Professional Documents
Culture Documents
4 PDF
4 PDF
Uploaded by
Mario SayasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
4 PDF
4 PDF
Uploaded by
Mario SayasCopyright:
Available Formats
co m m e nta r y
3. Rosen S, Peters CA, Chevalier RL et al. The kidney early event following ischemic injury. Am J Physiol dense intramembranous and mesangial
in congenital ureteropelvic junction obstruction: Renal Physiol 2010; 299: F479–F486.
a spectrum from normal to nephrectomy. J Urol 8. Heyman SN, Fuchs, Jaffe R et al. Renal
deposits were the hallmark of type II, also
2008; 179: 1257–1263. microcirculation and tissue damage during acute known as dense deposit disease (DDD).2
4. Girshovich A, Vinsonneau C, Perez J et al. Ureteral ureteral obstruction in the rat: the effect of saline In type III, deposits could be subendo-
obstruction promotes proliferation and differentia- infusion, indomethacin and radiocontrast.
tion of the renal urothelium into a bladder-like Kidney Int 1997; 51: 653–663.
thelial and subepithelial (Burkholder
phenotype. Kidney Int 2012; 82: 428–435. 9. Conte C, Riant E, Toutain C et al. FGF2 translatio- subtype) or produce complex intramem-
5. Wu XR, Lin JH, Walz T et al. Mammalian uroplakins. nally induced by hypoxia is involved in negative branous, subendothelial, and subepithelial
J Biol Chem 1994; 269: 13716–13724. and positive feedback loops with HIF-1 alpha.
6. Romih R, Korosec P, de Mello Jr W et al. PLoS One [online 2008; 3: e3078. formations with fraying of the lamina
Differentiation of epithelial cells in the urinary 10. Giaccia AJ, Simon MC, Johnson R. The biology densa (Strife and Anders subtype).3 Even
tract. Cell Tissue Res 2005; 320: 259–268. of hypoxia: the role of oxygen sensing in within the same biopsy or a given glomer-
7. Vinsonneau C, Girshovich A, Ben M’rad M et al. development, normal function and disease.
Intrarenal urothelium proliferation: an unexpected Genes Dev 2004; 18: 2183–2194. ulus, pathologists may observe overlap-
ping features between these subtypes,
defying easy classification. While hypo-
complementemia was a well-recognized
see original articles on pages 454 and 465 clinical feature of all these entities, with
the exception of C3 nephritic factor,
C3 glomerulopathy: what’s in causation was largely unknown.
Over the next two decades, increasing
a name? attention was paid to the composition of
the deposits detected by immunofluores-
Vivette D. D’Agati1 and Andrew S. Bomback2 cence. Type I was typically characterized
by deposits of immunoglobulin as well as
Whereas early classifications of membranoproliferative glomerulo- complement components; type II was
nephritis (MPGN) were based on morphologic features, the modern distinguished by deposits of C3 only;
approach is directed at immunofluorescence findings. Glomerular the type III Burkholder variant typically
deposits of C3 alone, without immunoglobulin, are the hallmark of had deposits of immunoglobulin and
complement; whereas the type III Strife
alternative complement pathway dysregulation through inherited or and Anders variant could manifest C3
acquired defects. These immunoglobulin-negative forms are referred either alone or in combination with
to as C3 glomerulopathy, which encompasses both dense deposit immunoglobulins. As long as the patho-
disease and C3 glomerulonephritis. Distinguishing C3 glomerulopathy genesis of these forms remained obscure,
from immunoglobulin-mediated MPGN is opening the way to better the classification was cumbersome to use
and perplexing to clinicians and patholo-
diagnostic, prognostic, and treatment algorithms.
gists alike.
