Professional Documents
Culture Documents
Echocardiographic Evaluation of Patent Ductus Arteriosus in Preterm Infants
Uploaded by
VMoraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Echocardiographic Evaluation of Patent Ductus Arteriosus in Preterm Infants
Uploaded by
VMoraCopyright:
Available Formats
Review
published: 21 June 2017
doi: 10.3389/fped.2017.00147
Romaine Arlettaz*
Department of Neonatology, University Hospital Zurich, Zurich, Switzerland
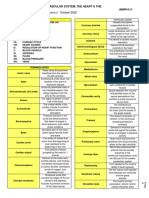
Patent ductus arteriosus (PDA) is part of the typical morbidity profile of the preterm
infant, with a high incidence of 8090% in extremely low birth weight infants born before
26weeks of gestation. Whereas spontaneous closure of the ductus arteriosus (DA) is
likely in term infants, it is less so in preterm ones. PDA is associated with increased mor-
tality and various comorbidities including cardiac failure, need for respiratory support,
bronchopulmonary dysplasia, pulmonary or intracranial hemorrhage, and necrotizing
enterocolitis; however, there is no proven causality between these morbidities and the
presence of DA. Thus, the indication to close PDA remains highly controversial. This
paper focuses on echocardiographic evaluation of PDA in the preterm infant and partic-
ularly on the echocardiographic signs of hemodynamic significance.
Keywords: preterm infant, patent ductus arteriosus, functional echocardiography, extremely low birth weight
Edited by: infant, ductus arteriosus
Cecile Tissot,
The University Childrens Hospital,
Switzerland
INTRODUCTION
Reviewed by:
Patrick O. Myers,
Preterm infants account for 612% of the newborn population and represent the main group of
Universit de Genve, Switzerland
Yogen Singh,
infants treated in neonatal intensive care units. Among the typical complications observed in pre-
Addenbrookes Hospital, term infants, patent ductus arteriosus (PDA) is frequent. Its incidence is inversely proportional to
United Kingdom the preterm infants gestational age, with a rate of about 20% in premature infants born at 32weeks of
*Correspondence:
gestation compared to an estimated 8090% in extremely low birth weight infants with a gestational
Romaine Arlettaz age of less than 26weeks (1, 2). The likelihood of spontaneous closure of the ductus arteriosus (DA)
romaine.arlettaz@usz.ch in full-term infants without congenital heart disease is very high; in the preterm infant, closure rates
are poorer (13). However, recent studies have shown that PDA will have spontaneously closed by
Specialty section: the end of the first week of life in about 73% of preterm infants with a gestational age of 28weeks (3).
This article was submitted According to the international literature, PDA is associated with not only increased mortality but
to Pediatric Cardiology, also various neonatal comorbidities (1, 2, 4, 5). These include cardiac failure, need for respiratory
a section of the journal support, need for supplemental oxygen, bronchopulmonary dysplasia, pulmonary hemorrhage,
Frontiers in Pediatrics
intraventricular hemorrhage, abnormal cerebral perfusion, and necrotizing enterocolitis. Against
Received: 13January2017 this background, it became common practice in 1990s to follow a strategy of aggressive medicamen-
Accepted: 12June2017 tous or surgical closure of PDA in very preterm infants. Nowadays, we know that there is no real
Published: 21June2017
proven causality between mortality, neonatal morbidities, and PDA (2, 5). The indications to close
Citation: PDA have, therefore, decreased dramatically, and the procedure remains controversial. The current
ArlettazR (2017) Echocardiographic approach is to limit treatment to infants most likely to benefit from intervention, i.e., extremely low
Evaluation of Patent Ductus
Arteriosus in Preterm Infants.
Front. Pediatr. 5:147. Abbreviations: DA, ductus arteriosus; hsPDA, hemodynamically significant patent ductus arteriosus; LA:Ao, left atrium to
doi: 10.3389/fped.2017.00147 aortic valve; LAX, long axis view; PDA, patent ductus arteriosus; SAX, short axis view.
Frontiers in Pediatrics | www.frontiersin.org 1 June 2017|Volume 5|Article 147
Arlettaz Echocardiographic Evaluation of PDA
birth weight infants, particularly those on respiratory support the DA. The only window which is not appropriate for detecting
and at risk of rapidly developing a hemodynamically significant DA is the apical four chamber view.
PDA (hsPDA) (5).
As clinical signs of PDA are not sensitive or specific enough, Ductal Size
all extremely preterm infants at risk of developing PDA should The most accurate view for measuring the size of the DA is the
undergo echocardiography. The main goal of the present review high left parasternal short axis window, also called ductal view.
is to define and develop the different steps in echocardiographic Concentrating on the main pulmonary artery, the origin of the
evaluation of PDA in the preterm infant. right pulmonary artery, which is not always visible, and of the
left pulmonary artery can be visualized; the DA is positioned to
the left of it. The DA should be measured at its narrowest point,
ECHOCARDIOGRAPHIC EVALUATION before its entry into the main pulmonary artery (Figure4).
