Professional Documents
Culture Documents
The EffectofMusicReinforcementforNon-NutritiveSuckingonNippleFeedingOfPrematureInfants PDF
The EffectofMusicReinforcementforNon-NutritiveSuckingonNippleFeedingOfPrematureInfants PDF
Uploaded by
Emaa AmooraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The EffectofMusicReinforcementforNon-NutritiveSuckingonNippleFeedingOfPrematureInfants PDF
The EffectofMusicReinforcementforNon-NutritiveSuckingonNippleFeedingOfPrematureInfants PDF
Uploaded by
Emaa AmooraCopyright:
Available Formats
Continuing Nursing Education
Posttest can be found on page 146.
The Effect of Music Reinforcement for
Non-Nutritive Sucking on Nipple Feeding
Of Premature Infants
Jayne M. Standley, Jane Cassidy, Roy Grant, Andrea Cevasco,
Catherine Szuch, Judy Nguyen, Darcy Walworth, Danielle Procelli,
Jennifer Jarred, Kristen Adams
T
he premature infants suck-
ing ability is a critical behav- In this randomized, controlled multi-site study, the pacifier-activated-lullaby sys-
ior for both survival and neu- tem (PAL) was used with 68 premature infants. Dependent variables were a) total
rological development, and number of days prior to nipple feeding, b) days of nipple feeding, c) discharge
must be sophisticated enough to sus- weight, and d) overall weight gain. Independent variables included contingent
tain independent nipple feeding. Oral music reinforcement for non-nutritive sucking for PAL intervention at 32 vs. 34 vs
feeding is a complex task for the pre- 36 weeks adjusted gestational age (AGA), with each age group subdivided into
mature infant affected by many vari- three trial conditions: control consisting of no PAL used vs. one 15-minute PAL
ables, especially the immaturity of the trial vs. three 15-minute PAL trials. At 34 weeks, PAL trials significantly shortened
neurological system and its readiness gavage feeding length, and three trials were significantly better than one trial. At
to coordinate the suck-swallow- 32 weeks, PAL trials lengthened gavage feeding. Female infants learned to nip-
breathe response. Research suggests ple feed significantly faster than male infants. It was noted that PAL babies went
that promoting non-nutritive sucking home sooner after beginning to nipple feed, a trend that was not statistically sig-
(NNS) will facilitate nipple feeding, nificant.
but more detailed investigation is
needed for development of effective
care protocols (McGrath & Braescu, essarily prolong hospitalization. This nally regulated rhythms (Goff, 1985).
2004). Feeding opportunities offered study was designed to test specific In fact, the appearance of sucking
too early may lead to negative physi- parameters of a music reinforcement behavior coincides with the first
ologic outcomes, such as apnea and protocol to promote NNS and subse- appearance of fetal brain waves. NNS
bradycardia. Delaying the initiation quent effects on duration of gavage is a reflex requiring physiologic matu-
of feeding opportunities may unnec- feeding. ration but is capable of being altered
by learning experiences (Anderson &
Vidyasagar, 1979; Bernbaum, Pereira,
Jayne M. Standley, PhD, MT-BC, is a Robert
O. Lawton Distinguished Professor of Music, Development of Watkins, & Peckham, 1983). NNS sig-
Florida State University and Tallahassee Non-Nutritive Sucking nificantly reduces distress and physio-
Memorial HealthCare, Tallahassee, FL. logical responses of premature infants
NNS is the first rhythmic behavior subjected to painful procedures (Boyle
Jane Cassidy, PhD, is Professor and Chair of in which the infant engages and is
Music Education, Louisiana State University et al., 2006; Cignacco et al., 2007;
theorized to contribute to neurologi- Mathai, Natrajan, & Rajalakshmi,
and Womans Hospital of Baton Rouge, Baton
Rouge, LA. cal development by facilitating inter- 2006; South, Strauss, South, Boggess,
Roy Grant, PhD, MT-BC, is a Retired
Professor of Music, the University of Georgia, Jennifer Jarred, MM, MT-BC, is a Music Therapist, Florida State University, Tallahassee, FL, and
Athens, GA. Lawnwood Regional Medical Center, Fort Pierce, FL.
Andrea Cevasco, PhD, MT-BC, is an Kristen Adams, MM, MT-BC, was a Music Therapy Intern, Florida State University and
Assistant Professor of Music Therapy, the Tallahassee Memorial HealthCare, Tallahassee, FL, at the time this article was written.
University of Alabama, Tuscaloosa, AL. Acknowledgments: Healing HealthCare Systems and Ohmeda Medical provided equipment
Catherine Szuch, MM, MT-BC, is a Research and technical support to the study. We are indebted to them for this support. The study would not
Assistant, the University of North Carolina have been possible without extensive assistance from a great many medical personnel. Sincere
Medical Center, Chapel Hill, NC. appreciation is expressed to the nursing staff and the physicians of the four nurseries involved:
Tallahassee Memorial HealthCare Neonatal Intensive Care Unit (Dr. Todd Patterson,
Judy Nguyen, MM, MT-BC, is a Music Neonatologist), Womans Hospital Baton Rouge Neonatal Intensive Care Unit (Dr. Steven
Therapist, Yale Childrens Hospital, New Spedale, Neonatologist), Athens Regional Medical Center Special Care Nursery (Dr. Lia Fasse,
Haven, CT. Neonatologist), and UNC Medical Center NC Childrens Hospital Newborn Critical Care Center
Darcy Walworth, PhD, MT-BC, is an (Dr. Dianne Marshall and Dr. Carl Bose, Neonatologists). Special appreciation is given to the fol-
Assistant Professor of Music Therapy, Florida lowing individuals who assisted with referrals or liaison within the hospitals: Luci Butler, MT, stu-
State University and Tallahassee Memorial dent at University of Georgia; Cori Pelletier, MT, student at University of Georgia; Jennifer
HealthCare, Tallahassee, FL. Whipple, MT-BC; and Cindy Quackenbush, RN, Kim Bloyd, RN, and Stephanie Bickis, RN, at
Danielle Procelli, MM, MT-BC, was a Music
Tallahassee Memorial HealthCare. We are most appreciative to the parents who allowed their
Therapy Intern, Florida State University and infants to participate in this study.
