicians Guidelines 1993 - 1
Trial of labour should be recommended to
all women who have had only one previous
CS. Except for:
Previous classical, T or unknown uterine incision
Previous hysterotomy or full thickness myomectomy
Previous uterine rupture
Any contraindication to labour in this pregnancy eg
placenta previa, transverse lie etc.
The wish of the patient is paramount
(and the partner should ideally also be involved)
Canadian College Surgeons & Physicians Guidelines 1993 - 2
The patient should be made aware of the
hospitals resources and any limitations
The previous obstetric record should be
consulted
Consultation with a specialist obstetrician is
not mandatory
Induction of labour with oxytocin or Foley
catheter is acceptable
Augmentation with oxytocin is acceptable but
caution required if arrest has occurred in the
active phase of labour
Canadian College Surgeons & Physicians Guidelines 1993 - 3
Continuous EFM required only when when
induction or augmentation of labour is used
The problem of false positives
No evidence that it is a specific indicator of scar
rupture
Epidural anaesthesia not contraindicated
Twins not contraindicated
Suspected fetal macrosomia & diabetes not
contraindicated
My guidelines for VBAC - 1
Patients are counselled that VBAC is not
appropriate if:
There is a classical, T-shaped or unknown
uterine incision
More than one CS has been performed
The previous CS was performed for failure to
progress in the active phase of labour i.e. >4 cm
dilated
Their BMI is >35
Patients accepted outside of these guidelines on a case- bycase basis.
My guidelines for VBAC - 2
Patients who are suitable for a trial of scar
should be told by their primary carer that
elective CS and VBAC have risks and
benefits.
They should:
Read on the subject RCOG 2008
Discuss it with an obstetrician
Their decision will be respected
Patients planning VBAC require one to one
preparation
My guidelines for VBAC - 3
Any available record about the previous CS
is scrutinized
The patient is provided with individualised
chance of success with VBAC & maternal
and fetal risks
Delivery in a place capable of emergency
laparotomy is recommended
Any limitation in the patients chosen place
of birth is discussed
The discussion is documented
My guidelines for VBAC - 4
Offer IOL by sweep membranes, ARM and
oxytocin in safe working hours at 39 41w
Cervical ripening with Foley but not PGs
If admitted in spontaneous labour then
review by obstetrician within 2 hrs is
desirable
IV line, group and save
Epidural if required.
Monitor by continuous CTG only if
oxytocin or epidural is in use
My guidelines for VBAC - 5
CS is recommended if there is failure to
progress i.e.
<1 cm per hour dilatation over >4 hrs and >3 cm and
good uterine activity
No head descent with >60 minutes active pushing in
the 2nd stage
Assisted delivery may be attempted according to
usual obstetric dictates
OR Fetal Distress i.e.
Scalp lactate >4.8 or CTG so abnormal as to warrant
scalp sampling by RCOG guidelines
My experience with VBAC - 1
330 private multigravid patients 2001 04
65 had undergone previous CS (20%)
32 attempted VBAC (50%)
21were successful (66%)
12 by SVD and 9 assisted
My experience with VBAC - 2
Among the 32 VBACs there were:
2 patients who had 2 previous CS (one with a thin lower
segment)
5 patients whose previous CS was for failure to progress
and 2 of these had a bigger baby during VBAC
1 patient who had a third degree tear in her first SVD,
elective CS for the second and SVD with an intact
perineum during VBAC
Any Questions or Comments?
