Professional Documents
Culture Documents
Out 11 PDF
Out 11 PDF
Uploaded by
ancoursOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Out 11 PDF
Out 11 PDF
Uploaded by
ancoursCopyright:
Available Formats
Combined Diet and Exercise Intervention in
the Workplace
Effect on Cardiovascular Disease Risk Factors
by Karen White, MS, RD, LDN, and Paul H. Jacques, PhD
research Abstract
This study assessed the effectiveness of a 12-week pilot employee wellness program in reducing risk factors for coronary
heart disease. Fifty university employees with at least one cardiovascular disease risk factor participated in the program.
Interventions focused on diet, exercise, and monthly workshops. Pre- and post-intervention measurements included
weight, body composition, blood pressure, total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipo-
protein (HDL) cholesterol, total cholesterol/HDL cholesterol ratio, triglycerides, and blood sugar. Twenty-five employees
had post-intervention measurements. A survey was administered to assess adherence. The correlation between adher-
ence and improvement in cardiovascular disease risk factors was also tested. Significant differences were observed
between pre- and post-intervention measurements of total cholesterol, LDL cholesterol, total cholesterol/HDL cholesterol
ratio, triglycerides, and weight. A significant correlation existed between self-reported level of participation in the diet
aspect of the program and improvement in LDL levels. This multi-component, 12-week pilot employee wellness program
was effective in reducing cardiovascular disease risk.
N
early two-thirds of all deaths among adults in and Treatment of High Blood Cholesterol in Adults, 2001;
the United States are attributed to coronary heart National Institutes of Health, 1998; U.S. Department of
disease, cancer, stroke, and diabetes (Centers for Agriculture and U.S. Department of Health & Human Ser-
Disease Control and Prevention, 2005). Diet contributes vices, 1992, 1995; U.S. Department of Health & Human
to the development of all four (Byers et al., 2002; Grun- Services, 2000; World Health Organization, 1998; World
dy, Pasternak, Greenland, Smith, & Fuster, 1999; Hubert, Health Organization Expert Committee, 1995). In June
Feinleib, McNamara, & Castelli, 1983; Krauss et al., 2004, the American Heart Association (AHA), American
2000; Seidell, 2000; Sherwin et al., 2004; Tuomilehto et Diabetes Association (ADA), and American Cancer Soci-
al., 2001). When stroke, hypertension, and coronary heart ety (ACS) published a joint scientific statement including
disease are included in the definition of cardiovascular recommendations for treating diabetes, cancer, and heart
disease (CVD), CVD accounts for more than one-third of disease (Eyre, Kahn, & Robertson, 2004). The recom-
the deaths among American adults (Hoyert, Heron, Mur- mendations focused on four areas: diet, exercise, cigarette
phy, & Kung, 2006). smoking, and health screenings.
To improve the health of the nation and reduce mortal- Worksite health promotion programs are an effi-
ity from these diseases, the U.S. government and several cient means of improving the health of a relatively large
government agencies have published recommendations or group of individuals (Anderson, Palombo, & Earl, 1998).
guidelines regarding dietary choices, weight, and physical Worksite interventions are convenient and accessible for
activity (Fletcher et al., 1996; Joint National Committee workers and often less expensive than programs offered
on Prevention, Detection, Evaluation, and Treatment of in clinical settings (Glantz & Seewald-Klein, 1986; Pelle-
High Blood Pressure, 2004; National Cholesterol Educa- tier, 1996; Sorensen & Himmelstein, 1992). Furthermore,
tion Program Expert Panel on the Detection, Evaluation, employers who pay for health insurance have a vested in-
terest in maintaining the cardiovascular wellness of their
About the Authors employees (Guico-Pabia, Murray, Teutsch, Wertheimer,
Ms. White is a dietitian, Bird Health Center, Western Carolina University,
Cullowhee, NC. Dr. Jacques is Assistant Professor of Management, West- & Berger, 2001).
ern Carolina University, Cullowhee, NC. Many employers have developed and assessed work-
march 2007, vol. 55, no. 3 109
Applying Research to Practice Recommended Ranges
Blood pressure < 120/< 80 mmHg
A wellness program of relatively short dura-
tion focusing on diet, exercise, laboratory and Total cholesterol < 200 mg/dl
anthropometric measures, and regular educa- LDL cholesterol < 100 mg/dl
tional workshops can be effective in reducing
cardiovascular disease (CVD) risk. If such Triglycerides < 150 mg/dl
improvements in CVD risk can be maintained, Fasting blood sugar < 100 mg/dl
a substantial cost-savings can be realized by
employers supporting such programs. BMI < 25
LDL = low-density lipoprotein; BMI = body mass index.
site wellness programs including both diet and exercise to
reduce CVD risk factors. The National Aeronautics and tion of the program required minimal staff, time, and
Space Administration (NASA) offered an 8-week diet and resources.
exercise intervention program, the Cardiovascular Risk
Reduction Program, to employees annually for 10 con- Methods
secutive years. The mean beginning total serum choles- Subjects
terol levels of the participants were significantly reduced Participants at a mid-sized regional comprehensive
each year (Angotti, Chan, Sample, & Levine, 2000). university were recruited via university e-mail advertis-
Another workplace health promotion program tar- ing the program. Fifty university staff and faculty with
geting diet and exercise to reduce CVD risk took a dif- at least one baseline measurement outside of the rec-
ferent approach. The 152 employees in the intervention ommended range (Sidebar) participated in the program.
group spent 4 days at a resort for intensive lectures and Forty-two of the 50 participants were female. The well-
training. The participants were assessed at baseline and ness program lasted 3 months. Employees were asked
at 3-month intervals for 1 year after the program. Those to complete surveys related to the program and submit
in the intervention group showed significant improve- logs of daily food servings and minutes of exercise. Pre-
ments in body mass index (BMI), systolic blood pres- and post-intervention measurements included BMI, body
sure, total cholesterol, and triglycerides (Muto & Yam- composition, blood pressure, total cholesterol, LDL cho-
auchi, 2001). lesterol, high-density lipoprotein (HDL) cholesterol, to-
A third study compared the effect of diet and exer- tal cholesterol/HDL cholesterol ratio, triglycerides, and
cise on CVD risks. The low-fat diet intervention group blood sugar. In addition, a post-intervention survey was
showed the greatest improvement in total cholesterol, administered 13 weeks after the pre-intervention mea-
low-density lipoprotein (LDL) cholesterol, and body surements were taken to assess adherence to different
weight (Pritchard, Nowson, Billington, & Wark, 2002). components of the intervention.
