Professional Documents
Culture Documents
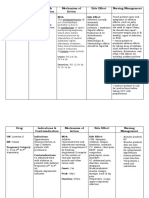
Phenytoin Dosage, Side Effects and Nursing Considerations
Uploaded by
Rhawnie B. GibbsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Phenytoin Dosage, Side Effects and Nursing Considerations
Uploaded by
Rhawnie B. GibbsCopyright:
Available Formats
Name /bks_53161_deglins_md_disk/phenytoin
02/17/2014 09:10AM
Plate # 0-Composite
pg 1 # 1
TIME/ACTION PROFILE (anticonvulsant effect)
phenytoin (fen-i-toyn)
Dilantin, Phenytek, Tremytoine
Classification
Therapeutic: antiarrhythmics (group IB), anticonvulsants
Pharmacologic: hydantoins
Pregnancy Category D
PEAK
DURATION
224 hr (1 wk)*
224 hr (1 wk)
0.51 hr (1 wk)
1.53 hr
412 hr
rapid
612 hr
1236 hr
1224 hr
Contraindications/Precautions
Contraindicated in: Hypersensitivity; Hypersensitivity to propylene glycol (phe-
Treatment/prevention of tonic-clonic (grand mal) seizures and complex partial seizures. Unlabeled Use: As an antiarrhythmic, particularly for ventricular arrhythmias associated with digoxin toxicity, prolonged QT interval, and surgical repair of
congenital heart diseases in children. Management of neuropathic pain, including
trigeminal neuralgia.
Action
Limits seizure propagation by altering ion transport. May also decrease synaptic
transmission. Antiarrhythmic properties as a result of shortening the action potential
and decreasing automaticity. Therapeutic Effects: Diminished seizure activity.
Termination of ventricular arrhythmias.
Pharmacokinetics
Absorption: Absorbed slowly from the GI tract. Bioavailability differs among products; the Dilantin and Phenytek preparations are considered to be extended products. Other products are considered to be prompt release.
Distribution: Distributes into CSF and other body tissues and fluids. Enters breast
milk; crosses the placenta, achieving similar maternal/fetal levels. Preferentially distributes into fatty tissue.
Protein Binding: Adults 90 95%;pprotein binding in neonates (up to 20% free
fraction available), infants (up to 15% free), and patients with hyperbilirubinemia,
hypoalbuminemia, severe renal dysfunction or uremia.
Metabolism and Excretion: Mostly metabolized by the liver; minimal amounts
excreted in the urine.
Half-life: 22 hr (range 7 42 hr).
Genetic Implication.
ONSET
PO
PO-ER
IV
*() time required for onset of action without a loading dose
Indications
Canadian drug name.
ROUTE
nytoin injection only); Alcohol intolerance (phenytoin injection and liquid only); Sinus bradycardia, sinoatrial block, 2nd- or 3rd-degree heart block, or Stokes-Adams
syndrome (phenytoin injection only); Concurrent use of delavirdine.
Use Cautiously in: All patients (mayqrisk of suicidal thoughts/behaviors); Hepatic or renal disease (qrisk of adverse reactions; dose reduction recommended for
hepatic impairment); Patients with severe cardiac or respiratory disease (use of IV
phenytoin may result in anqrisk of serious adverse reactions); OB: Safety not established; may result in fetal hydantoin syndrome if used chronically or hemorrhage in
the newborn if used at term; use with extreme caution; Lactation: Safety not established; Pedi: Suspension contains sodium benzoate, a metabolite of benzyl alcohol
that can cause potentially fatal gasping syndrome in neonates; Geri: Use of IV phenytoin may result in anqrisk of serious adverse reactions.
Exercise Extreme Caution in: Patients positive for HLA-B*1502 allele (unless exceptional circumstances exist where benefits clearly outweigh the risks).
Adverse Reactions/Side Effects
Most listed are for chronic use of phenytoin CNS: SUICIDAL THOUGHTS, ataxia, agitation, confusion, dizziness, drowsiness, dysarthria, dyskinesia, extrapyramidal syndrome, headache, insomnia, weakness. EENT: diplopia, nystagmus. CV: hypotension (q with IV phenytoin), tachycardia. GI: gingival hyperplasia, nausea,
constipation, drug-induced hepatitis, vomiting. Derm: STEVENS-JOHNSON SYNDROME,
TOXIC EPIDERMAL NECROLYSIS, hypertrichosis, rash, exfoliative dermatitis, pruritus,
purple glove syndrome. Hemat: AGRANULOCYTOSIS, APLASTIC ANEMIA, leukopenia,
megaloblastic anemia, thrombocytopenia. MS: osteomalacia, osteoporosis. Misc:
fever, lymphadenopathy.
