Professional Documents
Culture Documents
Association Measurement
Uploaded by
nva1995Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Association Measurement
Uploaded by
nva1995Copyright:
Available Formats
METHODOLOGY: THE SCIENCE OF EM MTHODOLOGIE : SCIENCE DE LA MU
Measures of association: an overview with examples
from Canadian emergency medicine research
Andrew Worster, MD;* Brian H. Rowe, MD
S EE
RELATED
E DITORIAL ,
PAGE
175.
0ABSTRACT
The authors of studies often report their results using abbreviated terms such as RR, OR, ARR, RRR
and NNT. These terms are quantities that express the strength of association between the dependent and independent variables and are collectively referred to as measures of association. The
similarity between these measures and the multiple terms by which each is referred can be confusing. The purpose of this article is to explain in a straightforward manner the purpose, derivation, and limitations of some of the more commonly used categorical measures of association, including relative risk, odds ratio, absolute and relative risk reduction and number needed to treat,
using results from recent emergency medicine studies published by Canadian researchers.
RSUM
Les auteurs dtudes prsentent souvent leurs rsultats en utilisant des abrviations comme RR, RC
(OR en anglais), ARR, RRR et NNT. Ces termes sont des quantits qui expriment le degr dassociation entre les variables dpendantes et indpendantes et quon appelle collectivement les
mesures dassociation. La similitude entre ces mesures et les multiples termes utiliss pour les identifier peuvent prter confusion. Le prsent article a comme objectif dexpliquer clairement le
but, la drivation et les limites de certaines des mesures les plus couramment utilises, notamment
le risque relatif, le rapport des cotes (odds ratio), la rduction absolue et relative du risque et le
nombre ncessaire pour traiter, en ayant recours aux rsultats dtudes rcentes en mdecine
durgence publis par des chercheurs canadiens.
Key words: Evidence-based medicine, emergency medicine, decision-making, therapeutics
Clinical scenario
A 32-year-old woman presents to the emergency department (ED) with acute asthma. After 3 hours of treatment
she feels much better, and her pulmonary function measurement is now 70% of predicted. A recent article suggests that she would have less risk of relapse if you added
inhaled corticosteroids to her oral prednisone treatment.1
The study reported a p value of 0.049, a relative risk reduction of 48%, an absolute risk reduction of 12% and a num-
ber needed to treat of 9. The patient asks why you think
she should take this and whether its any better than the
echinacea she currently takes. How do you summarize
these different results for yourself, for junior learners and
for the patient?
The basics
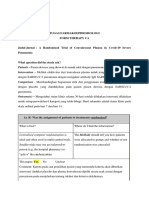
Familiarity with 22 tables is central to understanding
each of the measures of association.2 Table 1, a standard
*Research Coordinator, Research Division of Emergency Medicine, Hamilton Health Sciences Corporation, and McMaster University,
Hamilton, Ont.; Division of Emergency Medicine and Department of Public Health Sciences, University of Alberta, and Capital Health
Authority, Edmonton, Alta.
Received: Feb. 2, 2001; final submission: Apr. 28, 2001; accepted: May 15, 2001
This article has been peer reviewed.
July juillet 2001; 3 (3)
CJEM JCMU
219
Worster and Rowe
22 table, presents the dependent variable (outcome event)
across the top and the independent variables along the side,
with the experimental treatment listed above the control
treatment. This format is important because deviation from
it can alter future calculations.
When we speak of outcomes in clinical trials, we are
typically referring to things that happen to patients (e.g.,
death, surgery, stroke or disease recurrence). As these examples reveal, most outcomes in clinical trials are negative events especially death! An exception is in cardiac
arrest trials, where a commonly reported outcome is survival-to-hospital discharge. In addition, many outcomes
are dichotomous; that is, the patient either experienced
the event or did not. However, in order to express outcomes in a 22 table format, outcomes need not be dichotomous (nor must they be negative). For instance, we
can take a continuous variable such as peak expiratory
flow rate (PEFR) and set a cut-off point, such as 200
L/min, to differentiate a severe from a not-severe patient
group. In this case, the outcome is binary, but not necessarily a negative event.