One hundred sixty-seven employees identified as Twenty-five of the participants who began the pro-
high risk were enrolled in the Lucent-Takes-Heart car- gram had post-intervention measurements (5 male, 20
diovascular health management program. The interven- female). Because only eight participants returned logs,
tion included education, measurement of risk factors, and these data were not included in the analysis. A follow-up
individual counseling. At the 6-month follow-up, most inquiry directed at participants who did not complete the
participants reported increasing exercise or changing program revealed work schedules that grew increasingly
diet. The participants total cholesterol, LDL cholesterol, demanding as the semester progressed and reduced dis-
and blood pressure were significantly improved (Guico- cretionary time available for participation were the pre-
Pabia, Cioffi, & Shoner, 2002). dominate barriers.
A 3-month intervention for overweight individuals
consisted of a baseline survey, two counseling sessions, Interventions
and four individualized letters. Assessment measures in- Interventions associated with the wellness program
cluded a food frequency questionnaire and a 3-day food focused on dietary changes, following one of four ex-
record. At the end of the intervention, participants had ercise prescriptions, and participating in a minimum of
significantly reduced their body weight and total choles- four workshops in 3 months. The interventions were
terol (Okuda, Okamura, Kadowaki, Tanaka, & Ueshima, collectively referred to as the Healthy Cats pilot well-
2004). ness program. The AHA, ADA, and ACS jointly rec-
No worksite wellness programs have been devel- ommend weight loss to achieve and maintain a healthy
oped based on the new joint AHA, ADA, ACS recom- weight, and physical activity for at least 30 minutes 5 or
mendations. This study aimed to determine the efficacy more days each week. The Healthy Cats physical activ-
of a 12-week worksite wellness program based on these ity recommendations included four prescriptions based
recommendations for reducing CVD risk. Implementa- on baseline activity level. At the end of 12 weeks, each
110 AAOHN Journal
participant was to engage in physical activity for 30 Measures
minutes 6 days each week. Risk factors related to this study were measured us-
The AHA, ADA, and ACS (2004) jointly advise con- ing standard health care industry techniques. All partici-
suming at least five servings of fruits and vegetables daily, pants were given written instructions to fast for at least
choosing whole grains over processed or refined grains 12 hours prior to both the pretest and the posttest proto-
and sugars, substituting healthier fats for trans and satu- col. Fasting was defined as no caloric intake for at least
rated fats, monitoring portion sizes, and choosing foods 12 hours. Individuals obtaining the measurements were
to maintain a healthy weight. The Healthy Cats diet plan trained to use necessary equipment. Blood pressure was
was adapted from recommendations in the joint statement measured with a Welch Allyn Vital Signs Monitor (Welch
(Eyre et al., 2004), Dietary Guidelines for Americans (U.S. Allyn, Beaverton, OR). Weight and body composition
Department of Agriculture and U.S. Department of Health were determined with the Tanita BF-350 Body Composi-
& Human Services, 1995), the food pyramid (U.S. Depart- tion Analyzer Scale (Tanita Corporation of America, Inc.,
ment of Agriculture and U.S. Department of Health & Hu- Arlington Heights, IL), which measures the impedance,
man Services, 1992), and the Dietary Approaches to Stop or resistance, of a small electrical current passing through
Hypertension eating plan (Joint National Committee on the body. The higher an individuals body fat percentage,
Prevention, Detection, Evaluation, and Treatment of High the greater the resistance. Each participants age, gender,
Blood Pressure, 2004; National Institutes of Health, 1998; and height were entered into the body composition ana-
U.S. Department of Health & Human Services, 2000). lyzer, which uses electrodes in each foot pad to send a
The joint initiative recommends blood pressure, BMI, small electrical current throughout the body. Participants
cholesterol, and blood glucose screening; clinical breast removed their shoes and socks before stepping on the
examination and mammography; and cervical, colon, and analyzer, which was cleaned with a disinfectant wipe be-
prostate cancer screenings. This mid-sized regional com- tween participants.
prehensive university offers an employee health screening BMI was calculated in accordance with procedures
every semester that includes blood pressure, BMI, body defined by the National Institutes of Health (1998). BMI
composition, lipid profile, and fasting blood glucose. The is recommended when assessing overweight and obesity.
joint initiative also recommends smoking cessation, but All plasma assessments used in this study (blood
because none of the participants smoked, this was not a glucose, total cholesterol, LDL cholesterol, HDL choles-
focus of the intervention. terol, and triglycerides) were by a laboratory certified by
Hour-long workshops were scheduled at varying the College of American Pathologists. The laboratory fol-
times to accommodate participants schedules. All par- lows the standards developed by the Clinical and Labora-
ticipants attended a 1-hour program overview session of- tory Standards Institute (2006), an independent nonprofit
fered twice to promote attendance. The remaining work- organization developing and promoting the use of its
shops were designed following an interest assessment. laboratory methods standards. The total cholesterol/HDL
The most popular workshops were offered multiple times cholesterol ratio was calculated using the method defined
so more participants could attend. Nineteen workshops by Kannel and Wilson (1992), whereby total cholesterol
were offered during the Healthy Cats program covering is divided by HDL cholesterol. Assessments of normal
the following 10 topics: quick and healthy meals; stress blood (plasma) glucose and levels diagnostic of diabe-
and eating; yoga, stretching, and Pilates; exercise over- tes mellitus followed guidelines from the ADA (2006).