OF PDA Measurement of the ductal size is not very accurate. It is not
recommended to use the color Doppler, which can exaggerate the
General Considerations size. Measurements must always be performed using a consistent
It is important to consider some general guidelines when evaluat- technique. A PDA is considered small at <1.5 mm, moderate
ing PDA. Although DA is the focus of functional echocardiogra- when it ranges between 1.5 and 3mm, and large if the dimension
phy, the baby should always undergo a complete echocardiogram exceeds 3mm. SAX should not be chosen to measure ductal size
first. An initial echocardiogram enables (i) structural congenital because it is not always possible to differentiate the left pulmonary
heart disease to be excluded, (ii) biventricular function to be artery from the DA.
measured, and (iii) different aspects of transitional circulation to
be checked, as for example pulmonary pressures. Direction of the Shunt across the PDA
When performing functional echocardiography, it is also The direction of the shunt across the PDA can be right to left,
important to bear in mind the difficulties and challenges asso- bidirectional, or left to right. In order to document it, color
ciated with scanning a premature infant. Some babies are very Doppler is required. A right-to-left shunt across the PDA is more
small, they can be agitated or unstable, have a high heart rate, difficult to see: color Doppler will show a flow going from the
and sometimes a poor echo window, particularly if they are pulmonary artery toward the descending aorta. Thus, both great
ventilated and have severe underlying lung disease. Some simple arteries and the DA will appear blue on color Doppler because
tricks include the following: place the baby in the best position the blood moves away from the transducer. Placing pulsed
(slightly turned to the left with a slightly extended neck), scan the wave Doppler over the DA shows a Doppler wave below the
baby when it is in a quiet and stable state whenever possible, and baseline, usually during systole. Less often, a continuous flow
allow plenty of time. during systole and diastole can be observed, representing a pure
right-to-left shunt (Figure 5). When the pulmonary vascular
resistance falls, the shunt will be bidirectional with a flow above
Specific Evaluation of PDA the baseline during the systole and below the baseline during the
Echocardiographic evaluation of PDA in the preterm infant will diastole (Figure6). Velocities are usually low and suggest equal
help physicians answer the following questions: Is the DA patent? pressure in the pulmonary artery and the descending aorta. Color
What is its size? What is the direction of the shunt? Is the PDA Doppler shows alternating red and blue. Once the pulmonary
hemodynamically significant? pressure drops further, the shunt will be left to right and appears
red on color Doppler. On pulsed or continuous wave Doppler,
Ductal Patency maximal velocities during systole and diastole can be measured,
Patent ductus arteriosus can be seen on each of the classic echo see below. It is also possible to demonstrate shunt direction on
views, but the most preferred views are the parasternal short color Doppler using M-Mode (Figure6).
axis view (SAX) and the suprasternal view. With SAX, the DA
is visualized at the base of the heart by moving the probe slightly Is the PDA Hemodynamically Significant?
anteriorly toward the pulmonary artery. A small DA can easily In a physiological state, the pulmonary to systemic flow ratio
be missed on 2D pictures, thus pulsed wave Doppler and color (Qp:Qs) is 1. The right ventricular output reflects the systemic
Doppler are helpful (Figure1). Pulsed wave Doppler in the main blood flow whereas the left ventricular output reflects the pul-
pulmonary artery shows a quiet flow when the DA has closed and monary blood flow. The shunt across the patent foramen ovale
turbulent systolic and diastolic flow when DA is patent (Figure1). influences the right ventricular output, and the shunt across the
For the suprasternal view, the probe should be placed at a sagittal PDA influences the left ventricular output. Thus, ventricular
level at the midline in order to visualize the pulmonary artery on output measurements in a newborn infant with open DA and
the left and the descending aorta on the right of the picture. The foramen ovale are not very accurate.
DA appears between both great arteries (Figure2). In the case of hsPDA, the pulmonary blood flow increases due
Besides the SAX and suprasternal views, it is also possible to to the amount of blood running back from the descending aorta
see the DA in the parasternal long axis view (LAX) by moving into the lung circulation through PDA; this pattern is known as
the probe from the classic LAX anteriorly toward the pulmonary steal phenomenon. At the same time, the systemic blood flow
artery (Figure3). The subcostal LAX also allows the detection of decreases for the same reason. Qp:Qs ratio will increase.
Frontiers in Pediatrics | www.frontiersin.org 2 June 2017|Volume 5|Article 147
Arlettaz Echocardiographic Evaluation of PDA
FIGURE 1 | Visualization of patent ductus arteriosus in short axis view (SAX). (A) 2D SAX moved anteriorly, (B) same picture with color Doppler, (C) Doppler in the
main pulmonary artery by closed duct, and (D) Doppler in the main pulmonary artery by patent duct. MPA, main pulmonary artery; RPA, right pulmonary artery; LPA,
left pulmonary artery; AAo, ascending aorta.
FIGURE 2 | Visualization of patent ductus arteriosus (PDA) in suprasternal view. (A) Normal suprasternal view of the aortic arch, (B) suprasternal sagittal view with
pulmonary artery and descending aorta, and (C) color Doppler in a sagittal suprasternal view with PDA in red.
There is no clear clinical definition of hsPDA. Sosenko etal. and/or arterial hypotension requiring vasopressor treatment.
(6) mentioned hsPDA in the presence of clinical signs of PDA McNamara and Sehgal (7) proposed a staging system with a
associated either with pulmonary hemorrhage, or with cardio- comparison between clinical and echocardiographic criteria of
megaly and signs of pulmonary edema, as well as respiratory failure hsPDA.