Please leave a note on the Welcome
Page to this website
You might also like
- Human Sexuality in A Changing World 10th Edition.c2Document625 pagesHuman Sexuality in A Changing World 10th Edition.c2jakeNo ratings yet
- Vaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD December 2015Document36 pagesVaginal Birth After Caesarean (Vbac) : Max Brinsmead MB Bs PHD December 2015kikyNo ratings yet
- Vbac FinDocument15 pagesVbac FinCindy AgustinNo ratings yet
- LaparotomyDocument36 pagesLaparotomydenekeNo ratings yet
- General AnesthesiaDocument27 pagesGeneral AnesthesiadenekeNo ratings yet
- 13complications of 3rd Stage of Labour MCQDocument10 pages13complications of 3rd Stage of Labour MCQKamal El-Ghorory75% (4)
- Living with Metastatic Breast Cancer: Stories of Faith and HopeFrom EverandLiving with Metastatic Breast Cancer: Stories of Faith and HopeNo ratings yet
- PQCNC OBH Kickoff CMOP Learning Session - Maternal Mortality Closing The Gap 2017Document58 pagesPQCNC OBH Kickoff CMOP Learning Session - Maternal Mortality Closing The Gap 2017kcochran100% (1)
- Lameshow Statistik PDFDocument247 pagesLameshow Statistik PDFqel_harizah100% (1)
- Postterm PregnancyDocument16 pagesPostterm PregnancyrranindyaprabasaryNo ratings yet
- 2AN Group 3 Script/Flow For RLE CHN Duty RotationDocument8 pages2AN Group 3 Script/Flow For RLE CHN Duty RotationLouwella RamosNo ratings yet
- Vbac Acog 2010Document27 pagesVbac Acog 2010ariniNo ratings yet
- Predicting Cesarean Section AnDocument5 pagesPredicting Cesarean Section AnKEANNA ZURRIAGANo ratings yet
- Managing Women With Previous CS2Document27 pagesManaging Women With Previous CS2zynal20038222No ratings yet
- IOSRPHRDocument3 pagesIOSRPHRIOSR Journal of PharmacyNo ratings yet
- Bahan Utk VCDocument58 pagesBahan Utk VCTias DiahNo ratings yet
- Vaginal Delivery of TwinsDocument63 pagesVaginal Delivery of Twinsrake sardevaNo ratings yet
- Cervical Conization and The Risk of Preterm DeliveryDocument11 pagesCervical Conization and The Risk of Preterm DeliveryGelo ConcepcionNo ratings yet
- Bang UcupDocument34 pagesBang Ucupvannyanoy100% (1)
- My Pap Smear Is Abnormal !Document70 pagesMy Pap Smear Is Abnormal !Alena JosephNo ratings yet
- Caesarean SectionDocument29 pagesCaesarean SectionMuriel CardosoNo ratings yet
- Childbirth and The Female Pelvic Floor: Christopher Maher Wesley UrogynaecologyDocument54 pagesChildbirth and The Female Pelvic Floor: Christopher Maher Wesley UrogynaecologyVeronica MendozaNo ratings yet
- Statistics BusysprDocument25 pagesStatistics BusysprKeeranmayeeishraNo ratings yet
- Vaginal Birth After Cesarean, JurnalDocument19 pagesVaginal Birth After Cesarean, Jurnaldewi trisnaNo ratings yet
- C-Obs 38 Planned Vaginal Birth After C-Section New Jul 10Document7 pagesC-Obs 38 Planned Vaginal Birth After C-Section New Jul 10Aris SugiatnoNo ratings yet
- 12 .Tyraskis2017Document31 pages12 .Tyraskis2017dw21541No ratings yet
- Mid-Trimester Amniocentesis Fetal Loss Rate: Committee OpinionDocument5 pagesMid-Trimester Amniocentesis Fetal Loss Rate: Committee OpinionDivine Grace ValenzuelaNo ratings yet
- Placenta PreviaDocument5 pagesPlacenta PreviaYolanda Angulo BazánNo ratings yet
- Induction of Labour Versus Expectant Management For Nulliparous Women Over 35 Years of Age: A Multi-Centre Prospective, Randomised Controlled TrialDocument8 pagesInduction of Labour Versus Expectant Management For Nulliparous Women Over 35 Years of Age: A Multi-Centre Prospective, Randomised Controlled TrialAndinNo ratings yet
- 18B# Vaginal Birth After Cesarean Section PONEK 2020Document22 pages18B# Vaginal Birth After Cesarean Section PONEK 2020ruang obstetriNo ratings yet