view; emerging trends in diabetes management; healthy The Joint National Committee on Prevention, Detection,
snack foods; surviving special occasions; the food and Evaluation, and Treatment of High Blood Pressure (2004)
mood connection; grocery shopping; and family and diet- defines optimal blood pressure as a systolic blood pres-
ing. The most popular workshops were quick and healthy sure of 120 mmHg or less and a diastolic blood pressure
meals, exercise overview, surviving special occasions, the of 80 mmHg or less.
food and mood connection, and grocery shopping. The The degree to which participants followed the well-
facilitator at each workshop provided a handout and ei- ness program was measured by their responses to two
ther discussed the topic and answered questions or dem- survey items: I adhered to the Healthy Cats diet pro-
onstrated and led exercise sessions. gram and I adhered to the Healthy Cats exercise pro-
Participants received a notebook containing a meal gram. Participants responded to each item separately
plan, a week of sample menus, recipes, an individualized using a 5-point Likert scale ranging from strongly dis-
exercise program, a log to record food intake and physical agree to strongly agree. Scores for these two items
activity, and literature about resources related to physical were averaged, thereby resulting in an indication of the
activity on campus. They received discounts for aerobics participants overall adherence to the program.
classes offered on campus.
Overall, the wellness program was based on the Statistical Analysis
motivational principles studied by Horowitz (1985) and Paired two-sample t tests for means were used to
Fleury (1993), wherein participants in wellness programs compare pre- and post-intervention measurements for the
are motivated to achieve positive results via personal 25 participants who had both measurements. In addition,
awareness, thought activation, self-reinforcement, social a post-intervention survey was administered to assess
support or social feedback, and shifting their perspectives adherence with various components of the intervention.
toward an internal locus of control. The correlation between adherence with various program
march 2007, vol. 55, no. 3 111
Table 1
Significant Findings Associated With Cardiovascular Disease Risk Factors
Total LDL Total/HDL
Cholesterol Cholesterol Cholesterol Triglycerides Weight
(mg/dl) (mg/dl) (mg/dl) (mg/dl) (pounds)
50 participants pretest
Mean pretest 207 124 3.64 170 179.7
Range pretest 150 169 3.70 808 229.4
Median pretest 216 134 3.47 135 183
SD pretest 33.24 32.82 0.87 133 37.68
25 participants pretest
Mean pretest 201 118 3.41 160 176.4
Range pretest 128 169 3.70 808 120
Median pretest 202 123 3.20 104 177
SD pretest 35.42 37.49 0.95 173 31.6
Mean posttest 179* 103 3.11 132 173.3
Range posttest 141 138 3.70 558 114
Median posttest 178 107 3.07 99 176.7
SD posttest 31.03 31.69 0.82 112 28.2
LDL = low-density lipoprotein; HDL = high-density lipoprotein.
Note. Groups of 25 participants portrayed in this table reflect those who completed the program and had valid pretest and post-
test results. All reports of significance are based on tests of paired comparisons of participants pretest and posttest results.
*p < .001.
p < .01.
p < .05.
components and improvement in CVD risk factors was for 20 of them, whereas posttest levels were higher for
also tested via simple linear regression techniques (Co- 5. At the start of the program, only 23% of participants
hen & Cohen, 1983). had optimal LDL cholesterol levels (< 100 mg/dl); by the
end of the program, 32% of those re-tested had optimal
Results LDL cholesterol levels. Despite the drastic reduction in
Significant differences were observed between pre- total and LDL cholesterol levels, HDL cholesterol levels
and post-intervention measurements of total cholesterol remained essentially unchanged, leading to a significant
(p < .001), LDL cholesterol (p = .002), total cholesterol/ improvement in the total cholesterol/HDL cholesterol ra-
HDL cholesterol ratio (p = .015), triglycerides (p = .036), tio. At the start of the program, only 60% of participants
and weight (p = .01). In addition, a significant correlation had normal triglyceride levels (< 150 mg/dl) as defined
was found between self-reported level of participation in by the National Cholesterol Education Program (2001).
the diet aspect of the program and change in LDL levels However, 88% of those re-tested at the conclusion of the
(p = .018). Tables 1 and 2 display pre- and post-interven- program had normal triglyceride levels.
tion measurements. Twenty-six participants were weighed at the end of
The most noticeable improvements included a de- the program. They had lost 80 pounds combined, or an
crease in total cholesterol levels from 202 to 179 mg/dl. average of 3.2 pounds each. Sixty-two percent of those
This 23-point drop is clinically significant and correlates completing the program lost weight, for a total of 102
with significant reduction in CVD risk. Only 36.7% of pounds, or an average of 6.4 pounds each. Nine of the 25
participants had desirable cholesterol levels (< 200 mg/dl) participants who completed the program gained weight.
at the start of the program, but 72% of those re-tested had Those who gained weight gained an average of 2.2 pounds
desirable total cholesterol levels. Twelve (48%) of the 25 (range, 0.4 to 5 pounds).
participants who completed the program had normal cho- The baseline mean blood glucose level was normal
lesterol levels (total cholesterol < 200 mg/dl) at the outset. at 87 mg/dl. Systolic blood pressure and diastolic blood
A comparison of pretest cholesterol levels with posttest pressure were also normal at 122 and 79.2 mmHg, re-
levels of these 25 showed that total cholesterol dropped spectively. Statistically significant improvements were
112 AAOHN Journal
Table 2
Nonsignificant Findings Associated With Cardiovascular Disease Risk Factors
Systolic Diastolic
Blood Blood HDL
Pressure Pressure Cholesterol Blood Sugar
Body Fat (%) (mmHg) (mmHg) (mg/dl) (mg/dl)
50 participants pretest
Mean pretest 36.16 128 83 49 87.24
Range pretest 36.20 59 44 47 143
Median pretest 35.60 127 83 46 81
SD pretest 8.49 14.25 10.23 11.16 23.40
25 participants pretest
Mean pretest 36.40 127 82 51 86
Range pretest 27.8 48 41 46 94
Median pretest 38.10 126 82 53 83
SD pretest 9.05 13.12 9.58 12.22 17.69
Mean posttest 36.54 127 81 50 86
Range posttest 35.20 88 33 50 61
Median posttest 38.85 125 79 49 83
SD posttest 10.11 17.41 7.74 13.24 13.33
HDL = high-density lipoprotein.