Frontiers in Pediatrics | www.frontiersin.org 3 June 2017|Volume 5|Article 147
Arlettaz Echocardiographic Evaluation of PDA
FIGURE 3 | Visualization of patent ductus arteriosus in long axis view (LAX). (A) 2D classical LAX, (B) LAX slightly tilted anteriorly toward the pulmonary artery, and
(C) main pulmonary artery with pulmonary branches. RV, right ventricle; LV, left ventricle; AV, aortic valve; PV, pulmonary valve; MPA, main pulmonary artery; RPA,
right pulmonary artery; LPA, left pulmonary artery.
FIGURE 4 | Measurement of patent ductus arteriosus (PDA) size on suprasternal view. MPA, main pulmonary artery; RPA, right pulmonary artery; LPA, left
pulmonary artery.
The main echocardiographic criteria mentioned in the literature aortic valve, with the transducer placed perpendicular to it. The
include an enlargement of the left atrium with a left atrium to aor- aortic valve is measured just before its opening, at the end of
tic valve (LA:Ao) ratio of 1.5, and absent or retrograde diastolic the diastole, whereas the left atrium is measured at its maximal
flow in the descending aorta, absent or retrograde diastolic flow volume during the systole. The LA:Ao ratio should not exceed 1.5.
in the mesenteric superior artery and/or in the anterior cerebral This measurement is easy to perform but not very accurate for
artery, a moderate to large PDA diameter of 1.5 mm at the two reasons: first, the left atrium is not always easy to delimitate,
narrowest point, and an unrestrictive pulsatile transductal flow particularly because of the entrance of the pulmonary veins
(2, 5, 6, 812). into it. Second, the atrial shunt influences LA:Ao ratio as a large
foramen ovale or atrial septal defect will allow the engorged left
How Can We Measure These Parameters? atrium to empty into the right one.
LA:Ao ratio is measured on parasternal LAX using M-Mode A further sign of hsPDA is the absent or retrograde diastolic
(Figure 7). A cut is made in the left atrium at the level of the flow in the descending aorta. In order to visualize this, the
Frontiers in Pediatrics | www.frontiersin.org 4 June 2017|Volume 5|Article 147
Arlettaz Echocardiographic Evaluation of PDA
FIGURE 5 | Right-to-left shunt across the patent ductus arteriosus (PDA). (A) Short axis view; color Doppler flow pattern is blue during systole and diastole, (B) flow
across the PDA is below the baseline during systole, and (C) flow across the PDA is below the baseline during systole and diastole in the case of pure right-to-left
shunt. MPA, main pulmonary artery; RPA, right pulmonary artery; LPA, left pulmonary artery.
FIGURE 6 | Suprasternal view with (A) bidirectional shunt, (B) bidirectional shunt predominantly left-to-right, (C) left-to-right shunt on color Doppler, and
(D) left-to-right shunt on color Doppler M-Mode.
Frontiers in Pediatrics | www.frontiersin.org 5 June 2017|Volume 5|Article 147
Arlettaz Echocardiographic Evaluation of PDA
transducer has to be placed in the postductal descending aorta;
the pulsed wave Doppler is used. In a physiological situation, the
Doppler wave is anterograde during the systole and the diastole,
with the wave seen under the baseline. When the steal phenom-
enon appears, the end diastolic flow will be absent, and if the
Qp:Qs ratio further increases, the flow will be retrograde during
the whole diastole, appearing above the baseline (Figure 8).
This measurement is one of the most specific in evaluating the
hemodynamic significance of PDA.
In a similar way, the diastolic flow is measured in the
abdominal descending aorta and in the mesenteric superior
artery. Again, the diastolic flow should be anterograde and
is seen as a Doppler curve above the baseline. In the case of
hsPDA, it can be absent or even appear retrograde (Figure9).
In this case, the perfusion of the small intestine is assumed to
be compromised.
FIGURE 7 | Measurement of LA:Ao ratio in parasternal long axis view in
Last but not least, the Doppler flow pattern across the PDA
M-Mode.
is measured. This will show one of three patterns (Figure10).
FIGURE 8 | Suprasternal view: (A) color Doppler of the postductal descending aorta with (B) normal anterograde flow, (C) absent end diastolic flow, and
(D) pandiastolic retrograde flow.
Frontiers in Pediatrics | www.frontiersin.org 6 June 2017|Volume 5|Article 147
Arlettaz Echocardiographic Evaluation of PDA
FIGURE 9 | Subcostal view of the descending aorta abdominalis with visualization of the truncus coeliacus and superior mesenteric artery, (A) on 2D, (B) on color
Doppler, (C) with anterograde flow, (D) with absent end diastolic flow, and (E) with retrograde flow. TC, truncus coeliacus; SMA, superior mesenteric artery.
FIGURE 10 | Transductal flow on Doppler in short axis view or suprasternal view: (A,B) unrestrictive pulsatile flow and (C) restrictive continuous flow.
