Professional Documents
Culture Documents
Referat Iktiosis Pembahasan
Uploaded by
Patih GajahmadaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Referat Iktiosis Pembahasan
Uploaded by
Patih GajahmadaCopyright:
Available Formats
Critical Appraisal for Therapy Articles
THERAPY STUDY: Are the results of the trial valid? (Internal Validity)
What question did the study ask?
Patients – wanita hamil dengan risiko tinggi preeklamsi
Intervention – gabungan dari L-Arginine dengan vitamin antioksidan
Comparison – vitamin antioksidan
- placebo
Outcome(s) – L-Arginine menurunkan angka kejadian preeklamsi
1a. R- Was the assignment of patients to treatments randomised?
What is best? Where do I find the information?
Centralised computer randomisation is ideal and often The Methods should tell you how patients were allocated
used in multi-centred trials. Smaller trials may use an to groups and whether or not randomisation was
independent person (e.g, the hospital pharmacy) to concealed.
“police” the randomization.
This paper: Yes No Unclear
Comment: pada penelitian ini penulis menjelaskan pengambilan sampel wanita hamil dengan
risiko tinggi preeklamsi di ambil secara acak dengan cara staff dari departemen Obstetri
mereview pasien yang memiliki kualitas untuk penelitian. Pasien akan menerima satu dari
treatment tersebut secara acak. Investigator mengacak menggunakan centralised computer
randomisation.
1b. R- Were the groups similar at the start of the trial?
What is best? Where do I find the information?
If the randomisation process worked (that is, achieved The Results should have a table of "Baseline
comparable groups) the groups should be similar. The Characteristics" comparing the randomized groups on a
more similar the groups the better it is. number of variables that could affect the outcome (ie. age,
There should be some indication of whether differences risk factors etc). If not, there may be a description of group
between groups are statistically significant (ie. p values). similarity in the first paragraphs of the Results section.
This paper: Yes No Unclear
Comment:pada hasil peenlitian, peneliti telah menampilkan table Karakteritik dasar pasien
dari tiga kelompok yang masing-masing memiliki P = > 0,05 artinya ke-3 kelompok itu memiliki
karakteristik yang sama
2a. A – Aside from the allocated treatment, were groups treated equally?
What is best? Where do I find the information?
Apart from the intervention the patients in the different Look in the Methods section for the follow-up schedule,
groups should be treated the same, eg., additional and permitted additional treatments, etc and in Results for
treatments or tests. actual use.
This paper: Yes No Unclear
Comment: pada penelitian ini participant dijadwalkan untuk melakukan klinikal follow up setiap
3-4 minggu, antara lain mengukur tekanan arteri, pengambilan sampel darah 10 ml, menampung
urin 24 jam sehari sebelum follow up, pasien diminta mencatat konsumsi bars, dan peneliti
juga memberikan edukasi tentang nutrisi selama kehamilan pada semua partisipant
2b. A – Were all patients who entered the trial accounted for? – and were
they analysed in the groups to which they were randomised?
What is best? Where do I find the information?
Losses to follow-up should be minimal – preferably less The Results section should say how many patients were
than 20%. However, if few patients have the outcome of 1andomised (eg., Baseline Characteristics table) and how
interest, then even small losses to follow-up can bias the many patients were actually included in the analysis. You
results. Patients should also be analysed in the groups to will need to read the results section to clarify the number
which they were randomised – ‘intention-to-treat analysis’ . and reason for losses to follow-up.
University of Oxford, 2005 1
Critical Appraisal for Therapy Articles
This paper: Yes No Unclear
Comment: pada penelitian ini peneliti mengambil partisipan sebanyak 696 wanita. Partisipan
yang memenuhi criteria inklusi sebanyak 672 dan yang memenuhi criteria eksklusi sebanyak
24 partisipant. Dari clinical follow up, kurang dari 5% yang tidak terlewat untung dikunjungi
dari 3 grup tersebut.
3. M - Were measures objective or were the patients and clinicians kept
“blind” to which treatment was being received?
What is best? Where do I find the information?