not seen for blood sugar or blood pressure. Only three gram to initiate behaviors leading to a healthy diet and
participants had abnormal values at the beginning; none exercise.
of them changed to normal values. Despite these limitations, findings were positive and
A correlation existed between participation in the indicate the potential value of continuing this program
diet aspect of the program and change in LDL cholesterol to determine its efficacy with larger groups. Long-term
levels (p < .02). This was the only statistically significant interventions and studies investigating the link between
relationship between program components and objective employee wellness programs and health insurance claims
outcome measurements. are warranted to support expansion of such programs
throughout the United States and in countries with similar
Conclusion health care systems.
Small sample size and low program completion rate Overall, these results suggest the multi-component,
were limitations of this study. Although participants were 12-week pilot employee wellness program was effective
informed of the second testing date several times, many in reducing weight, total cholesterol, LDL cholesterol,
asked for another testing date. These requests suggested total cholesterol/HDL cholesterol ratio, and triglycer-
more than half of the participants completed the program ides. Adherence to the dietary component was linked to
but were not available for re-testing. Despite partici- reduced LDL cholesterol. Others (Anderson et al., 1998;
pants agreeing to the date and time of the posttests at the Glantz & Seewald-Klein, 1986; Pritchard et al., 2002;
programs outset, additional dates for posttest sampling Sorensen & Himmelstein, 1992) have found dietary in-
may have reduced apparent attrition rates. However, cost tervention effective. Of the worksite wellness interven-
constraints precluded adding dates and times for drawing tions mentioned at the beginning of this article, four led
posttest samples. to reductions in total cholesterol, three to reductions in
Lack of a comparison or control group was another LDL cholesterol and weight, and one to improvements
study limitation. Comparing results with those of a con- in cholesterol. Two of the interventions led to reductions
trol group would further strengthen the assumption that in blood pressure. The intervention of the current study
the wellness program was effective in reducing CVD did not, but few of the participants had elevated blood
risk. pressure.
Selection bias may have been a limitation of the Companies employing occupational health nurses
program. Individuals choosing to participate may have could coordinate similar programs. Occupational health
been motivated by factors unrelated to this specific pro- nurses could compile dietary guidelines and exercise pre-
march 2007, vol. 55, no. 3 113
scriptions, assess group interest, and develop workshops. Obesity as an independent risk factor for cardiovascular disease: A
Internal or external laboratories could be used to deter- 26-year follow-up of participants in the Framingham Heart Study.
Circulation, 67(5), 968-977.
mine changes in biological measures. Joint National Committee on Prevention, Detection, Evaluation, and
Treatment of High Blood Pressure. (2004). Seventh report of the
References Joint National Committee on Prevention, Detection, Evaluation,
American Diabetes Association. (2006). Diagnosis and classification of and Treatment of High Blood Pressure (JNC 7; NIH Publication No.
diabetes mellitus. Diabetes Care, 29(Suppl 1), S43-S48. 04-5230). Bethesda, MD: National Institutes of Health.
American Heart Association, American Diabetes Association, & Ameri- Kannel, W. B., & Wilson, P. W. F. (1992). Efficacy of lipid profiles in
can Cancer Society. (2004). Everyday choices for a healthier life. prediction of coronary disease. American Heart Journal, 124(3),
Medical Update, 30(1), 3. 768-774.
Anderson, J. V., Palombo, R. D., & Earl, R. (1998). The role of nutrition Krauss, R. M., Eckel, R. H., Howard, B., Appel, L. J., Daniels, S. R.,
in health promotion and disease prevention programs: Position of Deckelbaum, R., et al. (2000). AHA dietary guidelines: Revision
the American Dietetic Association. Journal of the American Dietetic 2000. A statement for healthcare professionals from the Nutri-
Association, 98(2), 205-208. tion Committee of the American Heart Association. Circulation,
Angotti, C. M., Chan, W. T., Sample, C. J., & Levine, M. S. (2000). 102(18), 2284-2299.
The combined dietary and exercise intervention for control of serum Muto, T., & Yamauchi, K. (2001). Evaluation of a multi-component
cholesterol in the workplace. American Journal of Health Promo- workplace health promotion program in Japan on CVD risk factors.
tion, 25(1), 9-16. Preventive Medicine, 33(6), 571-577.
Byers, T., Nestle, M., McTiernan, A., Doyle, C., Currie-Williams, A., National Cholesterol Education Program (NCEP) Expert Panel on the
Gansler, T., et al. (2002). American Cancer Society guidelines on Detection, Evaluation, and Treatment of High Blood Cholesterol in
nutrition and physical activity for cancer prevention: Reducing the Adults (Adult Treatment Panel III). (2001). Third report of the NCEP
risk of cancer with healthy food choices and physical activity. Amer- expert panel on the detection, evaluation, and treatment of high
ican Cancer Society 2001 Nutrition and Physical Activity Guide- blood cholesterol in adults (Adult Treatment Panel III; NIH Publica-
lines Advisory Committee. CA: A Cancer Journal for Clinicians, tion No. 01-3670). Bethesda, MD: National Institutes of Health.