Tallahassee Memorial HealthCare, Tallahassee, Statement of Disclosure: The authors reported no actual or potential conflict of interest in rela-
FL, at the time this article was written. tion to this continuing nursing education article.
138 PEDIATRIC NURSING/May-June 2010/Vol. 36/No. 3
& Thorp, 2005). Therefore, the pacifi- organization. Cues are not easily read, hospital days. These studies ranged
er as a stimulant for NNS appears to and transitions in state are not from 10 to 59 participants (Pinelli &
be very important to the premature smooth. When the infant is neurolog- Symington, 2000). Pacifiers given 10
infants well-being and care in the ically immature or shows poor behav- minutes prior to nipple feeding
neonatal intensive care unit (NICU). ioral state organization at feeding increased the inactive awake state of
In the NICU, NNS opportunities opportunities, heart rate increases, the infant and decreased the total
(pacifiers) have been paired with gav- and respiratory interruptions create length of time for ingestion of nutri-
age feedings and shown to promote apneic episodes. Sucking responses tion (McCain, 1995). Due to adverse
infant development in a variety of may be weak or uncoordinated. physiological reactions to prolonged
ways. NNS lowers heart rate (McCain, Energy consumption and effort dur- feeding, the standard of care for pre-
1995; Woodson & Hamilton, 1988) ing nutritive sucking in premature mature infants usually limits a nipple
and increases oxygenation (Burroughs, infants can reduce oxygen saturation feeding opportunity to 30 minutes
Asonye, Anderson-Shanklin, & and can expend calories resulting in (Gardner, Garland, Merenstein, &
Vidyasagar, 1978). It also increases weight loss (Hill, 1992). Prior to 34 Lubchenco, 1997). After that time,
weight gain of the infant even when weeks adjusted gestational age (AGA), the remaining nutrition is given by
nutritional intake is controlled (Field et gavage feeding (oral-gastric [OG] or gavage tube. Strengthening the suck
al., 1982; Kanarek & Shulman, 1992). naso-gastric [NG] tube) is necessary and increasing the rate of nutritional
It is theorized that NNS calms but stressful for the premature infant. intake is frequently a step to reducing
infants and facilitates lower activity the length of a nipple feeding
levels, resulting in energy conserva- episode. Most infants who can
tion and subsequent weight gain. This Development of Feeding demonstrate adequate oral intake of
theory is supported by the finding Ability nutrition within the 30-minute inter-
that NNS with gavage feeding results val are discharged within 24 hours
in increased duration of inactive alert The development of sucking abili- (McGrath & Braescu, 2004).
state and faster return to and ty for feeding is correlated with neu-
increased length of quiet sleep rological maturity, but not gestational
(DiPietro, Cusson, Caughy, & Fox, age or birth weight (McCain, 1992; Effects of Music Therapy
1994; Gill, Behnke, Conlon, McNeely, Medoff-Cooper & Gennaro, 1996).
& Anderson, 1988; Goff, 1985; Specifically, higher sucking pressure, In the NICU
McCain, 1992, 1995). Other benefits number of sucking bursts, and dura- Research has shown that a variety
of NNS during gavage feeding include tion of pauses between bursts at 34 of stimulation techniques adminis-
decreased length of hospital stay and weeks gestational age correlate with tered to pre-term infants can offset
decrease in necessity for tube feedings higher psychomotor scores at 6 some adverse neurological effects of
(Bernbaum et al., 1983; Field et al., months of age. Palmers (1993) assess- premature birth and the adverse conse-
1982). A meta-analysis on research ment of premature infants consistent- quences of prolonged hospitalization
assessing clinical outcomes of offering ly found an immature pattern of suck- (Britt & Myers, 1994; Gomes-Pedro et
NNS during gavage feeding found it ing, consisting of 3 to 5 sucks in a al., 1995; Harrison, 1985; Oehler, 1993;
decreased length of hospitalization by burst followed by a pause to breathe. Rauh et al., 1987). Music, particularly,
an average of 6.3 days and allowed More mature, term infants sucked 10 has been effective with premature
premature infants to begin bottle to 30 times in a prolonged burst and infants in increasing weight gain,
feeding an average of 2.9 days sooner alternated breathing with sucking. reducing observed stress behaviors,
(Schwartz, Moody, Yarndi, & Mature nutritive sucking coordina- reducing length of hospitalization by
Anderson, 1987). A more recent meta- tion would seem to be a highly up to 11 days for female (not male)
analysis using NNS with gavage feed- important goal for premature infants infants, and increasing oxygen satura-
ing also found a significant decrease for a variety of health, growth, and tion levels for short periods of time
in length of stay (Pinelli & developmental reasons. (Caine, 1992; Cassidy & Standley,
Symington, 2005). The coordinated suck-swallow- 1995; Chapman, 1979; Standley, 1998;
breathe response develops around the Standley & Moore, 1995; Whipple,
34th week of gestation and becomes 2008). Survey results show that 72% of
Feeding Problems of the possible when myelination of the U.S. NICUs play music for premature
medulla has occurred (McGrath & infants (Field, Hernandez-Reif, Feijo, &
Premature Infant Braescu, 2004). It is a precursor to Freedman, 2006).
The well, term infant is born capa- nutritive sucking ability and nipple Auditory capability is an early, dis-
ble of feeding with a coordinated, feeding. Medical procedures, such as criminative ability of the fetus
suck-swallow-breathe response that intubation, can delay the develop- (Cheour-Luhtanen et al., 1996). It has
occurs without detrimental changes ment of a coordinated sucking pat- been documented that as early as 18
in heart rate or respiratory capabili- tern in premature infants. The transi- weeks gestational age, loud sounds
ties. Further, the term infants behav- tion from gavage to nipple feeding is cause the fetal heart rate to increase,
ioral states are organized and easily often difficult for the premature and at 25 weeks, the major structures
read by caregivers. In the presence of infant, and sometimes long-term of the ear are essentially in place. At
food, crying due to hunger quickly problems develop, such as nipple 25 to 27 gestation weeks, most fetuses
moves to a state of alertness with the aversion or aversion to oral feeding begin to respond inconsistently to
infant focused for feeding. This occurs (Palmer, 1993). sound by moving or kicking (Cheour-
smoothly without detrimental physi- Oral feeding skill can be assisted Luhtanen et al., 1996). At 30 to 35
ological changes (McCain, 1992). through NNS. A Cochrane review of weeks, the infant hears maternal
Unlike the term infant, the prema- 19 studies on benefits of pacifiers with sounds, responds to these sounds,
ture infant is neurologically immature premature infants found that NNS and begins to discriminate among
and has impaired behavioral state significantly decreased number of speech sounds, particularly with
PEDIATRIC NURSING/May-June 2010/Vol. 36/No. 3 139
The Effect of Music Reinforcement for Non-Nutritive Sucking on Nipple Feeding of Premature Infants
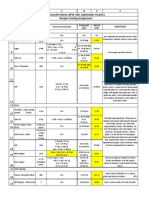
regard to pitch and rhythm Table 1.