Non-hemodynamically significant PDA has a high flow velocity transductal flow. If the PDA is moderately hemodynamically
during systole and diastole with a maximal velocity above 2m/s significant, the Doppler flow pattern has a maximal dias-
at the end of the diastole; this is called restrictive continuous tolic velocity of less than 2 m/s and is called unrestrictive
Frontiers in Pediatrics | www.frontiersin.org 7 June 2017|Volume 5|Article 147
Arlettaz Echocardiographic Evaluation of PDA
pulsatile transductal flow. In a large hsPDA, the flow is also by a bidirectional shunt and later a left-to-right shunt with low
an unrestrictive pulsatile transductal flow but the maximal ductal flow velocities (15). With the physiological lowering and
end-diastolic velocity is below 1m/s. Next to the absolute values, normalization of the pulmonary pressures, an increase in the
it is also possible to measure the ratio between the systolic and systolic and diastolic velocities is observed. Also, the ductal size
diastolic velocities. If the peak diastolic velocity is more than measured in the first 2days of life is a good predictor of develop-
50% of the peak systolic velocity, the flow pattern is restrictive. ment of symptomatic DA, which is not the case later in life.
If this ratio is less than 50%, the flow pattern is pulsatile suggest- Thus, the approach used in assessing hsPDA varies according
ing hemodynamically significant PDA. to the timing of echo.
Summary of Echocardiographic
Parameters of PDA DISCUSSION
The most specific echocardiographic parameters of PDA can
Echocardiographic evaluation of PDA in very preterm infants is
be divided into three groups: (i) the ductal characteristics,
one of the everyday activities in a neonatal intensive care unit and
(ii) overcirculation of the lungs, and (iii) systemic hypoperfusion.
is usually performed by not only pediatric cardiologists but also
The latter two are observed in the case of hsPDA.
by neonatologists or pediatric intensivists trained in functional
echocardiography. It is not easy to perform echocardiograms in
The Characteristics of PDA extremely preterm infants, and the fact that there is intra- as well
The characteristics of PDA are best evaluated by measuring as interobserver variability is certainly not optimal. Thus, it is
the ductal size and the velocities across the DA, both in a important to follow some basic rules. First, echocardiogram can
suprasternal sagittal view. The ductal diameter measured on focus on PDA only after a previous complete echo has excluded
the first day of life has a high sensitivity and specificity in structural congenital heart disease and measured ventricular
predicting the development of hsPDA (2). Further authors also function. Second, scanning a preterm infant can be challeng-
describe the association between ductal size and the need for ing, and the evaluation of PDA is time consuming, so it is also
further medicamentous or surgical closure (13). Measuring important to keep in mind the general considerations described
flow velocities from the suprasternal view gives information in this review.
about the direction of the shunt and allows pulmonary pres- If the echocardiogram of a preterm infant with PDA has been
sures to be assessed. Furthermore, quantification of the systolic performed by a neonatologist or intensivist, the echocardio-
and diastolic flow velocities across the PDA and particularly graphic findings should be confirmed by a pediatric cardiologist
the peak systolic to end diastolic flow velocity ratio is a good and a joint decision should be taken regarding treatment of PDA
predictor of ductal patency in preterm infants born before and follow-up of the baby.
32weeks of gestation (14). The debate on whether or not to treat PDA is beyond the
scope of the present review. However, many authors suggest
Pulmonary Hyperperfusion treating only babies presenting with hsPDA and showing clini-
Pulmonary hyperperfusion is best documented with a LA:Ao cal signs of respiratory failure. Indeed, a baby doing very well
ratio of 1.5, an increased flow across the mean pulmonary and not requiring ventilator support or supplemental oxygen
artery, an elevated diastolic flow in the left pulmonary artery, will usually not benefit from ductal closure. In this sense, echo-
and a mitral E/A ratio of >1.5 suggesting severe left heart cardiographic evaluation of PDA should be accompanied by the
pressure loading (2, 7). The most popular echocardiographic definition of its clinical significance. One possible approach is
parameter is the LA:Ao ratio which is easy to measure. However, the staging system published 10 years ago by McNamara and
this parameter is influenced by the shunt across the patent fora- Sehgal (7), setting out a detailed correlation between the clinical
men ovale. and echocardiographic signs. Neonatologists may find this help-
ful in deciding if and when to start medicamentous treatment
Systemic Hypoperfusion in order to close PDA.
Systemic hypoperfusion is best evaluated with the presence of a
retrograde flow in the descending aorta as well as in the anterior
cerebral and the superior mesenteric arteries. AUTHOR CONTRIBUTIONS
These parameters help to grade PDA as non-symptomatic,
or mildly, moderately, or severely hemodynamically significant. RA is the only author and has fully contributed to the manuscript.
The literature fails to agree on the best parameters for assess-
ing ductal significance, but Condo etal. suggested ductal size
and flow patterns to be the most sensitive (9). However, these ACKNOWLEDGMENTS
parameters have to be related to the clinical symptoms pre-
sented by the baby as well as its postnatal age. The hemodynamic All of the echocardiographic pictures were taken by me and are
transition, characterized by an elevated pulmonary vascular included with the written authorization of the patients parents.
resistance, will be reflected on echocardiography by a predomi- I would like to thank them all for allowing us to publish the
nantly right-to-left shunt in the first minutes of life, followed pictures.