52(2), 92-119. National Institutes of Health. (1998). Clinical guideline on the identifi-
Centers for Disease Control and Prevention. (2005). National vital cation, evaluation and treatment of overweight and obesity in adults:
statistics reports. Retrieved May 6, 2005, from www.cdc.gov/nchs/ The evidence report. Obesity Research, 6(Suppl 2), 51S-209S.
data/nvsr/nvsr53/nvsr53_15.pdf Okuda, N., Okamura, T., Kadowaki, T., Tanaka, T., & Ueshima, H.
Clinical and Laboratory Standards Institute. (2006). Current versions (2004). Weight-control intervention in overweight subjects at high
of CLSI documents. Retrieved May 22, 2006, from www.clsi.org/ risk of cardiovascular disease: A trial of a public health practical
Source/Custom/Currentdocs.cfm?Section=Current_Versions_of_ training program in a medical school. Nippon Koshu Eisei Zasshi,
CLSI_Documents 51(7), 552-560.
Cohen, J., & Cohen, P. (1983). Applied multiple regression/correlation Pelletier, K. R. (1996). A review and analysis of the health cost-effective
analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erl- outcome studies of comprehensive health promotion and disease
baum Associates. prevention programs at the worksite: 1993-1995 update. American
Eyre, H., Kahn, R., & Robertson, R. M. (2004). Preventing cancer, Journal of Health Promotion, 10(5), 380-388.
cardiovascular disease, and diabetes: A common agenda for the Pritchard, J. E., Nowson, C. A., Billington, T., & Wark, J. D. (2002).
American Cancer Society, the American Diabetes Association, Benefits of a year-long workplace weight loss program on CVD risk
and the American Heart Association. Circulation, 109(25), 3244- factors. Nutrition and Dietetics, 59(2), 87-96.
3255. Seidell, J. C. (2000). Obesity, insulin resistance and diabetes: A world-
Fletcher, G. F., Balady, G., Blair, S. N., Blumenthal J., Caspersen, C., wide epidemic. British Journal of Nutrition, 83(Suppl 1), S5-S8.
Chaitman, B., et al. (1996). Statement on exercise: Benefits and rec- Sherwin, R. S., Anderson, R. M., Buse, J. B., Chin, M., Eddy, D., Frad-
ommendations for physical activity programs for all Americans. A kin, J., et al. (2004). The prevention or delay of type 2 diabetes:
statement for health professionals by the Committee on Exercise American Diabetes Association and the National Institute of Dia-
and Cardiac Rehabilitation of the Council on Clinical Cardiology. betes and Digestive and Kidney Diseases. Diabetes Care, 27(Suppl
Circulation, 94(4), 857-862. 1), S47-S54.
Fleury, J. (1993). An exploration of the role of social networks in cardio- Sorensen, G., & Himmelstein, J. (1992). Worksite nutrition interven-
vascular risk reduction. Heart & Lung, 22(2),134-144. tion. In I. Ockene & J. Ockene (Eds.), Prevention of coronary heart
Glantz, K., & Seewald-Klein, T. (1986). Nutrition at the worksite: An disease (pp. 517-539). Boston: Little, Brown, and Company.
overview. Journal of Nutrition and Education Behavior, 18(Suppl Tuomilehto, J., Lindstrom, J., Eriksson, J. G., Valle, T. T., Hamalainen,
1), S1-S12. H., Elanne-Parikka, P., et al. (2001). Prevention of type 2 diabetes
Grundy, S. M., Pasternak, R., Greenland, P., Smith, S., & Fuster, V. mellitus by changes in lifestyle among subjects with impaired glu-
(1999). Assessment of cardiovascular risk by use of multiple-risk- cose tolerance. New England Journal of Medicine, 344(18), 1343-
factor assessment equations: A statement for healthcare profession- 1350.
als from the American Heart Association and the American College U.S. Department of Agriculture and U.S. Department of Health & Hu-
of Cardiology. Circulation, 100(13), 1481-1492. man Services. (1992). Food guide pyramid (Home and Garden Bul-
Guico-Pabia, C. J., Murray, J. F., Teutsch, S. M., Wertheimer, A. I., & letin No. 249). Washington, DC: U.S. Government Printing Office.
Berger, M. L. (2001). Indirect cost of ischemic heart disease to em- U.S. Department of Agriculture and U.S. Department of Health & Hu-
ployers. American Journal of Managed Care, 7(1), 27-34. man Services. (1995). Dietary guidelines for Americans. Washing-
Guico-Pabia, C. J., Cioffi, L., & Shoner, L. G. (2002). The Lucent- ton, DC: U.S. Government Printing Office.
Takes-Heart cardiovascular health management program: Success- U.S. Department of Health & Human Services. (2000). Healthy people
ful workplace screening. AAOHN Journal, 50(8), 365-372. 2010 (2nd ed.). Washington, DC: U.S. Government Printing Office.
Horowitz, L. G. (1985). The self-care motivation model: Theory and World Health Organization. (1998). Obesity: Preventing and manag-
practice in human development. Journal of School Health, 55(2), ing the global epidemic. Report of a WHO consultation on obesity.
57-61. Geneva: World Health Organization.
Hoyert, D. L., Heron, M. P., Murphy, S. L., & Kung, H. (2006). Deaths: World Health Organization Expert Committee. (1995). Physical sta-
Final data for 2003. Hyattsville, MD: National Center for Health tus: The use and interpretation of anthropometry. Report of a WHO
Statistics. Expert Committee (WHO Technical Report Series: 854). Geneva:
Hubert, H. B., Feinleib, M., McNamara, P. M., & Castelli, W. P. (1983). World Health Organization.