It is ideal if the study is ‘double-blinded’ – that is, both First, look in the Methods section to see if there is some
patients and investigators are unaware of treatment mention of masking of treatments, eg., placebos with the
allocation. If the outcome is objective (eg., death) then same appearance or sham therapy. Second, the
blinding is less critical. If the outcome is subjective (eg., Methods section should describe how the outcome was
symptoms or function) then blinding of the outcome assessed and whether the assessor/s were aware of the
assessor is critical. patients' treatment.
This paper: Yes No Unclear
Comment: pada penelitian ini peneliti menjelaskan bahwa Pasien tidak mengetahui dan tidak
bisa membedakan isi dari amplop tersebut karena penampilannya sama dan tidak ada
perbedaan rasa. Hanya investigator utama yang mengetahui kode dari masing-masing amplop
tertutup yang berisi treatment tersebut.
University of Oxford, 2005 2
Critical Appraisal for Therapy Articles
What were the results?
1. How large was the treatment effect?
Most often results are presented as dichotomous outcomes (yes or not outcomes that happen or don't happen) and can
include such outcomes as cancer recurrence, myocardial infarction and death. Consider a study in which 15% (0.15) of
the control group died and 10% (0.10) of the treatment group died after 2 years of treatment. The results can be
expressed in many ways as shown below.
What is the measure? What does it mean?
Relative Risk (RR) = risk of the outcome in the The relative risk tells us how many times more likely it is that
treatment group / risk of the outcome in the control an event will occur in the treatment group relative to the control
group. group. An RR of 1 means that there is no difference between the
two groups thus, the treatment had no effect. An RR < 1 means
that the treatment decreases the risk of the outcome. An RR > 1
means that the treatment increased the risk of the outcome.
In our example, the RR = 0.10/0.15 = 0.67 Since the RR < 1, the treatment decreases the risk of death.
Absolute Risk Reduction (ARR) = risk of the The absolute risk reduction tells us the absolute difference in the
outcome in the control group - risk of the outcome rates of events between the two groups and gives an indication
in the treatment group. This is also known as the of the baseline risk and treatment effect. An ARR of 0 means
absolute risk difference. that there is no difference between the two groups thus, the
treatment had no effect.
In our example, the ARR = 0.15 - 0.10 = 0.05 or 5% The absolute benefit of treatment is a 5% reduction in the death
rate.
Relative Risk Reduction (RRR) = absolute risk The relative risk reduction is the complement of the RR and is
reduction / risk of the outcome in the control group. probably the most commonly reported measure of treatment
An alternative way to calculate the RRR is to effects. It tells us the reduction in the rate of the outcome in the
subtract the RR from 1 (eg. RRR = 1 - RR) treatment group relative to that in the control group.
In our example, the RRR = 0.05/0.15 = 0.33 or 33% The treatment reduced the risk of death by 33% relative to that
Or RRR = 1 - 0.67 = 0.33 or 33% occurring in the control group.
Number Needed to Treat (NNT) = inverse of the The number needed to treat represents the number of patients
ARR and is calculated as 1 / ARR. we need to treat with the experimental therapy in order to prevent
1 bad outcome and incorporates the duration of treatment.
Clinical significance can be determined to some extent by looking
at the NNTs, but also by weighing the NNTs against any harms or
adverse effects (NNHs) of therapy.
In our example, the NNT = 1/ 0.05 = 20 We would need to treat 20 people for 2 years in order to prevent
1 death.
2. How precise was the estimate of the treatment effect?
The true risk of the outcome in the population is not known and the best we can do is estimate the true risk based on the
sample of patients in the trial. This estimate is called the point estimate. We can gauge how close this estimate is to
the true value by looking at the confidence intervals (CI) for each estimate. If the confidence interval is fairly narrow then
we can be confident that our point estimate is a precise reflection of the population value. The confidence interval also
provides us with information about the statistical significance of the result. If the value corresponding to no effect falls
outside the 95% confidence interval then the result is statistically significant at the 0.05 level. If the confidence interval
includes the value corresponding to no effect then the results are not statistically significant.