Kidney International (2012) 82, 379–381. doi:10.1038/ki.2012.80 In the past decade, our understanding
of the role of complement in the patho-
genesis of MPGN has illuminated the field
Among glomerular diseases, none has is defined as mesangial interposition and and led to a paradigm shift in classifica-
undergone greater conceptual metamor- duplication of glomerular basement mem- tion (Figure 1). First, the observation that
phosis over the past five years than mem- branes, typically associated with periph- a number of patients with intramembra-
branoproliferative glomerulonephritis eral capillary wall immune deposits. Over nous dense deposits lack an MPGN pat-
(MPGN). In the 1970s, before there was the next two decades, many secondary tern altogether caused the designation
knowledge of pathogenesis, MPGN was forms with clear etiologic associations MPGN II to be discarded in favor of DDD.
categorized on the basis of histologic and (such as related to cryoglobulinemia, dys- Second, pathologists began emphasizing
ultrastructural findings.1–3 The membran- proteinemia, autoimmune disease, and in their reports the presence of isolated
oproliferative pattern of glomerular injury infections) were differentiated from the deposits of C3 in examples of MPGN type
primary idiopathic form. But the patho- I and type III. A major breakthrough was
1Department of Pathology, College of Physicians logic classification of primary MPGN the discovery of genetic mutations or
and Surgeons, Columbia University, New York, New remained problematic because it was deficiencies in complement-regulatory
York, USA and 2Department of Medicine, College based largely on the ultrastructural proteins in patients with isolated C3
of Physicians and Surgeons, Columbia University, appearance and location of deposits, deposits.4,5 Thereafter, ‘C3 glomerulopa-
New York, New York, USA devoid of pathogenetic context. thy’ assumed center stage as a newly rec-
Correspondence: Vivette D. D’Agati, College
Subendothelial and mesangial deposits ognized subgroup encompassing DDD
of Physicians and Surgeons, Department of
Pathology, Columbia University, 630 W. 168th predominated in type I MPGN, where the and those examples of type I and type III
Street, New York, New York 10032, USA. membranoproliferative pattern was typi- (now termed ‘C3 glomerulonephritis’;
E-mail: vdd1@columbia.edu cally well developed.1 Highly electron- C3GN) in which immunofluorescence
Kidney International (2012) 82 379
com m enta r y
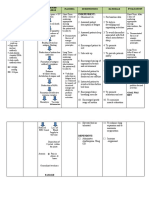
HISTORICAL
stration by Sethi et al.8 that the proteomic
MPGN type II, or dense
CLASSIFICATION MPGN type I
deposit disease (DDD)
MPGN type III profile of C3GN by mass spectrometry
is similar to that of DDD (with predom-
inance of C3 and distal complement path-
Mesangial prolifer-
ation with mesangial Diverse glomerular MPGN pattern, way components) further supports the
LIGHT interposition and histology with or usually with membranous emerging view that the presence of C3
MICROSCOPY GBM duplications without MPGN pattern features alone is the major hallmark of alternative
(MPGN pattern)
complement pathway dysregulation in C3
Mesangial and Mesangial and Mesangial, subendothelial, glomerulopathy, independent of histo-
ELECTRON
MICROSCOPY
subendothelial intramembranous highly subepithelial, and/or logic and ultrastructural features.
deposits electron-dense deposits intramembranous deposits However, the pitfall of lumping diseases
into a single descriptor or category is an
implied assumption of homogeneity.