Risk vs. odds
Next we need to define and differentiate two terms: risk
and odds. Risk is simply the probability of an event occurring.2 The term risk generally implies a negative event;
we dont describe people as being at risk of winning a lottery. However, the clinical event need not necessarily be
unfavourable to the patient even though the results of the
trial are described in terms of risk. Odds differ from risk in
that odds involves 2 probabilities instead of 1, and these 2
probabilities are expressed in the form of a ratio. Specifically, odds is the ratio of the probability of an event occurring to the probability of the event not occurring.2 This order in the ratio occurrence over non-occurrence is
important if one is to interpret the results accurately. For
example, if of every 100 ED chest pain patients with a normal initial ECG, 60 are found to have an acute coronary
syndrome (ACS) and 40 are not, the risk or probability of
these patients developing ACS is 60/100 or 0.6.2 However,
the odds among these 100 patients of developing an ACS
are 60:40 or 1.5.2
Relative risk (RR)
One way to measure the results in a cohort study or randomized controlled trial (RCT) is to compare the number of
outcome events in the treatment group vs. the number in the
control group.3 The relative risk (RR), or risk ratio, does
just that. It is a measure of the probability of occurrence of
an event in those who received the experimental treatment
(exposed group) compared (relative) to those who received
the standard or control treatment (not exposed).4
The relative risk is defined as (see Table 1 for definitions):
RR = Incidence in treatment group / Incidence in control group
= [A / (A + B)] / [C / (C + D)]
= A (C + D) / C (A + B)
An RR of 1 indicates that the outcome rate is the same in
both groups, therefore, the experimental group is no better
or worse off than the control group. An RR < 1 indicates
that the outcome rate is lower in the exposed (treatment)
group than the unexposed (control) group. This signifies an
effective treatment. If the outcome is a negative event such
as death, an RR < 1 would indicate that there are fewer
deaths in the treatment group than in the control group. In
this case, the experimental treatment is superior to the
standard treatment. Also, the further the RR is from 1, the
greater the effect size or difference between the 2 groups.
It follows that an RR >1 indicates the reverse, suggesting
that the experimental treatment is inferior to the control
treatment.
Table 2 was taken from an RCT of acute asthma treatment, wherein ED patients were discharged with oral corticosteroids plus either budesonide (an inhaled corticosteroid) or placebo.1 The main outcome event was relapse,
defined as an unscheduled visit for worsening asthma
symptoms within 21 days of discharge. Of the 94 patients
randomized to budesonide, 12 (12.8%) relapsed. Conversely, 23 (24.5%) of the 94 patients randomized to
placebo relapsed.
Table 1. A typical 22 table
Outcome events
Treatment
(exposure)
Control
(no exposure)
Total
220
Table 2. Asthma relapse with budesonide vs. placebo
Yes
No
Total no. of patients
per group
(A + B)
(C + D)
(A + C)
(B + D)
(A + B + C + D)
Relapse within 21 days
Yes
No
Total
Treatment
(budesonide)
Control (placebo)
12
23
82
71
94
94
Total
35
153
188
CJEM JCMU
July juillet 2001; 3 (3)
Measures of association
The incidence of the primary outcome (relapse) was
12/94 (0.128) in the inhaled corticosteroid (ICS) group and
23/94 (= 0.245) in the control (placebo) group. The RR is,
therefore, 0.128/0.245 = 0.522. We can conclude that the
relative risk of asthma relapse with ICS is 0.52. When the
outcome is an adverse event, an RR < 1 suggests the treatment is superior to the control. An RR of 0.52, therefore,
shows ICS to be superior to placebo. Expressed as a percent (52%), we can say that the risk of relapse with ICS is
approximately 52% (or one half) of that with placebo.
Unfortunately, RR does not tell us the baseline event
rate. In this example, the baseline event rate would be the
rate of asthma relapse in patients discharged without ICS.5
RR only reveals whether the outcome rate in the treatment
group is more (RR > 1), the same (RR = 1), or less (RR <
1) than it is in the control group. Another limitation is that
the RR cannot be calculated from non-cohort or RCT studies. This is because in casecontrol studies the investigator
selects the number of case and control subjects according
to whether they have experienced the outcome event and,
subsequently, predetermines the proportion of individuals
with the outcome event.4,5 In such studies, the odds ratio
(OR) is a more correct measure of association to apply.
Relative risk reduction
The relative risk reduction (RRR) is a quantification of
how much the treatment reduces the risk of the outcome
relative to the baseline outcome event rate. Wherein the
baseline risk of an outcome event is the event rate in the
control group defined by C/(C + D), the RRR is the difference in outcome event rates between the control and treatment groups divided by the outcome event rate in the control group.