Interactions
Drug-Drug: Maypthe effects of delavirdine, resulting in loss of virologic response and potential resistant (concurrent use contraindicated). Acute ingestion of
CAPITALS indicate life-threatening, underlines indicate most frequent.
Strikethrough Discontinued.
PDF Page #1
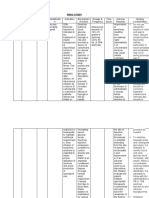
Name /bks_53161_deglins_md_disk/phenytoin
02/17/2014 09:10AM
2
alcohol, amiodarone, benzodiazepines, capecitabine, chloramphenicol, cimetidine, disulfiram estrogens, ethosuximide, felbamate, fluconazole, fluorouracil, fluoxetine, fluvastatin, fluvoxamine, gabapentin, halothane, isoniazid, itraconazole, ketoconazole, methylphenidate, oxcarbazepine,
omeprazole, phenothiazines, salicylates, sertraline, succinamides, sulfonamides, ticlopidine, tolbutamide, topiramate, trazodone, voriconazole and
warfarin mayqlevels. Chronic ingestion of alcohol, barbiturates, carbamazepine, fosamprenavir, nelfinavir, reserpine, ritonavir, and vigabatrin mayp
levels. Maypthe effects of amiodarone, atorvastatin, benzodiazepines, carbamazepine, corticosteroids, cyclosporine, digoxin, doxycycline, efavirenz,
estrogens, fluvastatin, indinavir, lopinavir/ritonavir, methadone, mexiletine, nelfinavir, nisoldipine, oral contraceptives, paroxetine, quinidine, rifampin, ritonavir, saquinavir, simvastatin, tacrolimus, theophylline, topiramate, and warfarin. IV phenytoin and dopamine may cause additive hypotension.
Additive CNS depression with other CNS depressants, including alcohol, antihistamines, antidepressants, opioids, and sedative/hypnotics. Antacids mayp
absorption of orally administered phenytoin.qsystemic clearance of antileukemic
drugs teniposide and methotrexate which has been associated with a worse event
free survival, phenytoin use is not recommended in children undergoing chemotherapy for acute lymphocytic leukemia. Calcium and sucralfatepphenytoin absorption.
Drug-Natural Products: St. Johns Wort mayplevels.
Drug-Food: Phenytoin maypabsorption of folic acid. Concurrent administration
of enteral tube feedings maypphenytoin absorption. Folic acid mayplevels.
Route/Dosage
IM administration is not recommended due to erratic absorption and pain on injection. Oral route should be used whenever possible.
Anticonvulsant
PO (Adults): Loading dose of 15 20 mg/kg as extended capsules in 3 divided doses
given every 2 4 hr; maintenance dose 5 6 mg/kg/day given in 1 3 divided doses;
usual dosing range 200 1200 mg/day.
PO (Children 10 16 yr): 6 7 mg/kg/day in 2 3 divided doses.
PO (Children 7 9 yr): 7 8 mg/kg/day in 2 3 divided doses.
Plate # 0-Composite
pg 2 # 2
PO (Children 4 6 yr): 7.5 9 mg/kg/day in 2 3 divided doses.
PO (Children 0.5 3 yr): 8 10 mg/kg/day in 2 3 divided doses.
PO (Neonates up to 6 mo): 5 8 mg/kg/day in 2 divided doses, may require q 8 hr
dosing.
IV (Adults): Status epilepticus loading dose 15 20 mg/kg. Rate not to exceed
25 50 mg/min. Maintenance dose same as PO dosing above.
IV (Children): Status epilepticus loading dose 15 20 mg/kg at 1 3 mg/kg/
min. Maintenance dose same as PO dosing above.
Antiarrhythmic
IV (Adults): 50 100 mg q 10 15 min until arrhythmia is abolished, or a total of 15
mg/kg has been given, or toxicity occurs.
