Professional Documents
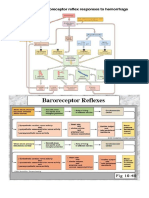
Culture Documents
Effects of Hypertonic Saline On Myocardial Contractility in Anaesthetized
Uploaded by
liyaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effects of Hypertonic Saline On Myocardial Contractility in Anaesthetized
Uploaded by
liyaCopyright:
Available Formats
1. vet. Pharmacol. Therap. 1 7 , 21 1-2 1 7, 1994.
Effects of hypertonic saline on myocardial contractility in anaesthetized
P. W. HELLYER & Hellyer, P.W., Meyer, R.E. Effects of hypertonic saline on myocordial contracti-
R. E. MEYER lity in anaesthetized pigs. 1. vet. Pharmacol. Therap. 1 7 , 211-2 17.
The cardiac effects of hypertonic saline (HS, 7.5% NaCl) were evaluated using a
Department of Anatomy, Physiological
number of indices derived from the left ventricular (LV) pressurevolume rela-
Sciences and Radiology. North Carolina
State University, College of Veterinary Medicine, tionship. Left ventricular end-systolicelastance (elastance), the slope of the end-
4700 Hillsborough Street, Raleigh. systolic pressure-volume relationship, end-systolic elastance normalized for
N C 2 7 6 0 6 , USA enddiastolic volume (elastance(,,,,), the rate of rise of LV pressure (dPldt,,,),
and dP/dt,,/end-diastolic volume were used to assess myocardial contractility.
Pigs were anaesthetized with isoflurane and instrumented for haemodynamic
measurements, LV pressure, and volume (conductance catheter) determina-
tions. Elastance was determined during transient (8-10 s) caudal vena caval
balloon occlusion. Following instrumentation, the end-tidal isoflurane concen-
tration was reduced and maintained at 1 minimum alveolar concentration
(1.5%).Pigs were randomly administered either 0.9%NaCl (n = 7) or HS (n =
9) at a dose of 4 ml/kg, over 3 min into the right atrium. There were no signifi-
cant differences in LV or haemodynamic measurements between isotonic saline
and HS treated pigs a t any time point. Elastance, elastance(,,,,, and
dP/dt,,,/end-diastolic volume did not change in either treatment group. In con-
trast, dPldt,, increased significantly (P < 0.015) at 5 min compared to base-
line after treatment with HS. End-diastolic volume increased significantly from
5 to 30 min following treatment with HS. Left ventricular end-diastolic pres-
sure increased significantly at 5 and 60 min in HS treated pigs. Central venous
and pulmonary arterial wedge pressures, and cardiac index increased signifi-
cantly at 5 min after treatment with HS. Total peripheral resistance decreased
significantly at 5 min, followed by a return to baseline in the HS group. These
results suggest that HS is not a positive inotrope in the anaesthetized pig and
that increases in cardiac index are primarily due to an increased preload.
(Paper received 14 January 1993; accepted for publication 3 June 1993)
Peter W. Hellyer, DVM, MS, Department of Anatomy, Physiological Sciences and
Radiology, North Carolina State University, College of Veterinary Medicine, 4700
Hillsborough Street, Raleigh, NC 27606, USA
INTRODUCTION al., 1986), increased adrenergic activity secondary to cate-
cholamine release (Liang & Hood, 1978), activation of a pul-
Hypertonic saline (HS 7.5% sodium chloride solution) at a rate of monary vagal reflex (Younes et al.. 1 9 8 5 ) , and increased
4-5 ml/kg intravenously (i.v.) increases cardiac output and myocardial Contractility (Kien et al.. 1991a. b) have been postu-
mean arterial pressure to a greater degree than a n equivalent lated to play important roles.
volume of isotonic saline in cats (Bitterman et al.. 1987; Muir & Although it has been proposed that hypertonic solutions
Sally, 1989),dogs (Velasco et al., 1980), swine (Traverso et al.. increase cardiac contractility, conflicting evidence suggests that
1987; Wade et al.. 1989). horses (Schmall et al., 1990), and hyperosmotic, ionic solutions are negative inotropes.
sheep (Nakayama et a!., 1984) with hypovolaemic hypotension. Intracoronary injections of hyperosmolar solutions of glucose
The mechanism(s) responsible for the beneficial haemodynamic and mannitol, with osmolality from 300 to 1800 milliosmols
effects of HS are not completely understood, but increased venous (rn0sm) increased cardiac contractility in anesthetized dogs
return secondary to an increased plasma volume (Schertel et al., whereas hyperosmolar NaCl (900 m0sm) caused marked
1990),decreased peripheral vascular resistance (Rocha-e-Silva et decreases in contractility (Newell et al.. 1980). Hyperosmolar
1. vet. Phannacol. Therap. 1 7 , 211-2 17. 1994 211
2 12 P.W. Hellyer 6 R. E. Meyer
solutions of sucrose or urea (osmolality > 400-450 mosm) istered at a rate of approximately 10 ml/kg/h during instrumen-
administered to dogs had a negative inotropic effect, resulting in tation.
cardiac failure (Wildenthal et al., 1969a). This is in contrast to
solutions that had an osmolality less than 400 mosm, in which
contractility was increased. Isolated rat hearts infused with 7.5% Instrumentation
NaCl had depressed ventricular function: however, the infusion
The left and right carotid arteries, the left jugular vein, and the
of equimolar sucrose (2400 mOsm) had a positive inotropic effect
left and right femoral veins were surgically exposed and isolated.
(Brown et al., 1990). Thus, excess concentrations of Na' may
A flow-directed,thermistor-tipped Swan-Ganz catheter (Edwards
attenuate the positive inotropic effects of hyperosmolar solutions.
Labs,) was inserted in the right femoral vein and passed retro-
In addition to the direct effects of hyperosmolar solutions on con-
grade with the distal port in the pulmonary artery and the proxi-
tractility, hypertonic NaCl may act through an increase in
mal port in the right atrium. Pulmonary arterial and right atrial
plasma catecholamine concentrations in anaesthetied dogs
pressures were measured using balanced and calibrated trans-
(Liang & Hood, 1978). PAdrenergic receptor blockade with
ducers (Statham P23 ID). The zero reference measurement was
practolol abolished the positive haemodynamic effects of hyper-
considered to be at the level of the right atrium. Polyethylene
tonic NaCl, indicating the importance of catecholamines in. the
tubing was inserted in the jugular vein for the administration of
haemodynamic effects of hypertonic NaCl.
drugs and i.v. fluids. A balloon-occlusion catheter (Medi-Tech
Changes in preload and afterload induced by the rapid admin-
Inc.) was inserted in the left femoral vein and passed to the cau-
istration of HS confound the evaluation of myocardial contractil-
dal vena cava. A dual-tipped, high fidelity micromanometer
ity. Ideally, evaluation of left ventricular (LV) contractility should
catheter (Millar Instruments) was inserted in the left carotid
utilize indices that are sensitive to changes in inotropic state, are
artery and positioned with the distal transducer in the left ventri-
independent of changes in preload and afterload, and are insensi-
cle and the proximal transducer in the aorta to measure pres-
tive to changes in heart rate (Kass & Maughan, 1988).
sures. Placement of catheters was confirmed by observation of
Isovolemic contraction phase indices, such as dP/dt,,. are sensi-
characteristic pressures and waveforms.