RRR = ([C / (C + D)] [A / (A + B)]) / [C / (C + D)]
= (0.245 0.128) / 0.245 = 0.48
Absolute risk reduction (ARR)
The ARR has several synonyms, including attributable relative risk, attributable risk, attributable risk reduction, and
risk difference.5,6 Where RR gives a ratio of risk (an indication of the relative risk of exposure) and RRR gives the reduction in baseline risk relative to control, the ARR combines both the baseline outcome event rate and the risk
reduction in the treatment group to give the actual risk difference between the treatment and control groups.5
ARR = Incidence in control group Incidence in treatment group
= [C / (C + D)] [A / (A + B)]
Using the results from the budesonide example in Table 2:
ARR = 0.245 0.128 = 0.117
we convert these numbers to percent by simply multiplying by 100 to arrive at:
ARR = 24.5% 12.8% = 11.7%
Since the RRR is expressed as a percent: 0.48 100% =
48%. The shorter method of performing this calculation is
from the RR:5
RRR = (1 RR) 100%
= (1 0.52) 100%
= 48%
From the budesonide example we see that ICS reduced the
baseline risk of asthma relapse at 21 days by 48% relative
to placebo.
Although the RRR is the most commonly reported measure of dichotomous treatment effect, it gives the decisionmaker no indication of the absolute number of people who
July juillet 2001; 3 (3)
might benefit from the intervention and, therefore, no indication of the cost-effectiveness of the intervention.6 In our
ICS example, an RRR of 48% appears very impressive,
and for those patients who benefit, it is very impressive.6,7
However, it doesnt tell us what the risk of relapse is without ICS. If the risk of asthma relapse was rare (e.g.,
1:1000), an RRR = 48% means that only about 1:2000 patients would benefit. In this case, the relative risk reduction
is high, but the absolute benefit to the population is low.6
Alternatively, small relative risk reductions may provide
significant benefit to the population if the condition is
common. An example of a common disorder with significant impact on society is stroke. A treatment that produced
a 5% relative reduction in strokes would confer a huge
benefit to the population as a whole.6,7
This means that the absolute reduction in 21-day relapse
from asthma in the ICS patients is 11.7%.2 Hence, 11.7%
fewer patients relapsed in the ICS group than in the
placebo group. This is a much lower number than the
RRR, making the treatment effect appear less impressive.
Expressing results in relative terms (the risk of relapse in
the treatment group is 52% of that in the placebo group)
can make them seem very different than expressing them
in absolute terms (11.7% fewer patients relapsed). The
ARR provides more information about treatment effectiveness, in that it tells us what the consequences are of not
treating the patient (i.e., the percentage of control patients
who experience the outcome event).5,6 The main limitation
of the ARR is the usefulness of this number to the clinician
CJEM JCMU
221
Worster and Rowe
who has to decide whether or not to start his or her patients
on this therapy.
Number needed to treat (NNT)
NNT, the number of patients who need to be given the
treatment in order to prevent one outcome event, is a useful
measure for explaining the likelihood of benefit from treatment.6 Moreover, NNT is intuitive to both physicians and
patients. Like the ARR, NNT provides a treatment effect
size result that incorporates both the baseline outcome
event rate and the risk reduction in the treatment group. It
can be argued, the ARR is more useful than the NNT because it expresses the results in more concrete terms and
allows for treatment effect comparisons to be made with
other disorders.6 The NNT is simply the reciprocal of the
ARR:
NNT = 1 / ARR
= 1 / 0.117 = 8.54
Hence, by inverting 11.7% i.e., we arrive at 8.54.2 Therefore, the number of asthma patients we need to treat with
ICS to prevent one relapse is 9.1 NNT changes inversely
with both the baseline outcome event rate and the RR;
therefore, an increase in event rate or relative risk mean
that fewer patients need to be treated in order to prevent
one outcome event. Conversely, a decrease in the risk of
the event will result in a higher NNT.
Odds ratio (OR)
As with the ARR, the OR has a number of synonymous
terms, including relative odds and cross-product ratio.1
Other terms often incorrectly used synonymously with
OR include relative risk (RR) and risk ratio. The OR is
the ratio of the probability of an outcome event in one
group (treatment or exposure) to the probability of the
outcome event the other group (control or nonexposure).2,3 The OR is a useful measure of treatment effect in RCTs and, as with the RR, the OR indicates that
the outcome rate in the treatment group is more (OR > 1),
the same (OR = 1), or less (OR < 1) than in the control
group.6 In casecontrol studies on etiology, the OR indicates the probability of exposure to causative agent given
the outcome.
