Professional Documents
Culture Documents
Hemolysis in Serum Samples Drawn by Emergency Department Personnel Versus Laboratory Phlebotomists
Uploaded by
muhammadhanifmohdfahmiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hemolysis in Serum Samples Drawn by Emergency Department Personnel Versus Laboratory Phlebotomists
Uploaded by
muhammadhanifmohdfahmiCopyright:
Available Formats
왗your lab focus 왘
science [phlebotomy | blood banking/transfusion medicine | coagulation and hematology]
Hemolysis in Serum Samples Drawn by
Emergency Department Personnel versus
Laboratory Phlebotomists
Edward R. Burns, MD, Noriko Yoshikawa, MD
Department of Pathology, Albert Einstein College of Medicine and Montefiore Medical Center, New York, NY
왘 The study examined the rates of found when the following parameters were over the role of the pneumatic-tube sys-
hemolysis in 2 sample populations compared: distal arm draw versus antecu- tems in hemolysis. Studies have shown
and compared the techniques used bital fossa draw (P=0.0054), 22 gauge plas- that parameters such as hemoglobin,
to draw blood. tic cannula versus 20 gauge cannula potassium, LDH, and acid phosphatase,
왘 The frequency of hemolysis was (P=0.0104), less than half-full tube draw chosen as markers for hemolysis, rise in
significantly higher in the samples versus greater than or equal half-full tube samples transported through pneumatic-
coming from the Emergency draw (P=0.0159), tourniquet compression tube systems, particularly if the specimen
Department (ED). time of greater than 2 minutes versus less tubes are less than half full, or if the spec-
than or equal 2 minutes (P=0.016), and plas- imens were sent though the system re-
Pre-analytic mechanical hemolysis of tic versus metal cannulas (P=0.0164). Lo- peatedly.6,8-10 Other studies have found
blood samples can lead to inaccurate labo- gistic regression of these data to control for that potassium, LDH, and serum hemo-
ratory results. It can cause spuriously ele- confounding variables demonstrated that the globin are not altered when blood is sent
vated levels of potassium, lactate following factors contributed most to caus- through pneumatic tubes.4,5,7 Variability
dehydrogenase (LDH), and other analytes. ing mechanical hemolysis: drawing from a in results may result from system differ-
We examined the rates of hemolysis in 2 vein in the distal arm and drawing through a ences in properties such as length, speed,
sample populations, a hospital medical narrower gauge needle. Use of a standard- acceleration, and number of turns.
ward and an emergency department, and ized protocol for blood drawing can reduce Observations by treating physicians
compared the techniques used to draw the rate of pre-analytic hemolysis by more and clinical laboratory staff suggest that
blood in order to determine which factors than 7-fold. Drawing blood from the antecu- the rate of hemolysis in samples drawn in
play a true role in causing excess mechani- bital fossa using a needle of 20 gauge or emergency departments exceeds those
cal hemolysis. more can best reduce hemolysis. drawn by professional laboratory phle-
We calculated the rate of hemolysis in botomists. We examined the rates of he-
4,021 patients. We then examined 202 pro- Background molysis in these 2 sample populations
cedures for various factors involved in the Pre-analytic mechanical hemolysis of and compared the techniques used to
blood drawing process to determine blood samples can lead to inaccurate lab- draw blood in order to determine which
which, if any, have an increased chance of oratory results and delays in patient care. factors play a role in causing excess pre-
causing mechanical hemolysis. These in- Hemolysis may result in spuriously ele- analytical hemolysis.
cluded needle gauge and material, site of vated serum potassium and bilirubin, as
venipuncture, tourniquet compression well as acid phosphatase, zinc, magne- Materials and Methods
time, level of tube fill, use of Vacutainer or sium, albumin, and creatine kinase (CK).1 The study received approval from the
syringe, and the use of extension tubing. There are various external factors that medical center institutional review board.