tive and relatively specific for changes in inotropic state provided
A 7 French, multielectrode. conductance volume catheter
that preload does not change (Kass et al., 1987). Left ventricular
(Webster Laboratories) was inserted in the right carotid artery
end-systolic elastance (elastance), the slope of the maximal end-
and positioned in the left ventricle along the ventricular long
systolic pressure-volume relationship, is a relatively load-inde-
axis. The conductance catheter consisted of 11 equally spaced
pendent and sensitive index of myocardial contractile state
electrodes (0.85 cm apart) at the distal end of the catheter. The
(Kass et d.,1987). In this study, we tested the hypothesis that
distal electrode was positioned within the apex of the left ventri-
the rapid administration (over 3 min) of a small volume (4
cle and the most proximal electrode(s) was positioned just above
rnl/kg) of 7.5% NaCl would increase cardiac contractility, as
the aortic valve. A constant 2 0 kHz current, with a n amplitude
measured by elastance, in isoflurane-anaesthetied. normo-
of 30 PA RMS, was applied between electrodes 1 and 11. Five
volaemic pigs.
independent voltage differences were measured between five
adjacent pairs of electrodes and converted to left ventricular vol-
ume by a conditioning amplifier (Sigma-5, Leycom). Proper posi-
MATERIALS AND METHODS
tioning of the conductance catheter in the left ventricle was con-
firmed by observation of the segmental volume signals generated
Animal preparation
from the conductance catheter in relation to the QRS complex of
Sixteen domestic pigs, weighing 23.0 f 0.4 kg (mean f SEM), the ECG. The segmental volume signal decreases immediately
derived from a specific-pathogen free source, were the subjects of after the R wave associated with ventricular ejection. Therefore,
this study. All pigs were treated humanely in accordance with coupling of the electrical and mechanical activities of the heart
National Institute of Health guidelines for the use of experimental was used to ensure proper positioning of the conductance
animals and with approval of the Institutional Animal Care and catheter. The catheter was adjusted until at least four of the five
Use Committee at North Carolina State University. Food, but not volume segments were correctly placed in the left ventricle. Total
water, was withheld for 12 h prior to the induction of anesthesia. ventricular volume was derived from the sum of the individual
Pigs were anaesthetized with isoflurane in 0,by facemask, oro- volume segments with a small adjustment for the apical seg-
tracheally intubated, and ventilated at a constant tidal volume. ments (Baan et al., 1981, 1984). Once positioned, the conduc-
Ventilation was controlled to maintain arterial CO, tensions at tance catheter was not moved for the remainder of the experi-
approximately 40 mmHg and end-tidal CO, at approximately ment.
5%. End-tidal CO, was measured continuously with a Hewlett- The time-varying LV volume was determined from the sum of
Packard infrared gas analyzer; The concentration of isoflurane the segmental conductances, the specific conductivity of the
was adjusted to maintain a surgical plane of anesthesia during blood, the interelectrode distance, and the conductance of struc-
the instrumentation period. Expired anaesthetic concentra- tures surrounding the ventricular cavity (parallel conductance).
tions were measured continuously with an anaesthetic agent The conductance catheter cardiac output was calibrated by com-
monitor (Biochem 8100).Lactated Ringers solution was admin- paring it to the cardiac output measured by thermodilution
1. vet. Pharmacol. Therap. 17,211-217,1994
Hypertonic saline and myocardial contractility 2 13
under steady state conditions, according to the methods time period. Cardiac output was normalized for body weight and
described by Kass (Kass et al., 1988). The gain for the segmental expressed as cardiac index (CI. ml/s/kg). Pulmonary vascular
volume signals was adjusted until the conductance cardiac out- resistance (mmHg/ml/s/kg) was calculated as: PVR = (P, -
put equalled the thermodilution cardiac output. A correction Ppaw)/CI, where P, = mean pulmonary arterial pressure and PWw
term for the parallel conductance was calculated following the = pulmonary arterial wedge pressure. Total peripheral resistance
administration of 5 ml of HS into the right atrium (Baan et al., (mmHg/ml/s/kg) was calculated as: TPR = (Pma- CVP)/CI. where
1984). The correction term was determined at least twice, the P,, = mean aortic pressure and CW = central venous pressure.
results averaged, and the values entered into the computer for Elastance was calculated from the end-systolic points from
the remainder of the experiment. each pressurevolume loop during caudal vena caval occlusion
Steady-state LV pressure and volume signals were obtained (Conduct PC, Leycom). Only those pressurevolume loops, in
over an 8 s period at end-expiration with the ventilator turned which the end-systolic pressure was greater than 65 mmHg were
off. Once the end-tidal CO, and systolic arterial pressure returned used in the calculation of elastance. Premature beats and the
to their previous values (generally I 1 min), the ventilator was subsequent beat were not used in the calculation of elastance.
turned off again at end-expiration and LV pressure and volume The absolute value of elastance is somewhat dependent upon
signals obtained during transient (8-10 s) caudal vena caval bal- heart size, making comparisons between animals dif6cult.
loon occlusion. Therefore, normalized elastance (mmHg) was calculated as: elas-
tance,,,,, = elastance x V,, where V, = steady-state LV end-
diastolic volume (Berko et al., 1987). The slope of the dP/dt,, -
Experimentalprotocol
V, relationship was used to minimize the effects of preload on
Following instrumentation, sodium heparin (5000 USP units, dPldt,,. Only those slopes in which the correlation coefficient
i.v.) was administered to maintain patency of catheters. The was greater than 0.5 were used for further statistical analysis.
isoflurane concentration was reduced to maintain a constant
end-tidal anaesthetic concentration (1 minimum alveolar con- Statistical analysis
centration, 1.5%) (Eisele et al.. 1985). Neuromuscular blockade
was induced by administering pancuronium bromide (0.1 Data are expressed as mean & SEM. Statistical analysis was done
mg/kg, i.v.) and repeated as needed to prevent reflex muscular using an univariate split plot analysis with time as the split plot
movement. Baseline LV and haemodynamic measurements (t = factor. Means were compared between treatment groups at each
0) were taken 30 min after reaching a stable end-tidal anaes- level of time using an independent t-test and were considered sig-
thetic concentration. Pigs were randomly administered either nificantly different at P < 0.05. Means were compared between
7.5%NaCl (HS, n = 9),or 0.9% NaCl (control, n = 7) at a dose of t i e s within a treatment group by use of a paired t-test. Since
4 ml/kg over 3 min into the right atrium. Left ventricular and there were six time measurements. a total of 15 t-tests were per-
haemodynamic measurements were obtained at time = 5, 15. formed in each group. A t-test was considered significantly differ-
30. 45, and 60 min. Since a large bolus of HS will change the ent at P < 0.001 to give an overall alpha level < 0.01 5 (15 x
resistance properties of the blood, the specific conductivity of the 0.001 = 0.015). Blood for measurement of packed cell volume
blood was measured immediately before each determination of and total plasma proteins was collected at only three time points
LV volume and the conductance signal adjusted accordingly. (t = 0, 30, and 60 min). Therefore, differences over time within
Packed cell volume and total plasma proteins were measured at each group were considered significant at P < 0.01 to give an
30 and 60 min. The pigs were killed at the end of the experimen- overall alpha level < 0.03 ( 3 x 0.01 = 0.03).
tal protocol, while still anaesthetized, with a bolus of KCl in the
left ventricle. RESULTS
Left ventricular measurements
Analysis
There were no significant differences in LV measurements
Left ventricular, aortic, and pulmonary arterial pressures, and
between isotonic saline and HS treated pigs at any time point.
the ECG were recorded with a multichannel physiograph
Myocardial contractility, as assessed by elastance, elastance,,,,,,
(Honeywell, VR12). Each analog signal from the physiograph
or dPldt,,/V, did not change with the administration of either
was digitized at 200 Hz and stored on a microcomputer using the
HS or isotonic saline (Table 1).The rate of rise of LV pressure
Codas data acquisition program (Dataq Instruments). Digitized
increased significantly at 5 min compared to baseline, but had
data were analyzed following the end of the experiment.
returned towards baseline by 15 min in the HS group (Table 1).