(Lecanuet, Granier-Deferre, & Busnel, Design and Number of Subjects by Gender
1995). The premature infant ready for
transition to nipple feeding has the PAL Trials by Gestational Age Male n Female n Total n
ability to hear, discriminate, and ben- 32 Weeks AGA
efit from auditory input.
At term birth, females are more No-contact control 4 4 8
developed with regard to hearing 1 PAL trial 4 4 8
(Cassidy & Ditty, 2001), have better
tactile and oral sensitivity, and are 3 PAL trials 4 4 8
more responsive to smiling, sweet 34 Weeks AGA
tastes, talking, eye-to-eye contact, and
the pacifier. Cerebral blood flow in No-contact control 4 4 8
girls is significantly lower than in 1 PAL trial 4 4 8
males. Male infants demonstrate
more startles, more muscle activity, 3 PAL trials 3 3 6
and more physical strength. With 36 Weeks AGA
regard to auditory capability at birth,
male infants actually have shorter No-contact control 3 4 7
cochlea, fewer hair cells, and less 1 PAL trial 4 4 8
response to aural stimuli. Female
infants hear high frequencies better 3 PAL trials 3 4 7
than males, which is particularly Total n 33 35 68
advantageous when listening to
music with its wide range of frequen- Note: PAL = pacifier-activated lullaby.
cies (Cassidy & Ditty, 2001).
A meta-analysis of studies using
music in the NICU demonstrated sig- Purpose of Study weeks AGA. These age groupings were
nificant clinical benefits across a vari- chosen for the following reasons:
ety of physiological and behavioral The purpose of this study was to NICU personnel disagree on when to
measures (Standley, 2002). Linguistics ascertain the effect of the pacifier-acti- intervene to begin oral feeding train-
research showed that lullabies of all vated lullaby system (PAL) on cessa- ing. Some believe the infant is too
cultures combine language informa- tion of gavage feeding of premature neurologically immature to benefit
tion and use calming, rhythmic stim- infants due to oral feeding achieve- from intervention prior to 34 weeks.
uli. Because it is desirable to reduce ment. Cessation of gavage feeding Others believe that starting interven-
stress and calm premature infants in was operationally defined as the date tion before 34 weeks facilitates the
the NICU and because infants leaving of the last gavage feeding given by infants transition from gavage feed-
the womb too early are missing lan- NICU personnel. Specific aims were ing at 34 weeks. Infants still not nip-
guage input from their mothers voic- to: ple feeding at 36 weeks are considered
es, lullabies are the music of choice Determine whether gender affects seriously delayed, and benefits of typ-
for pacification and language devel- achievement of nipple feeding ical NICU interventions are ques-
opment of premature infants skills resulting from PAL usage. tioned. Therefore, it was decided to
(Standley, 1998, 2003a). Determine whether number of test intervention at 34 weeks AGA
Prior studies have shown that con- PAL trials (0, 1, or 3) affect nipple and the two weeks before and after
tingent music (such as pacifier-activat- feeding skills. this midpoint. One trial vs. three tri-
ed lullabies [PALs]) increased pacifier Determine whether age at PAL als were contrasted because prior
sucking rate of premature infants intervention (32, 34, or 36 weeks research with the PAL showed that
more than 2.5 times (Standley, 2000) AGA) affects nipple feeding skills. infants learned to suck frequently
and also increased subsequent feeding enough to sustain the music in one
rate (Standley, 2003b). Infants given trial and improved their oral feeding
one PAL trial 30 minutes prior to a late Method rate after only one trial. It was
afternoon oral feeding attempt signifi- unknown whether only one trial
cantly increased the amount of nutri- Participants and Design might affect the number of days until
tion ingested/minute when compared The design of this study was a 3x3- independent nipple feeding was
to their feeding rate during a morning block design contrasting number of achieved, and three trials seemed suf-
oral feeding attempt. Cevasco and repetitions of PAL trials by gestational ficient to note changes in nipple feed-
Grant (2005) used the PAL in multiple age at the beginning of the trial. Table ing benefits if they would occur due
trials with 62 premature infants and 1 details the design and number of to PAL intervention.
found strong trends for increased participants in each group. Following Dependent variables were:
weight gain with increasing age and referral and receipt of informed con- Days prior to nipple feeding com-
PAL trials, though these increases were sent, premature infants who were puted by counting days from
not substantial enough to be statisti- born prior to 32 weeks gestational age birth to date of last OG/NG feed
cally significant. Little other research as measured by Dubowitz criteria recorded on each infants daily
exists to determine the most appropri- were randomly assigned by gender to chart by nurses.
ate age to begin music reinforcement three intervention groups (no-contact Days of nipple feeding prior to
for NNS or the number of trials neces- control, 1 PAL trial, or 3 PAL trials) discharge computed by counting
sary to facilitate nipple feeding of pre- and further divided into time of inter- days from last OG/NG feed to dis-
mature infants. vention occurring at 32, 34, or 36 charge date. (Note: The two meas-
140 PEDIATRIC NURSING/May-June 2010/Vol. 36/No. 3
ures of feeding days when added piration or apnea, flushing or effects and were especially recorded to
together equal length of hospital- mottling of skin, tremors, startles, reduce alerting musical stimuli.