The contributions of the various processes may cause hemolysis, including the The first part of the study involved a vali-
to hemolysis were compared using chi- gauge of the cannula and the pressure dation of the casual observation of
square analysis and Fisher’s exact test. Lo- exerted on the blood at the time of draw- increased frequency of hemolysis
gistic regression was then used to best ing.2,3 A syringe can generate enough observed in specimens drawn in the ED
378 model those factors that are most likely to pressure to cause hemolysis when used compared to those from a non-emergency
produce mechanical hemolysis. with a large bore needle.2 Syringes are department setting. We performed a retro-
The rate of hemolysis among capable of creating a higher pressure dif- spective analysis of data on 2,992 chem-
emergency department drawn specimens ferential than a Vacutainer, leading to istry panels from the ED and 1,029 from
was 12.4% versus 1.6% for those drawn by more hemolysis in vitro.2 Hemolysis may a routine medicine ward in an acute care
laboratory personnel (P<0.0001). Statisti- also result from mechanical trauma oc- teaching hospital over a period of 11
cally significant differences in the rate of curring during transport to the clinical weeks. The total number of specimens
hemolysis (ie, greater hemolysis) were laboratory. There has been much debate analyzed was culled from the laboratory
laboratorymedicine> may 2002> number 5> volume 33 ©
Downloaded from https://academic.oup.com/labmed/article-abstract/33/5/378/2657228
by guest
on 31 March 2018
왗your lab focus 왘
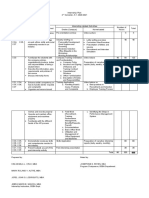
information system. The number of he- Hemolysis in association with individual parameters.
molyzed samples was determined by in-
vestigating the “Daily Comment Logs” Parameters n # hemolyzed P-value/test
T1
for the “hemolysis” comment in the com-
puter that identifies rejected specimens as Antecubital 94 4 0.0054
analytically unacceptable. These logs in- distal arm 100 18 Chi-squared
clude the department from which each of 22G-IV 33 10 0.0123
the hemolyzed samples originated. 20G-IV 115 12 Chi-squared
Prior to beginning the study, the abil- <1/2 full 70 13 0.0159
ity of the technologists to properly identify >1/2 full 128 8 Chi-squared
hemolysis was ascertained. A sample of Plastic 163 22 0.0164
whole blood was hemolyzed with ammo- Metal 37 0 Fisher’s
nium chloride and the serum was Extension 77 7 0.68
separated. Ten serial dilutions of the no extension 125 15 Chi-squared
clearly hemolyzed serum were made using syringe 10 1 1.0
normal non-hemolyzed serum as the dilu- no syringe 192 21 Fisher’s
ent. The samples thus ranged from normal
through grossly hemolyzed as ascertained
by spectrophotometric analysis at the he- catheter gauge, fullness of the tubes, and Logistic regression of these data was
moglobin peak absorption wavelength. use of the extension tubing were analyzed used to control for confounding variables.
Each technologist involved in the study using chi-squared test. Fisher’s exact prob- The site, fullness, and catheter material
was tested and certified as to their ability ability test was used for tourniquet time, were included in the analysis. Catheter
to properly identify the presence of hemol- catheter material, and use of the syringe. gauge was excluded because of its relation
ysis. The percentages of hemolyzed sam- to the catheter material type, all of the
ples from the medical ward and the ED Results catheters being plastic. Logistic regression
were compared. Data were analyzed using by SAS software demonstrated that the
the chi-squared test. Comparison of ED to Medical Floor following factors contributed most to caus-
The second part of the study exam- A total of 4,021 samples were ing mechanical hemolysis: 1) drawing
ined possible causes of hemolysis. We di- reviewed. Hemolysis was considerably from a vein in the distal arm (P=0.034),
rectly observed 204 blood drawings in the more frequent in the ED samples. Of the and 2) the fullness of the tube (P=0.026).