Pulmonary arterial wedge and central venous pressures were dis-
End-diastolic volume increased significantly from 5 to 30 min fol-
played on the physiograph and recorded manually. The rate of
lowing treatment with HS. whereas -end-diastolic pressure
rise of LV pressure (dPldt,,) was determined by analysis of the
increased significantly at 5 and 60 min in HS pigs (Table 1).
digitized data, using a waveform oriented analysis package
(Dataq Instruments). Cardiac output was determined by ther-
modilution, using 5 ml of 5% dextrose (OOC), with the mean of Haemodynamic and blood constituent measurements
three determinations accepted as the experimental value for each There were no significant differences in haemodynamic or blood
1. vet. Pharmacol. Therap. 17,211-2 17, 1994
2 14 P. W.Hellyer b R. E. Meyer
Table 1.Left ventricular measurements from control and HS treated pigst
Time (minl
Parameter Treatment 0 5 15 30 45 60
Elastance
(mmHglml) Control 2.1 f 0.6 2.0 f 0.5 2.1 f 0.7 2.4 f 0.9 2.3 f 0.9 2.2 f 0.7
HS 1.7 f 0.2 1,5 f 0.2 1.5 f 0.2 1.4 f 0.2 1.4 f 0.2 1.4 f 0.1
Hastance,,,,,
( m g ) Control 95 f 18 89 f 14 93 f 18 98 f 20 95 f 19 95f16
HS 105 f 15 89f11 9 0 f 11 85f9 8 7 f 10 85f10
dP/dt,,
(mmHg/s) Control 1725 f 189 1728 f 173 1708 f 159 1708 f 157 1551 f 136 1664 f 156
Hs 1593 f 95 1881 f 95' 1685 f 74 1739 f 154 1 6 4 0 f 111 1591 f 98
dPldt,,lV,
(mmHg/s/ml) Control 20 f 9.8 37 i 16.0 32 f 12.8 28 f 16.4 25 f 7.6 29 f 13.4
HS 18 f 5.4 12 f 1.0 11 f 0 . 4 14 f 2.4 12 f 3.2 12 f 1.8
End-diastolic
volume (ml) Control 58f11 61 f 11 59 f 11 59 f 11 5 7 f 12 5 8 f 11
HS 64f8 77 f 8* 75 f 8' 76 f 9* 68 f 10 64f8
Enddiastolic
pressure (mmHg) Control 8.0 f 1.7 11 f 1.4 10 f 1.3 9.0 f 1.7 9.0 f 2.2 9.0 f 1.8
HS 7.0 f 1.4 11 f 1.4' 9.0 f 1.4 9.0 f 1.5 9.0 f 1.5 10 f l.6*
*Significantlydifferent(P < 0.015) from 0 min value: tFollowing baseline measurements (t = 0),pigs were administered either 0.9% NaCl (Control) or
7.5%)NaCl (HS) at a dose of 4 mllkg over 3 min. Results are mean f SEM.
constituent measurements between isotonic saline and HS sure did not change in either treatment group. Pulmonary vas-
treated pigs at any time point. Hypertonic saline produced a sig- cular resistance tended to decrease at 5 min following HS: how-
nificant, but transient, increase in cardiac index compared to ever, the differences were not significant (Table 2 ) . Packed cell
baseline that peaked at 5 min (Fig. 1).This was accompanied by volume decreased significantly at 30 and 6 0 min in the HS
a significant decrease in total peripheral resistance compared to group, whereas total plasma proteins decreased in both groups at
baseline at 5 min. followed by a return towards baseline, in the 30 and 60 min (Table 3).
HS group (Fig. 2 ) . Systolic and mean aortic pressures, and heart
rate did not change in either treatment group (Table 2). Central
venous pressure and pulmonary arterial wedge pressure tran- DISCUSSION
siently increased at 5 min and returned towards baseline by 1 5
min in HS treated pigs (Table 2 ) . Mean pulmonary arterial pres- The aim of this study was to determine if changes in myocardial
2.9 o 0.9% N a C l
A 7.5% N a C l
o 0.9% NaCl
2.6 A 7.5% NaCl
4-
2.7
2.6
2.5
n
coo
si 2.4
;.-22
8' 2.3
2.2
2.1
1 I
2.0
0
0 15 30 45 60
Time (min) 0 15 30 45 60
Time (min)
Fig. 1. Cardiac index (mean f SEM) at baseline (t = 0) and at 5, 15. 30. Fig. 2. Total peripheral resistance (mean f SEM)at baseline ( t = 0) and
45 and 60 min following treahent with either 0.9% NaCl (control. n = at 5. 15. 30,45 and 60 mln following treatment with either 0.9% NaCl
7) or 7.5%NaCl (HS, n = 9). *Significantlydifferent (P < 0.015) from 0 (control, n = 7) or 7.5% NaCl (HS, n = 9). *Significantlydifferent (P <
min value. 0.01 5) from 0 min value.
1.vet. Pharmacol. Therup. 17.211-217. 1994
Hypertonic saline and myocardial contractility 2 15
Table 2. Haemodynamic measurements from control and HS treated pigsf
Time (min)
_____ _____ ~
Parameter Treatment 0 5 15 30 45 60
Systolic arterial pressure
( m g ) Control 94 15.2 96 f 5.7 96 f 5.1 95 f 6.0 90 f 6.0 92 f 7.3
HS 93 1 3.0 93 f 3.0 91 f 2.7 94 f 3.4 91 f 3.1 90 f 3.0
Mean arterial pressure
(mmHg) Control 77 1 4.0 79 f 4.4 80 f 4.2 79 f 5.1 73 f 5.0 74 f 6.3
HS 79 k 2.8 78 f 2.6 76 f 2.8 80 f 3.5 77 f 3.3 76 f 2.7
Heart rate
(beatdmin) Control 122 f 11.6 118 f 9.6 120 f 10.7 119 f 12.1 111 f 7.0 111 f 8.0
HS 1 1 7 f 7.0 121 f 5.1 119 f 6.0 119 f 8.0 119 f 7.7 113 k 6.4
Central venous pressure
(mmHg) Control 5 f 1.2 6 f 1.5 6 f 1.5 6 f 1.5 5 f 1.4 5 f 1.6
HS 7 f 1.5 8 f 1.7' 7f 1.6 7 f 1.5 7 f 1.4 7 f 1.5
Pulmonary arterial wedge
pressure (mmHg) Control 8 1 1.3 9 f 1.3 9 f 1.4 8 f 1.3 8 f 1.2 9 f 1.3
HS 8 f 1.6 10 f 1.7' 9 f 1.7 8 f 1.6 8 f 1.5 8 f 1.6
Mean pulmonary
arterial pressure (mmHg) Control 17 f 1.8 18 f 1.5 17 f 1.7 17 f 1.5 17 f 1.8 17 f 1.6
HS 15 k 1.2 16 f 1.4 15 f 1.5 15 f 1.5 15 f 1.4 15 f 1.4
Pulmonary vascular
resistance (mmHg/ml/s/kg) Control 4.2 f 0.4 3.8 f 0.4 3.4 f 0.4 4.1 f 0.5 4.3 f 0.7 4.0 f 0.5
HS 3.7 f 0.2 2.7 f 0.4 3.7 f 0.5 3.6 f 0.2 3.9 f 0.5 4.0 k 0.4
*Signiilcantlydifferent ( P < 0.01 5) from 0 min value: fFollowing baseline measurements (t = O), pigs were administered either 0.9%NaCl (Control) or
7.5%NaCl (HS) at a dose of 4 ml/kg over 3 min. Results are mean f SEM.