PO (Adults): Loading dose: 250 mg 4 times daily for 1 day, then 250 mg twice daily
for 2 days, then maintenance at 300 400 mg/day in divided doses 1 4 times/day.
IV (Children): 1.25 mg/kg q 5 min, may repeat up to total loading dose of 15 mg/kg.
Maintenance dose 5 10 mg/kg/day in 2 3 divided doses IV or PO.
NURSING IMPLICATIONS
Assessment
Monitor closely for notable changes in behavior that could indicate the
emergence or worsening of suicidal thoughts or behavior or depression.
Assess oral hygiene. Vigorous cleaning beginning within 10 days of initiation of
phenytoin therapy may help control gingival hyperplasia.
Assess patient for phenytoin hypersensitivity syndrome (fever, skin
rash, lymphadenopathy). Rash usually occurs within the first 2 wk of
therapy. Hypersensitivity syndrome usually occurs at 3 8 wk but may
occur up to 12 wk after initiation of therapy. May lead to renal failure,
rhabdomyolysis, or hepatic necrosis; may be fatal.
Observe patient for development of rash. Discontinue phenytoin at the
first sign of skin reactions. Serious adverse reactions such as exfoliative,
purpuric, or bullous rashes or the development of lupus erythematosus,
Stevens-Johnson syndrome, or toxic epidermal necrolysis preclude further use of phenytoin or fosphenytoin. Stevens-Johnson syndrome and
toxic epidermal necrolysis are significantly more common in patients
with a particular human leukocyte antigen (HLA) allele, HLA-B*1502
(occurs almost exclusively in patients with Asian ancestry, including including Han Chinese, Filipinos, Malaysians, South Asian Indians, and
2015 F.A. Davis Company
CONTINUED
PDF Page #2
Name /bks_53161_deglins_md_disk/phenytoin
02/17/2014 09:10AM
Implement seizure precautions.
When transferring from phenytoin to another anticonvulsant, dosage adjustments
CONTINUED
phenytoin
pg 3 # 3
Implementation
Plate # 0-Composite
Thais). Avoid using phenytoin or fosphenytoin as alternatives to carbamazepine
for patients who test positive. If less serious skin eruptions (measles-like or scarlatiniform) occur, phenytoin may be resumed after complete clearing of the rash.
If rash reappears, further use of fosphenytoin or phenytoin should be avoided.
Assess mental status (orientation, mood, behavior) before and periodically during therapy. Monitor closely for notable changes in behavior
that could indicate the emergence or worsening of suicidal thoughts or
behavior or depression.
Seizures: Assess location, duration, frequency, and characteristics of seizure activity. EEG may be monitored periodically throughout therapy.
Monitor BP, ECG, and respiratory function continuously during administration of
IV phenytoin and throughout period when peak serum phenytoin levels occur
(15 30 min after administration).
Arrhythmias: Monitor ECG continuously during treatment of arrhythmias.
Lab Test Considerations: Monitor CBC, serum calcium, albumin, and
hepatic function tests prior to and monthly for the first several months,
then periodically during therapy.
May causeqserum alkaline phosphatase, GGT, and glucose levels.
Monitor serum folate concentrations periodically during prolonged therapy.
Toxicity and Overdose: Monitor serum phenytoin levels routinely. Therapeutic blood levels are 10 20 mcg/mL (8 15 mcg/mL in neonates) in patients with
normal serum albumin and renal function. In patients with altered protein binding
(neonates, patients with renal failure, hypoalbuminemia, acute trauma), free phenytoin serum concentrations should be monitored. Therapeutic serum free phenytoin levels are 1 2 mcg/mL.
Progressive signs and symptoms of phenytoin toxicity include nystagmus, ataxia,
confusion, nausea, slurred speech, and dizziness.
Potential Nursing Diagnoses
Risk for injury (Indications)
Impaired oral mucous membrane (Side Effects)
Canadian drug name.
Genetic Implication.
are made gradually over several weeks.
When substituting fosphenytoin for oral phenytoin therapy, the same total daily
dose may be given as a single dose. Unlike parenteral phenytoin, fosphenytoin may
be given safely by the IM route.
PO: Administer with or immediately after meals to minimize GI irritation. Shake
liquid preparations well before pouring. Use a calibrated measuring device for accurate dose. Chewable tablets must be crushed or chewed well before swallowing.