114 AAOHN Journal
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
You might also like
- Nutrition Knowledge, Attitudes, and Self-Regulation As PDFDocument9 pagesNutrition Knowledge, Attitudes, and Self-Regulation As PDFJoem cNo ratings yet
- Open FracturesDocument43 pagesOpen FracturesMohd Johari Mohd ShafuwanNo ratings yet
- Low Carb StudyDocument15 pagesLow Carb StudycphommalNo ratings yet
- dc14-0018 FullDocument8 pagesdc14-0018 FullLo RakNo ratings yet
- Development and Pilot Study of Group-Based Dietary Self-Management Program For Community Dwellers With HypertensionDocument14 pagesDevelopment and Pilot Study of Group-Based Dietary Self-Management Program For Community Dwellers With HypertensionNur Fadillah B21741419601No ratings yet
- Moderators and Mediators of Behaviour Change in A Lifestyle Program For Treated Hypertensives: A Randomized Controlled Trial (ADAPT)Document9 pagesModerators and Mediators of Behaviour Change in A Lifestyle Program For Treated Hypertensives: A Randomized Controlled Trial (ADAPT)Shayan AlPah DoWg KhalidNo ratings yet
- Alternate Day Fasting and Endurance Exercise Combine To Reduce Body Weight and Favorably Alter Plasma Lipids in Obese HumansDocument10 pagesAlternate Day Fasting and Endurance Exercise Combine To Reduce Body Weight and Favorably Alter Plasma Lipids in Obese HumansAndres CaceresNo ratings yet
- Lifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Document10 pagesLifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Agil SulistyonoNo ratings yet
- Am J Clin Nutr 2015 Cespedes Ajcn.Document4 pagesAm J Clin Nutr 2015 Cespedes Ajcn.Jhon Sahatma SinagaNo ratings yet
- Richardson Synthesis Summative 280613Document13 pagesRichardson Synthesis Summative 280613api-217086261No ratings yet
- A Randomized Trial of An Intervention To Improve Self-Care Behaviors of African-American Women With Type 2 DiabetesDocument7 pagesA Randomized Trial of An Intervention To Improve Self-Care Behaviors of African-American Women With Type 2 DiabetesanadamonNo ratings yet
- Lifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Document9 pagesLifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Agil SulistyonoNo ratings yet
- Intermittent Fasting: The Choice For A Healthier LifestyleDocument11 pagesIntermittent Fasting: The Choice For A Healthier LifestyleShamyl Farooq KhanNo ratings yet
- Practices Associated With Weight Loss VeDocument8 pagesPractices Associated With Weight Loss VePedro FerreiraNo ratings yet
- Randomized Trial of Two Mind-Body Interventions For Weight-Loss MaintenanceDocument13 pagesRandomized Trial of Two Mind-Body Interventions For Weight-Loss MaintenanceputriNo ratings yet
- The Long-Term Effects of Lifestyle Change On Blood Pressure: One-Year Follow-Up of The ENCORE StudyDocument8 pagesThe Long-Term Effects of Lifestyle Change On Blood Pressure: One-Year Follow-Up of The ENCORE StudyMarlia NoveliaNo ratings yet
- Hypertension Improvement.....Document4 pagesHypertension Improvement.....Ling 보차No ratings yet
- Clinical Guideline: Annals of Internal MedicineDocument8 pagesClinical Guideline: Annals of Internal MedicineYulias YoweiNo ratings yet
- Jakicic Et Al 2015 ObesityDocument13 pagesJakicic Et Al 2015 ObesityLushy Ayu DistaNo ratings yet
- Tinsley 2018Document8 pagesTinsley 2018mpharmqaNo ratings yet
- Dietary Strategies For Weight Loss MaintenanceDocument10 pagesDietary Strategies For Weight Loss MaintenanceMARKETDIGITAL BNNo ratings yet
- Nutrition and Physical Activity Programs For Obesity Treatment (PRONAF Study) : Methodological Approach of The ProjectDocument11 pagesNutrition and Physical Activity Programs For Obesity Treatment (PRONAF Study) : Methodological Approach of The ProjectRodrigo DelgadoNo ratings yet
- Weight Management Clinical TrialsDocument7 pagesWeight Management Clinical TrialschuariwapoohNo ratings yet
- Dietary Intakes Associated With Successful Weight Loss and Maintenance During The Weight Loss Maintenance TrialDocument10 pagesDietary Intakes Associated With Successful Weight Loss and Maintenance During The Weight Loss Maintenance TrialParth LalNo ratings yet
- Canadian Journal of DiabetesDocument7 pagesCanadian Journal of DiabetesBroc Il SerbatoioNo ratings yet
- Comparison of Weight-Loss Diets With Different Compositions of Fat, Protein, and CarbohydratesDocument15 pagesComparison of Weight-Loss Diets With Different Compositions of Fat, Protein, and CarbohydratesMichael HubbertNo ratings yet
- InduvidualDocument20 pagesInduvidualapi-422930884No ratings yet
- Bacon - Size Acceptance and IntuitIve Eating - JADA.05Document8 pagesBacon - Size Acceptance and IntuitIve Eating - JADA.05Evelyn Tribole, MS, RD100% (2)
- Intermittent Fasting Combined With Calorie Restriction Is Effective For Weight Loss and Cardio-Protection in Obese WomenDocument9 pagesIntermittent Fasting Combined With Calorie Restriction Is Effective For Weight Loss and Cardio-Protection in Obese Womenpriya1832No ratings yet
- Emagrecimento Determinantes ShowwwwDocument41 pagesEmagrecimento Determinantes ShowwwwÉomer LanNo ratings yet