As compared with atypical hemolytic ure-
C3 with IgG C3 with IgG
IMMUNO- and/or
C3 alone C3 alone C3 alone
and/or mic syndrome, which is also strongly
FLUORESCENCE IgM, C1 IgM, C1 associated with dysregulated alternative
complement pathway activity, C3 glomer-
C3GN DDD C3GN ulopathy manifests a much broader
MODERN
CATEGORIES spectrum of clinical presentation, histopa-
thology, genetic abnormalities, comple-
MPGN type I C3 glomerulopathy MPGN type Ill
ment activity, and prognosis. Servais et al.,
Figure 1 | The evolving classification of membranoproliferative glomerulonephritis (MPGN). looking only at the adult patients in their
Until recently, the classification of primary MPGN into types I, II, and III was based primarily on cohort, found worse 10–year renal sur-
histologic features (light microscopy) and the ultrastructural location and electron density of the
deposits (electron microscopy). With our increased understanding of the role of complement in vival in patients with DDD than in
the pathogenesis of these conditions, the immunofluorescence findings now play a crucial role in patients with MPGN type I and C3GN;7
categorizing MPGN as immunoglobulin-mediated vs. non-immunoglobulin-mediated disease; the Sethi et al., in their smaller cohort, also
latter grouping, which is distinguished by isolated C3 staining on immunofluorescence, has been report worse outcomes in DDD than in
termed ‘C3 glomerulopathy.’ C3 glomerulopathy encompasses C3 glomerulonephritis (C3GN) and
dense deposit disease (DDD). GBM, glomerular basement membrane; IgG, immunoglobulin G; C3GN and suggest that C3GN may be a
IgM, immunoglobulin M. less aggressive entity.8 One possible expla-
nation is the much higher rate of C3
nephritic factor (C3NeF) positivity in
reveals isolated deposits of C3, underscor- stabilize the C3 convertase of the alterna- DDD (86.4% in the French cohort, in
ing the pathogenetic importance of tive pathway (e.g., C3 nephritic factors) or accordance with the approximately 80%
dysregulation of the alternative comple- target the inhibitory complement factors rate described in other cohorts)9 than in
ment pathway. Thus, the modern approach (e.g., factor H autoantibodies). These C3GN (45.3% in the French cohort and
to classification distinguishes those forms abnormalities promote excessive activa- 50% in the American cohort).7,8 Yet even
of MPGN with deposits of C3 only tion of the alternative complement path- this discrepancy is open to question, as
(known as C3 glomerulopathy and includ- way in the fluid phase, with deposition of Servais et al. report a fluctuation of the
ing both DDD and C3GN) from MPGN complement debris, including breakdown C3NeF activity in one-third of their
with deposits of immunoglobulin and products of C3b and components of the patients during follow-up and a normal
complement.6 terminal complement cascade, in the range of serum C3 levels in approximately
The reports from Servais et al.7 and glomerular capillary wall. A reclassifica- 40% of C3NeF-positive patients, suggest-
Sethi et al.8 in this issue of Kidney Interna- tion of MPGN into immunoglobulin- ing that the C3NeF-stabilized C3 conver-
tional highlight the strengths and weak- mediated disease (prompting a work-up tase may be subject to regulation by other
nesses of the term ‘C3 glomerulopathy.’ As for infectious, autoimmune, or dyspro- factors.7 The authors hypothesize that
validation of the classification, defective teinemia-associated etiologies) vs. com- complement-regulatory membrane cofac-
control of the alternative complement plement-mediated disease (prompting a tor protein (MCP) variants may explain
pathway was detectable in 71% of patients work-up of the alternative pathway) this heterogeneity of disease in C3 glomer-
in the French cohort7 (which included should lead to better diagnostic and treat- ulopathy.7 However, they are not able to
cases of C3GN, DDD, and MPGN type I) ment algorithms and, ideally, improved show a functional role of their proposed
and 100 % of those in the American outcomes in these diseases. For example, at-risk MCP haplotype, and the P-values
cohort8 (which included cases of C3GN 9 of the 12 patients with C3GN in the reported for the selected single-nucleotide
only). This defect can be due to mutations American cohort were initially misclassi- polymorphisms in the MCP gene are
in complement proteins (such as C3, fac- fied as having MPGN type I ( n = 4), not robust enough to denote significance,
tor B, factor H, and factor I) or due MPGN type III (n = 1), and postinfectious particularly without replication in an
to acquired autoantibodies that either glomerulonephritis (n = 4). The demon- independent cohort.7
380 Kidney International (2012) 82
co m m e nta r y
One of the most intriguing findings to tions in the complement factor H locus on and raise the question of whether increased
emerge from the French cohort is the human chromosome 1q32.11 C3NeF has activity of the alternative complement
identification of alternative complement also been identified in some patients with pathway on a genetic basis might promote
pathway dysregulation in more than half postinfectious glomerulonephritis. 12 autoimmune phenomena by unbridled
of the 48 patients with MPGN type I.7 In Because patients with complement- activation (and perhaps conformational
fact, a C3NeF was identified as frequently regulatory disorders are not protected change) of the C3 convertase. These find-
in MPGN type I as in C3GN. The termi- from development of other immune- ings suggest a two-hit disease model in
nology ‘C3 glomerulopathy’ is intended mediated glomerulonephritides, future some people. Larger cohorts are needed to
for immunoglobulin-negative diseases, studies will be needed to explore the evaluate the prevalence of this phenome-
to highlight the underlying alternative potential contribution of alternative path- non and the implications for evidence-
pathway dysregulation as opposed to acti- way complement dysregulation beyond based treatment.