Capsules may be opened and mixed with food or fluids for patients with difficulty
swallowing. To prevent direct contact of alkaline drug with mucosa, have patient
swallow a liquid first, follow with mixture of medication, then follow with a full
glass of water or milk or with food.
If patient is receiving enteral tube feedings, 2 hr should elapse between feeding
and phenytoin administration. If phenytoin is administered via nasogastric tube,
flush tube with 2 4 oz water before and after administration.
Do not interchange chewable phenytoin tablets with phenytoin sodium capsules,
because they are not bioequivalent.
Capsules labeled extended may be used for once-a-day dose; those labeled
prompt may result in toxic serum levels if used for once-a-day dose.
IV Administration
IV: Slight yellow color will not alter solution potency. If refrigerated, may form
precipitate, which dissolves after warming to room temperature. Discard solution
that is not clear.
To prevent precipitation and minimize local venous irritation, follow infusion with
0.9% NaCl through the same needle or catheter. Avoid extravasation; phenytoin is
caustic to tissues; may lead to purple glove syndrome. Monitor infusion site
closely.
Direct IV: Administer undiluted. Rate: Administer at a rate not to exceed 50 mg
over 1 min in adults or 1 3 mg/kg/min in neonates. Rapid administration may
result in severe hypotension, cardiovascular collapse, or CNS depression.
Intermittent Infusion: Diluent: Administer by mixing with no more than 50
mL of 0.9% NaCl. Concentration: 1 10 mg/mL. Administer immediately following admixture. Use tubing with a 0.45- to 0.22-micron in-line filter. Rate:
Complete infusion within 1 hr at a rate not to exceed 50 mg/min. In patients who
CAPITALS indicate life-threatening, underlines indicate most frequent.
Strikethrough Discontinued.
PDF Page #3
Name /bks_53161_deglins_md_disk/phenytoin
02/17/2014 09:10AM
4
may develop hypotension, patients with cardiovascular disease, or geriatric patients maximum rate of 25 mg/min [may be as low as 5 10 mg/min]. Maximum
rate in neonates is 1 3 mg/kg/min. Monitor cardiac function and BP throughout
infusion.
Y-Site Compatibility: cisplatin.
Y-Site Incompatibility: acyclovir, alemtuzumab, alfentanil, amikacin, aminocaproic acid, aminophylline, amphotericin B cholesteryl, amphotericin B colloidal, amphotericin B lipid complex, amphotericin B liposome, ampicillin, ampicillin/sulbactam, anidulafungin, argatroban, ascorbic acid, atracurium,
atropine, azathioprine, aztreonam, benztropine, bivalirudin, bumetanide, buprenorphine, butorphanol, calcium chloride, calcium gulconate, carboplatin,
carmustine, caspofungin, cefazolin, cefepime, cefoperazone, cefotaxime, cefotetan, cefoxitin, ceftazidime, ceftriaxone, cefuroxime, chloramphenicol, chlorpormazine, ciprofloxacin, clindamycin, cyanocobalamine, cyclophosphamide, cyclosporine, cytarabine, dactinomycin, dantrolene, daptomycin, dexamethasone,
dexmedetomidine, dexrazoxane, diltiazem, diazoxide, digoxin, diltiazem, diphenhydramine, dobutamine, docetaxel, dolasetron, dopamine, doxacurium, doxorubicin hydrochloride, doxorubicin liposomal, doxycycline, enalaprilat, ephedrine, epinephrine, epirubicin, epoetin alfa, eptifibatide, ertapenem, erythromycin,
etoposide, etoposide phosphate, fenoldopam, fentanyl, fludarabine, fluorouracil,
folic acid, furosemide, ganciclovir, gemcitabine, gentamicin, glycopyrrolate,
granisetron, haloperidol, heparin, hetastarch, hydralazine, hydrocortisone sodium succinate, hydromorphone, hydroxyzine, idarubicin, ifosfamide, imipenem/
cilastatin, indomethacin, insulin, irinotecan, isoproterenol, ketamine, ketorolac,
labetalol, levofloxacin, lidocaine, linezolid, lorazepam, magnesium sulfate, mannitol, mechlorethamine, meperidine, metaraminol, methadone, methotrexate,
methyldopate, methylprednisolone, metoclopramide, micafungin, midazolam,
milrinone, mitoxantrone, morphine, moxifloxacin, multivitamin infusion, mycophenolate, nafcillin, nalbuphine, naloxone, nesiritide, nicardipine, nitroglycerin,
nitroprusside, norepinpehrine, octreotide, ondansetron, oxacillin, oxytocin, paclitaxel, palonosetron, pamidronate, pantoprazole, papaverine, pemetrexed, penicillin G, pentamidine, pentazocine, pentobarbital, phenobarbital, phentolamine,
phenylephrine, phytonadione, piperacillin/tazobactam, potassium acetate, potassium chloride, procainamide, prochlorperazine, promethazine, propofol, propranolol, protamine, pyridoxime, quinupristin/dalfopristin, ranitidine, rocuron-
Plate # 0-Composite
pg 4 # 4
ium, sodium acetate, sodium bicarbonate, streptokinase, succinylcholine,
sufentanil, tacrolimus, teniposide, theophylline, thiamine, thiotepa, ticarcillin/clavulanate, tigecycline, tirofiban, tobramycin, tolazoline, trimethoprim/sulfamethoxazole, vancomycin, vasopressin, vecuronium, verapamil, vinblastine, vincristine, vinorelbine, vitamin B complex with C, voriconazole, zoledronic acid.