1. pada hasil penelitian ini didapatkan bahwa L-arginine+vitamin lebih menurunkan
resiko pre-eklamsia/eclamsia dibanding dengan placebo dilihat dari ARR 0,17
(ARR≠0) dan RR 0,42 (RR<1). L-arginine+vitamin dapat menurunkan resiko pre-
eklamsia/eclamsia sebanyak 17% .
University of Oxford, 2005 3
Critical Appraisal for Therapy Articles
Vitamins lebih menurunkan resiko pre-eklamsia/eclamsia dibanding dengan placebo
dilihat dari ARR 0,07 (ARR≠0) dan RR 0,74 (RR<1). Vitamin dapat menurunkan
resiko pre-eklamsia/eclamsia sebanyak 7%.
Sedangkan L-arginine+vitamin lebih menurunkan resiko pre-eklamsia/eclamsia
dibanding dengan vitamin dilihat dari ARR 0,09 (ARR≠0) dan RR 0,56 (RR<1). L-
arginine+vitamin dapat menurunkan resiko pre-eklamsia/eclamsia sebanyak 9% .
2. pada penelitian ini didapatkan perbandingan L-arginine+vitamin dengan placebo
memiliki hasil yang signifikan dengan p value 0,001 (P<0,05) dan 95% confidence
intervals (CI) 0,28 sampai 0,62. Sehingga pemberian L-arginine+vitamin berefek
terhadap penurunan kejadian pre-eclamsia/eclamsia dibanding dengan placebo.
perbandingan vitamin dengan placebo memiliki hasil yang tidak signifikan dengan p
value 0,52 (P>0,05) dan 95% confidence intervals (CI) 0,54 sampai 1,02. Sehingga
pemberian vitamin tidak berefek terhadap penurunan kejadian pre-
eclamsia/eclamsia dibanding dengan placebo.
perbandingan L-arginine+vitamin dengan vitamin memiliki hasil yang signifikan dengan
p value 0,004 (P<0,05) dan 95% confidence intervals (CI) 0,37 sampai 0,85.
Sehingga pemberian L-arginine+vitamin berefek terhadap penurunan kejadian pre-
eclamsia/eclamsia dibanding dengan vitamin.
Will the results help me in caring for my patient? (ExternalValidity/Applicability)
The questions that you should ask before you decide to apply the results of the study to your patient are:
Is my patient so different to those in the study that the results cannot apply?
Is the treatment feasible in my setting?
Will the potential benefits of treatment outweigh the potential harms of treatment for my patient?
University of Oxford, 2005 4
You might also like
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyFrom EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyRating: 1 out of 5 stars1/5 (1)
- Worksheet Appraisal AZALEADocument5 pagesWorksheet Appraisal AZALEAArini NurlelaNo ratings yet
- Centralised Computer Randomisation Is: Critical Appraisal For Therapy ArticlesDocument4 pagesCentralised Computer Randomisation Is: Critical Appraisal For Therapy ArticleshadzaliegNo ratings yet
- THERAPY STUDY RESULTS VALIDDocument4 pagesTHERAPY STUDY RESULTS VALIDAhmad BukhariNo ratings yet
- RCT Appraisal Sheets 2005 English-1 1Document5 pagesRCT Appraisal Sheets 2005 English-1 1api-479716004No ratings yet
- RCT Appraisal Sheets 2005 EnglishDocument4 pagesRCT Appraisal Sheets 2005 EnglishAmanda SoebadiNo ratings yet
- Worksheet Therapy-CebmDocument3 pagesWorksheet Therapy-Cebmteddy sNo ratings yet
- Therapy Studies What Question Did The Study Ask?Document2 pagesTherapy Studies What Question Did The Study Ask?Apt RiskaNo ratings yet
- CRITICAL APPRAISAL Mas WikoDocument10 pagesCRITICAL APPRAISAL Mas WikoEliataMariaMahanaimNo ratings yet