vation of the classical pathway by anti- C3 glomerulopathy.
gen–antibody immune complexes. How, Screening tests of alternative comple- DISCLOSURE
The authors declared no competing interests.
then, should we classify the MPGN type I ment pathway activity may help clear up
patients described here with genetic some of this confusion and provide much-
REFERENCES
abnormalities in factor H (n = 5) or factor needed physiologic information supporting 1. Levy M, Gubler MC, Sich M et al. Immunopathology
I (n = 3) or with positive C3NeF activity the diagnosis of C3 glomerulopathy. Sethi of membranoproliferative glomerulonephritis
(n = 18)? One possible explanation is that et al. used three different screening tests of with subendothelial deposits (Type 1 MPGN).
Clin Immunol Immunopathol 1978; 10: 477–492.
these patients were previously misclassi- the alternative pathway in their cohort of 2. Habib R, Gubler M-C, Loirat C et al. Dense
fied as MPGN type I, akin to some patients C3GN: a hemolytic assay, an alternative deposit disease: a variant of membranopro-
liferative glomerulonephritis. Kidney Int 1975; 7:
in the American C3GN cohort, and that pathway functional assay, and levels of 204–215.
the immunoglobulin staining was trace serum membrane attack complex.8 In such 3. Strife CF, McEnery PT, McAdams AJ et al.
and inconsequential; the lack of central a small cohort, in which most patients Membranoproliferative glomerulonephritis
with disruption of the glomerular basement
review of all biopsies in this study, as the showed remarkable stability of disease membrane. Clin Nephrol 1977; 7: 65–72.
authors themselves acknowledge, is there- despite varied treatment regimens, it is 4. Appel GB, Cook HT, Hageman G et al.
fore a major limitation.7 Small amounts impossible to discern whether these mark- Membranoproliferative glomerulonephritis type
II (dense deposit disease): an update. J Am Soc
of immunoglobulin may become trapped ers of alternative pathway activity are linked Nephrol 2005; 16: 1392–1403.
in areas of sclerosis or accumulate in to outcomes. Such testing would likely have 5. Servais A, Fremeaux-Bacchi V, Lequintrec M
podocyte protein resorption droplets, been far more informative in the larger et al. Primary glomerulonephritis with isolated
C3 deposits: a new entity which shares common
confounding immunofluorescence inter- French cohort but was not performed.7 genetic risk factors with haemolytic uraemic
pretation. However, if we are to accept that Instead, levels of C3 and C4 were used as syndrome. J Med Genet 2007; 44: 193–199.
these cases truly have immunoglobulin baseline markers of complement activity, 6. Sethi S, Fervenza FC. Membranoproliferative
glomerulonephritis: pathogenetic heterogeneity
deposits alongside serologic evidence of which by themselves are substandard in and proposal for a new classification. Semin
alternative pathway dysregulation, should these complex diseases; not surprisingly, Nephrol 2011; 31: 341–348.
7. Servais A, Noël L-H, Roumenina LT et al. Acquired
we now consider these as yet another sub- neither low C3 ( < 600 mg/l) nor very low and genetic complement abnormalities play a
type of C3 glomerulopathy? These find- C3 ( < 200 mg/l) levels were predictive of critical role in dense deposit disease and other C3
ings suggest more commonality between renal outcomes.7 Wider access to the types glomerulopathies. Kidney Int 2012; 82: 454–463.