Frontiers in Pediatrics | www.frontiersin.org 8 June 2017|Volume 5|Article 147
Arlettaz Echocardiographic Evaluation of PDA
REFERENCES 10. Vanhaesebrouck S, Zonnenberg I, Vandervoort P, Bruneel E,
Van Hoestenberghe MR, Theyskens C. Conservative treatment for patent
1. Bose CL, Laughon MM. Patent ductus arteriosus: lack of evidence for ductus arteriosus in the preterm. Arch Dis Child Fetal Neonatal Ed (2007)
common treatments. Arch Dis Child Fetal Neonatal Ed (2007) 92:F498502. 92:F2447. doi:10.1136/adc.2006.104596
doi:10.1136/adc.2005.092734 11. Iwashima S, Ishikawa T. Quantitative, noninvasive assessment of patent ductus
2. Heuchan AM, Clyman RI. Managing the patent ductus arteriosus: current arteriosus shunt flow by measuring proximal isovelocity surface area on color
treatment options. Arch Dis Child Fetal Neonatal Ed (2014) 99:F4316. Doppler imaging. Circ J (2014) 78:23028. doi:10.1253/circj.CJ-14-0229
doi:10.1136/archdischild-2014-306176 12. Tauzin L, Joubert C, Noel AC, Bouissou A, Moulies ME. Effects of persistent
3. Rolland A, Shankar-Aguilera S, Diomand D, Zupan-Simunek V, Boileau P. patent ductus arteriosus on mortality and morbidity in very low-birthweight
Natural evolution of patent ductus arteriosus in the extremely preterm infants. Acta Paediatr (2012) 101:41923. doi:10.1111/j.1651-2227.2011.02550.x
infant. Arch Dis Child Fetal Neonatal Ed (2015) 100:F558. doi:10.1136/ 13. Tschuppert S, Doell C, Arlettaz-Mieth R, Baenziger O, Rousson V, Balmer C,
archdischild-2014-306339 etal. The effect of ductal diameter on surgical and medical closure of patent
4. Benitz WE. Treatment of persistent patent ductus arteriosus in preterm ductus arteriosus in preterm neonates: size matters. JThorac Cardiovasc Surg
infants: time to accept the null hypothesis? JPerinatol (2010) 30:24152. (2008) 135:7882. doi:10.1016/j.jtcvs.2007.07.027
doi:10.1038/jp.2010.3 14. Smith A, Maguire M, Livingstone V, Dempsey EM. Peak systolic to end
5. Kluckow M, Jeffery M, Gill A, Evans N. A randomised placebo-controlled diastolic flow velocity ratio is associated with ductal patency in infants below
trial of early treatment of the patent ductus arteriosus. Arch Dis Child Fetal 32 weeks of gestation. Arch Dis Child Fetal Neonatal Ed (2014) 100:F1326.
Neonatal Ed (2014) 99:F99104. doi:10.1136/archdischild-2013-304695 doi:10.1136/archdischild-2014-306439
6. Sosenko IRS, Fajardo MF, Claure N, Bancalari E. Timing of patent ductus 15. Van Vonderen JJ, te Pas AB, Kolster-Bijdevaate C, van Lith JM, Blom NA,
arteriosus treatment and respiratory outcome in premature infants: a Hooper SB, et al. Non-invasive measurements of ductus arteriosus flow
double-blind randomized controlled trial. JPediatr (2012) 160:92935. directly after birth. Arch Dis Child Fetal Neonatal Ed (2014) 99:F40812.
doi:10.1016/j.jpeds.2011.12.031 doi:10.1136/archdischild-2014-306033
7. McNamara PJ, Sehgal A. Towards rational management of the patent ductus
Conflict of Interest Statement: The author declares that the research was
arteriosus: the need for disease staging. Arch Dis Child Fetal Neonatal Ed
conducted in the absence of any commercial or financial relationships that could
(2007) 92:F4247. doi:10.1136/adc.2007.118117
be construed as a potential conflict of interest.
8. Sellmer A, Bjerre JV, Schmidt MR, McNamara PJ, Hjortdal VE, Host B, etal.
Morbidity and mortality in preterm neonates with patent ductus arteriosus Copyright 2017 Arlettaz. This is an open-access article distributed under the terms
on day 3. Arch Dis Child Fetal Neonatal Ed (2013) 98:F50510. doi:10.1136/ of the Creative Commons Attribution License (CC BY). The use, distribution or
archdischild-2013-303816 reproduction in other forums is permitted, provided the original author(s) or licensor
9. Condo M, Evans N, Bellu R, Kluckow M. Echocardiographic assessment of are credited and that the original publication in this journal is cited, in accordance
ductal significance: retrospective comparison of two methods. Arch Dis Child with accepted academic practice. No use, distribution or reproduction is permitted
Fetal Neonatal Ed (2012) 97:F358. doi:10.1136/adc.2010.207233 which does not comply with these terms.