- Patients - Intervention - Comparison - Outcome(s)Document3 pagesPatients - Intervention - Comparison - Outcome(s)Intan SetyadewiNo ratings yet
- Patients - Intervention - Comparison - Outcome(s) - Knowledge GapDocument4 pagesPatients - Intervention - Comparison - Outcome(s) - Knowledge GapAmal NajiNo ratings yet
- RCT Appraisal Sheets 2005 EnglishDocument2 pagesRCT Appraisal Sheets 2005 EnglishF NNo ratings yet
- Worksheet Therapy CebmDocument3 pagesWorksheet Therapy Cebmandynightmare97No ratings yet
- RCT Appraisal Sheets 2005 English-2Document6 pagesRCT Appraisal Sheets 2005 English-2tsyrahmaniNo ratings yet
- Critical Appraisal Jurnal Asam Traneksamat Pada MelasmaDocument4 pagesCritical Appraisal Jurnal Asam Traneksamat Pada MelasmaMsrirrrNo ratings yet
- (OBAT CINA) CAT TherapyDocument6 pages(OBAT CINA) CAT TherapyArga PRNo ratings yet
- Tugas Farepid - CA - 198114152Document11 pagesTugas Farepid - CA - 198114152JeanieNo ratings yet
- Critical Appraisal for Therapy ArticlesDocument4 pagesCritical Appraisal for Therapy ArticlesMahardhika AcintyaNo ratings yet
- Critical Appraisal For Therapy Articles: Are The Results of The Trial Valid? (Internal Validity)Document4 pagesCritical Appraisal For Therapy Articles: Are The Results of The Trial Valid? (Internal Validity)Putri Widya AndiniNo ratings yet
- Randomised: Differences Between Groups Are Statistically Significant P ValuesDocument6 pagesRandomised: Differences Between Groups Are Statistically Significant P ValuesArga PRNo ratings yet
- Critical Therapy Study ResultsDocument4 pagesCritical Therapy Study ResultsAinur 'iin' RahmahNo ratings yet
- Patients - Intervention - Comparison - Outcome(s)Document4 pagesPatients - Intervention - Comparison - Outcome(s)sahirbuleNo ratings yet
- Critical ApraisalDocument4 pagesCritical Apraisalfauziah qurrota a'yuniNo ratings yet
- Kritisi Artikel - Ni Nengah Susilawati - 152191105 - BDocument5 pagesKritisi Artikel - Ni Nengah Susilawati - 152191105 - BShilaNo ratings yet
- Critical Appraisal TafaDocument7 pagesCritical Appraisal TafaFabric FameNo ratings yet
- Critical Appraisal of Therapy Study ValidityDocument3 pagesCritical Appraisal of Therapy Study ValidityOtty Mitha OctrizaNo ratings yet
- Critical Appraisal for Therapy Study ResultsDocument3 pagesCritical Appraisal for Therapy Study ResultsVeysusanNo ratings yet
- Telaah Kritis Jurnal 2Document9 pagesTelaah Kritis Jurnal 2Ayu Vitha ViginiaNo ratings yet
- CA Therapy Artikel 09Document5 pagesCA Therapy Artikel 09Christiana TrijayantiNo ratings yet
- Critical Appraisal for Therapy Studies WorksheetDocument2 pagesCritical Appraisal for Therapy Studies WorksheetAdwin AlamsyaputraNo ratings yet
- Worksheet Therapy CebmDocument5 pagesWorksheet Therapy CebmZulfan RifqiawanNo ratings yet
- C - II - 3 - Critical AppraisalDocument10 pagesC - II - 3 - Critical AppraisalWahyu NandaNo ratings yet
- Crit AppDocument5 pagesCrit AppdikkaNo ratings yet
- EBM Dan Critical AppraisalDocument7 pagesEBM Dan Critical AppraisalNovia Ariani DewiNo ratings yet
- Therapystudy: Are The Results of The Trial Valid? (Internal Validity)Document6 pagesTherapystudy: Are The Results of The Trial Valid? (Internal Validity)Sinta AgustinaNo ratings yet