OR = AD/CB
Many confuse RR and OR. Unlike RR, the OR is not an
accurate measure of risk.4,6 OR tends to slightly overestimate RR, but as the frequency of outcome events or dis222
ease incidence becomes smaller and approaches zero, the
OR and RR will become increasingly equal.4 Thus for rare
events, the OR is a good approximation of RR. We can
also see from the OR formula where the term cross-product ratio comes from.8
OR = AD/CB
RR = A(C + D) / C(A + B)
From the example above we can calculate the OR:
OR = (12 71) / (23 82)
= 852 / 1886
= 0.452
The OR (0.452) in this example is quite different from the
RR (0.522).2 However, if we reduce the incidence (A and
C) by a factor of 10 (Table 3), then re-calculate the OR, we
will see that it more closely approximates the RR.
OR = (12 917) / (23 928) RR = 12 (23 + 917) / 23 (12 + 928)
OR = 11,004 / 21,344
RR = 11,280 / 21,620
OR = 0.516
RR = 0.522
As predicted, the OR approximates the RR as the incidence becomes very small.
Odds ratios are also easily generated from logistic regression models, where the purpose is to quantify the predictive
relationship between the independent and dependent variables using the former to predict the latter.8 An excellent
example comes from the Ontario Prehospital Advanced Life
Support (OPALS) Study Group, who analyzed 6331 cardiac
arrest calls to determine how strongly each of 5 independent
factors contributed to the survival of prehospital cardiac arrest patients.9 The strongest association came from the variables, witnessed arrest and bystander CPR, which had
ORs of 3.9 and 3.7 respectively. Knowing this, we can say
that a cardiac arrest victim who suffered a witnessed arrest is
approximately 3.9 times more likely to survive than one
whose arrest was not witnessed. Similarly, patients who receive bystander CPR are approximately 3.7 times more
likely to survive to hospital discharge than those who do not.
The odds ratio is also the measure of choice in meta-analysis
(systematic reviews) where it refers to the probability that
the outcome will occur in the treatment group.6 In another
Table 3. Asthma relapse with lower incidence rates
Relapse of symptoms
within 21 days
Yes
No
Total
Treatment
(budesonide)
Control (placebo)
12
23
928
917
940
940
Total
35
1845
1880
CJEM JCMU
July juillet 2001; 3 (3)
Measures of association
Canadian study that pooled the results of 6 RCTs comparing
mortality rates of patients treated with prehospital thrombolysis to those treated with in-hospital thrombolysis, the OR
was 0.83.10 Since the OR < 1, we can conclude that the outcome (all cause mortality) is less common in the experimental group (prehospital thrombolysis recipients) than in the
control group (in-hospital thrombolysis recipients).
Precision
Measures of association, like all measures, are merely estimates of the truth. Therefore, it is often helpful to calculate
95% confidence intervals (CIs) around the derived estimate. Confidence intervals describe the precision of the estimate and help determine whether the result is statistically
significant. The 95% CI represents the value range that the
true value will fall within 95% of the time. In other words,
although we can rarely know the exact true value (e.g., the
proportion of asthmatic patients who relapse in the
whole world), if we know the 95% CI, we can be 95% certain that the true population value lies somewhere within
this interval. Since an OR or RR value of 1.0 indicates no
difference between the treatment and control groups, a
95% CI that includes the value 1.0 is not statistically significant. In other words, regardless of the value of our
measure of association, if it has a 95% CI that includes 1.0,
it is very possible that there is no treatment effect. Similarly, CIs for the ARR or RRR that include a value of zero
are also not statistically significant.
Summary
This article has attempted to explain and clarify the advantages and disadvantages of common measures of association. With respect to RR and OR, readers should remember
that if these parameters are > 1, the outcome event is more
common in the treatment group. If they are = 1, the outcome rate is the same in the treatment and control groups,
and if they are < 1, the outcome rate is lower in the treatment group than in the control group.