Frontiers in Pediatrics | www.frontiersin.org 9 June 2017|Volume 5|Article 147
You might also like
- Natural Way To Lower Blood Pressure Without Making Blood PressureDocument3 pagesNatural Way To Lower Blood Pressure Without Making Blood Pressurekirang gandhi100% (1)
- Pacemaker Invasive Cardiac PacingDocument57 pagesPacemaker Invasive Cardiac PacingAhmad Khalil Ahmad Al-SadiNo ratings yet
- Cardiovascular Physiology MCQsDocument24 pagesCardiovascular Physiology MCQsKlarens Affana63% (8)
- Hemodynamic MonitoringDocument10 pagesHemodynamic MonitoringDivya Joy100% (1)
- Patent Ductus ArteriosusDocument6 pagesPatent Ductus ArteriosusnidyaparasayuNo ratings yet
- Peritoneal Dialysis Manual: A Guide for Understanding the TreatmentFrom EverandPeritoneal Dialysis Manual: A Guide for Understanding the TreatmentRating: 5 out of 5 stars5/5 (1)
- Patent Ductus Arteriosus: by Dr. Hanan Zekri Khaled Lecturer of Pediatrics Pediatric CardiologyDocument36 pagesPatent Ductus Arteriosus: by Dr. Hanan Zekri Khaled Lecturer of Pediatrics Pediatric CardiologyEira RajkumarNo ratings yet
- The Diagnosis and Management of The Acute Abdomen in Pregnancy-Greenspan, Peter, Springer Verlag (2017)Document284 pagesThe Diagnosis and Management of The Acute Abdomen in Pregnancy-Greenspan, Peter, Springer Verlag (2017)AndreaAlexandraNo ratings yet
- Patent Ductus Arteriosus NewDocument16 pagesPatent Ductus Arteriosus NewchelNo ratings yet
- Chapter 12 - Heart-1Document63 pagesChapter 12 - Heart-1Thania IslaNo ratings yet
- Cardiovascular DisorderDocument88 pagesCardiovascular DisorderSandeepNo ratings yet
- Pda Nuru PDFDocument18 pagesPda Nuru PDFSiti AisyahNo ratings yet
- Manegment PCADocument9 pagesManegment PCAhassam_650No ratings yet
- Pulmonary Vascular Obstructive Disease Prevention: A Case Report of Management Approach in CAVSD With Large PDADocument4 pagesPulmonary Vascular Obstructive Disease Prevention: A Case Report of Management Approach in CAVSD With Large PDAArthur WiyonoNo ratings yet
- I1551 6776 12 3 138 PDFDocument9 pagesI1551 6776 12 3 138 PDFIvan VeriswanNo ratings yet
- 3. a Clinical and Echocardiographic Approach to Evaluation of Patent Ductus Arteriosus in Preterm InfantsDocument6 pages3. a Clinical and Echocardiographic Approach to Evaluation of Patent Ductus Arteriosus in Preterm InfantsAfi ArdineNo ratings yet
- Pediatrics in Review 2001 McDaniel 265 70Document8 pagesPediatrics in Review 2001 McDaniel 265 70misbah_mdNo ratings yet
- Role of Neonatologist-Performed Echocardiography in The Assessment and T Management of Patent Ductus Arteriosus Physiology in The NewbornDocument6 pagesRole of Neonatologist-Performed Echocardiography in The Assessment and T Management of Patent Ductus Arteriosus Physiology in The Newbornannie.estdiNo ratings yet
- Causes and Treatment of Patent Ductus Arteriosus (PDADocument3 pagesCauses and Treatment of Patent Ductus Arteriosus (PDACitra WulandariNo ratings yet
- JAIN 2015_PDA diagnosis evaluation and managementDocument10 pagesJAIN 2015_PDA diagnosis evaluation and managementRafael JustinoNo ratings yet
- Early Surgical Closure of Atrial Septal Defect Improves Clinical Status of Symptomatic Young Children With Underlying Pulmonary AbnormalitiesDocument10 pagesEarly Surgical Closure of Atrial Septal Defect Improves Clinical Status of Symptomatic Young Children With Underlying Pulmonary AbnormalitiesAbdurrahman HasanuddinNo ratings yet
- Editorial: Atrial Septal Defect in Adults: Does Repair Always Mean Cure?Document3 pagesEditorial: Atrial Septal Defect in Adults: Does Repair Always Mean Cure?Andrey AndrNo ratings yet
- ZLJM_17_2007603Document5 pagesZLJM_17_2007603Faradiba MaricarNo ratings yet
- Ductus ArteriosoDocument17 pagesDuctus ArteriosoJohn Romero CevallosNo ratings yet
- 1echocardiography and The NeonatologistDocument4 pages1echocardiography and The NeonatologistAbuAlezzAhmedNo ratings yet
- Spontaneous Closure of Patent Ductus Arteriosus in Infants 1500 GDocument8 pagesSpontaneous Closure of Patent Ductus Arteriosus in Infants 1500 GBrave KazmiNo ratings yet
- Atent Ductus Arteriosus in Preterm InfantsDocument8 pagesAtent Ductus Arteriosus in Preterm InfantsLissaberti AmaliahNo ratings yet
- Midterms Group 5Document25 pagesMidterms Group 5Karina MadriagaNo ratings yet