contractility contribute to the haemodynamic response to HS. uted to a change in preload and not an increase in inotropic
Contractility was measured using an index, elastance, derived state. This conclusion is further supported by no change in the
from LV pressure-volume relationships, which is relatively inde- slope of the dPldt,, versus V, relationship.
pendent of changes in heart rate and loading conditions. The In this study, we used several indices of contractility, elas-
results of this study indicate that HS does not change contractil- tance, elastance,,,,,, and dP/dt,,/V, to evaluate myocardial
ity in normovolemic, isoflurane-anaesthetized pigs. inotropic state. Virtually all indices used to evaluate myocardial
The rapid administration of HS has been shown to increase inotropic state in vivo have some degree of load dependency,
venous return to the heart and thereby increase preload (Schertel including elastance (Kass et ul., 1987). The magnitude of sensi-
et al.,1990). Increased preload was evident in the present investi- tivity to changes in inotropic state detected by elastance is not as
gation by a significant increase in LV end-diastolic volume, con- great as with other indices: however. the advantage of elastance
sidered to be the most appropriate measure of LV preload since is its minimal dependence upon changes in preload and afterload.
there is a close relationship between LV volume and muscle Comparison of elastance between animals is confounded by the
length (Sagawa et al., 1988). Significant increases in LV end- dependence of elastance on heart size: therefore, elastance was
diastolic pressure, central venous pressure, and pulmonary arter- normalized for baseline end-diastolic volume (Berko et al., 1987).
ial wedge pressure further support the conclusion of an increased We also evaluated the relationship of dPldt,,, to end-diastolic
preload following the administration of HS. Therefore. the signifi- volume. which decreases the dependence of dPldt,,, on changes
cant increase in dPldt,,, at t = 5 min in the HS group was attrib- in preload while maintaining its sensitivity to changes in con-
m:-- Table 3. Blood constituents from control and
1uue (llllrl)
HS treated pigst
Parameter Treatment 0 30 60
Packed cell volume (%) Control 31 f 1.1 31 f 1.4 31 f 1.0
HS 3 1 f 1.3 29 f 1.6' 29 f 1.4'
Total plasma proteins (g/dl) Control 5.4 f 0.1 5.2 f 0.1* 5.2 f 0.1*
HS 5.3 f 0.2 5.0 f 0.2* 5.0 f 0.2*
~~
*Significantlydifferent (I' < 0.03) from 0 min value: tFollowing baseline measurements (t = 0).
pigs were administered either 0.9% NaCl (Control) or 7.5% NaCl (HS) at a dose of 4 ml/kg over
3 min. Results are mean f SEM.
1. vet. Pharmacol. Therap. 17,211-2 17, 1994
216 P. W.Hellyer6 R. E. MeMer
tractility (Kass et ul., 1987). Unfortunately, dPldt,,lV, is still pressure, contractility (+dPldt), and relaxation rate (4Pldt)
dependent on changes in afterload. In the present study, elas- (Brown et al., 1990). Similarly, increases in ionic strength by the
tance, elastance(,,,,, and dPldt,,lV, did not change signifi- addition of chloride or potassium salts decreased, whereas
cantly following treatment with HS. Since the primary haemody- increases in osmolality with the addition of sucrose did not alter,
namic change was an increase in preload (increased 'enddias- the maximum calcium-regulated force in detergent-skinned ven-
tolic volume) with minimal change in afterload (slight decrease tricular muscle from guinea-pigs (Kentish, 1984). Increasing the
in aortic blood pressure), all of these indices should accurately amount of sodium in the perfusate caused a n initial decrease in
reflect any changes in inotropic state if they were present. dPldt in the vascularly perfused rabbit intraventricular septum
Therefore, we conclude that HS is not a positive inotrope in nor- (Tillisch & Langer, 1974). On the other hand, increasing osmo-
movolaemic. isoflurane-anaesthetiied pigs, even though dPldt,, lality up to that of serum (330 mOsmll) with either sucrose or
and cardiac index increased significantly at 5 min. mannitol increased developed tension in cat papillary muscle
Determination of LV volume has been simplified by the devel- (Koch-Weser, 1963). Increases in osmolality by mannitol or
opment of the conductance (volume) catheter (Baan et ul., sucrose increased tension in isolated heart tissues provided the
1981). Using this catheter, LV volume can be rapidly determined increase in osmolality was less than or equal to 150 mOsm/l
on a beat to beat basis in man and animals (Baan et al., 1984). (Wildenthal et ul., 1969b: Beyer et ul., 1986: Allen & Smith,
Volume measurements made by the conductance catheter, cou- 1987). The intracellular concentration of calcium ( [Ca2+li)also
pled with simultaneous pressure measurements from a high- influences the inotropic effects of non-ionic, hyperosmolar solu-
fidelity micromanometer catheter, are used to construct beat to tions, such that tissues with a low [CaZ+lirespond with a positive
beat pressure-volume loops. In this study, we measured LV pres- inotropic effect whereas a negative inotropic effect is seen in tis-
sure and volume during transient (< 8 s) periods with the venti- sues with a high [Caz+],(Nayler, 1961: Willerson et ul., 1974,
lator turned off at end-expiration in order to eliminate the effects 1978: Wildenthal et al.. 1975: Kawata et al., 1983). The evi-
of positive pressure ventilation on the measured variables. A brief dence suggests that hyperosmolar. ionic solutions exert a direct
period of load alteration is required in order to generate the end- negative inotropic effect whereas non-ionic, hyperosmolar solu-
systolic pressure-volume points necessary for calculation of elas- tions exert a positive inotropic effect provided the increase in
tance. Preload was reduced in this study by inflation of a balloon osmolality is less than 150 m0smll and that [Ca2+Ii is low.
catheter positioned in the caudal vena cava. Alterations in load- In summary, the administration of a small volume (4mllkg)
ing conditions can evoke reflex sympathetic responses which of HS into the right atrium resulted in a significant. but transient
would be expected to increase the measure of contractility. increase in cardiac index. The mechanism responsible for this
Evidence of autonomic reflexes has been demonstrated after 10 s increase in cardiac index is primarily an increase in preload,
of sustained preload reduction: therefore, we l i i t e d the caudal demonstrated as an increase in LV end-diastolic volume.
vena caval balloon occlusion to 8-10 s (Kass et al., 1986). Myocardial contractility, measured by elastance, did not
Our findings that HS had no effect on contractility differ from increase, indicating that HS had no positive inotropic effect.
those of Kien (Kien et al., 1991a). In that study, halothane-
anaesthetized, normovolaemic dogs were administered HS (7.5%
ACKNOWLEDGMENTS
NaCI) at a dose of 5 mllkg, i.v., over 1 min. Elastance, derived
from the end-systolic pressurdiameter relationship, increased
The authors thank Delta Plummer for her expert technical assis-
significantly from 10 to 60 min following treatment with HS.