- Order 5553454.editedDocument5 pagesOrder 5553454.editedonka melissaNo ratings yet
- Ntrs 513-Final PaperDocument8 pagesNtrs 513-Final Paperapi-203339953No ratings yet
- Dietary Counselling and Food Fortification in Stable COPD: A Randomised TrialDocument7 pagesDietary Counselling and Food Fortification in Stable COPD: A Randomised TrialJames Cojab SacalNo ratings yet
- Uma Comparação de Dieta Versus Programas de Dieta + Exercícios para Melhoria Da Saúde em Mulheres de Meia-Idade Com Sobrepeso - InglêsDocument23 pagesUma Comparação de Dieta Versus Programas de Dieta + Exercícios para Melhoria Da Saúde em Mulheres de Meia-Idade Com Sobrepeso - InglêsJuliana MontovaniNo ratings yet
- Commercial Weight Loss ProgramsDocument13 pagesCommercial Weight Loss ProgramsJenny Rivera100% (1)
- Modified Mediterranean Diet Score and Cardiovascular Risk in A North American Working PopulationDocument10 pagesModified Mediterranean Diet Score and Cardiovascular Risk in A North American Working Populationapi-356847931No ratings yet
- Effects of Worksite Health Promotion Interventions On Employee Diets: A Systematic ReviewDocument7 pagesEffects of Worksite Health Promotion Interventions On Employee Diets: A Systematic ReviewUtami LukitaNo ratings yet
- Review ArticleDocument17 pagesReview ArticleEgy Sunanda PutraNo ratings yet
- Oti2018 7412686Document17 pagesOti2018 7412686NataliaNo ratings yet
- Acceleration Training For Improving Physical Fitness and Weight Loss in Obese WomenDocument11 pagesAcceleration Training For Improving Physical Fitness and Weight Loss in Obese WomennazkudutNo ratings yet
- Da QingDocument18 pagesDa QingAlina PopaNo ratings yet
- Weight Science: Evaluating The Evidence For A Paradigm ShiftDocument13 pagesWeight Science: Evaluating The Evidence For A Paradigm ShiftJes BakerNo ratings yet
- Effects of Ingestion of A Commercially Available Thermogenic Dietary Supplement On Resting Energy Expenditure, Mood State and Cardiovascular MeasuresDocument8 pagesEffects of Ingestion of A Commercially Available Thermogenic Dietary Supplement On Resting Energy Expenditure, Mood State and Cardiovascular Measuresannish_fitriNo ratings yet
- Review of Low-Carb Vs High-Carb DietsDocument15 pagesReview of Low-Carb Vs High-Carb Dietswtbliss100% (8)
- Effect of Weight Control Counselling in Overweight and Obese Young AdultsDocument7 pagesEffect of Weight Control Counselling in Overweight and Obese Young AdultsAryNo ratings yet
- Comparison of The Atkins Ornish Weight Watchers and Zone Diets For Weight Loss and Heart Disease Risk ReductionDocument12 pagesComparison of The Atkins Ornish Weight Watchers and Zone Diets For Weight Loss and Heart Disease Risk ReductionbhelelihleNo ratings yet
- 1279 3878 1 PBDocument7 pages1279 3878 1 PBAdiyanto DidietNo ratings yet
- Diabetes MellitusDocument8 pagesDiabetes Mellitusi_anitaNo ratings yet
- Is Dieting Good For You?: Prevalence, Duration and Associated Weight and Behaviour Changes For Speci®c Weight Loss Strategies Over Four Years in US AdultsDocument8 pagesIs Dieting Good For You?: Prevalence, Duration and Associated Weight and Behaviour Changes For Speci®c Weight Loss Strategies Over Four Years in US AdultsAdriana MadeiraNo ratings yet
- Mudanças Na Composição Corporal Com Dieta Hipocalórica Combinada Com Atividade Física Sedentária, Moderada e Intensa - Um Ensaio Clínico Randomizado - InglêsDocument21 pagesMudanças Na Composição Corporal Com Dieta Hipocalórica Combinada Com Atividade Física Sedentária, Moderada e Intensa - Um Ensaio Clínico Randomizado - InglêsJuliana MontovaniNo ratings yet
- Physiology Laboratory Evaluating Metabolic Syndrome in A MedicalDocument5 pagesPhysiology Laboratory Evaluating Metabolic Syndrome in A MedicalTambunta TariganNo ratings yet
- Appi Ps 201400535 PDFDocument6 pagesAppi Ps 201400535 PDFArif IrpanNo ratings yet
- Nin Research Paperon DiabetesDocument4 pagesNin Research Paperon DiabetesAvantikaNo ratings yet
- داش دايت.fDocument8 pagesداش دايت.fesraaelkordy60No ratings yet
- Bismillah Fix Hba1c3Document8 pagesBismillah Fix Hba1c3NsafifahNo ratings yet
- Dietas de Baixa CaloriaDocument11 pagesDietas de Baixa CaloriaDesolation FestNo ratings yet
- DMSO 27665 Randomized Double Blind Placebo Controlled Linear Dose Cross 011712Document7 pagesDMSO 27665 Randomized Double Blind Placebo Controlled Linear Dose Cross 011712Perfero CaffeNo ratings yet
- Health 2013082314512668 PDFDocument4 pagesHealth 2013082314512668 PDFesbat07No ratings yet
- Financial Impact of A Comprehensive Multisite Workplace Health Promotion ProgramDocument7 pagesFinancial Impact of A Comprehensive Multisite Workplace Health Promotion ProgramGaurav SharmaNo ratings yet
- Diets Among Obese IndividualsDocument26 pagesDiets Among Obese IndividualsjuanpabloefNo ratings yet
- Dash Diet For Beginners - Lower Your Blood Pressure For Healthy Weight LossFrom EverandDash Diet For Beginners - Lower Your Blood Pressure For Healthy Weight LossNo ratings yet
- Coombs and Gell ClassificationDocument34 pagesCoombs and Gell ClassificationAnamNo ratings yet
- Spitting To SurviveDocument2 pagesSpitting To SurviveAnamNo ratings yet