In the clinical scenario described at the beginning of this
article, you would explain to the patient that, while there
are no guarantees she will remain relapse-free, her chance
of asthma relapse within 3 weeks of ED discharge is about
twice as great without ICS than with ICS (RRR = 48%;
RR = 0.52). You might also explain that approximately
12% (ARR = 11.7%) fewer patients would be expected to
relapse when treated with ICS than with placebo, and that
of every 9 patients treated with ICS, at least 1 will avoid
relapse. Furthermore, youre unaware of any studies on the
July juillet 2001; 3 (3)
efficacy of echinacea in the treatment of acute asthma in
the emergency setting and are unable to comment on its
possible effectiveness. However, you are aware that high
quality evidence fails to support the use of a variety of
homeopathic treatments in chronic asthma.11
Acknowledgments: We wish to thank Dr. David Sackett for his guidance
in writing this article. We would also like to thank Drs. Laurie J. Morrison
and Ian Stiell for so promptly responding to our request for studies published by Canadian emergency physicians.
This paper was funded by the Hamilton Health Sciences Corporation,
Hamilton, Ont.
References
1. Rowe BH, Bota GW, Fabris L, Therrien SA, Milner RA, Jacono
J. Inhaled budesonide in addition to oral steroids to prevent
asthma relapse following discharge from the emergency department: a randomized controlled trial. JAMA 1999;281:2119-26.
2. Last JM. A dictionary of epidemiology. 3rd ed. New York: Oxford University Press; 1995.
3. McKibbon A, Eady A, Marks S. PDQ: Evidence-based principles and practice. Hamilton (ON): BC Decker Inc.; 1999.
4. Streiner DL, Norman GR. PDQ: Epidemiology. 2nd ed. St.
Louis: Mosby; 1996.
5. Jaeschke R, Guyatt G, Shannon H, Walter S, Cook D, Heddle N.
Basic statistics for clinicians. 3. Assessing the effects of treatment: measures of association. CMAJ 1995;152(3):351-7.
6. Laupacis A, Sackett DL, Roberts RR. An assessment of clinically useful measures of the consequences of treatment. N Engl
J Med 1988;318(26):1728-33.
7. Jaeschke R, Guyatt GH, Sackett DL. Users guides to the medical literature. II. How to use an article about therapy or prevention. B. What were the results and will they help me in caring
for my patients? The Evidence-Based Medicine Working
Group. JAMA 1994;271(1):59-63.
8. Lang TA, Secic M. How to report statistics in medicine: annotated guidelines for authors, editors, and reviewers. Philadelphia:
American College of Physicians; 1997.
9. Stiell IG, Wells GA, Field BJ, Spaite DW, De Maio VJ, Ward R,
et al, for the OPALS Study Group. Improved out-of-hospital cardiac arrest survival through the inexpensive optimization of an
existing defibrillation program: OPALS study phase II. Ontario
Prehospital Advanced Life Support. JAMA 1999;281:1175-81.
10. Morrison LJ, Verbeek PR, McDonald A, Sawadsky B: A metaanalysis of prehospital thrombolysis and the effect on mortality
in acute myocardial infarction. JAMA 2000;283:2686-92.
11. Linde K, Jobst KA. Homeopathy for chronic asthma [Cochrane
review]. In: The Cochrane Library, Issue 1, 2001. Oxford: Update Software.
Correspondence to: Dr. Andrew Worster, Department of Emergency Medicine, Hamilton Health Sciences Corporation, 237 Barton St. E, Hamilton
ON L8N 3Z5; 905 521-2100 x73136, fax 905 527-7051, worster@hhsc.ca
CJEM JCMU
223
You might also like
- Tugas Farepid - CA - 198114152Document11 pagesTugas Farepid - CA - 198114152JeanieNo ratings yet
- Telaah Kritis Jurnal 2Document9 pagesTelaah Kritis Jurnal 2Ayu Vitha ViginiaNo ratings yet
- EBM Dan Critical AppraisalDocument7 pagesEBM Dan Critical AppraisalNovia Ariani DewiNo ratings yet