tance in this study. We also thank Anne Hellkamp for her assis-
The two studies differed in many aspects, including the species
tance with statistical analysis. This study was supported by the
used (dog vs. pig), the anesthetic used (halothane vs. isoflurane),
College of Veterinary Medicine research funds.
and the rate of HS administration (1 min vs. 3 min). More impor-
tantly, HS was administered directly into the right atrium in our
study, whereas it was administered i.v. in Kien's study. It is possi- REFERENCES
ble that a bolus of HS administered i.v. would be diluted to a
Allen. D.G. & Smith, G.L. (1987) The effects of hypertonicity on tension
greater extent than an intra-atrial injection before reaching the
and intracellular calcium concentration in ferret ventricular muscle.
coronary artery. Administering HS directly into the right atrium Iournal of Physiology, 3 8 3 , 4 25-439.
may have resulted in the hyperosmolar, ionic solution exerting a Baan. J., Jong. T.T.A., Kerkhof. P.L.M..Moene, R.J., Van Dijk, A.D., Van
direct depressant effect upon the heart. This is supported by a Der Velde, E.T. et al. (1981) Continuous stroke volume and cardiac
previous report in which three of Eve cats administered HS into output from intra-ventricular dimensions obtained with impedance
catheter. CardiovascularResearch, 15. 328-334.
the aortic root died within 15 min (Muir & Sally, 1989). Thus, it
Baan, J., Van Der Velde. E.T.. De Bruin. H.G.. Smeenk, G.J., Koops. J., Van
is possible that any indirect, positive inotropic effects of HS were Dijk, A.D. et al. (1984) Continuous measurement of left ventricular
attenuated by a direct cardiodepressant effect of the hyperosmo- volume in animals and humans by conductance catheter. Circulation,
lar solution in our pigs. 70,812-823.
In vitro studies further support the hypothesis that ionic, Berko. B.. Gaasch, W.H.. Tanigawa. N.. Smith, D. & Craige, E.
(1987) Disparity between ejection and end-systolicindexes of left ven-
hyperosmolar solutions exert a direct, negative inotropic effect. tricular contractllity in mitral regurgitation. Circulation, 7 5 , 13 10-
Rat hearts (Langendorff preparation) infused with 7.5% NaC1, 1319.
with or without dextran, had depressed ventricular developed Beyer, T., Jepsen, L.S., Lullmann, H. & Ravens, U. (1986) Responses to
J. vet. Pharmacol. Therap. 17,211-217, 1994
Hypertonic saline and myocardial contractility 2 1 7
hypertonic solutions in guinea-pig atria: changes in action potentials, Nayler. W.G.(1961) Influence of hypertonic solutions on ventricular
force of contraction and calcium content. Journal of Molecular and contractile activity. American Journal of Physiology, 201,682-686.
Cellular Cardiology. 18.81-89. Newell, J.D.. Higgins. C.B., Kelley, M.J., Green. C.E., Schmidt, W.S. &
Bitterman. H., Triolo. J. & Lefer, A.M. (1987) Use of hypertonic saline in Haigler. F. (1980) The influence of hyperosmolality on left ventricular
the treatment of hemorrhagic shock. Circulatory Shock, 21,271-283. contractile state: disparate effects of nonionic and ionic solutions.
Brown, J.M., Grosso. M.A. & Moore, E.E. (1990) Hypertonic saline and Investigative Radiology, 1 5 , 363-3 70.
dextran: impact on cardiac function in the isolated rat heart. The Rocha-e-Silva. M.. Negraes, G.A., Soares, A.M., Pontieri. V. & Loppnow.
Journal of Trauma, 30, 646-650. L. (1986) Hypertonic resuscitation from severe hemorrhagic shock
Fisele. P.H., Talken, L. & Eisele. J.H. (1985) Potency of isoflurane and patterns of regional circulation. Circulatory Shock, 19, 165-1 75.
nitrous oxide in conventional swine. Laboratory Animal Science. 35, Sagawa. K.. Maughan, L., Suga. H. & Sunagawa, K. (1988) Cardiac
76-78. Contraction and Pressure-Volume Relationship. pp. 1-41. Oxford
Kass, D.A. & Maughan. W.L. (1988) From ‘Emax’ to pressure-volume University Press, Oxford.
relations: a broader view. Circulation, 77, 1203-1212. Schertel, E.R., Valentine, A.K., Rademakers, A.M. & Muir. W.W. (1990)
Kass, D.A., Yamazaki. T., BurkholT, D.. Maughan. W.L. & Sagawa. K. Influence of 7% NaCl on the mechanical properties of the systemic cir-
(1986) Determination of left ventricular end-systolic pressure-volume culation in the hypovolemic dog. Circulatory Shock, 31.203-2 14.
relationships by the conductance (volume) catheter technique. Schmall. L.M., Muir, W.W. & Robertson, J.T. (1990) Haemodynamic
Circulation. 73, 586-595. effects of small volume hypertonic saline in experimentally induced
Kass, D.A., Maughan. W.L.. Guo. Z.M.. Kono. A.. Sunagawa, K. & haemorrhagic shock. Equine Veterinary Journal. 2 2 , 2 73-277.
Sagawa, K. (1987) Comparative influence of load versus inotropic Tillisch, J.H. & Langer. G.A. (1974) Myocardial mechanical responses
states on indexes of ventricular contractility: experimental and theo- and ionic exchange in high-sodium perfusate. Circulation Research, 34,
retical analysis based on pressurevolume relationships. Circulation, 40-50.
76,1422-1436. Traverso. L.W.. Bellamy. R.F., Hollenbach, SJ. & Witcher, L.D. (1987)
Kass, D.A., Midei. M., Graves, W.. Brinker. J.A. & Maughan. W.L. (1988) Hypertonic sodium chloride solutions: effect on hemodynamics and
Use of a conductance (volume) catheter and transient inferior vena survival after hemorrhage in swine. The Journal of Trauma. 27.32-39.
caval occlusion for rapid determination of pressure-volume relation- Velasco, I.T.. Pontieri, V.. Rocha E Silva. M. & Lopes. O.U. (1980)
ships in man. Catheterization and Cardiovascular Diagnosis, 15, Hyperosmotic NaCl and severe hemorrhagic shock. American journal of
192-202. Physiology, 239. H664H673.
Kawata, H., Ohba. M.. Hatae. J. & Kishi, M. (1983) A study on the mecha- Wade, C.E.. Hannon. J.P., Bossone, C.A., Hunt, M.M.. Loveday. J.A.,
nism of twitch potentiation by hypertonic solution in the frog atrial Coppes, R. et al. (1989) Resuscitation of conscious pigs following hem-
muscle. Journal of Molecular and Cellular Cardiology, 15.28 1-293. orrhage: comparative efficacy of small-volume resuscitation.
Kentish. J.C. (1984) The inhibitory effects of monovalent ions on force Circulatory Shock, 29, 193-204.
development in detergent-skinned ventricular muscle from guinea-pig. Wildenthal. K., Miemiak. D.S. & Mitchell, J.H. (1969a) Acute effects of
journal ofPhysiology. 352, 353-374. increased serum osmolality on left ventricular performance. American
Kien. N.D.. Kramer. G.C. & White, D.A. (1991a) Acute hypotension Journal of Physiology. 216,898-904.
caused by rapid hypertonic saline infusion in anesthetized dogs. Wildenthal. K.. Skelton, C.L. & Coleman, H.N. (1969b) Cardiac muscle
Anesthesia Analgesia. 73, 597-602. mechanics in hyperosmotic solutions. American Journal of Physiology.