- WaterDocument2 pagesWaterAnamNo ratings yet
- Dean R. Lillard, Rebekka Christopoulou-Life-Course Smoking Behavior - Patterns and National Context in Ten Countries-Oxford University Press (2015)Document305 pagesDean R. Lillard, Rebekka Christopoulou-Life-Course Smoking Behavior - Patterns and National Context in Ten Countries-Oxford University Press (2015)Anam100% (2)
- Outline: Oleh: Septi Dewi RachmawatiDocument11 pagesOutline: Oleh: Septi Dewi RachmawatiAnamNo ratings yet
- Journal of Healthcare Management Sep/Oct 1998 43, 5 Proquest Health ManagementDocument14 pagesJournal of Healthcare Management Sep/Oct 1998 43, 5 Proquest Health ManagementAnamNo ratings yet
- Dampak Kesehatan Ekonomi Perilaku DL: DAN Merokok IndonesiaDocument5 pagesDampak Kesehatan Ekonomi Perilaku DL: DAN Merokok IndonesiaAnamNo ratings yet
- Etiologi Diabetes InsipidusDocument1 pageEtiologi Diabetes InsipidusAnamNo ratings yet
- MRI Magnetic Resonance Imaging (MRI) Written by Brian Krans - Medically Reviewed by Published On July 9, 2012Document6 pagesMRI Magnetic Resonance Imaging (MRI) Written by Brian Krans - Medically Reviewed by Published On July 9, 2012AnamNo ratings yet
- Diet For HemodialisisDocument11 pagesDiet For HemodialisisAnamNo ratings yet
- WWW - Saskatoonhealthregion.ca/ Where Is Magnetic Resonance Imaging Performed?Document6 pagesWWW - Saskatoonhealthregion.ca/ Where Is Magnetic Resonance Imaging Performed?AnamNo ratings yet
- Infection Control: Ageng Bakhtiar RDocument6 pagesInfection Control: Ageng Bakhtiar RAnamNo ratings yet
- Nursing Care Plan AbortionDocument3 pagesNursing Care Plan Abortionnengsk84% (19)
- Pharmacology Module Answers Quizzes and Test Bank 1Document228 pagesPharmacology Module Answers Quizzes and Test Bank 1Justine Rabanes100% (2)
- Website Advt EnglishDocument7 pagesWebsite Advt EnglishsapnaNo ratings yet
- PE 10-Module 1-Q2Document18 pagesPE 10-Module 1-Q2Gloria TolentinoNo ratings yet
- Coronavirus (COVID-19) Quiz Review For NursesDocument11 pagesCoronavirus (COVID-19) Quiz Review For Nurseshasan ahmdNo ratings yet
- Innovative Approaches For Improving Maternal and Newborn Health - A Landscape AnalysisDocument19 pagesInnovative Approaches For Improving Maternal and Newborn Health - A Landscape AnalysisAli Abubakar AuduNo ratings yet
- Metamizole A Review Profile of A Well Known Forgotten Drug Part II Clinical ProfileDocument16 pagesMetamizole A Review Profile of A Well Known Forgotten Drug Part II Clinical ProfileTifanny WijayaNo ratings yet
- Health Effects Smoking & Tobacco Use CDCDocument1 pageHealth Effects Smoking & Tobacco Use CDCNisa septianiNo ratings yet
- UP WSS Tender April 2020Document6 pagesUP WSS Tender April 2020Shweta JoshiNo ratings yet
- Differential Diagnosis of Periapical RadiopacitiesDocument19 pagesDifferential Diagnosis of Periapical RadiopacitiesNaishadh DalalNo ratings yet
- KMC ProjectDocument2 pagesKMC ProjectNadiya RashidNo ratings yet
- Elizabeth Gilbert CVDocument2 pagesElizabeth Gilbert CVapi-577634408No ratings yet
- Medication Administration QuestionsDocument17 pagesMedication Administration QuestionsJacqueline Greer100% (1)
- Probiotics and Prebiotics Health ClaimDocument3 pagesProbiotics and Prebiotics Health ClaimPhilipNo ratings yet
- Plan of Action NutritionDocument31 pagesPlan of Action NutritionMary Rose MartinezNo ratings yet
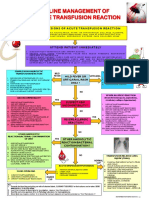
- Transfusion Reaction PDFDocument1 pageTransfusion Reaction PDFKah Man GohNo ratings yet
- Personal HygieneDocument15 pagesPersonal HygieneIvan ToledoNo ratings yet
- MIMS JPOG 2020 Issue 03 ID PDFDocument48 pagesMIMS JPOG 2020 Issue 03 ID PDFAji NugrozzNo ratings yet
- Care Plan Template CompleteDocument6 pagesCare Plan Template Completeapi-643737824No ratings yet
- Tatiana Novak Resume 2019Document2 pagesTatiana Novak Resume 2019api-490390347No ratings yet
- Worrier To WarriorDocument33 pagesWorrier To WarriorClarice LangitNo ratings yet
- COVID 19 Return To Work 1591258538Document1 pageCOVID 19 Return To Work 1591258538rememberNo ratings yet
- Class CHAPTER 9 - Circulatory With AnswersDocument59 pagesClass CHAPTER 9 - Circulatory With AnswersSara VinuyaNo ratings yet
- Stomatitis Venenata: A Rarity: Case ReportDocument2 pagesStomatitis Venenata: A Rarity: Case ReportJoel Nathaniel Richard JosephNo ratings yet
- NPCDCS Budget and Financial Statement 2021-22Document2 pagesNPCDCS Budget and Financial Statement 2021-22ekta priyawandanaNo ratings yet
- Physical Education: Quarter 3 - Module 1: Benefits of Health-Related FitnessDocument19 pagesPhysical Education: Quarter 3 - Module 1: Benefits of Health-Related FitnessHERNAN JAY BUYOKNo ratings yet
- Designation of Anti-Drug Abuse Council - Reporting System (Adac-Rs) Focal Person and EncodersDocument1 pageDesignation of Anti-Drug Abuse Council - Reporting System (Adac-Rs) Focal Person and Encoderscamille quezonNo ratings yet
- Tinea PedisDocument4 pagesTinea PedisElga Rahadian ArsyahNo ratings yet
- ADA COVID Int Guidance Treat Pts PDFDocument8 pagesADA COVID Int Guidance Treat Pts PDFFavio LunaNo ratings yet