- Presentation On TherapyDocument21 pagesPresentation On TherapyMarjorie CepeNo ratings yet
- Anesthesiologists (ASA) I: THERAPY STUDY: Are The Results of The Trial Valid? (Internal Validity)Document4 pagesAnesthesiologists (ASA) I: THERAPY STUDY: Are The Results of The Trial Valid? (Internal Validity)Sandra Lydiayana Aisyah AzharNo ratings yet
- Critical Appraisal Checklist For An Article On Treatment or PreventionDocument4 pagesCritical Appraisal Checklist For An Article On Treatment or PreventionSaina AbasNo ratings yet
- Critical Appraisal Checklist For An Article OnDocument4 pagesCritical Appraisal Checklist For An Article OnTiaz DiniutamiNo ratings yet
- Critical Appraisal Therapy Study by DR BhismaDocument28 pagesCritical Appraisal Therapy Study by DR BhismaAhmadAfiyyuddinNo ratings yet
- Angel Yudiakristi - Praktikum 5Document10 pagesAngel Yudiakristi - Praktikum 5Angel MaharaniNo ratings yet
- Therapystudy: Are The Results of The Trial Valid? (Internal Validity)Document10 pagesTherapystudy: Are The Results of The Trial Valid? (Internal Validity)WiraNo ratings yet
- RCT+Appraisal+sheets. TherapyDocument2 pagesRCT+Appraisal+sheets. Therapydian_c87No ratings yet
- Checklist RCTDocument5 pagesChecklist RCTFajar SukmajayaNo ratings yet
- Laporan Resmi Praktikum Pharmaceutical Kardio Endokrin Pertemuan V Critical Appraisal (Ebm)Document16 pagesLaporan Resmi Praktikum Pharmaceutical Kardio Endokrin Pertemuan V Critical Appraisal (Ebm)evangeline keisha annabelNo ratings yet
- Critical Appraisal of Articles On TherapyDocument46 pagesCritical Appraisal of Articles On TherapyAditya Rachman Van Der ArjunaqueeNo ratings yet
- Twice Weekly FluticasoneDocument4 pagesTwice Weekly FluticasoneAudrey GillNo ratings yet
- A List A Statistical Definition For The CICM Fellowship ExamDocument5 pagesA List A Statistical Definition For The CICM Fellowship ExamSimon WongNo ratings yet
- EBM Worksheets (Therapy, Diagnosis, Prognosis, Economic, Guideline, Decision Making)Document15 pagesEBM Worksheets (Therapy, Diagnosis, Prognosis, Economic, Guideline, Decision Making)Soffatul AzizahNo ratings yet
- Table 2A Critical Appraisal Vaccine Therapy EfficacyDocument10 pagesTable 2A Critical Appraisal Vaccine Therapy Efficacy7CANTIKA PRAMESWARI HANANTONo ratings yet
- Critical Appraisal of TherapyDocument34 pagesCritical Appraisal of Therapyapi-19733840No ratings yet
- Make A NewSenin 26 Januari 2015 EBM GLOSARY Dr. Akhmad EdiDocument12 pagesMake A NewSenin 26 Januari 2015 EBM GLOSARY Dr. Akhmad EdinaotonaoiNo ratings yet
- Evidence-Based Medicine Therapy: Dr. Dr. Rina Amelia, MARS Departemen Kedokteran Komunitas FK USUDocument40 pagesEvidence-Based Medicine Therapy: Dr. Dr. Rina Amelia, MARS Departemen Kedokteran Komunitas FK USUSamuel TanNo ratings yet
- Evidence-Based Medicine Therapy: Dr. Rina Amelia, MARSDocument43 pagesEvidence-Based Medicine Therapy: Dr. Rina Amelia, MARSRezky IlhamNo ratings yet
- Confidence Intervals II AJPDocument5 pagesConfidence Intervals II AJPJu ChangNo ratings yet
- Association MeasurementDocument5 pagesAssociation Measurementnva1995No ratings yet
- "Evidence-Based Medicine" TherapyDocument54 pages"Evidence-Based Medicine" TherapyRuthra Devi NarayanasamyNo ratings yet