- In Vitro Fertilization For M6 Students: YL TsaiDocument49 pagesIn Vitro Fertilization For M6 Students: YL TsaiLee BoborasNo ratings yet
- Cesarean VsDocument8 pagesCesarean Vsapi-427591170No ratings yet
- Vbac - YurDocument20 pagesVbac - YurkikiNo ratings yet
- Vaginal Birth After Cesarean Delivery (VBAC) Definition/AbbreviationDocument3 pagesVaginal Birth After Cesarean Delivery (VBAC) Definition/AbbreviationCalvin TranNo ratings yet
- Uteri Ne Rupture Duri NG Labor Among Women With P R Ior Cesar Ean Deliver YDocument22 pagesUteri Ne Rupture Duri NG Labor Among Women With P R Ior Cesar Ean Deliver Yzero thirteen eighty oneNo ratings yet
- Prior Cesarean Delivery: 100 Years of ControversyDocument17 pagesPrior Cesarean Delivery: 100 Years of ControversyNoahYudhaNo ratings yet
- Cervical Stitch Give Birth Kelompok 2Document78 pagesCervical Stitch Give Birth Kelompok 2Larose Rossyta SariNo ratings yet
- Caesarean Birth and Risk of Subsequent Preterm Birth: A Retrospective Cohort StudyDocument9 pagesCaesarean Birth and Risk of Subsequent Preterm Birth: A Retrospective Cohort Studyluis albenis mendoza guerraNo ratings yet
- Cesarean DeliveryDocument13 pagesCesarean DeliveryCindy LidiaNo ratings yet
- Maternal Morbidity Associated With Multiple Repeat Cesarean DeliveriesDocument7 pagesMaternal Morbidity Associated With Multiple Repeat Cesarean Deliveriesdewi wahyuniNo ratings yet
- Critical Appraisal Ayu RonoDocument41 pagesCritical Appraisal Ayu Ronoamarendra WardhanaNo ratings yet
- Identifying Risk Factors For Uterine RuptureDocument15 pagesIdentifying Risk Factors For Uterine RuptureSakena NurzaNo ratings yet
- Knight Et Al-2014-BJOG An International Journal of Obstetrics & GynaecologyDocument10 pagesKnight Et Al-2014-BJOG An International Journal of Obstetrics & GynaecologyAndrian drsNo ratings yet
- 06 SC AlarmDocument34 pages06 SC AlarmYosie Yulanda PutraNo ratings yet
- 730 2113 1 PBDocument7 pages730 2113 1 PBFitrahMyatunNo ratings yet
- Vaginal BirthDocument7 pagesVaginal BirthMentari Cipta SeptikaNo ratings yet
- Uterine Rupture After Previous Caesarean Section: EpidemiologyDocument12 pagesUterine Rupture After Previous Caesarean Section: EpidemiologymacNo ratings yet
- Jurnal SCDocument3 pagesJurnal SCmorningNo ratings yet
- To Vbac or Not To Vbac: PerspectiveDocument3 pagesTo Vbac or Not To Vbac: Perspectiveharani roimaNo ratings yet
- Evidence Based: Vaginal Birth After Cesarean: First ResearchDocument2 pagesEvidence Based: Vaginal Birth After Cesarean: First ResearchGodfrey AntolinNo ratings yet
- Cervical Cancer Screening Recommendations, 2012: The American Society For Colposcopy and Cervical PathologyDocument55 pagesCervical Cancer Screening Recommendations, 2012: The American Society For Colposcopy and Cervical PathologyKharisma AlifahNo ratings yet
- Vbac Success 2013Document6 pagesVbac Success 2013040193izmNo ratings yet
- Pregnancy Outcome of Single Previous Cesarean SectionDocument4 pagesPregnancy Outcome of Single Previous Cesarean SectionDhesy WildayaniNo ratings yet
- Practice Bulletin: Vaginal Birth After Previous Cesarean DeliveryDocument14 pagesPractice Bulletin: Vaginal Birth After Previous Cesarean DeliveryFernando González PeruggiNo ratings yet
- 2.april 2020 Estimation of Risk Factors For MultiparousDocument4 pages2.april 2020 Estimation of Risk Factors For MultiparousTushar BahetiNo ratings yet
- Factors Associated With Successful Vaginal Birth After Cesarean Section and Outcomes in Rural Area of AnatoliaDocument8 pagesFactors Associated With Successful Vaginal Birth After Cesarean Section and Outcomes in Rural Area of AnatoliaIllona SaharaNo ratings yet
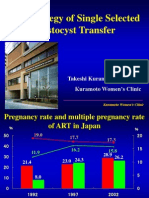