ED of the hospital. The study population 2,992 blood drawings from the ED, 372
included any patient who came into the (12.4%) were hemolyzed. Of the 1,029 Discussion
ED needing chemistry work. This included samples from the medical floor, 16
pediatric patients. No patient demograph- (1.6%) were hemolyzed (P<0.0001). ED vs Medical Floor
ics other than sample number were The frequency of hemolysis was sig-
recorded. Only red top tubes drawn for Phlebotomy Technique Analysis nificantly higher in the samples coming
chemistry panels were included in the Chi-squared analysis showed that the from the ED. Blood samples from the
study. Blood samples were drawn by either occurrence of hemolysis in samples medical floor were predominantly drawn
ED nurses or technicians. Cannula type drawn through 20 gauge plastic catheters by trained phlebotomists who used
and gauge were left to the discretion of the was less [T1] than that from 22 gauge straight Vacutainer needles and butterflies
nurse or technician who drew the sample, catheters (P=0.0123). Hemolysis from and transported the blood to the labora-
as was the site of puncture. The type and plastic catheters versus metal needles tory by hand. These individuals had all
gauge of the cannula, use of extension (butterflies or straight) was significantly undergone formal training and certifica-
piece or syringe, and site of puncture were greater (P=0.0164). Chi-squared analysis tion in blood drawing techniques. In con-
recorded. The level to which the Vacutain- of hemolysis in blood samples drawn trast, the blood samples from the ED
ers were filled was determined by compar- from the antecubital fossa (AC) was less were largely drawn through plastic
ison to a reference tube that was filled with than from those drawn distal to the ante- catheters and were transported via pneu-
water and marked in milliliter graduations. cubital fossa (P=0.0054). The fullness of matic tube. The ED phlebotomists were 379
All samples were transported to the chem- the sample tubes, less than half versus trained in the ED and were not certified.
istry laboratory by pneumatic tubes. The greater than or equal to half, was also The site of puncture in the phlebotomist
endpoint of hemolysis was determined by significant (P=0.0159); the fuller tubes drawn group was primarily in the antecu-
the chemistry laboratory technician. We showing less hemolysis. Use of extension bital fossa as opposed to the ED group
reviewed The “Daily Comment Logs” to tubing or a syringe during blood drawing which was more distal. Although inade-
determine which samples were labeled as did not effect the occurrence of hemolysis quately documented, this may be a source
“hemolyzed.” Results of the site, IV (P=0.68, P=1.00). of variation between the 2 groups.
© laboratorymedicine> may 2002> number 5> volume 33
Downloaded from https://academic.oup.com/labmed/article-abstract/33/5/378/2657228
by guest
on 31 March 2018
왗your lab focus 왘
Observed Technique Study The barriers to reducing hemolysis 2. Sharp MK, Mohammad SF. Scaling of hemolysis
Although the chi-squared analysis include personal preference and feasibil- in needles and catheters. Ann of Biomedical
Engineering. 1998;26:788-797.
showed plastic vs metal cannulas as ity. It is common in emergency medicine
3. Kennedy C, Angemuller S, King R, et al. A
being significantly different, the logistic to draw blood samples from the distal
comparison of hemolysis rates using intravenous
regression analysis showed this factor arm when placing IVs to reduce the num- catheters versus venipuncture tubes for obtaining
to be noncontributory. Logistic regres- ber of venipunctures. Emergency depart- blood samples. J Emerg Nursing.
sion analysis revealed that the key vari- ment personnel avoid placing the IV in 1996;22(6):566-569.
ables were site of draw and fullness of the antecubital fossa because of the possi- 4. Greendyke RM, Banzhaf JC, Pelysko S, et al.
the tubes. The antecubital fossa may be bility of the catheter bending and Immunologic studies of blood samples
transported by a pneumatic tube system. Am J
more favorable than the distal arm be- obstructing infusions when the patient Clin Pathol. 1976;68(4):508-510.