- Therapy - Siti Setiati Evidence Based MedicineDocument33 pagesTherapy - Siti Setiati Evidence Based MedicinejoeNo ratings yet
- Appraising Evidence for Therapy Articles Using PICO, Validity, Applicability & NNTDocument5 pagesAppraising Evidence for Therapy Articles Using PICO, Validity, Applicability & NNTMike CabotageNo ratings yet
- Jurnal Mas Za PDFDocument9 pagesJurnal Mas Za PDFPatih GajahmadaNo ratings yet
- Jurnal Mas Za PDFDocument9 pagesJurnal Mas Za PDFPatih GajahmadaNo ratings yet
- Jurnal 8 LMBRDocument8 pagesJurnal 8 LMBRDadang SyarieffidayatNo ratings yet
- Depres IDocument8 pagesDepres Ikiller childNo ratings yet
- Jurnal 8 LMBRDocument8 pagesJurnal 8 LMBRDadang SyarieffidayatNo ratings yet
- Nutrients 08 00751Document14 pagesNutrients 08 00751Patih GajahmadaNo ratings yet
- Depres IDocument8 pagesDepres Ikiller childNo ratings yet
- Nutrients 08 00751Document14 pagesNutrients 08 00751Patih GajahmadaNo ratings yet
- 2 RCT+Appraisal+sheets 2005Document13 pages2 RCT+Appraisal+sheets 2005Patih GajahmadaNo ratings yet
- ECT Buat Bipolar PDFDocument8 pagesECT Buat Bipolar PDFPatih GajahmadaNo ratings yet
- Nutrients: Vitamin D and Age-Related Macular DegenerationDocument15 pagesNutrients: Vitamin D and Age-Related Macular DegenerationPatih GajahmadaNo ratings yet
- Nutrients 08 00751Document14 pagesNutrients 08 00751Patih GajahmadaNo ratings yet
- Jurnal 8 LMBRDocument8 pagesJurnal 8 LMBRDadang SyarieffidayatNo ratings yet
- Faring It IsDocument8 pagesFaring It IsMuhammad sukronNo ratings yet
- Testing For Helicobacter Pylori Infection - Validation and Diagnostic Yield of A Near Patient Test in Primary Care PDFDocument4 pagesTesting For Helicobacter Pylori Infection - Validation and Diagnostic Yield of A Near Patient Test in Primary Care PDFminiwhiteyNo ratings yet
- Referat Iktiosis PembahasanDocument4 pagesReferat Iktiosis PembahasanPatih GajahmadaNo ratings yet
- Cover Journal ReadingDocument1 pageCover Journal ReadingPatih GajahmadaNo ratings yet
- 2 Dejc16-258Document12 pages2 Dejc16-258Patih GajahmadaNo ratings yet
- Jadwal Jaga Harian KOAS OBGYN FK UNIMUS RSUD Tugurejo SemarangDocument1 pageJadwal Jaga Harian KOAS OBGYN FK UNIMUS RSUD Tugurejo SemarangPatih GajahmadaNo ratings yet
- Jurnal Anestesi Alfan BENZODIAZEPINESDocument4 pagesJurnal Anestesi Alfan BENZODIAZEPINESPatih GajahmadaNo ratings yet
- Jurnal Mas Za PDFDocument9 pagesJurnal Mas Za PDFPatih GajahmadaNo ratings yet
- Lamp 12 Media Edukasi PosterDocument1 pageLamp 12 Media Edukasi PosterPatih GajahmadaNo ratings yet
- ShoppingDocument1 pageShoppingPatih GajahmadaNo ratings yet
- Jurnal Mas Za PDFDocument9 pagesJurnal Mas Za PDFPatih GajahmadaNo ratings yet
- Essential Nutrition Actions PDFDocument144 pagesEssential Nutrition Actions PDFAmany MokhtarNo ratings yet
- Bahasa Arab Sekitar Kamar MandiDocument2 pagesBahasa Arab Sekitar Kamar MandiRizky FebrianNo ratings yet
- SITXFSA001 - Written AssessmentDocument15 pagesSITXFSA001 - Written Assessmenthazem khudairNo ratings yet
- Biorisk Amp ModelDocument6 pagesBiorisk Amp ModelJennifer Santos100% (1)
- Rhea TestDocument3 pagesRhea Testerma090308No ratings yet