- The Strategy of Single Selected Blastocyst Transfer: Takeshi Kuramoto MD, PHD Kuramoto Women'S ClinicDocument43 pagesThe Strategy of Single Selected Blastocyst Transfer: Takeshi Kuramoto MD, PHD Kuramoto Women'S ClinicDian Isti AngrainiNo ratings yet
- Acta Obstet Gynecol Scand 2018 Lindblad Wollmann Risk of Repeat Cesarean Delivery in Women Undergoing Trial of LaborDocument6 pagesActa Obstet Gynecol Scand 2018 Lindblad Wollmann Risk of Repeat Cesarean Delivery in Women Undergoing Trial of LaborMillennials ShopifyNo ratings yet
- Simcox 2009Document6 pagesSimcox 2009Aulya ArchuletaNo ratings yet
- BMC Pregnancy and Childbirth: Jodie M Dodd, Caroline A Crowther, Janet E Hiller, Ross R Haslam and Jeffrey S RobinsonDocument9 pagesBMC Pregnancy and Childbirth: Jodie M Dodd, Caroline A Crowther, Janet E Hiller, Ross R Haslam and Jeffrey S RobinsonSyahrullah Ramadhan UllaNo ratings yet
- Cesarean Birth Mothering PonteDocument16 pagesCesarean Birth Mothering PonteL. BarriolaNo ratings yet
- Previous Preterm Cesarean Delivery and Risk of Uterine Rupturein Subsequent Trial of LaborDocument28 pagesPrevious Preterm Cesarean Delivery and Risk of Uterine Rupturein Subsequent Trial of LaborDjlatino LatinoNo ratings yet
- Labour Admission Test: International Journal of Infertility and Fetal Medicine December 2011Document8 pagesLabour Admission Test: International Journal of Infertility and Fetal Medicine December 2011IndhumathiNo ratings yet
- Low Primary Cesarean Rate and High VBAC Rate With Good Outcomes in An Amish Birthing CenterDocument8 pagesLow Primary Cesarean Rate and High VBAC Rate With Good Outcomes in An Amish Birthing CenterStefanichalisnia 96No ratings yet
- Twins PecepDocument8 pagesTwins Pecepjj_cani91No ratings yet
- Meaza Respiratory FinalDocument85 pagesMeaza Respiratory FinaldenekeNo ratings yet
- BurnDocument30 pagesBurndenekeNo ratings yet
- EngDocument65 pagesEngWhinet Jojo TerunaNo ratings yet
- Chest TubeDocument22 pagesChest TubedenekeNo ratings yet
- FB and CellulitisDocument42 pagesFB and CellulitisdenekeNo ratings yet
- Surgicla TechniqueDocument47 pagesSurgicla TechniquedenekeNo ratings yet
- CHAPTER 1-Intro Duction of AnesthesiaDocument28 pagesCHAPTER 1-Intro Duction of AnesthesiadenekeNo ratings yet
- Wound HealingDocument47 pagesWound HealingdenekeNo ratings yet
- Spinal AnesthesiaDocument29 pagesSpinal AnesthesiadenekeNo ratings yet
- Neonatal Resusitation NIME 2009Document55 pagesNeonatal Resusitation NIME 2009denekeNo ratings yet
- Approach To Surgical PTDocument31 pagesApproach To Surgical PTdenekeNo ratings yet
- 21.diabetes Mellitus in PregnancyDocument47 pages21.diabetes Mellitus in Pregnancydeneke100% (1)
- Preterm Labor and DeliveryDocument21 pagesPreterm Labor and DeliverydenekeNo ratings yet
- Spinal AnesthesiaDocument29 pagesSpinal AnesthesiadenekeNo ratings yet
- HypertDocument2 pagesHypertdenekeNo ratings yet
- Motor LesionsDocument30 pagesMotor Lesionsdeneke0% (1)
- 10.multiple GestationDocument49 pages10.multiple GestationdenekeNo ratings yet
- Infective Endo.Document8 pagesInfective Endo.denekeNo ratings yet
- Pyramidal TractDocument48 pagesPyramidal TractdenekeNo ratings yet
- 17 IugrDocument48 pages17 IugrdenekeNo ratings yet
- CPRDocument52 pagesCPRdenekeNo ratings yet
- 3.Dxs of PregnancyDocument24 pages3.Dxs of PregnancydenekeNo ratings yet
- 26 PcosDocument66 pages26 PcosdenekeNo ratings yet
- 5 AncDocument40 pages5 AncdenekeNo ratings yet
- 16 PromDocument18 pages16 PromdenekeNo ratings yet
- 16 PromDocument18 pages16 PromdenekeNo ratings yet
- 8.perinatal DXDocument35 pages8.perinatal DXdenekeNo ratings yet
- Guide To SexDocument16 pagesGuide To SexNiţu MarianNo ratings yet