- Use of Occlutech Fenestrated Atrial Septal Defect Occluder in ASD Associated Pulmonary Arterial HypertensionDocument4 pagesUse of Occlutech Fenestrated Atrial Septal Defect Occluder in ASD Associated Pulmonary Arterial HypertensionMaruliNo ratings yet
- PDA-postligasyon Syndrome 2018 FR PediatricsDocument12 pagesPDA-postligasyon Syndrome 2018 FR PediatricsFunda TüzünNo ratings yet
- Case Study ON: University of Perpetual Help System Cauayan City, IsabelaDocument27 pagesCase Study ON: University of Perpetual Help System Cauayan City, Isabelaliam0831No ratings yet
- Debo Ode 2018Document23 pagesDebo Ode 2018MaluNo ratings yet
- PDA ManagementDocument8 pagesPDA ManagementHujiLokoNo ratings yet
- Ijnrd 8 125Document13 pagesIjnrd 8 125Muhammad Halil GibranNo ratings yet
- Pda 2Document18 pagesPda 2Jicko Street HooligansNo ratings yet
- Michelle E. Van Der Laan, Does Not AffectDocument7 pagesMichelle E. Van Der Laan, Does Not AffectLissaberti AmaliahNo ratings yet
- Current Controversies in The Management of Patent Ductus Arteriosus in Preterm InfantsDocument6 pagesCurrent Controversies in The Management of Patent Ductus Arteriosus in Preterm InfantsManju KumariNo ratings yet
- Cia CivDocument6 pagesCia CivCamila Fda. Muñoz G.No ratings yet
- Treatment of Patent Ductus Arteriosus PDFDocument8 pagesTreatment of Patent Ductus Arteriosus PDFFeny MardiyantiNo ratings yet
- Early Human Development: SciencedirectDocument8 pagesEarly Human Development: SciencedirectYurika Elizabeth SusantiNo ratings yet
- Acyanotic and Cyanotic Congenital Heart DiseasesDocument7 pagesAcyanotic and Cyanotic Congenital Heart DiseasesAndrewNo ratings yet
- Device Closure of Patent Ductus Arteriosus - Congenital Heart Desk Foundation BangladeshDocument22 pagesDevice Closure of Patent Ductus Arteriosus - Congenital Heart Desk Foundation BangladeshTri RachmadijantoNo ratings yet
- Down Cardiac ProblemsDocument6 pagesDown Cardiac Problemstuman20076933No ratings yet
- Nirs Preterm ScreeenDocument6 pagesNirs Preterm ScreeenLissaberti AmaliahNo ratings yet
- Pediatrics in Review 2001 McDaniel 265 70Document8 pagesPediatrics in Review 2001 McDaniel 265 70Darrel Allan MandiasNo ratings yet
- Asd FixDocument5 pagesAsd Fixratna putriNo ratings yet
- jtd-10-S24-S2953Document13 pagesjtd-10-S24-S2953Faradiba MaricarNo ratings yet
- Congenital Heart Disease Presentation and ManagementDocument4 pagesCongenital Heart Disease Presentation and ManagementCh RajeshNo ratings yet
- Arteriosus Fails To Close After Birth. Early Symptoms Are Uncommon, But in The First Year of Life IncludeDocument3 pagesArteriosus Fails To Close After Birth. Early Symptoms Are Uncommon, But in The First Year of Life IncludeFranz Josef ArnucoNo ratings yet
- Patent Ductus ArteriosusDocument3 pagesPatent Ductus ArteriosusMika SaldañaNo ratings yet
- Pediatrics - Neonatal ICUDocument2 pagesPediatrics - Neonatal ICUJasmine KangNo ratings yet
- Approach To A Newborn With Suspected CHD: February 2012Document10 pagesApproach To A Newborn With Suspected CHD: February 2012akshayajainaNo ratings yet
- Contemporary Outcomes of Percutaneous Closure of Patent Ductus Arteriosus in Adolescents and Adults PDFDocument8 pagesContemporary Outcomes of Percutaneous Closure of Patent Ductus Arteriosus in Adolescents and Adults PDFMuhammad IrfanNo ratings yet
- Brown Et Al 2017 Length of Time On Peritoneal Dialysis and Encapsulating Peritoneal Sclerosis Position Paper For IspdDocument13 pagesBrown Et Al 2017 Length of Time On Peritoneal Dialysis and Encapsulating Peritoneal Sclerosis Position Paper For IspdGema CanalesNo ratings yet
- Prophylactic and Early Targeted Treatment of Patent Ductus ArteriosusDocument5 pagesProphylactic and Early Targeted Treatment of Patent Ductus Arteriosusannie.estdiNo ratings yet
- Patent Ductus Arteriosus: A Contemporary Perspective For The Pediatric and Adult Cardiac Care ProviderDocument23 pagesPatent Ductus Arteriosus: A Contemporary Perspective For The Pediatric and Adult Cardiac Care ProviderLissaberti AmaliahNo ratings yet
- PPK Tata Laksana Patent Ductus Arteriosus (PDADocument98 pagesPPK Tata Laksana Patent Ductus Arteriosus (PDAAdit Wendy YRNo ratings yet
- Neonatal Cardiac Emergencies GuideDocument4 pagesNeonatal Cardiac Emergencies GuideEstellaNo ratings yet
- Follow-Up Transcatheter Closure of Atrial Septal Defect in Young Children: Results andDocument7 pagesFollow-Up Transcatheter Closure of Atrial Septal Defect in Young Children: Results andKholid KuNo ratings yet