Additive Incompatibility: Do not admix with other solutions or medications,
especially dextrose, because precipitation will occur.
Patient/Family Teaching
Instruct patient to take medication as directed, at the same time each day. If a dose
is missed from a once-a-day schedule, take as soon as possible and return to regular dosing schedule. If taking several doses a day, take missed dose as soon as possible within 4 hr of next scheduled dose; do not double doses. Consult health care
professional if doses are missed for 2 consecutive days. Abrupt withdrawal may
lead to status epilepticus.
May cause drowsiness or dizziness. Caution patient to avoid driving or other activities requiring alertness until response to medication is known. Do not resume
driving until physician gives clearance based on control of seizure disorder.
Caution patient to avoid alcohol and CNS depressants. Advise patient to notify
health care professional of all Rx or OTC medications, vitamins, or herbal products being taken and to consult with health care professional before taking other
medications and alcohol.
Instruct patient on importance of maintaining good dental hygiene and seeing
dentist frequently for teeth cleaning to prevent tenderness, bleeding, and gingival
hyperplasia. Institution of oral hygiene program within 10 days of initiation of phenytoin therapy may minimize growth rate and severity of gingival enlargement. Patients under 23 yr of age and those taking doses 500 mg/day are at increased risk
for gingival hyperplasia.
Advise patient that brands of phenytoin may not be equivalent. Check with health
care professional if brand or dose form is changed.
Advise diabetic patients to monitor blood glucose carefully and to notify health
care professional of significant changes.
Instruct patient to notify health care professional of medication regimen prior to
treatment or surgery.
Advise patient not to take phenytoin within 2 3 hr of antacids.
Advise patient to carry identification describing disease process and medication
regimen at all times.
2015 F.A. Davis Company
CONTINUED
PDF Page #4
Name /bks_53161_deglins_md_disk/phenytoin
02/17/2014 09:10AM
Plate # 0-Composite
pg 5 # 5
5
PDF Page #5
CONTINUED
phenytoin
Instruct patients that behavioral changes, skin rash, fever, sore throat,
mouth ulcers, easy bruising, petechiae, unusual bleeding, abdominal
pain, chills, pale stools, dark urine, jaundice, severe nausea or vomiting, drowsiness, slurred speech, unsteady gait. swollen glands,or persistent headache should be reported to health care professional immediately. Advise patient and family to notify health care professional if
thoughts about suicide or dying, attempts to commit suicide; new or
worse depression; new or worse anxiety; feeling very agitated or restless; panic attacks; trouble sleeping; new or worse irritability; acting aggressive; being angry or violent; acting on dangerous impulses; an extreme increase in activity and talking, other unusual changes in behavior
or mood occur.
Advise female patients to use an additional nonhormonal method of contraception
during therapy and until next menstrual period. Instruct patient to notify health
care professional if pregnancy is planned or suspected. Encourage patients who
become pregnant to enroll in the North American Antiepileptic Drug (NAAED)
Pregnancy Registry by calling 1-888-233-2334 or on the web at
www.aedpregnancyregistry.org. Enrollment must be done by patients themselves.