ization.) flayed fingers or hand in stop Recording criteria included no
Discharge weight recorded on the position, eye rolling or floating, changes in tempo, no changes in vol-
dis whimpering, hiccoughing, spit- ume level, no key changes, and no
Weight gain computed by sub- ting up, and gagging. No such changes in accompaniment style. The
tracting birth weight from dis- responses were noted in response music was presented at 65 dB (Scale
charge weight. to the PAL. C) via small speakers placed binaural-
Participants were referred for the Infants were not held but ly in the incubator above the infants
study by medical staff when the remained in the crib or incubator head. The music sustained for 10 sec-
infant was deemed able to tolerate lying on their backs or sides to onds and subsequently shut off unless
two simultaneous modes of stimula- reduce additional stimulation. reactivated by another suck, therefore
tion (pacifier and auditory stimula- PAL pacifier pressure = one bar on making the presentation of music
tion) and if still gavage feeding at machine menu to begin training. stimuli contingent on the sucking
time of study. Upon referral, the Treatment duration = maximum behavior of the infant. All infants
infant was randomly assigned to a of 15 minutes opportunity for were lying on their backs or sides dur-
trial condition by age group. If the sucking. ing PAL trials. Although it did not
infant achieved nipple feeding prior Discontinue when infant rejects occur, provisions were made in the
to attaining the randomly assigned pacifier twice or falls asleep. protocol to discontinue use of the
age, the infant was not enrolled in the Researchers were not a part of the pacifier if signs of infant stress were
study. The protocol for the study medical staff but were professionals observed. PAL settings allowed music
excluded infants who: who came to the NICU at the same reinforcement after one trigger (suck)
Were intubated at the time of the time each day to run PAL trials. and at the lowest amount of pressure
study. Medical staff that made referrals for change (weakest suck).
Had severe abnormalities that the study and who determined readi- The experimental infants received
affected ability to suck, feed, or ness for discharge were blind as to either one 15-minute trial with the
learn, including abnormalities of whether the infants were subsequent- PAL or three trials within a 5-day peri-
the oral cavity, hydrocephalus, ly enrolled in the study or to their od at the time of their achieving the
Down syndrome, and significant random assignment of intervention randomly assigned age and still rely-
neurological disorders, such as group. Many infants received PAL ing on gavage feeding. PAL trials
intraventricular hemorrhage of clinical treatment by the research occurred at the same time each day
levels III or IV, periventricular team, but medical personnel were not between 4:00 to 5:00 p.m. and were
leukomalacia, or hypoxic- aware whether a specific infants PAL not given in relationship to feeding
ischemic encephalopathy. usage occurred for the purpose of data times of individual participants. A
Had positive results on screen for collection for this study. Participants prior study that had compared morn-
illegal drug use by the mother. in this study received only the num- ing and afternoon feeding rates had
Criteria for referral included the ber of PAL trials specified in the group shown the PAL intervention to be
infant: cohort to which they were randomly effective in this time frame (Standley,
Was determined to be able to tol- assigned. 2003b). The no-contact control
erate two simultaneous modes of groups met the same criteria but
stimulation (pacifier and auditory Sites received no PAL intervention. Data
stimulation). The study was conducted by music were recorded by the researchers from
Had no indication of infection therapy researchers from four major the nurses notes. Nurses were blind
requiring quarantine. universities at four critical care nurs- to the purpose of the study and to
Was ready to begin some OG eries in regional hospitals in the infants status in the study. Data
feeds. southeast. It was approved by the included date of birth, birth weight,
Protocol was as follows: Human Subjects Committees at each gestational age by Dubowitz criteria at
Medical staff of the NICU made university and by the Institutional birth, date of last gavage (naso-gastric
referral for PAL. Review Boards at each hospital. The or oral-gastric) feeding, discharge
PAL was presented at least a half sites included Site A, a 40-bed Level III date, and discharge weight.
hour prior to a scheduled feeding. NICU; Site B, a 68-bed Level III NICU;
The nurse caring for the child Site C, a 10-bed special care nursery;
gave permission on the day the and Site D, a 48-bed Level III newborn
Results
PAL was presented, affirming that critical care center. Because some sites completed
additional stimulation was appro- many more participants than others,
priate for the child at that time. Procedure data were analyzed by site to deter-
(Sometimes infants had had a Contingent music was delivered mine if location affected results.
stressful day, and further stimuli via the PAL (Standley, 2000). With Tables 2 and 3 show birth weight and
were contraindicated.) this equipment, an infant sucks on a gestational age at birth by site and
Music was located adjacent to and Wee Soothie pacifier fitted with an gender.
outside the crib or incubator with adaptor housing a computer chip that SPSS Two-Way Analysis of birth
decibel level averaging 60 to 65 activates a CD player outside the gestational age by gender and site
dB measured at infants ear (Scale incubator. The music stimulus was a showed no differences for gestational
C, 1 volume bar on PAL machine). continuous selection of lullabies sung age at birth among sites (F = 2.522, df
The protocol stipulated that the by a young female with minimal = 3, p = 0.066) or for gender by site (F
use of PAL would be discontinued accompaniment. The lullabies were = 1.286, df = 3, p = 0.288). Overall, the
if signs of infant distress were traditional lullabies selected by the gestational age at birth for all males
observed, including irregular res- music therapists for their soothing was significantly earlier than that for
PEDIATRIC NURSING/May-June 2010/Vol. 36/No. 3 141
The Effect of Music Reinforcement for Non-Nutritive Sucking on Nipple Feeding of Premature Infants
Table 2. all females (F = 5.529, df = 1, p =
Mean Birth Weight in Kilograms by Site and Gender 0.022). SPSS Two-Way Analysis of
birth gestational age by randomly
Site Male Female Overall Mean assigned age groups at time of study
and by number of trials showed no
Site A (n = 28) 1.0758 1.0824 1.0796
significant difference among PAL tri-
Site B (n = 18) 1.296 1.1572 1.165 als groups (F = 2.016, df = 2, p = 0.142)
and also showed that infants random-
Site C (n = 18) 1.2580 1.3896 1.3238*
ly assigned to the 36-week age group
Site D (n = 4) 1.2583 0.5530 1.0820 at time of study were born significant-
ly earlier than infants in other age
Overall Mean Weight 1.1949 1.1655 1.1798 groups (F = 4.11, df = 2, p = 0.021).
Notes: N = 68; no significant difference by gender. This was predictable and inevitable
*p < 0.05, Site C babies significantly higher in birth weight than Site A and Site D because infants born earlier have
babies. more difficulty learning to nipple feed
and are more likely to still be gavage
feeding at 36 weeks adjusted gesta-
tional age.