- Patent Ductus Arteriosus ClosureDocument7 pagesPatent Ductus Arteriosus ClosureDard TongNo ratings yet
- OkeeaeDocument6 pagesOkeeaeZulqi SusiloNo ratings yet
- Pulmonary Arterial Hypertension in Infants With Chronic Lung Disease: Will We Ever Understand It?Document5 pagesPulmonary Arterial Hypertension in Infants With Chronic Lung Disease: Will We Ever Understand It?Adrian KhomanNo ratings yet
- OperabilityinL RDocument6 pagesOperabilityinL RVimal NishadNo ratings yet
- Effect of Patent Ductus Arteriosus On Pulmonary Vascular DiseaseDocument6 pagesEffect of Patent Ductus Arteriosus On Pulmonary Vascular Diseasebagas rachmadiNo ratings yet
- JPM 2005 030Document4 pagesJPM 2005 030Noon ChaiNo ratings yet
- JCDD 09 00114 v2Document17 pagesJCDD 09 00114 v2Faki D'pasnizerNo ratings yet
- Congenital Nephrotic SyndromeDocument8 pagesCongenital Nephrotic SyndromeVMoraNo ratings yet
- Pediatric Burn ResucitationDocument9 pagesPediatric Burn ResucitationVMoraNo ratings yet
- Pediatric Burn ResucitationDocument9 pagesPediatric Burn ResucitationVMoraNo ratings yet
- ESPGHAN 2017 Complementary FeedingDocument14 pagesESPGHAN 2017 Complementary FeedingChristian Camilo MNo ratings yet
- Algoritmos Gastroenterología PediátricaDocument3 pagesAlgoritmos Gastroenterología PediátricaVMoraNo ratings yet
- Hemodynamics of Cardiac Arrest: Michael. P. Frenneaux and Stig SteenDocument22 pagesHemodynamics of Cardiac Arrest: Michael. P. Frenneaux and Stig SteenJai BabuNo ratings yet
- Physical Examination of The NewbornDocument36 pagesPhysical Examination of The NewbornKaren Joyce TribianaNo ratings yet
- Cardiodynamics - Dra-1. ValerioDocument7 pagesCardiodynamics - Dra-1. ValerioJorelyn FriasNo ratings yet
- Heart and Circulatory System - Female VoiceDocument2 pagesHeart and Circulatory System - Female VoiceMeily ChandraNo ratings yet
- Endocrine System Hormones GuideDocument71 pagesEndocrine System Hormones GuideLittle StuartNo ratings yet
- General Biology 2 ReviewerDocument23 pagesGeneral Biology 2 ReviewerKassandra Cassiopeia MendiolaNo ratings yet
- Original Investigation: JamaDocument11 pagesOriginal Investigation: JamaAdel SALLAMNo ratings yet
- Cardiac Cycle: Understanding the Heart's Vital RhythmDocument20 pagesCardiac Cycle: Understanding the Heart's Vital RhythmKemoy Francis100% (1)
- Exercise Physiology Lecture Note (Specialization)Document97 pagesExercise Physiology Lecture Note (Specialization)Shameem AliNo ratings yet
- Cath Lab Essentials: Basic Hemodynamics For The Cath Lab and ICUDocument38 pagesCath Lab Essentials: Basic Hemodynamics For The Cath Lab and ICUDr. TomNo ratings yet
- What Is Echo?: 1.1 BASIC NotionsDocument21 pagesWhat Is Echo?: 1.1 BASIC NotionsJeet GhoshNo ratings yet
- Assessment Outcomes Interventions Rationale Evaluation for Labor PainDocument2 pagesAssessment Outcomes Interventions Rationale Evaluation for Labor PainArian May MarcosNo ratings yet
- Abnormal heart sounds explainedDocument3 pagesAbnormal heart sounds explainedmuhammad azizulhakimNo ratings yet
- Human Cardiovascular PhysiologyDocument5 pagesHuman Cardiovascular PhysiologyKirsten CruzadoNo ratings yet
- Cardiomyopathy Dilated CardiomyopathyDocument5 pagesCardiomyopathy Dilated Cardiomyopathym3d1k100% (1)
- Murmurs Made Easy Epomedicine 2Document1 pageMurmurs Made Easy Epomedicine 2KC Dela RosaNo ratings yet
- Physical Assessment of Patient With Cardiovascular DisorderDocument3 pagesPhysical Assessment of Patient With Cardiovascular Disordermichelle marquezNo ratings yet
- Uia 10 CARDIOVASCULAR PHYSIOLOGYDocument7 pagesUia 10 CARDIOVASCULAR PHYSIOLOGYLiliesther Erminda Hernandez VallecilloNo ratings yet
- CA Mega Brochure 1090-Rev-B EngDocument6 pagesCA Mega Brochure 1090-Rev-B EngMuhammad Mahbøøb SadiqNo ratings yet
- ANAT Unit 3 Cardiac Conduction System NotesDocument15 pagesANAT Unit 3 Cardiac Conduction System NotesSilvia-Mihaela TatomirNo ratings yet
- Cardio Notes 1Document8 pagesCardio Notes 1Lindsay Grace MandarioNo ratings yet
- DC-N2 Datasheet - 160428Document16 pagesDC-N2 Datasheet - 160428Sayuri SuárezNo ratings yet
- Fisiologia Do Sistema Cardiovascular II e III - TextoDocument6 pagesFisiologia Do Sistema Cardiovascular II e III - TextoDavidson De AraújoNo ratings yet
- 1.08 - The Cardiovascular System, The Heart & The Blood VesselsDocument9 pages1.08 - The Cardiovascular System, The Heart & The Blood Vessels13PLAN, SENTH RUEN, ANo ratings yet