Emphasize the importance of routine exams to monitor progress. Patient should
have routine physical exams, especially monitoring skin and lymph nodes, and
EEG testing.
Evaluation/Desired Outcomes
Decrease or cessation of seizures without excessive sedation.
Suppression of arrhythmias.
Relief of neuropathic pain.
Why was this drug prescribed for your patient?
Canadian drug name.
Genetic Implication.
CAPITALS indicate life-threatening, underlines indicate most frequent.
Strikethrough Discontinued.
You might also like
- VenoferDocument13 pagesVenoferLuciano H.Vivas M.No ratings yet
- Dolan Drug StudyDocument3 pagesDolan Drug StudyLian Robbie BautistaNo ratings yet
- PrednisoneDocument3 pagesPrednisoneMaja DeraNo ratings yet
- Indometacin MonographDocument9 pagesIndometacin MonographQuiKe PvNo ratings yet
- FlagylDocument3 pagesFlagylAdrianne BazoNo ratings yet
- KetoconazoleDocument2 pagesKetoconazolenatinlalaNo ratings yet
- Managing dextrose therapyDocument2 pagesManaging dextrose therapySanket TelangNo ratings yet
- Drug Study on CelecoxibDocument11 pagesDrug Study on CelecoxibPrincess Brigitte R. PATE�ANo ratings yet
- OB Drug StudyDocument12 pagesOB Drug StudyCj AttoNo ratings yet
- AmloDocument1 pageAmloamy navajaNo ratings yet
- HaemaccelinfDocument9 pagesHaemaccelinfSisca YulistianaNo ratings yet
- (Generic Name) ® Drotaverine 40mgDocument2 pages(Generic Name) ® Drotaverine 40mgSangar Sardar100% (1)
- See Full Prescribing Information For Complete Boxed WarningDocument43 pagesSee Full Prescribing Information For Complete Boxed WarningParishan SaeedNo ratings yet
- Drug Study Ssalbutamol7Document3 pagesDrug Study Ssalbutamol7Gorgeouschelle FeriaNo ratings yet
- Drug Study On EPINEPHRINEDocument6 pagesDrug Study On EPINEPHRINEshadow gonzalezNo ratings yet
- EMERGENCY DRUG STUDYDocument3 pagesEMERGENCY DRUG STUDYGrace Santos MirandaNo ratings yet
- Ertapenem (Invanz)Document1 pageErtapenem (Invanz)Adrianne BazoNo ratings yet
- Prazosin Tablet (Prazosin)Document6 pagesPrazosin Tablet (Prazosin)Chenta Bulan MerinduNo ratings yet
- Methyldopa nursing management for hypertensionDocument4 pagesMethyldopa nursing management for hypertensionRico Mae ValenciaNo ratings yet
- Drug StudyDocument5 pagesDrug StudyRai D. MacapantonNo ratings yet
- DoxycyclineDocument18 pagesDoxycyclineSabab MunifNo ratings yet
- AminophyllineDocument6 pagesAminophyllineapi-3797941100% (1)
- CoversylDocument3 pagesCoversylianecunarNo ratings yet
- DS (Calcium + Vit. D)Document6 pagesDS (Calcium + Vit. D)Mary April MendezNo ratings yet
- Linezolid (Zyvox)Document1 pageLinezolid (Zyvox)ENo ratings yet
- Verapamil HCLDocument3 pagesVerapamil HCLMae Ann Bueno CastillonNo ratings yet
- Fludrocortisone (Florinef)Document17 pagesFludrocortisone (Florinef)passer byNo ratings yet
- Drug StudyDocument3 pagesDrug StudyKwin SaludaresNo ratings yet
- Drug Analysis CefoxitinDocument2 pagesDrug Analysis CefoxitinNika LoNo ratings yet
- Isoprenaline Infusion 2016Document3 pagesIsoprenaline Infusion 2016Glory Claudia KarundengNo ratings yet
- Antimalarial DrugsDocument7 pagesAntimalarial DrugsHilmanNo ratings yet
- Serratiopeptidase tablets effectively treat inflammationDocument12 pagesSerratiopeptidase tablets effectively treat inflammationdracula386No ratings yet
- Drug StudyDocument6 pagesDrug Studyjohnclement_dcNo ratings yet
- Drug StudyDocument6 pagesDrug StudyChickz HunterNo ratings yet