Table 3. SPSS Two-Way Analysis of birth
Mean Gestational Age at Birth by Site and Gender weight data by gender and site
showed no significant difference by
Site Male Female Overall Mean gender (F = 2.342, df = 1, p = 0.131)
but differences by site. Infants from
Site A (n = 28) 29.0 28.5 28.7 Site C had significantly higher birth
Site B (n = 18) 29.6 28.9 29.3 weights (F = 2.910, df = 3, p = 0.042)
than the infants at Site A (p = 0.014)
Site C (n = 18) 30.1 30.0 30.1 and at Site D (p = 0.040). SPSS Two-
Site D (n = 4) 30.3 26.0 29.2 Way Analysis of birth weight data by
age at study and by trials showed no
Overall Mean Weight 29.6* 28.9 29.2 significant differences among trials (F
= 1.345, df = 2, p = 0.270). Again, as
Notes: N = 68; no significant difference by site. expected, the infants in the 36-week
*p < 0.05, males significantly older than females at birth. age group at the time of the study
were born with significantly lower
birth weights than those in all other
age groups (F = 6.867, df = 2, p =
Table 4. 0.002).
Mean Subject Characteristics by Age at Study and by PAL Trials Because infant characteristics data
showed few statistical differences by
Birth Age in site or gender, data were pooled for
PAL Trials by Gestational Age Birthweight in Kg Gestational Weeks subsequent analyses. Table 4 shows
32 Weeks AGA pooled birthweight and gestational
age at birth data for participants by
Control (n = 8) 1.39 30.4 age at study and trials.
1 PAL trial (n = 8) 1.26 29.3 Data for each of the four depend-
ent variables were subjected to Two-
3 PAL trials (n = 8) 1.27 29.6 Way Analyses of Variance for compar-
32-week total 1.31 29.8 ison by gender and trials. Females (M
= 7.03) nipple fed significantly longer
34 Weeks AGA prior to discharge than did males (M =
Control (n = 8) 1.09 28.9 5.70, p < 0.0001). This means they
succeeded in nipple feeding sooner
1 PAL trial (n = 8) 1.25 29.3 than males. This result was expected
3 PAL trials (n = 6) 1.42 30.6 because female premature infants
generally show faster maturation
34-week total 1.24 29.5 than male infants (Standley, 2003a).
36 Weeks AGA There were no other gender differ-
ences on any of the four dependent
Control (n = 7) 0.91 28.1 variables or by number of trials.
1 PAL trial (n = 8) 0.94 27.9 Analysis by site showed that
infants at Site A were discharged at
3 PAL trials (n = 7) 1.12 29.3 significantly lower weights than other
36-week total 1.18 28.4 sites (F = 14.919, df = 3, 60, p =
0.0001), but they were also born at
Note: N = 68. slightly lower birth weights than the
other participants. Subsequently,
their weight gain was also significant-
ly less while in the hospital (F = 4.883,
142 PEDIATRIC NURSING/May-June 2010/Vol. 36/No. 3
Table 5.
Results: Means and (Standard Deviations) by PAL Trial Groups and Age at Study
PO Days to
PAL Trials by Gestational Age Gavage Days Discharge Discharge Weight Weight Gain
32 Weeks AGA
Control (n = 8) 33.25* 6.63 2.1974 k 0.8025 k
(8.50) (3.74) (0.4086) (0.2523)
1 PAL trial (n = 8) 46.75 5.13 2.2759 k 1.0193 k
(17.33) (2.36) (0.5998) (0.5920)
3 PAL trials (n = 8) 48.50 6.00 2.4533 k 1.1829 k
(15.89) (3.59) (0.5670) (0.5033)
34 Weeks AGA
Control (n = 8) 58.88 10.25 2.5100 k 1.4233 k
(13.10) (12.19) (0.3962) (0.4772)
1 PAL trial (n = 8) 46.88* 3.88 2.2816 k 1.0340 k
(14.67) (2.75) (0.3636) (0.4245)
3 PAL trials (n = 6) 35.17* 4.17 2.1808 k 0.7597 k
(8.40) (1.83) (0.1776) (0.3073)
36 Weeks AGA #
Control (n = 7) 67.71 6.711 2.2514 k 1.3487 k
(13.39) (3.90) (0.4853) (0.4518)
1 PAL trial (n = 8) 68.88 6.50 2.2426 k 1.3049 k
(25.34) (2.45) (0.2831) (0.3100)
3 PAL trials (n = 7) 64.71 7.86 2.6280 k 1.5097 k*
(21.48) (3.53) (0.6168) (0.6055)
Notes: N = 68.
*p < 0.05, significantly different within age group, PAL trials significantly shortened length of gavage feeding for 34-week babies, and
3 trials were significantly better than 1 trial. PAL trials significantly increased length of gavage feeding for 32-week babies.
# p < 0.05, significantly different across age groups, all 36-week AGA infants were gavage fed significantly longer than the other two
groups. Overall, 36-week AGA infants gained significantly more weight than the other age groups.
df = 3, 60, p = 0.004). Overall, data significant (F = 2.758, df = 4, p = number of PAL trials affected benefits.
showed little difference among vari- 0.036). No other comparisons were PAL trials significantly shortened
ables by site, and gender was equal- significant. length of gavage feeding for 34-week
ized in the random assignment Analysis of total weight gain from babies, and three trials were signifi-
among groups; therefore, it was birth to discharge was significant for cantly better than one trial. PAL trials
assumed these groupings did not age at study (F = 4.629, df = 2, p = significantly increased length of gav-
affect overall results of PAL trials, and 0.014). Tukey HSD post hoc analysis age feeding for 32-week babies. These
data were pooled for further analyses. showed that the 36-week AGA infants results would indicate that the PAL is
Results for each of the four gained significantly more weight than most effective when introduced at 34
dependent variables were subjected to the other two age groups, but this was gestational weeks, the point in time
Two-Way Analyses of Variance for expected because they were born when most infants are deemed neuro-
comparison by age at study and num- smaller and stayed in the hospital logically ready to nipple feed (McGrath
ber of PAL trials. Table 5 shows means, longer. & Braescu, 2004).