- Worksheet Appraisal AZALEADocument5 pagesWorksheet Appraisal AZALEAArini NurlelaNo ratings yet
- Statics MRCGP 2015Document22 pagesStatics MRCGP 2015AlexandraOsmanNo ratings yet
- (OBAT CINA) CAT TherapyDocument6 pages(OBAT CINA) CAT TherapyArga PRNo ratings yet
- RCT Appraisal Sheets 2005 English-2Document6 pagesRCT Appraisal Sheets 2005 English-2tsyrahmaniNo ratings yet
- Critical Appraisal For Therapy Articles: Are The Results of The Trial Valid? (Internal Validity)Document4 pagesCritical Appraisal For Therapy Articles: Are The Results of The Trial Valid? (Internal Validity)Putri Widya AndiniNo ratings yet
- Epidemiology Med RevisionDocument4 pagesEpidemiology Med RevisionswamysamsonNo ratings yet
- Randomised: Differences Between Groups Are Statistically Significant P ValuesDocument6 pagesRandomised: Differences Between Groups Are Statistically Significant P ValuesArga PRNo ratings yet
- Angel Yudiakristi - Praktikum 5Document10 pagesAngel Yudiakristi - Praktikum 5Angel MaharaniNo ratings yet
- Referat Iktiosis PembahasanDocument4 pagesReferat Iktiosis PembahasanPatih GajahmadaNo ratings yet
- Uworld - INTERNAL MEDICINEDocument131 pagesUworld - INTERNAL MEDICINENikxyNo ratings yet
- EBM GlossaryDocument4 pagesEBM GlossaryJanBarlaanNo ratings yet
- RCT Appraisal Sheets 2005 English-1 1Document5 pagesRCT Appraisal Sheets 2005 English-1 1api-479716004No ratings yet
- Relative RiskDocument8 pagesRelative Riskzhelle2No ratings yet
- Critical Appraisal for Therapy ArticlesDocument4 pagesCritical Appraisal for Therapy ArticlesMahardhika AcintyaNo ratings yet
- Ann Rheum Dis-2003-Osiri-316-21Document7 pagesAnn Rheum Dis-2003-Osiri-316-21Imuzz Al GhassanNo ratings yet
- CA Therapy Artikel 09Document5 pagesCA Therapy Artikel 09Christiana TrijayantiNo ratings yet
- Worksheet Therapy-CebmDocument3 pagesWorksheet Therapy-Cebmteddy sNo ratings yet
- Centralised Computer Randomisation Is: Critical Appraisal For Therapy ArticlesDocument4 pagesCentralised Computer Randomisation Is: Critical Appraisal For Therapy ArticleshadzaliegNo ratings yet
- Confidence Intervals II AJPDocument5 pagesConfidence Intervals II AJPJu ChangNo ratings yet
- RCT Appraisal Sheets 2005 EnglishDocument4 pagesRCT Appraisal Sheets 2005 EnglishAmanda SoebadiNo ratings yet
- Crit AppDocument5 pagesCrit AppdikkaNo ratings yet
- Worksheet Therapy CebmDocument3 pagesWorksheet Therapy Cebmandynightmare97No ratings yet
- Relative Risk and Absolute Risk ReductionDocument4 pagesRelative Risk and Absolute Risk ReductionMatthew Lei0% (1)
- Patients - Intervention - Comparison - Outcome(s)Document3 pagesPatients - Intervention - Comparison - Outcome(s)Intan SetyadewiNo ratings yet
- CRITICAL APPRAISAL Mas WikoDocument10 pagesCRITICAL APPRAISAL Mas WikoEliataMariaMahanaimNo ratings yet
- Risk & Causation: Frances Aviles MD MPH BsDocument47 pagesRisk & Causation: Frances Aviles MD MPH BsEthar LoveNo ratings yet
- RCT Appraisal Sheets 2005 EnglishDocument2 pagesRCT Appraisal Sheets 2005 EnglishF NNo ratings yet
- Critical Appraisal of Therapy Study ValidityDocument3 pagesCritical Appraisal of Therapy Study ValidityOtty Mitha OctrizaNo ratings yet
- MBT5g7fpQcGU YO36YHBEg - Summative Quiz Time To Event SolutionsDocument7 pagesMBT5g7fpQcGU YO36YHBEg - Summative Quiz Time To Event Solutionsmia widiastutiNo ratings yet
- PCR 7 51Document3 pagesPCR 7 51Rifky Fauzan MuhamadNo ratings yet
- Patients - Intervention - Comparison - Outcome(s)Document4 pagesPatients - Intervention - Comparison - Outcome(s)sahirbuleNo ratings yet
- Peds Journal Club 1A-Article About TherapyDocument15 pagesPeds Journal Club 1A-Article About TherapyAditya Rachman Van Der ArjunaqueeNo ratings yet