- Ketesse Pain Reliever GuideDocument8 pagesKetesse Pain Reliever GuideDhurai OnelyNo ratings yet
- EpinephrineDocument6 pagesEpinephrineapi-3797941100% (2)
- Side Effects:: AtropineDocument7 pagesSide Effects:: AtropinekletadaNo ratings yet
- IV Fluid Therapy Guide for Safer Patient CareDocument1 pageIV Fluid Therapy Guide for Safer Patient CarePatricia VasquezNo ratings yet
- Drug PrilosecDocument1 pageDrug PrilosecSrkocher100% (1)
- Drug Study FUROSEMIDE (Eugene San)Document2 pagesDrug Study FUROSEMIDE (Eugene San)Ana LanticseNo ratings yet
- Metoclopramide (Reglan)Document1 pageMetoclopramide (Reglan)ENo ratings yet
- Cefpodoxime Proxetil - Print VersionDocument5 pagesCefpodoxime Proxetil - Print Versionchristina_1990No ratings yet
- Pathophysiology of Nephrotic SyndromeDocument1 pagePathophysiology of Nephrotic SyndromeKristian Karl Bautista Kiw-isNo ratings yet
- Medication for Postpartum HemorrhageDocument1 pageMedication for Postpartum HemorrhageclarimerNo ratings yet
- Omeprazole Nursing ResponsibilitiesDocument2 pagesOmeprazole Nursing ResponsibilitiesRea LynNo ratings yet
- Drug StudyDocument11 pagesDrug StudyKenn yahweexNo ratings yet
- Mesna: Mesna, Sold Under The BrandDocument17 pagesMesna: Mesna, Sold Under The BrandAndry HamdaniNo ratings yet
- Albuterol, Accuneb Drug CardDocument2 pagesAlbuterol, Accuneb Drug Carddnw876No ratings yet
- DRUG NAME: Hydroxyurea: Synonym (S) : Common Trade Name (S) : ClassificationDocument7 pagesDRUG NAME: Hydroxyurea: Synonym (S) : Common Trade Name (S) : ClassificationDewinta AbutNo ratings yet
- NCP and Drug Study Forms FINALDocument9 pagesNCP and Drug Study Forms FINALVince Troy AquinoNo ratings yet
- Miglitol (Glyset)Document1 pageMiglitol (Glyset)ENo ratings yet
- Detrol (Tolterodine)Document1 pageDetrol (Tolterodine)ENo ratings yet
- The Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016Document10 pagesThe Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016ddandan_2No ratings yet
- Colestipol Hydrochloride Nursing ConsiderationsDocument3 pagesColestipol Hydrochloride Nursing ConsiderationsAbby AngNo ratings yet
- Emergency Drugs Drug StudyDocument15 pagesEmergency Drugs Drug StudyCathrine Sandile Tangwara100% (1)
- Drug Card PhenytoinDocument5 pagesDrug Card PhenytoinGifther JohnNo ratings yet
- Brand Name: Dilantin Generic Name: Phenytoin Indication: Dilantin Is IndicatedDocument4 pagesBrand Name: Dilantin Generic Name: Phenytoin Indication: Dilantin Is Indicatedianecunar100% (1)
- Pedia Drug StudyDocument11 pagesPedia Drug StudyPeetah PanNo ratings yet
- Drug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrDocument7 pagesDrug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrMary EnsomoNo ratings yet
- 63 Must Know Lab Values Cheat Sheet - NCLEX (Caribbean Nurses of Puerto Rico and Latin America) PDFDocument4 pages63 Must Know Lab Values Cheat Sheet - NCLEX (Caribbean Nurses of Puerto Rico and Latin America) PDFChristineBiankii100% (1)
- Script BBDocument2 pagesScript BBRhawnie B. GibbsNo ratings yet
- Food Sovereignty, Food Security and Health Equity: A Meta-Narrative Mapping ExerciseDocument16 pagesFood Sovereignty, Food Security and Health Equity: A Meta-Narrative Mapping ExerciseRhawnie B. GibbsNo ratings yet
- Alphabet Worksheets From A To ZDocument28 pagesAlphabet Worksheets From A To ZFadi Al Shhayed100% (1)
- Informed Consent JournalDocument8 pagesInformed Consent JournalRhawnie B. GibbsNo ratings yet