standard deviations, and significance Analysis of weight gain for age at The sample was very small in the
comparisons among means using study by PAL trials was significant (F = 36-week age group receiving three PAL
Tukey post hoc analysis. 2.739, df = 4, p = 0.037). Tukey HSD post trials due to the rarity of infants meet-
Analysis of gavage feeding days hoc analysis showed no significance for ing criteria for continued inclusion in
showed significance for age at study specific age by trial comparisons. the study. Specifically, most infants
(F = 14.137, df = 2, p = 0.0001). Tukey enrolled at 36 weeks who were not nip-
HSD post hoc analysis showed that all ple feeding began to do so after one
36-week AGA infants took significant- Discussion PAL trial. Therefore, it was impossible
ly longer to oral feed than the 32 or to fulfill the planned cohort for the 36-
34-week infants, and three PAL trials The purpose of this study was to week, three-trial group. This age group
shortened the interval, but not signif- ascertain whether the PAL benefitted deserves further study with a design
icantly so. Analysis of gavage feeding infant transition from gavage to nipple that does not require multiple PAL tri-
days for age at study by trials was also feeding, and if age of presentation or als at this gestational age.
PEDIATRIC NURSING/May-June 2010/Vol. 36/No. 3 143
The Effect of Music Reinforcement for Non-Nutritive Sucking on Nipple Feeding of Premature Infants
Overall, the results of this PAL pro- presentation and multiple trials had non-crying, preterm neonates. Research in
Nursing and Health, 1(2), 69-75.
tocol by age at study and trials do not never been attempted. This protocol Caine, J. (1992). The effects of music on the selected
demonstrate significant weight gain proved effective in significantly short- stress behaviors, weight, caloric and formula
benefits except those related to longer ening gavage days for 34-week AGA intake, and length of hospital stay of premature
stay in the hospital. Similar to findings infants. Future research must be exact and low birth weight neonates in a newborn
intensive care unit. Journal of Music Therapy,
by Cevasco and Grant (2005), there are in assessing and comparing specific 28(4), 180-192.
trends that may warrant future protocol parameters to improve care Cassidy, J., & Ditty, K. (2001). Gender differences
research with revised protocols and procedures. Much more research in among newborns on a transient otoacoustic
design. Cevasco and Grant (2005) this area is warranted. emissions test for hearing. Journal of Music
Therapy, 38(1), 28-35.
showed increasing weight gain with Cassidy, J., & Standley, J. (1995). The effect of music
increasing age and increasing PAL listening on physiological responses of prema-
usage; however, this study demonstrat- Clinical Implications ture infants in the NICU. Journal of Music
ed such results in the 36-age group Therapy, 37(4), 208-227.
A PAL intervention can significant- Cevasco, A., & Grant, R. (2005). Effect of the pacifier
only. This studys results for weight ly shorten gavage feeding days and activated lullaby on weight gain of premature
gain by age may be primarily due to length of hospitalization for premature infants. Journal of Music Therapy, 42(2), 123-
36-week infants longer stay in the infants when used at the specific gesta- 139.
NICU associated with necessity for tion age of 34 weeks. The intervention
Chapman, J.S. (1979). Influence of varied stimuli on
development of motor patterns in the prema-
completion of three trials prior to dis- protocol should begin with a PAL treat- ture infant. In G. Anderson & B. Raff (Eds.),
charge. ment of 15 minutes approximately 30 Newborn behavioral organization: Nursing
It should be noted that there were minutes prior to a feeding trial and research and implications (pp. 61-80). New
several confounding factors in this should continue daily until the infant
York: Alan Liss.
Cheour-Luhtanen, M., Alho, K., Sainio, K., Rinne, T.,
study. Every infant from whom con- is independently nipple feeding. The Reinikainen, K., Pohjavuouri, M., ... Naatanen,
sent was received and who was ran- lullaby selected for reinforcement of R. (1996). The ontogenetically earliest discrimi-
domly assigned to the 32 to 33-week sucking should be in the native lan- native response of the human brain.
age group completed participation in Psychophysiology, 33, 478-481.
guage of the infants family if possible. Cignacco, E., Hamers, J., Stoffel, L., van Lingen, R.,
the project. However, some assigned to In this way, the infant will be receiving Gessler, P., McDougall, J., & Nelle, M. (2007).
the 34 to 35-week age group and many critical language input while being The efficacy of non-pharmacological interven-
more assigned to the 36 to 37- week reinforced for sucking. The protocol tions in the management of procedural pain in
age group graduated and failed to used in this study is recommended.
preterm and term neonates. A systematic liter-
ature review. European Journal of Pain, 11(2),
complete the study because they began 139-152.
nipple feeding or were discharged Criteria for Referral DiPietro, J., Cusson, R., Caughy, M., & Fox, N. (1994).
before conclusion of trials. Infant is determined to be able to Behavioral and physiologic effects of nonnutri-
Independent feeding is one main crite- tolerate two simultaneous modes
tive sucking during gavage feeding in pre-term
infants. Pediatric Research, 36(2), 207-214.
rion for discharge, and infants who of stimulation (pacifier and audi- Field, T., Hernandez-Reif, M., Feijo, L., & Freedman,J.
began to feed well were immediately tory stimulation). (2006). Prenatal, perinatal and neonatal stimu-
sent home. Since the research design Infant has no severe abnormali- lation: A survey of neonatal nurseries. Infant
required that some infants at 34 or 36 Behavior and Development, 29(1), 24-31.
ties that affect ability to suck/feed Field, T., Ignatoff, E., Stringer, S., Brennan, J.,
weeks AGA still need gavage feeding or to learn, including abnormali- Greenberg, R., Widmayer, S., & Anderson, G.
throughout three PAL trials across 3 to ties of the oral cavity, hydro- (1982). Nonnutritive sucking during tube feed-
5 days, a bias for length of stay was cre- cephalus, Down syndrome, signif- ings: Effects on preterm neonates in an inten-
ated for the two older groups. Some sive care unit. Pediatrics, 70(3), 381-384.
icant neurological disorders (PVL, Gardner, S.L., Garland, K.R., Merenstein,S. L., &
participants excelled at acquiring nip- IVH, HIE). Lubchenco, L.O. (1997). The neonate and the
ple feeding skills and left before com- Infant has no indication of infec- environment Impact on development. In G.B.
pleting the research trials. tion requiring quarantine. Merenstein & S.L. Gardner (Eds.). Handbook of
The PAL shows some potential for neonatal intensive care (4th ed.) (pp. 564-608).