Kien. N.D.. Reitan, J.A., White. D.A.. Wu, C.H. & Eisele, J.H. (1991b) 217.302-306.
Cardiac Contractility and blood flow distribution following resuscita- Wddenthal, K.. Adcock. R.C., Crie. J.S., Templeton, G.H., Willerson. J.T.
tion with 7.5% hypertonic saline in anesthetized dogs. Circulatory (1975) Negative inotropic influence of hyperosmotic solutions on car-
Shock. 35, 109-116. diac muscle. American Journal oJPhysiology, 229. 1505-1 509.
Koch-Weser. J. (1963) Influence of osmolarity of perfusate on contractil- Willerson, J.T.. Crie. J.S., Adcock, R.C., Templeton. G.H. & Wildenthal, K.
ity of mammalian myocardium. American Journal of Physiology, 204, (1974) Influence of calcium on the inotropic actions of hyperosmotic
9 5 7-9 62. agents, norepinephrine, paired electrical stimulation, and treppe.
Liang, C.S. & Hood, W.B. (1978) Mechanism of cardiac output response lournal of Clinical Investigation. 54,957-964.
to hypertonic sodium chloride infusion in dogs. American Journal o/ Willerson. J.T., Wheelan, S.. Adcock, R.C., Templeton. G.H. & Wddenthal,
Physiology, 235, H18-H22. K. (1978) Species differences in responses to hyperosmolality and
Muir, W.W. 81Sally, J. (1989) Small-volume resuscitation with hyper- D600 in cat and rat heart. American Journal of Physiology, 235.
tonic saline solution in hypovolemic cats. American lournu1 of H276-H280.
Veterinary Research. 5 0 . 1883-1888. Younes, R.N.. Aun, F., Tomida, R.W. & Birolini. D. (1985) The role of
Nakayama, S., Sibley. L.. Gunther, R.A., Holcroft. J.W. & Kramer, G.C. lung innervation in the hemodynamic response to hypertonic sodium
(1984) Small-volume resuscitation with hypertonic saline (2.400 chloride solutions in hemorrhagic shock. Surgery, 98.900-906.
mOsm/Liter) during hemorrhagic shock. Circulatory Shock, 13,
149-159.
1. vet. Pharmacol. Therap. 17,211-217. 1994
You might also like
- Checklist For Cardiopulmonary ResuscitationDocument2 pagesChecklist For Cardiopulmonary Resuscitationvishnu100% (1)
- Acfrogas81a C3gdggyv4xgrao Mdfic3te - x187f1 87lztljhozqte1uwyasvd30we4h6qfxqnls Kkx4fhvgdzsyhiidv6ruak2jsebl1ta-o6xhpricpgy55ribskr1dafecu67-RbikzqhDocument126 pagesAcfrogas81a C3gdggyv4xgrao Mdfic3te - x187f1 87lztljhozqte1uwyasvd30we4h6qfxqnls Kkx4fhvgdzsyhiidv6ruak2jsebl1ta-o6xhpricpgy55ribskr1dafecu67-RbikzqhSiseneg Tasma100% (1)
- Nursing Care PlanDocument7 pagesNursing Care Planmcd7r883% (6)
- BiomechanicsDocument29 pagesBiomechanicsDrGurinder Kanwar100% (5)
- Gastric distension causes peripheral vasoconstriction in anaesthetized pigsDocument12 pagesGastric distension causes peripheral vasoconstriction in anaesthetized pigsHimanshu SharmaNo ratings yet
- Net Notes CardioDocument9 pagesNet Notes CardioJess PeltraNo ratings yet
- Standar Operasional ProsedurDocument10 pagesStandar Operasional ProsedurRitha MariaNo ratings yet
- Ajpheart 00081 2017Document13 pagesAjpheart 00081 2017jorge escobar pintoNo ratings yet
- 10 1124@jpet 106 116566Document10 pages10 1124@jpet 106 116566Caesar Catalin CaratasuNo ratings yet
- 1757 7241 21 86Document12 pages1757 7241 21 86Nicco MarantsonNo ratings yet
- Chronic Interactions Between Carotid Baroreceptors and Chemoreceptors in Obesity HypertensionDocument14 pagesChronic Interactions Between Carotid Baroreceptors and Chemoreceptors in Obesity HypertensionCaesar Catalin CaratasuNo ratings yet
- Effects of Saffan Cardiopulmonary in Healthy: FunctionDocument4 pagesEffects of Saffan Cardiopulmonary in Healthy: FunctionHocicos Y PatasNo ratings yet
- Anesthesia Case of The Month: HistoryDocument4 pagesAnesthesia Case of The Month: HistoryThomas GilangNo ratings yet
- Journals Javma 217 2 Javma.2000.217.231-PreviewDocument2 pagesJournals Javma 217 2 Javma.2000.217.231-PreviewJasna IsovićNo ratings yet
- Evolution of The Stone HeartDocument6 pagesEvolution of The Stone HeartHeitor PóvoasNo ratings yet
- ECG findings in a dog with pericardial effusion and cardiac tamponadeDocument5 pagesECG findings in a dog with pericardial effusion and cardiac tamponadeDewa Aix61No ratings yet
- Partial Extracorporeal Circulation in Acute Heart Failure : Naci M - Bor, M .DT and Andre P - Rieben, B .SDocument10 pagesPartial Extracorporeal Circulation in Acute Heart Failure : Naci M - Bor, M .DT and Andre P - Rieben, B .SGonzalo ReitmannNo ratings yet
- Effects of gravity inversion on blood pressure and eye pressureDocument5 pagesEffects of gravity inversion on blood pressure and eye pressurecookie “cookihakies” anonymeNo ratings yet
- Hemodynamic Monitoring in ShockDocument6 pagesHemodynamic Monitoring in Shockdiana25No ratings yet
- 2019 Journal of Surgical ResearchDocument8 pages2019 Journal of Surgical ResearchFernando ZanoniNo ratings yet
- 33 PDFDocument3 pages33 PDFZeptalanNo ratings yet
- 2020 Sanjeev Physiology International 2020Document15 pages2020 Sanjeev Physiology International 2020maloymandalNo ratings yet
- Comparison of 3% and 7.5% Hypertonic Saline in Resuscitation After Traumatic Hypovolemic ShockDocument6 pagesComparison of 3% and 7.5% Hypertonic Saline in Resuscitation After Traumatic Hypovolemic ShockTedja PrakosoNo ratings yet
- Severe pulmonary hypertension and heart abnormalities in a dog with lungworm infectionDocument4 pagesSevere pulmonary hypertension and heart abnormalities in a dog with lungworm infectionPutri AfrindaNo ratings yet
- Aortic Dissection Associated With Aortic Aneurysms and Posterior Paresis in A DogDocument7 pagesAortic Dissection Associated With Aortic Aneurysms and Posterior Paresis in A DogMuhamad Abdul MubdiNo ratings yet
- ajpheart.1985.249.4.h867Document9 pagesajpheart.1985.249.4.h867Rakibul HasanNo ratings yet
- 1 s2.0 S0741521495702881 MainDocument12 pages1 s2.0 S0741521495702881 MainRonald VillaNo ratings yet
- TolvaptanDocument10 pagesTolvaptanMARCIA VELECELANo ratings yet
- Human Physiological Responses To Immersion Into Water of Different TemperaturesDocument7 pagesHuman Physiological Responses To Immersion Into Water of Different TemperaturesMarcia FlorianiNo ratings yet