- Measles: A Highly Contagious Viral DiseaseDocument30 pagesMeasles: A Highly Contagious Viral DiseaseEarl Mel Dustin LaoNo ratings yet
- Epid 1.1Document194 pagesEpid 1.1devtarioNo ratings yet
- Hospital Waste ManagementDocument40 pagesHospital Waste Managementamir khanNo ratings yet
- Polio EradicationDocument9 pagesPolio Eradicationsobia salmanNo ratings yet
- MDH Order - Food Service EstablishmentsDocument2 pagesMDH Order - Food Service EstablishmentsDavid M. Higgins IINo ratings yet
- Cultural Competence or Cultural Humility Moving Beyond The DebateDocument4 pagesCultural Competence or Cultural Humility Moving Beyond The DebateEstela MedinaNo ratings yet
- Artificial Insemination - Docx1Document3 pagesArtificial Insemination - Docx1carol ann saliseNo ratings yet
- Chapter 1. Physical Activity and ExerciseDocument46 pagesChapter 1. Physical Activity and ExerciseYousef BobadillaNo ratings yet
- Sudan: African Medical Students AssociationDocument18 pagesSudan: African Medical Students AssociationAfrican Medical Students Association at IUANo ratings yet
- List of Colleges and Courses ReportDocument78 pagesList of Colleges and Courses Reportnptel nptelNo ratings yet
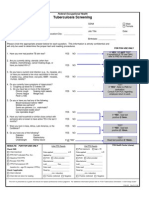
- FOH-25 Tuberculosis Screening (M.25)Document1 pageFOH-25 Tuberculosis Screening (M.25)Maria CabañasNo ratings yet
- Prevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDDocument7 pagesPrevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDMusainah FeisalNo ratings yet
- Health: Quarter 4 - Module 3: Ways To Prevent Non-Communicable DiseasesDocument26 pagesHealth: Quarter 4 - Module 3: Ways To Prevent Non-Communicable DiseaseskiahjessieNo ratings yet
- National Ten-Year Cancer Control Strategy - 2021-2025 RoadmapDocument76 pagesNational Ten-Year Cancer Control Strategy - 2021-2025 RoadmapWac GunarathnaNo ratings yet
- Gynaecology GP Study Afternoon MR Rehan SalimDocument36 pagesGynaecology GP Study Afternoon MR Rehan SalimFrida AtallahNo ratings yet
- Activated Sludge Process: Nelson Pynadathu Rumjit (13MEE0006)Document22 pagesActivated Sludge Process: Nelson Pynadathu Rumjit (13MEE0006)dhanushNo ratings yet
- H1N1 Swine FlupptDocument28 pagesH1N1 Swine FlupptDr. Hesham Zaatar100% (1)
- Clinical Trial Details (PDF Generation Date:-Wed, 05 Jul 2023 16:49:36 GMT)Document3 pagesClinical Trial Details (PDF Generation Date:-Wed, 05 Jul 2023 16:49:36 GMT)BALTAZAR OTTONELLONo ratings yet
- Food Safety Practices Among Vendors in Capaoay San Jacinto PangasinanDocument4 pagesFood Safety Practices Among Vendors in Capaoay San Jacinto PangasinanPatricia Mae SabadoNo ratings yet
- pID - CA OVARIUMDocument21 pagespID - CA OVARIUMMaria TifaniNo ratings yet
- NURSING RESEARCH-Questionnaire On Sexually Transmitted InfectionsDocument3 pagesNURSING RESEARCH-Questionnaire On Sexually Transmitted InfectionsEJ Cubero, R☤NNo ratings yet
- DAFTAR PUSTAKA PebDocument2 pagesDAFTAR PUSTAKA PebFatya WelinsaNo ratings yet
- HAND WASHING Content FinalDocument5 pagesHAND WASHING Content Finalsrimalathi100% (1)
- Annual Report MoH 2021-CompressedDocument381 pagesAnnual Report MoH 2021-CompressedDING TIAN YUNo ratings yet
- Online Assignment 4Document6 pagesOnline Assignment 4Ab Staholic BoiiNo ratings yet