8. Sethi S, Fervenza FC, Zhang Y et al. C3
MPGN type I and C3 glomerulopathies of genetic and complement testing glomerulonephritis: clinicopathologic findings,
than previously recognized and raise the described in both studies should allow complement abnormalities, glomerular proteomic
question of whether patients with dys- more etiology-specific diagnosis. profile, treatment and follow-up. Kidney Int 2012;
82: 465–473.
regulated alternative complement path- Another provocative finding is the iden- 9. Zhang Y, Meyer NC, Wang K et al. Causes of alter-
way may not also develop disease-causing tification of both C3NeF and a genetic native pathway dysregulation in dense deposit
immune deposits containing immu- defect in the complement pathway in a disease. Clin J Am Soc Nephrol 2012; 7: 265–274.
10. Bao L, Haas M, Quigg RJ. Complement factor H
noglobulin and complement in the course proportion of patients in the French deficiency accelerates development of lupus
of antigen-driven immune responses. cohort: among 24 patients with an identi- nephritis. J Am Soc Nephrol 2011; 22: 285–295.
Such observations are consistent with fied mutation in a complement gene, 13 11. Gharavi AG, Kiryluk K, Choi M et al. Genome-wide
association study identifies susceptibility loci for
the predisposition to immune complex- also had detectable C3NeF.7 Why is there IgA nephropathy. Nat Genet 2011; 43: 321–327.
mediated lupus nephritis in MRL-lpr mice coexistence of inherited and acquired 12. Fremeaux-Bacchi V, Weiss L, Demouchy C et al.
Hypocomplementaemia of poststreptococcal
with genetic deletion of complement fac- abnormalities of the alternative comple- acute glomerulonephritis is associated with C3
tor H10 and the increased susceptibility to ment pathway in such cases? These num- nephritic factor [C3NeF] IgG autoantibody activity.
IgA nephropathy in people with muta- bers are difficult to ascribe to coincidence Nephrol Dial Transplant 1994; 9: 1747–1750.
Kidney International (2012) 82 381
You might also like
- A Doctor's 4-Step Program To Treat Autoimmune Disease: THE IMMUNE SYSTEM RECOVERY PLAN by Susan BlumDocument65 pagesA Doctor's 4-Step Program To Treat Autoimmune Disease: THE IMMUNE SYSTEM RECOVERY PLAN by Susan BlumSimon and Schuster85% (26)
- Robbins Questions Chp1-10Document28 pagesRobbins Questions Chp1-10verbatimmt100% (1)
- Advances in Immunology: I D C D PDocument12 pagesAdvances in Immunology: I D C D PDatulna Benito Mamaluba Jr.No ratings yet
- MD MCQ NewDocument109 pagesMD MCQ Newhimantha20059918100% (5)
- ImmunityDocument53 pagesImmunityDrSyeda RimaNo ratings yet
- Connective Tissue DZDocument1 pageConnective Tissue DZAndre GarciaNo ratings yet
- MIMS Abbreviation IndexDocument1 pageMIMS Abbreviation IndexBrian Harris100% (1)
- Antiphospholipid SyndromeDocument38 pagesAntiphospholipid SyndromeossamafoudaNo ratings yet
- RheumatologyDocument28 pagesRheumatologyOanaroxana Varsa100% (2)
- (Mackay) Autoimmune Disease OverviewDocument11 pages(Mackay) Autoimmune Disease OverviewrodtobingNo ratings yet
- Test For Mci ScreeningDocument43 pagesTest For Mci ScreeningGulamenasir AhmednasirwalaNo ratings yet
- Give Away CBQDocument26 pagesGive Away CBQGreggy Francisco Lara100% (4)
- Dermatological Diseases of The Nose and Ears - An Illustrated Guide - C. Baykal, K. Yazganoglu (Springer, 2010) WWDocument150 pagesDermatological Diseases of The Nose and Ears - An Illustrated Guide - C. Baykal, K. Yazganoglu (Springer, 2010) WWthanos bakourasNo ratings yet