- PIIS0016508597003843Document8 pagesPIIS0016508597003843Mudassar SattarNo ratings yet
- Effect Artery Lingual Arterial In: BloodDocument3 pagesEffect Artery Lingual Arterial In: BloodPrashant AgrawalNo ratings yet
- Legal Medicine: Akina Nara, Toshihiko Aki, Takeshi Funakoshi, Kyoko Uchida, Haruka Nakayama, Koichi UemuraDocument3 pagesLegal Medicine: Akina Nara, Toshihiko Aki, Takeshi Funakoshi, Kyoko Uchida, Haruka Nakayama, Koichi Uemuradesta widayatNo ratings yet
- Gelafusin and Lactate RingerDocument5 pagesGelafusin and Lactate RingerMaaidamzNo ratings yet
- A Study of Echo in Patients With Rheumatic Mitral Stenosis and Normal Indian PerspectiveDocument4 pagesA Study of Echo in Patients With Rheumatic Mitral Stenosis and Normal Indian PerspectivemkmzafarNo ratings yet
- Evaluation of Diastolic Function With Doppler Echocardiography: The PDF FormalismDocument10 pagesEvaluation of Diastolic Function With Doppler Echocardiography: The PDF Formalismjhon contrerasNo ratings yet
- Acute Hypercalcemic Hypertension in Man: Role of Hemodynamics, Catecholamines, and ReninDocument5 pagesAcute Hypercalcemic Hypertension in Man: Role of Hemodynamics, Catecholamines, and ReninRo KohnNo ratings yet
- Ascites With Right Heart Failure in A Dog: Diagnosis and ManagementDocument5 pagesAscites With Right Heart Failure in A Dog: Diagnosis and ManagementairaNo ratings yet
- Paranjapeetal 2019PLRMpigsDocument10 pagesParanjapeetal 2019PLRMpigsCristina RamirezNo ratings yet
- Bove 1979Document8 pagesBove 1979Arthur PiresNo ratings yet
- The Nature of Hyperglycemia in Canine Anaphylactic ShockDocument15 pagesThe Nature of Hyperglycemia in Canine Anaphylactic ShockMihai StoicaNo ratings yet
- MainDocument11 pagesMainDhonz R AdiwaramanNo ratings yet
- Azotemia in Cats With Feline Hypertrophic Cardiomyopathy: Prevalence and Relationships With Echocardiographic VariablesDocument7 pagesAzotemia in Cats With Feline Hypertrophic Cardiomyopathy: Prevalence and Relationships With Echocardiographic VariablesJuan Fernando Herrera CiroNo ratings yet
- Ondan Hipo 3Document5 pagesOndan Hipo 3putri maharani andesNo ratings yet
- Hipertensión PortalDocument5 pagesHipertensión PortalJose Manuel Garcia RuedaNo ratings yet
- Doppler Study of Renal Circulation in Pregnancy HypertensionDocument7 pagesDoppler Study of Renal Circulation in Pregnancy HypertensionRizko Putra PradanaNo ratings yet
- Chronic Baroreflex Activation Restores Spontaneous Baroreflex Control and Variability of Heart Rate in Obesity-Induced HypertensionDocument10 pagesChronic Baroreflex Activation Restores Spontaneous Baroreflex Control and Variability of Heart Rate in Obesity-Induced HypertensionCaesar Catalin CaratasuNo ratings yet
- AUMENTAR MAP 65-85 No Mejorar Urina y LactatoDocument4 pagesAUMENTAR MAP 65-85 No Mejorar Urina y LactatoCurro InglesNo ratings yet
- Evolving Indications For Permanent PacemakersDocument12 pagesEvolving Indications For Permanent PacemakersJazmín Alejandra AGNo ratings yet
- Paper Valenti Et Al 1Document5 pagesPaper Valenti Et Al 1Érica Engrácia ValentiNo ratings yet
- Passive Leg Raising and Fluid Responsiveness Monnet CCM 2006Document6 pagesPassive Leg Raising and Fluid Responsiveness Monnet CCM 2006Leiniker Navarro ReyNo ratings yet
- Anaesthetic Management of Abdominal Aorta AneurysmDocument4 pagesAnaesthetic Management of Abdominal Aorta Aneurysmaswin febriaNo ratings yet
- Pi Is 0007091217435811Document6 pagesPi Is 0007091217435811Julio AltamiranoNo ratings yet
- CC 13182Document10 pagesCC 13182tendriayuNo ratings yet
- Hypoxia-Induced Coronary Flow Changes in The Perfused Rat Heart: Effects of High L-Carnitine ConcentrationsDocument5 pagesHypoxia-Induced Coronary Flow Changes in The Perfused Rat Heart: Effects of High L-Carnitine ConcentrationsNoemiNo ratings yet
- Europeanifmbembec2011 Submission 408Document4 pagesEuropeanifmbembec2011 Submission 408László DézsiNo ratings yet
- Li 1995Document5 pagesLi 1995Mumtaz MaulanaNo ratings yet
- Laparoscopic cholecystectomy neuroendocrine responsesDocument5 pagesLaparoscopic cholecystectomy neuroendocrine responsesRidski D. MiruNo ratings yet
- Adrenergic Response to Morphine-Diazepam AnesthesiaDocument6 pagesAdrenergic Response to Morphine-Diazepam Anesthesiajuan david castillo campoNo ratings yet
- Hipertonic SalineDocument7 pagesHipertonic SalineMARIA SALOMONNo ratings yet
- Brain Damage Following Severe Acute Normovolemic Hemodilution in Combination With Controlled Hypotension in RatsDocument7 pagesBrain Damage Following Severe Acute Normovolemic Hemodilution in Combination With Controlled Hypotension in RatsEvaldo MamedesNo ratings yet
- Potent Pressor Effect of Hypoxia in Sleep Apnea PatientsDocument6 pagesPotent Pressor Effect of Hypoxia in Sleep Apnea PatientsDiego SolaqueNo ratings yet
- Norepinephrine Kinetics and Dynamics in Septic Shock and Trauma PatientsDocument7 pagesNorepinephrine Kinetics and Dynamics in Septic Shock and Trauma PatientsMoh SuriyawalNo ratings yet
- Ideal Permissive Hypotension To Resuscitate Uncontrolled Hemorrhagic Shock and The Tolerance Time in RatsDocument9 pagesIdeal Permissive Hypotension To Resuscitate Uncontrolled Hemorrhagic Shock and The Tolerance Time in RatsSandara ParkNo ratings yet
- Central Venous Pressure: Its Clinical Use and Role in Cardiovascular DynamicsFrom EverandCentral Venous Pressure: Its Clinical Use and Role in Cardiovascular DynamicsNo ratings yet
- Kottner SeptDocument9 pagesKottner SeptliyaNo ratings yet
- Briefing On COVID 19 Autopsy Feb 2020 PDFDocument14 pagesBriefing On COVID 19 Autopsy Feb 2020 PDFliya100% (2)
- An Update On Treatment and Management of Pediatric SLEDocument11 pagesAn Update On Treatment and Management of Pediatric SLEArkina BalluweelNo ratings yet
- 01 GDL Maimunahni 764 1 Kti - Maim 9Document7 pages01 GDL Maimunahni 764 1 Kti - Maim 9fransiskaNo ratings yet