- "Evidence-Based Medicine" TherapyDocument54 pages"Evidence-Based Medicine" TherapyRuthra Devi NarayanasamyNo ratings yet
- Evidence-Based Medicine Therapy: Dr. Rina Amelia, MARSDocument43 pagesEvidence-Based Medicine Therapy: Dr. Rina Amelia, MARSRezky IlhamNo ratings yet
- UW Notes - 6 - Public HealthDocument27 pagesUW Notes - 6 - Public HealthMADDYNo ratings yet
- Critical Appraisal for Therapy Study ResultsDocument3 pagesCritical Appraisal for Therapy Study ResultsVeysusanNo ratings yet
- THERAPY STUDY RESULTS VALIDDocument4 pagesTHERAPY STUDY RESULTS VALIDAhmad BukhariNo ratings yet
- Evidence-Based Medicine Therapy: Dr. Dr. Rina Amelia, MARS Departemen Kedokteran Komunitas FK USUDocument40 pagesEvidence-Based Medicine Therapy: Dr. Dr. Rina Amelia, MARS Departemen Kedokteran Komunitas FK USUSamuel TanNo ratings yet
- Critical Therapy Study ResultsDocument4 pagesCritical Therapy Study ResultsAinur 'iin' RahmahNo ratings yet
- Therapy Studies What Question Did The Study Ask?Document2 pagesTherapy Studies What Question Did The Study Ask?Apt RiskaNo ratings yet
- Evidence on Harmful Effects of Medical InterventionsDocument22 pagesEvidence on Harmful Effects of Medical InterventionsRezaNo ratings yet
- Data Analysis and InterpretationDocument65 pagesData Analysis and InterpretationYus AniNo ratings yet
- C - II - 3 - Critical AppraisalDocument10 pagesC - II - 3 - Critical AppraisalWahyu NandaNo ratings yet
- Patients - Intervention - Comparison - Outcome(s) - Knowledge GapDocument4 pagesPatients - Intervention - Comparison - Outcome(s) - Knowledge GapAmal NajiNo ratings yet
- Make A NewSenin 26 Januari 2015 EBM GLOSARY Dr. Akhmad EdiDocument12 pagesMake A NewSenin 26 Januari 2015 EBM GLOSARY Dr. Akhmad EdinaotonaoiNo ratings yet
- Epidemiology 2020Document37 pagesEpidemiology 2020amelietunNo ratings yet
- Critical Appraisal Checklist For An Article On Treatment or PreventionDocument4 pagesCritical Appraisal Checklist For An Article On Treatment or PreventionSaina AbasNo ratings yet
- 2 General Principles of Research Design and AnalysisDocument6 pages2 General Principles of Research Design and AnalysisMohamed Elprince AdelNo ratings yet
- Cox Proportional Hazards and Case-Control StudiesDocument5 pagesCox Proportional Hazards and Case-Control StudiesWaqas NadeemNo ratings yet
- Measures of AssociationDocument40 pagesMeasures of AssociationErmiasNo ratings yet
- Laporan Resmi Praktikum Pharmaceutical Kardio Endokrin Pertemuan V Critical Appraisal (Ebm)Document16 pagesLaporan Resmi Praktikum Pharmaceutical Kardio Endokrin Pertemuan V Critical Appraisal (Ebm)evangeline keisha annabelNo ratings yet
- (CPG) Philippine Periodic Health Examination Phase 1 - Evidence SummariesDocument159 pages(CPG) Philippine Periodic Health Examination Phase 1 - Evidence SummariesKaren Mae PadillaNo ratings yet
- Basic ConceptsDocument37 pagesBasic ConceptsDocwocNo ratings yet
- Table 2A Critical Appraisal Vaccine Therapy EfficacyDocument10 pagesTable 2A Critical Appraisal Vaccine Therapy Efficacy7CANTIKA PRAMESWARI HANANTONo ratings yet
- Critical Appraisal Checklist For An Article OnDocument4 pagesCritical Appraisal Checklist For An Article OnTiaz DiniutamiNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyFrom EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyRating: 1 out of 5 stars1/5 (1)
- The Pediatric Mandible I. A Primer On Growth and DevelopmentDocument10 pagesThe Pediatric Mandible I. A Primer On Growth and DevelopmentJulián David Ríos ZuluagaNo ratings yet
- Artificial Intelligence in Rheumatology: Applications and ChallengesDocument39 pagesArtificial Intelligence in Rheumatology: Applications and ChallengesMaryame BoutkhilNo ratings yet
