0% found this document useful (0 votes)
1K views38 pagesThe Canadian Triage and Acuity Scale: Education Manual: Version 2.5, 2012
triase
Uploaded by
abdullahmushlihCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
1K views38 pagesThe Canadian Triage and Acuity Scale: Education Manual: Version 2.5, 2012
triase
Uploaded by
abdullahmushlihCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
- Introduction
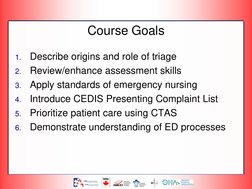
- Course Goals
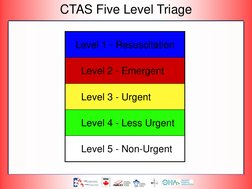
- CTAS Five Level Triage
- Module 1: Fundamentals of Triage
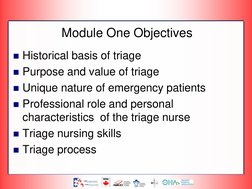
- Module One Objectives
- Evolution of Triage
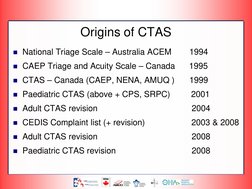
- Origins of CTAS
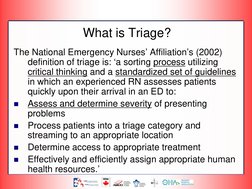
- What is Triage?
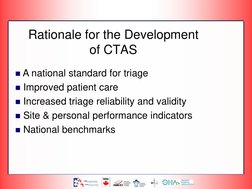
- Rationale for the Development of CTAS
- The Benefits of Triage
- Avoiding Triage as 'Access Block'
- Triaging with Overcrowding
- Emergency Patients are Unique
- Role of Triage Nurse
- Triage Nursing
- Triage Nursing Skills
- The Process of Triage
- Triage Documentation
- Module One - Review
- References