- Daftar Pustaka Dr. Tutty Ariani, SPDVDocument8 pagesDaftar Pustaka Dr. Tutty Ariani, SPDVliyaNo ratings yet
- PsikiatriDocument7 pagesPsikiatriliyaNo ratings yet
- Daftar Pustak1Document2 pagesDaftar Pustak1liyaNo ratings yet
- DfpusDocument9 pagesDfpusliyaNo ratings yet
- Balist 2Document2 pagesBalist 2liyaNo ratings yet
- 0034 7167 Reben 72 04 0889Document7 pages0034 7167 Reben 72 04 0889liyaNo ratings yet
- BalistikDocument11 pagesBalistikliyaNo ratings yet
- Melioidosis in The PhilippinesDocument12 pagesMelioidosis in The PhilippinesliyaNo ratings yet
- GagaljntungDocument9 pagesGagaljntungliyaNo ratings yet
- 1 SS Skin Cancer - Chapter 1Document12 pages1 SS Skin Cancer - Chapter 1Muhammad IqbalNo ratings yet
- 14 Asrar ElahiDocument9 pages14 Asrar ElahiliyaNo ratings yet
- Daftar Pustaka ObesDocument4 pagesDaftar Pustaka ObesliyaNo ratings yet
- Daftar Pustaka ObesDocument4 pagesDaftar Pustaka ObesliyaNo ratings yet
- Gastroenterology 4 1062Document4 pagesGastroenterology 4 1062darr artNo ratings yet
- Epidermolysis Bullosa Simplex: Case Report: Ernawati HidayatDocument5 pagesEpidermolysis Bullosa Simplex: Case Report: Ernawati HidayatliyaNo ratings yet
- HyperopiaDocument2 pagesHyperopialiyaNo ratings yet
- Henoch Schonlein in 535 Chineese - Youying Mao2014Document7 pagesHenoch Schonlein in 535 Chineese - Youying Mao2014liyaNo ratings yet
- Skripsi Tanpa Bab PembahasanDocument95 pagesSkripsi Tanpa Bab PembahasantymonNo ratings yet
- Are Acute Exacerbations of Chronic Inflammatory Appendicitis Triggered by Coprostasis And/or Coproliths?Document4 pagesAre Acute Exacerbations of Chronic Inflammatory Appendicitis Triggered by Coprostasis And/or Coproliths?liyaNo ratings yet
- Jones Et Al-1983-Journal of Ultrasound in Medicine PDFDocument5 pagesJones Et Al-1983-Journal of Ultrasound in Medicine PDFliyaNo ratings yet
- Medico-legal risks in travel medicineDocument3 pagesMedico-legal risks in travel medicineliyaNo ratings yet
- DM PamfletDocument2 pagesDM PamfletliyaNo ratings yet
- Botulinum Toxin: (Botulism)Document3 pagesBotulinum Toxin: (Botulism)liyaNo ratings yet
- 201 279 1 SMDocument4 pages201 279 1 SMliyaNo ratings yet
- Medico LegalcasesneedamoreprofessionalapproachDocument4 pagesMedico LegalcasesneedamoreprofessionalapproachliyaNo ratings yet
- Psychology Canadian 2nd Edition Ciccarelli Test BankDocument42 pagesPsychology Canadian 2nd Edition Ciccarelli Test BankMichaelAllenrazne100% (10)
- San Pablo City Earth and Life Science Diagnostic TestDocument2 pagesSan Pablo City Earth and Life Science Diagnostic TestFermin Artificio Clorado Jr.No ratings yet
- Focused Neurological AssessmentDocument23 pagesFocused Neurological AssessmentNabil Abd El-tawab100% (1)
- Kinesiology of Shoulder Complex MusclesDocument7 pagesKinesiology of Shoulder Complex MusclesAlya Putri KhairaniNo ratings yet
- Drug StudyDocument4 pagesDrug Studysilverblade36No ratings yet
- ANAPHY Lec Session #4 - SAS (Agdana, Nicole Ken)Document10 pagesANAPHY Lec Session #4 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNo ratings yet
- Newborn Resuscitation GuidelinesDocument7 pagesNewborn Resuscitation GuidelinesYwagar YwagarNo ratings yet
- Test Bank For Principles of Anatomy and Physiology 15th Edition by TortoraDocument24 pagesTest Bank For Principles of Anatomy and Physiology 15th Edition by TortoraKennethGarciabqej100% (35)
- Endocrine Physiology LaboratoryDocument1 pageEndocrine Physiology LaboratoryRizza Mae Salvania100% (1)
- Overview of The Immune System 2020Document31 pagesOverview of The Immune System 2020mehakNo ratings yet
- 5.6 Muscle Energy Techniques For The Pelvis 167-171Document5 pages5.6 Muscle Energy Techniques For The Pelvis 167-171maricartiNo ratings yet
- Bacteriophages Taxonomy and ClassificationDocument9 pagesBacteriophages Taxonomy and ClassificationTariq MunirNo ratings yet
- GCE Biology Marking SchemeDocument33 pagesGCE Biology Marking SchemeRabea2222sweetandsouNo ratings yet
- Baqri&Coomans 1973 - Dorylaimida Descritos Por Stekhoven y Teunissen 1938Document57 pagesBaqri&Coomans 1973 - Dorylaimida Descritos Por Stekhoven y Teunissen 1938Miguelillo_HernandezNo ratings yet
- Bile NotesDocument1 pageBile NotesRichel Ameryl DasocNo ratings yet
- Borg Scale in Strength TrainingDocument11 pagesBorg Scale in Strength TrainingCésar Ayala Guzmán100% (1)
- Session #34 SAS - AnaPhy (Lab)Document7 pagesSession #34 SAS - AnaPhy (Lab)Cristina SottoNo ratings yet
- Neuroimaging in Mild Traumatic Brain Injury: # Springer Science+Business Media, LLC 2010Document14 pagesNeuroimaging in Mild Traumatic Brain Injury: # Springer Science+Business Media, LLC 2010Sara Gonzalo RodríguezNo ratings yet
- Bloodborne Script FormattedDocument74 pagesBloodborne Script FormattedRooWWNo ratings yet
- Proper Posture and AlignmentDocument3 pagesProper Posture and Alignmentschorleworle100% (1)
- University of Gondar College of Medicine and Health Sciences Department of Medical PhysiologyDocument202 pagesUniversity of Gondar College of Medicine and Health Sciences Department of Medical PhysiologyGifti DemisseNo ratings yet
- Medical Surgical Nursing Exam 19 NLE Style 100 Items Nurseslabs December 2012 NLE ResultsDocument21 pagesMedical Surgical Nursing Exam 19 NLE Style 100 Items Nurseslabs December 2012 NLE ResultsKaren Ann M. Estrada100% (1)
- Your Peak Flow Diary PDFDocument11 pagesYour Peak Flow Diary PDFkalli987No ratings yet
- Hold the foot firmly in dorsiflexion to relax the gastrocnemiusmuscle and expose the Achilles tendon fullyDocument13 pagesHold the foot firmly in dorsiflexion to relax the gastrocnemiusmuscle and expose the Achilles tendon fullyNurul Huda M ShahrinNo ratings yet
- Chapter 1: Introduction To Motivation and EmotionDocument9 pagesChapter 1: Introduction To Motivation and EmotionElla Rene MartinNo ratings yet
- Grade 9 Biology - Lesson Note April 8,2020Document10 pagesGrade 9 Biology - Lesson Note April 8,2020micahxNo ratings yet