Infant is not on ventilator or St. Louis, MO: Mosby.
facilitating nipple feeding, and contin- CPAP. Gill, N., Behnke, M., Conlon, M., NcNeely, J., &
ued research is warranted to further Infant is ready to begin some OG Anderson, G. (1988). Effect of nonnutritive
refine the PAL intervention protocols. feeds. sucking on behavioral state in preterm infants
Nipple feeding is necessary for dis- before feeding. Nursing Research, 37(6), 347-
350.
charge. Infants begin training at 34 Goff, D.M. (1985). The effects of nonnutritive sucking
weeks AGA, and a few succeed imme- References on state regulation in pre-term infants.
diately. However, very low birth Anderson, G., & Vidyasagar, D. (1979). Development Dissertation Abstracts International, 46(8-B),
weight infants and those intubated for of sucking in premature infants from 1 to 7 days 2835.
longer periods have great difficulty post birth. Birth Defects: Original Article Series, Gomes-Pedro, J., Patricio, M., Carvalho, A.,
15(7), 145-171. Goldschmidt, T., Torgal-Garcia, F., & Monteiro,
with this task. Many infants remain Bernbaum, J., Pereira, G., Watkins, J., & Peckham, G. M. (1995). Early intervention with Portuguese
hospitalized solely due to inability to (1983). Nonnutritive sucking during gavage mothers: A 2-year follow-up. Journal of
oral feed. At a U.S. average NICU cost feeding enhances growth and maturation in Developmental and Behavioral Pediatrics,
premature infants. Pediatrics, 71(1), 41-45. 16(1), 21-28.
of approximately $2000/day, this can Harrison, L. (1985). Effects of early supplemental
Boyle, E., Freer, Y., Khan-Orakzai, A., Watkinson, M.,
be an expensive and depressing period Wright, E., Ainsworth, J., & McIntosh, N. (2006). stimulation programs for premature infants:
for the family awaiting discharge Sucrose and non-nutritive sucking for the relief Review of the literature. Maternal-Child Nursing
(Standley, 2003a). Interventions that of pain in screening for retinopathy: A ran- Journal, 14(2), 69-90.
can speed up this process without domised controlled trial. Archives in Disease in Hill, A. (1992). Preliminary findings: A maximum oral
Childhood: Fetal and Neonatal Edition, 91(3), feeding time for premature infants, the relation-
physiologic harm to the infant are 166-168. ship to physiological indicators. Maternal-Child
highly desired. In prior research, one Britt, G., & Myers, B. (1994). The effects of Brazelton Nursing Journal, 20(2), 81-92.
PAL intervention proved to be highly intervention: A review. Infant Mental Health, Kanarek, K., & Shulman, D. (1992). Non-nutritive
effective in increasing sucking rate and 15(3), 278-292. sucking does not increase blood levels of gas-
Burroughs, A., Asonye, U., Anderson-Shanklin, G., & trin, motilin, insulin and insulin-like growth factor
subsequent feeding rate. However, a Vidyasagar, D. (1978). The effect of nonnutritive 1 in premature infants receiving enteral feed-
specific PAL protocol testing age of sucking on transcutaneous oxygen tension in ings. Acta Paediatrica Scandinavica, 81, 974-
977.
144 PEDIATRIC NURSING/May-June 2010/Vol. 36/No. 3
Lecanuet, J., Granier-Deferre, C., & Busnel, M. Palmer, M.M. (1993). Identification and management Standley, J. (1998). The effect of music and multi-
(1995). Human fetal auditory perception. In J.P. of the transitional suck pattern in premature modal stimulation on physiologic and develop-
Lecanuet, W.P. Fifer, N.A. Krasnegor, & W.P. infants. Journal of Perinatal and Neonatal mental responses of premature infants in
Smotherman, (Eds.), Fetal development: A psy- Nursing, 7(1), 66-75. neonatal intensive care. Pediatric Nursing,
chobiological perspective (pp. 239-262). Pinelli, J., & Symington, A. (2000). How rewarding can 24(6), 532-538.
Hillsdale, NJ: Lawrence Erlbaum Associates. a pacifier be? A systematic review of non-nutri- Standley, J. (2000). The effect of contingent music to
Mathai, S. Natrajan, N., & Rjalakshmi, N. (2006). A tive sucking in pre-term infants. Neonatal increase non-nutritive sucking of premature
comparative study of nonpharmacological Network, 19(8), 4-8. infants. Pediatric Nursing, 26(5), 493-499.
methods to reduce pain in neonates. Indian Pinelli, J., & Symington, A. (2005). Non-nutritive suck- Standley, J. (2002). A meta-analysis of the efficacy of
Pediatrics, 43(12), 1070-1075. ing for promoting physiologic stability and nutri- music therapy for premature infants. Journal of
McCain, G. (1992). Facilitating inactive awake states tion in pre-term infants. Cochrane Database of Pediatric Nursing, 17(2), 107-113.
in pre-term infants: A study of three interven- Systematic Reviews, 2005(4): CD001071. Standley, J. (2003a). Music therapy with premature
tions. Nursing Research, 41(3), 157-160. Rauh, V., Nurcombe, B., Achenbach, T., & Howell, C. infants: Research and developmental interven-
McCain, G. (1995). Promotion of pre-term infant nip- (1987). The mother-infant transaction program: tions. Silver Spring, MD: American Music
ple feeding with non-nutritive sucking. Journal An intervention for the mothers of low-birth- Therapy Association.
of Pediatric Nursing, 10(1), 3-8. weight infants. In N. Gunzenhauser (Ed.), Infant Standley, J. (2003b). The effect of music-reinforced
McGrath, J., & Braescu, A. (2004). State of the sci- stimulation: For whom, what kind, when, and non-nutritive sucking on feeding rate of prema-
ence: Feeding readiness in the preterm infant. how much? Skillman, NJ: Johnson & Johnson ture infants. Journal of Pediatric Nursing, 18(3),
Journal of Perinatal & Neonatal Nursing, 18(4), Baby Products. 169-173.