cause of the faster flow due to its in- moves their arm. They are more likely to
5. Stair TO, Howell JM, Fitzgerald DJ, et al.
creased diameter and reduced draw blood from the distal arm. Likewise, Hemolysis of blood specimens transported from
resistance. In addition, smaller cannulas it may be difficult to fill a specimen tube ED to laboratory by pneumatic tube. Am J
may be used for distal blood draws. The despite one’s best efforts. Emergency Med. 1995;13(4):484.
fullness of the tubes may affect hemol- Use of a standardized protocol for 6. Steige H, Jones JD. Evaluation of pneumatic-tube
ysis through the poorly understood ef- blood drawing can reduce the rate of pre- system for deliver of blood specimens. Clin Chem.
1971;17(12):1160-1164.
fect of pneumatic tube transportation. analytic hemolysis by more than 7-fold.
7. Poznanski W, Smith F, Bodley F. Implementation
Further investigation is necessary to Hemolysis can best be reduced by draw-
of a pneumatic-tube system for transport of blood
elucidate the causes. ing blood from the antecubital fossa and specimens. Am J Clin Pathol. 1977;70:291-295.
The endpoint for hemolysis used in by completely filling the tube 8. Pragay DA, Edwards L, Toppin M, et al.
this study, though not quantifiable, is true Evaluation of an improved pneumatic-tube system
to life. Samples are rejected not because Acknowledgements suitable for transportation of blood specimens.
their spectrophotometer reading indicates We would like to thank the staff of the Clin Chem. 1974;20(1): 57-60.
excessive hemolysis, but because the Einstein-Weiler Hospital Emergency De- 9. Weaver DK, Miller D, Leventhal EA, et al.
Evaluation of a computer-directed pneumatic-tube
technician perceives it to be hemolyzed. partment for their cooperation and support.
system for pneumatic transport of blood
Newer clinical chemistry analyzers have specimens. Am J Clin Pathol. 1977;70:400-405.
built in “hemolysis” flags that reject spec- 1. Henry JB. Clinical Diagnosis and Management by 10. Pragay DA, Fan P, Brinkley S, et al. A computer
imens that exceed a predetermined spec- Laboratory Methods. 19th Edition, Philadelphia: directed pneumatic tube system: Its effects on
trophotometric standard for hemolysis. PA: W.B. Saunders Co, 1996. specimens. Clin. Biochem. 1980;13(6):259-261.
380
laboratorymedicine> may 2002> number 5> volume 33 ©
Downloaded from https://academic.oup.com/labmed/article-abstract/33/5/378/2657228
by guest
on 31 March 2018
You might also like
- Aqx 082Document6 pagesAqx 082Hedo HidayatNo ratings yet
- Int J Lab Hematology - 2021 - Kitchen - International Council For Standardization in Haematology ICSH Recommendations ForDocument12 pagesInt J Lab Hematology - 2021 - Kitchen - International Council For Standardization in Haematology ICSH Recommendations ForLaboratorium RS BELLANo ratings yet
- The Effect of Blood DrawingDocument6 pagesThe Effect of Blood Drawingrince noveliaNo ratings yet
- Lippi 2018Document6 pagesLippi 2018Harika PutraNo ratings yet
- Serum Indices 2Document12 pagesSerum Indices 2mgaNo ratings yet
- Erythrocyte Sedimentation Rate Journey Verifying A New Method For An Imperfect TestDocument3 pagesErythrocyte Sedimentation Rate Journey Verifying A New Method For An Imperfect TestRina ErlinaNo ratings yet
- Recommendations For Processing of Blood Samples For Coagulation TestingDocument12 pagesRecommendations For Processing of Blood Samples For Coagulation TestingRandy HuyhuaNo ratings yet