- PIIS0031302523001691Document2 pagesPIIS0031302523001691regina stefaniNo ratings yet
- Medical Progress: Review ArticlesDocument12 pagesMedical Progress: Review ArticlesgibsonrajanNo ratings yet
- Membranous Nephropathy: From Models To Man: Review SeriesDocument8 pagesMembranous Nephropathy: From Models To Man: Review SeriesmmsNo ratings yet
- Pyoderma Gangrenosum: A Review: Cutaneous PathologyDocument11 pagesPyoderma Gangrenosum: A Review: Cutaneous PathologyBela RomanNo ratings yet
- 13 CR Lethal MidlineDocument3 pages13 CR Lethal MidlineSudhir BayyaNo ratings yet
- Zoltan Vajo, Clair A. Francomano, Douglas J. Wilkin: Printed in U.S.ADocument17 pagesZoltan Vajo, Clair A. Francomano, Douglas J. Wilkin: Printed in U.S.AAndy HongNo ratings yet
- Medical WagesDocument5 pagesMedical WagesnusyratNo ratings yet
- Advances in Molecular Pathology Into Brain Tumor DiajDocument29 pagesAdvances in Molecular Pathology Into Brain Tumor DiajAkshhata NarulkarNo ratings yet
- Update On Membranoproliferative GNDocument9 pagesUpdate On Membranoproliferative GNSalvador GoveaNo ratings yet
- Neutrophil Disorders and Their ManagementDocument14 pagesNeutrophil Disorders and Their Managementmeharalibhatti1No ratings yet
- Alzheimer's Disease-To Cure? From CauseDocument7 pagesAlzheimer's Disease-To Cure? From CauseamifideleNo ratings yet
- Membranoproliferative GlomerulonephritisDocument7 pagesMembranoproliferative GlomerulonephritisRobertNo ratings yet
- Granulomas in The Gastrointestinal Tract: Deciphering The Pandora 'S BoxDocument12 pagesGranulomas in The Gastrointestinal Tract: Deciphering The Pandora 'S BoxapowataNo ratings yet
- Aging Cell - 2014 - Linehan - Aging Impairs Peritoneal But Not Bone Marrow Derived Macrophage PhagocytosisDocument10 pagesAging Cell - 2014 - Linehan - Aging Impairs Peritoneal But Not Bone Marrow Derived Macrophage Phagocytosiszeemalbari3No ratings yet
- The M Protein of Group A Streptococcus Is A Key Virulence Factor and A Clinically Relevant Strain Identification MarkerDocument12 pagesThe M Protein of Group A Streptococcus Is A Key Virulence Factor and A Clinically Relevant Strain Identification MarkerEnockNo ratings yet
- Cerebral Malaria Immunopathology PDFDocument11 pagesCerebral Malaria Immunopathology PDFAurelia WetondieNo ratings yet
- Orsonneau 1989Document4 pagesOrsonneau 1989Joana BarbosaNo ratings yet
- GBM (The Terminator)Document3 pagesGBM (The Terminator)Cristhian Jossef Motta ZevallosNo ratings yet
- Genpath - Glomerular Diseases (Primary Glomerulopathies (Nephritic) )Document5 pagesGenpath - Glomerular Diseases (Primary Glomerulopathies (Nephritic) )Julie Gemarino LumasagNo ratings yet
- 1.4 Amyloidosis Lecture Slides - 2022-23Document42 pages1.4 Amyloidosis Lecture Slides - 2022-23dlee021129No ratings yet
- IgA NephropathyDocument5 pagesIgA NephropathyLara Patricia TamsiNo ratings yet
- 2000 Annual ReviewsDocument49 pages2000 Annual Reviewstkovats.lopes3No ratings yet
- AmylopidPolymorphism - Journal of Internal Medicine - 2018 - F Ndrich - Amyloid Fibril Polymorphism A Challenge For Molecular Imaging and TherapyDocument20 pagesAmylopidPolymorphism - Journal of Internal Medicine - 2018 - F Ndrich - Amyloid Fibril Polymorphism A Challenge For Molecular Imaging and TherapyAmbra SalamandraNo ratings yet