- G.V. Black's Classification and Class I Cavity PreparationDocument57 pagesG.V. Black's Classification and Class I Cavity PreparationPrakuz Harmony SubedifiedNo ratings yet
- Piston Water MeterDocument2 pagesPiston Water MeterMark PamularNo ratings yet
- Mode of AssignmentDocument95 pagesMode of AssignmentQasim AliNo ratings yet
- Sheath CurrentsDocument5 pagesSheath Currentsscribdkkk100% (1)
- Barriers To Nurse - Patient Communication in Saudi Arabia: An Integrative ReviewDocument10 pagesBarriers To Nurse - Patient Communication in Saudi Arabia: An Integrative Reviewmark3dasaNo ratings yet
- English Form 2 Mod23042022001Document10 pagesEnglish Form 2 Mod23042022001Qiash JontezNo ratings yet
- Hazard Identification 2. Risk AssessmentDocument5 pagesHazard Identification 2. Risk AssessmentNoreen Syakireen Binti NormanNo ratings yet
- Flatworms Round Worms and Anne Lids LabDocument6 pagesFlatworms Round Worms and Anne Lids LabBellaNo ratings yet
- MaryamDocument1 pageMaryamHAIZA FATHIMANo ratings yet
- Diesel Engine Operation and DiagDocument76 pagesDiesel Engine Operation and DiagHafiezul Hassan100% (3)
- Restraint Prevalence and Perceived Coercion Among Psychiatric Inpatientsfrom South IndiaDocument7 pagesRestraint Prevalence and Perceived Coercion Among Psychiatric Inpatientsfrom South IndiaEdson HilárioNo ratings yet
- Libyan cuisine: Bazin, asida and moreDocument3 pagesLibyan cuisine: Bazin, asida and moreAndy Atehortua CiroNo ratings yet
- 2) VT Report Test FormatDocument3 pages2) VT Report Test FormatMoin KhanNo ratings yet
- SOP - APS - PUR - 02A - Flow Chart For PurchaseDocument2 pagesSOP - APS - PUR - 02A - Flow Chart For Purchaseprakash patelNo ratings yet
- Inas Faiqah BT Mohd Helmi (An Infant Suing Through Her Father and Next Friend, Mohd Helmi Bin Abdul Aziz) V Kerajaan Malaysia & OrsDocument15 pagesInas Faiqah BT Mohd Helmi (An Infant Suing Through Her Father and Next Friend, Mohd Helmi Bin Abdul Aziz) V Kerajaan Malaysia & Orsshukri77No ratings yet
- Crop RotationsDocument19 pagesCrop RotationsSarwar M. RasheedNo ratings yet
- Pipe Material & Dimension Standard MatrixDocument2 pagesPipe Material & Dimension Standard MatrixHemantNo ratings yet
- 2005 Petro Lab GuidelinesDocument11 pages2005 Petro Lab Guidelinesalomaritrq100% (1)
- APA Style Guide for Student PapersDocument24 pagesAPA Style Guide for Student PapersHeureuse MamanNo ratings yet
- Sibling RivalryDocument2 pagesSibling Rivalrycarlokim14No ratings yet
- RP F107 PDFDocument45 pagesRP F107 PDFPriyam KmNo ratings yet
- Contracts Summary: 601 Totaling $4.76 BillionDocument186 pagesContracts Summary: 601 Totaling $4.76 BillionJAGUAR GAMINGNo ratings yet
- FT-IR Analysis of Hock ProcessDocument4 pagesFT-IR Analysis of Hock ProcessmohsengolestanzadehNo ratings yet
- Wind Energy 6Document12 pagesWind Energy 6Shanthi RameshNo ratings yet
- Adult Assessment: Head To Toe Assessment Is The Baseline and Ongoing Data That Is Needed OnDocument2 pagesAdult Assessment: Head To Toe Assessment Is The Baseline and Ongoing Data That Is Needed OnAldrin NavarroNo ratings yet
- Service Manual For High Efficiency High Ambient Amazon 20180726Document400 pagesService Manual For High Efficiency High Ambient Amazon 20180726Syedimam100% (1)
- Complete Dummy's Guide to a Diffusion Pumped Vacuum SystemDocument4 pagesComplete Dummy's Guide to a Diffusion Pumped Vacuum Systemjokerbuddy01No ratings yet
- ProVent - MANN + HUMMEL ProVent - Oil Separator For Open and Closed Crankcase Ventilation SystemsDocument29 pagesProVent - MANN + HUMMEL ProVent - Oil Separator For Open and Closed Crankcase Ventilation SystemsJosephNo ratings yet