- Essay On EmONC On Reducing Maternal MortalityDocument3 pagesEssay On EmONC On Reducing Maternal MortalityBenjaminNo ratings yet
- UNIT 5 LAB Technological Timeline Mariam SalhienDocument5 pagesUNIT 5 LAB Technological Timeline Mariam SalhienMariam SalhienNo ratings yet
- Case Scenario IDocument2 pagesCase Scenario IGynesis Lim RoqueroNo ratings yet
- Activity Sheets in Science 5 Quarter 2, Week 1: Parts of The Reproductive System and Their FunctionsDocument6 pagesActivity Sheets in Science 5 Quarter 2, Week 1: Parts of The Reproductive System and Their Functionsricardo salayonNo ratings yet
- Ectopic PregnancyDocument38 pagesEctopic PregnancyLovelyjade ReyesNo ratings yet
- The Perception of Pregnant Women Towards Antenatal Care at Madina Polyclinic-Ghana: A Descriptive Exploratory StudyDocument13 pagesThe Perception of Pregnant Women Towards Antenatal Care at Madina Polyclinic-Ghana: A Descriptive Exploratory StudyP'Babe Cece AdumoahNo ratings yet
- Save The GirlDocument11 pagesSave The GirlMeenakshi HandaNo ratings yet
- Preterm Prelabor Rupture of Membranes - Management and Outcome - UpToDateDocument35 pagesPreterm Prelabor Rupture of Membranes - Management and Outcome - UpToDatemaminyaarNo ratings yet
- Elden Ring (Video Game) - Works Archive of Our OwnDocument1 pageElden Ring (Video Game) - Works Archive of Our OwnAndrew ABell0% (1)
- PLGF Pelican Study Key PointsDocument3 pagesPLGF Pelican Study Key PointsGabriel Cadavid GilNo ratings yet
- Fetal Death in Utero Radiology Reference Article PDFDocument1 pageFetal Death in Utero Radiology Reference Article PDFMoe Wai MyintNo ratings yet
- BrochureDocument20 pagesBrochureAnjali MohanNo ratings yet
- Mechanisms of Action and Effectiveness of Contraception MethodsDocument2 pagesMechanisms of Action and Effectiveness of Contraception Methodsjaimedelafuente22No ratings yet
- Microgest InsertDocument1 pageMicrogest InsertChodhur BhodhurNo ratings yet
- Hubungan Karakteristik Ibu Inpartu Terhadap Kejadian Perdarahan Postpartum Di Rsu Budi Kemuliaan Periode Tahun 2019Document10 pagesHubungan Karakteristik Ibu Inpartu Terhadap Kejadian Perdarahan Postpartum Di Rsu Budi Kemuliaan Periode Tahun 2019MiMa Muach LadyzNo ratings yet
- High-Risk Pregnancy Premature Rupture of Membranes (PROM)Document3 pagesHigh-Risk Pregnancy Premature Rupture of Membranes (PROM)elimcangcoNo ratings yet
- CHN and OBDocument91 pagesCHN and OBJoshua Christian GanNo ratings yet
- Menstrual Cycle and Ovulation Period PDFDocument3 pagesMenstrual Cycle and Ovulation Period PDFSalman AmirNo ratings yet
- Ucsp Kinship and FamilyDocument9 pagesUcsp Kinship and FamilycdcheijdnekjdNo ratings yet
- Multiple PregnancyDocument28 pagesMultiple PregnancyFarxan Da Napolian BwoyNo ratings yet
- Obg Icd-10 Pregnancy, Childbirth, PuerperiumDocument11 pagesObg Icd-10 Pregnancy, Childbirth, PuerperiumarifianjuariNo ratings yet
- Oligohydramnios - Etiology, Diagnosis, and Management - UpToDateDocument23 pagesOligohydramnios - Etiology, Diagnosis, and Management - UpToDateJUAN FRANCISCO OSORIO PENALOZANo ratings yet
- Childhood Sexual Abuse, Relationship Satisfaction, and Sexual Risk Taking in A Community Sample of WomenDocument9 pagesChildhood Sexual Abuse, Relationship Satisfaction, and Sexual Risk Taking in A Community Sample of WomenScott PymNo ratings yet
- 1151 3608 1 PBDocument7 pages1151 3608 1 PBNilam SariNo ratings yet
- Nhs Forth Valley: Management of Acute Inversion of UterusDocument5 pagesNhs Forth Valley: Management of Acute Inversion of UterusMelissa Aina Mohd YusofNo ratings yet
- Dip Obst (SA) Past Papers - 2020 1st Semester 1-6-2023Document1 pageDip Obst (SA) Past Papers - 2020 1st Semester 1-6-2023Neo Latoya MadunaNo ratings yet