353-368. Schwartz, R., Moody, L., Yarndi, H., & Anderson, G. Standley, J., & Moore, R. (1995). Therapeutic effects
Medoff-Cooper, B., & Gennaro, S. (1996). The corre- (1987). A meta-analysis of critical outcome vari- of music and mothers voice on premature
lation of sucking behaviors and Bayley Sclaes ables in non-nutritive sucking in pre-term infants. Pediatric Nursing, 21(6), 509-512, 574.
of Infant Development at six months of age in infants. Nursing Research, 36(5), 292-295. Whipple, J. (2008). The effect of music-reinforced non-
VLBW infants. Nursing Research, 45(5), 291- South, M., Strauss, R., South, Al. Boggess, J., & nutritive sucking on state of preterm, low birth-
296. Thorp, J. (2005). The use of non-nutritive suck- weight infants experiencing heelstick. Journal of
Oehler, J. (1993). Developmental care of low birth ing to decrease the physiologic pain response Music Therapy, 45(3), 227-272.
weight infants. Advances in Clinical Nursing during neonatal circumcision: A randomized Woodson, R., & Hamilton, C. (1988). The effect of
Research, 28(2), 289-301. controlled trial. American Journal of Obstetrics nonnutritive sucking on heart rate in preterm
and Gynecology, 193(2), 537-542. infants. Developmental Psychobiology, 21(3),
207-213.
PEDIATRIC NURSING/May-June 2010/Vol. 36/No. 3 145
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hazen Williams EquationDocument5 pagesHazen Williams Equationprabhjot123100% (1)
- 2014 Annual Report GeneaDocument120 pages2014 Annual Report GeneaPeterDavidNo ratings yet
- Pathophysiology NSAID Induced UGIB Gouty Arthritis and Gouty NephropathyDocument2 pagesPathophysiology NSAID Induced UGIB Gouty Arthritis and Gouty NephropathyghellersNo ratings yet
- Repro MindmapDocument3 pagesRepro MindmapghellersNo ratings yet
- Nursing Diagnosis Fvd2Document2 pagesNursing Diagnosis Fvd2ghellersNo ratings yet
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)ghellersNo ratings yet
- Erik Eriksons Psycho Social Development TheoryDocument23 pagesErik Eriksons Psycho Social Development TheoryRaven Dave AtienzaNo ratings yet
- MCST Stimuli-CompressedDocument10 pagesMCST Stimuli-Compressedapi-470437967No ratings yet
- El TB 04Document2 pagesEl TB 04Fayyaz NadeemNo ratings yet
- API BGD DS2 en Excel v2 4685979Document339 pagesAPI BGD DS2 en Excel v2 4685979Areesha KamranNo ratings yet
- Igcse: Definitions & Concepts of ElectricityDocument4 pagesIgcse: Definitions & Concepts of ElectricityMusdq ChowdhuryNo ratings yet
- A Shew Recipe Costing XLSX 2Document2 pagesA Shew Recipe Costing XLSX 2api-242204869No ratings yet
- Grade 10 Lesson 3 Earthquake Seismic WaveDocument34 pagesGrade 10 Lesson 3 Earthquake Seismic Wavemae ann perochoNo ratings yet
- PN NCLEX Integrated A 1Document75 pagesPN NCLEX Integrated A 1jedisay1100% (1)
- Idioms With Hindi 1Document32 pagesIdioms With Hindi 1yqwe1093100% (1)
- Playbook Launchpackage Cassida Chain Oil XteDocument11 pagesPlaybook Launchpackage Cassida Chain Oil XteKiệt NgôNo ratings yet
- Hindu Code Bill Hindu Law Research PaperDocument4 pagesHindu Code Bill Hindu Law Research Paperputt jatt daNo ratings yet
- Grade 6 DLL Science 6 q3 Week 1Document5 pagesGrade 6 DLL Science 6 q3 Week 1MICHELE PEREZNo ratings yet
- Model No: ATBOX-G3-J4125: Product HighlightDocument2 pagesModel No: ATBOX-G3-J4125: Product HighlightTamNo ratings yet
- THW1.soft Drinks vCOMPLETEDocument2 pagesTHW1.soft Drinks vCOMPLETEjunho yoonNo ratings yet
- Write Up of Salt Analysis NH CL: Acidic Radical (Order Will BeDocument4 pagesWrite Up of Salt Analysis NH CL: Acidic Radical (Order Will BeRoshan AnsariNo ratings yet
- Amador D. Sandoval: Personal InformationDocument4 pagesAmador D. Sandoval: Personal InformationJohn Dela CruzNo ratings yet
- ΑΝΤΙΔΡΑΣΤΗΡΙΑ PDFDocument1 pageΑΝΤΙΔΡΑΣΤΗΡΙΑ PDFk_168911826No ratings yet
- Comparison ASTM A 3388 & ISO 11496Document1 pageComparison ASTM A 3388 & ISO 11496Rahul MoottolikandyNo ratings yet
- HMT SeminarDocument4 pagesHMT SeminarBhavesh JainNo ratings yet
- TissuesDocument49 pagesTissuessunnysinghkaswaNo ratings yet
- Sub-Compact Tractors: CT1021 CT1025Document16 pagesSub-Compact Tractors: CT1021 CT1025Abhinandan PadhaNo ratings yet
- Mental Health TheoriesDocument6 pagesMental Health TheoriesRodzel Oñate BañagaNo ratings yet
- Compiled 84 Halaman TropmedDocument78 pagesCompiled 84 Halaman TropmedDapot SianiparNo ratings yet
- The Development of AgricultureDocument6 pagesThe Development of AgricultureKaterin ZapataNo ratings yet
- MELCs SCIENCEDocument26 pagesMELCs SCIENCEArquero NosjayNo ratings yet
- Drug Dependency Examination (DDE)Document38 pagesDrug Dependency Examination (DDE)Ace VisualsNo ratings yet
- Password Based Circuit Breaker Control To Ensure Electric Line Mans Safety and Load Sharing IJERTCONV5IS13135Document4 pagesPassword Based Circuit Breaker Control To Ensure Electric Line Mans Safety and Load Sharing IJERTCONV5IS13135Pratiksha SankapalNo ratings yet
- Sexual Orientation: Gender, Transgender, and ConformanceDocument4 pagesSexual Orientation: Gender, Transgender, and ConformanceMaria GiannisiNo ratings yet