- CSA Step-By-step Guide CS Edit 02.03.07Document45 pagesCSA Step-By-step Guide CS Edit 02.03.07Rhawnie B. GibbsNo ratings yet
- FDA Bans Times Natural Capsules, X Plus Men, OthersDocument2 pagesFDA Bans Times Natural Capsules, X Plus Men, OthersGhanaWeb EditorialNo ratings yet
- Filgrastim Boosts Neutrophil Recovery After ChemotherapyDocument3 pagesFilgrastim Boosts Neutrophil Recovery After ChemotherapyKyla Barrera TabungarNo ratings yet
- Drug-Induced Liver Disease.Document16 pagesDrug-Induced Liver Disease.Dr. Ammar Khalil100% (1)
- Autonomic Nervous System DrugsDocument11 pagesAutonomic Nervous System Drugssbjon984924100% (1)
- Pharmacy (2014)Document4 pagesPharmacy (2014)Ali Ghahreman50% (2)
- Pharm Exam1Document17 pagesPharm Exam1Jill Putman Beistline75% (4)
- Larry's Complaint c1Document32 pagesLarry's Complaint c1Jeff MorrisNo ratings yet
- Anaphylaxis: Identification, Management and PreventionDocument5 pagesAnaphylaxis: Identification, Management and PreventionÓscar A. Castejón CruzNo ratings yet
- Critical Care Antibiotic GuideDocument1 pageCritical Care Antibiotic GuideAdna NelsonNo ratings yet
- Marketing Management FinalDocument22 pagesMarketing Management FinalRadhey Sham SNo ratings yet
- Amitriptyline 25 MG Tablets BP: Patient Information LeafletDocument2 pagesAmitriptyline 25 MG Tablets BP: Patient Information LeafletAri SyairiNo ratings yet
- Minimum Infusion Volume PDFDocument25 pagesMinimum Infusion Volume PDFบอส เลิศเกียรติรัชตะNo ratings yet
- Video de Evidence Live LongerDocument3 pagesVideo de Evidence Live LongerLiliana López0% (1)
- Ameriplan-Health Ameriplan BrochureDocument5 pagesAmeriplan-Health Ameriplan Brochureapi-242298828No ratings yet
- L30030 ATR FTIR Spectra of Pharmaceutical Tablets and CapsulesDocument11 pagesL30030 ATR FTIR Spectra of Pharmaceutical Tablets and CapsulesPrianurraufikachmadNo ratings yet
- Hospital Pharmacy Group 6Document67 pagesHospital Pharmacy Group 6Anonymous qlIp8U100% (1)
- Dangers of Prescribed Psychiatric DrugsDocument4 pagesDangers of Prescribed Psychiatric DrugsNikos TaramasNo ratings yet
- BooksDocument2 pagesBooksCharudatta RakhundeNo ratings yet
- Druge Abuse FinalDocument3 pagesDruge Abuse FinalJmart84No ratings yet
- Food-To-Drug InteractionDocument5 pagesFood-To-Drug InteractionChloe PaguelNo ratings yet
- Cardiology 2012 MrcppassDocument127 pagesCardiology 2012 MrcppassRaouf Ra'fat SolimanNo ratings yet
- EyeDocument12 pagesEyePatziedawn GonzalvoNo ratings yet
- PNF Form No. 4 - ExemptionDocument4 pagesPNF Form No. 4 - ExemptionKen SanchezNo ratings yet
- HydrochlorothiazideDocument1 pageHydrochlorothiazideKatie McPeekNo ratings yet
- R.A. 10918 - The Philippine Pharmacy ActDocument4 pagesR.A. 10918 - The Philippine Pharmacy ActAndrea Lois OteyzaNo ratings yet
- Chapter 12: Medication Dosage Forms and Routes of AdministrationDocument29 pagesChapter 12: Medication Dosage Forms and Routes of AdministrationJana EncaboNo ratings yet
- Multiple IV Bolus AdministrationDocument21 pagesMultiple IV Bolus AdministrationIka NurzijahNo ratings yet
- MCQ 1Document9 pagesMCQ 1Hasan MohamedNo ratings yet
- Pre-Operation Checklist for Voice Feminization Surgery (VFSDocument2 pagesPre-Operation Checklist for Voice Feminization Surgery (VFSRachel SchererNo ratings yet
- Format FormulairumDocument76 pagesFormat FormulairumfennyrahmaNo ratings yet