- Mud I Gonda 2013Document3 pagesMud I Gonda 2013Febyan AbotNo ratings yet
- Financial Support: Necrotic Xanthogranuloma With Disseminated Annular LesionsDocument3 pagesFinancial Support: Necrotic Xanthogranuloma With Disseminated Annular LesionsSango AyraNo ratings yet
- Bioethical Aspects in Type I NeurofibromatosisDocument4 pagesBioethical Aspects in Type I NeurofibromatosisRomana VulturarNo ratings yet
- Nephrotic Syndrome After Treatment With PamidronateDocument5 pagesNephrotic Syndrome After Treatment With PamidronateTim Engineer HD RSUD Dr. SoetomoNo ratings yet
- Ashraf Et Al 2015Document8 pagesAshraf Et Al 2015lucaNo ratings yet
- Glomerulonefritis ComplementoDocument10 pagesGlomerulonefritis ComplementoPaola ZuluagaNo ratings yet
- Renal Biopsy Pathology 2011Document10 pagesRenal Biopsy Pathology 2011AnamNo ratings yet
- s03 - Fibrosis From Mechanisms To MedicineDocument12 pagess03 - Fibrosis From Mechanisms To MedicineWilly CaballeroNo ratings yet
- Nephritic SyndromeDocument15 pagesNephritic Syndrome76q88b4yrxNo ratings yet
- 6137 20449 1 PB PDFDocument6 pages6137 20449 1 PB PDFNaima TariqNo ratings yet
- Interstitial Fluid Flow Induces Myofibroblast Differentiation and Collagen Alignment in VitroDocument9 pagesInterstitial Fluid Flow Induces Myofibroblast Differentiation and Collagen Alignment in VitroPedro FonsecaNo ratings yet
- Organising PneumoniaDocument12 pagesOrganising PneumoniaA. RaufNo ratings yet
- Membranous GNDocument12 pagesMembranous GNdr belaNo ratings yet
- NIH Public Access: Author ManuscriptDocument28 pagesNIH Public Access: Author ManuscriptAlfonso LemaNo ratings yet
- Articol Clonare CFTRDocument1 pageArticol Clonare CFTRPancu CristianaNo ratings yet
- Rejeksi AllograftDocument10 pagesRejeksi AllograftIndra kusuma mardiaNo ratings yet
- The de Finition of Primary and Secondary Glioblastoma: ReviewDocument9 pagesThe de Finition of Primary and Secondary Glioblastoma: Reviewalexandre06frNo ratings yet
- Ameratunga 2000Document3 pagesAmeratunga 2000pipilepew14No ratings yet
- ORENSTEIN 2002 - Cystic Fibrosis - A 2002 UpdateDocument9 pagesORENSTEIN 2002 - Cystic Fibrosis - A 2002 UpdateRafael JustinoNo ratings yet
- Skin Barrier Defects in AtopicDocument20 pagesSkin Barrier Defects in AtopicDaniel SatyoNo ratings yet
- Ni Hms 281302Document9 pagesNi Hms 281302Aline CristinaNo ratings yet
- Granulomatous Diseases of Lung PDFDocument24 pagesGranulomatous Diseases of Lung PDFBasit RafiqiNo ratings yet
- The Evolving Landscape of Primary Immunodeficiencies: EditorialDocument2 pagesThe Evolving Landscape of Primary Immunodeficiencies: EditorialEnrico Emilio LatorracaNo ratings yet
- Modifications Epigenetiques Et Maladies Humaines (Translate PDFDocument26 pagesModifications Epigenetiques Et Maladies Humaines (Translate PDFAkadiri AdjibadéNo ratings yet
- Management of Gastric Neuroendocrine Tumors A ReviewDocument22 pagesManagement of Gastric Neuroendocrine Tumors A ReviewROSARIO PAZ MILLÁNNo ratings yet
- Inmunodeficiencia Variable ComunDocument6 pagesInmunodeficiencia Variable ComunItzel AraujoNo ratings yet
- The Paradox of Tumor-Associated Neutrophils Fueling Tumor Growth With Cytotoxic SubstancesDocument7 pagesThe Paradox of Tumor-Associated Neutrophils Fueling Tumor Growth With Cytotoxic SubstancesPilar AufrastoNo ratings yet
- Nejm 2013 Nefropatía IgaDocument13 pagesNejm 2013 Nefropatía Igacesar gonzalezNo ratings yet
- Solga2015 PDFDocument13 pagesSolga2015 PDFPaige MunroeNo ratings yet
- The Immune Response To Infection With Treponema Pallidum, The Stealth PathogenDocument8 pagesThe Immune Response To Infection With Treponema Pallidum, The Stealth Pathogenhazem alzedNo ratings yet
- Review: Phagocytic Clearance in NeurodegenerationDocument13 pagesReview: Phagocytic Clearance in NeurodegenerationEric DyneNo ratings yet
- Transverse Myelitis: Clinical PracticeDocument9 pagesTransverse Myelitis: Clinical PracticearnabNo ratings yet
- Kotlyar 2020Document16 pagesKotlyar 2020Merab KvintradzeNo ratings yet
- CKD - Molecular Profiling Reveals A Common Metabolic Signature of Tissue FibrosisDocument27 pagesCKD - Molecular Profiling Reveals A Common Metabolic Signature of Tissue FibrosisCher IshNo ratings yet
- Biochemical and Molecular Aspects of Selected Cancers: Volume 2From EverandBiochemical and Molecular Aspects of Selected Cancers: Volume 2Thomas G. Pretlow IINo ratings yet
- WLD Disease Perceptions Society Views Infographic 070417Document1 pageWLD Disease Perceptions Society Views Infographic 070417Pslem SelangorNo ratings yet
- Systemic Lupus ErythematosusDocument13 pagesSystemic Lupus ErythematosusGrace RoselinyNo ratings yet
- Antiphospholipid Antibody Syndrome: Pathogenesis, Diagnosis, and Management in PregnancyDocument5 pagesAntiphospholipid Antibody Syndrome: Pathogenesis, Diagnosis, and Management in PregnancyRaul DoctoNo ratings yet
- Ncp-For-Sle-Fatigue-And-Pain EDITEDDocument4 pagesNcp-For-Sle-Fatigue-And-Pain EDITEDJordz PlaciNo ratings yet
- OB-GYN QuestionsDocument10 pagesOB-GYN QuestionsArianne Joy C. TamarayNo ratings yet
- Student Project: Cutaneous Discoid LupusDocument28 pagesStudent Project: Cutaneous Discoid LupusFaradilla Novita AnggreiniNo ratings yet
- Lupus ErythematosusDocument19 pagesLupus ErythematosusLakshya J Basumatary100% (2)
- GOKU-Rheumatology-SLE-OTHER-Connective Tissue Diseases and VasculitisDocument30 pagesGOKU-Rheumatology-SLE-OTHER-Connective Tissue Diseases and VasculitisCas BuNo ratings yet
- CH 19 Nursing Care of Patients With Immune System DisordersDocument2 pagesCH 19 Nursing Care of Patients With Immune System DisordersZachary T Hall0% (1)
- Obstetrics and Gynecology NotesDocument73 pagesObstetrics and Gynecology NotesHaspreet GillNo ratings yet
- Fibromyalgia DR, Isti PDFDocument40 pagesFibromyalgia DR, Isti PDFradiologi igdNo ratings yet
- Diagnostic Approach in Patients With Arthritis PDFDocument38 pagesDiagnostic Approach in Patients With Arthritis PDFPowool LalaNo ratings yet
- The Sydney Classification Criteria For Definite Antiphospholipid SyndromeDocument7 pagesThe Sydney Classification Criteria For Definite Antiphospholipid SyndromechereliadinarNo ratings yet
- Annular LesionsDocument8 pagesAnnular LesionshpmcentreNo ratings yet
- Lupus ppt-1Document33 pagesLupus ppt-1api-282231236No ratings yet
- Jurnal SLEDocument7 pagesJurnal SLEDevinta NauraNo ratings yet
- Lupus - Client Brochure Rdramirez v2Document4 pagesLupus - Client Brochure Rdramirez v2api-437843157No ratings yet
- Antiphospholipid Antibody Syndrome The.2 PDFDocument5 pagesAntiphospholipid Antibody Syndrome The.2 PDFJunita Nelly Esther JosephNo ratings yet
- BJD Methotrxate PDFDocument22 pagesBJD Methotrxate PDFSoumya MarangadNo ratings yet