- Impact of Low Volume Citrate Tubes On Results of First Line Hemostasis TestingDocument6 pagesImpact of Low Volume Citrate Tubes On Results of First Line Hemostasis TestingSidney WatersNo ratings yet
- Platelet Counting by The Coulter LH 750, Sysmex XE 2100Document7 pagesPlatelet Counting by The Coulter LH 750, Sysmex XE 2100blanket_thNo ratings yet
- Erroneous Automated Optical Platelet Counts PDFDocument8 pagesErroneous Automated Optical Platelet Counts PDFfar faraNo ratings yet
- HarrisADVIA2120methods LabHema2005 11 47-61 PDFDocument16 pagesHarrisADVIA2120methods LabHema2005 11 47-61 PDFSilvânia RochaNo ratings yet
- Test-1 Analyzer and Conventional Westergren Method For Erythrocyte Sedimentation Rate: A Comparative Study Between Two LaboratoriesDocument6 pagesTest-1 Analyzer and Conventional Westergren Method For Erythrocyte Sedimentation Rate: A Comparative Study Between Two LaboratoriesSyarifah Tridani FitriaNo ratings yet
- HarrisADVIA2120methods LabHema2005 11 47-61 PDFDocument16 pagesHarrisADVIA2120methods LabHema2005 11 47-61 PDFedu_14cNo ratings yet
- Preanalytical ErrorsDocument3 pagesPreanalytical Errorspieterinpretoria391No ratings yet
- Bruegel 2015Document15 pagesBruegel 2015my accountNo ratings yet
- PG Lab 2 VenipunctureDocument26 pagesPG Lab 2 VenipunctureFlordabee Mercurio PaniaguaNo ratings yet
- Jurnal VaskularDocument5 pagesJurnal VaskulardrelvNo ratings yet
- Quality Standards For Sample Processing, Transportation, and Storage in Hemostasis TestingDocument11 pagesQuality Standards For Sample Processing, Transportation, and Storage in Hemostasis TestingGunay AliyevaNo ratings yet
- BiochemMed2019 01Document6 pagesBiochemMed2019 01iq_dianaNo ratings yet
- CQ HematoDocument8 pagesCQ HematoRizky Pratama NurhakimNo ratings yet
- PIV Blood DrawsDocument7 pagesPIV Blood Drawsphidelt649No ratings yet
- Clinical BiochemistryDocument25 pagesClinical Biochemistrymirzafahad82005No ratings yet
- Venous Blood CollectionDocument4 pagesVenous Blood CollectionSheila Mae BuenavistaNo ratings yet
- Berk Ow 2013Document10 pagesBerk Ow 2013langit rizki yuditamaNo ratings yet
- Blood Wastage in A Tertiary Hospital Laboratory in Tacloban CityDocument25 pagesBlood Wastage in A Tertiary Hospital Laboratory in Tacloban CityralfNo ratings yet
- Albumin Change in 24 HoursDocument6 pagesAlbumin Change in 24 HoursfloNo ratings yet
- HEMOLYSISDocument2 pagesHEMOLYSISchandra-vinnakotaNo ratings yet
- Bai 2008Document8 pagesBai 2008Rahadian FaisalNo ratings yet
- Point of Care Hematocrit and Hemoglobin in Cardiac Surgery-A ReviewDocument6 pagesPoint of Care Hematocrit and Hemoglobin in Cardiac Surgery-A ReviewDiego AngelesNo ratings yet
- Preanalytical Variables and Their Influence On The Quality of Laboratory ResultsDocument4 pagesPreanalytical Variables and Their Influence On The Quality of Laboratory Resultsapi-165321926No ratings yet
- Evaluation of The Abbott CELL-DYN 4000 HematologyDocument10 pagesEvaluation of The Abbott CELL-DYN 4000 Hematologypasamuco473No ratings yet
- Adiga, U., Yogish, S., 2016, Hemolytic Index - A Tool To Measure Hemolysis inDocument4 pagesAdiga, U., Yogish, S., 2016, Hemolytic Index - A Tool To Measure Hemolysis inanisahfauziyyahNo ratings yet
- Guidance For Storing Blood Samples in Laboratories Performingcomplete Blood Count With DifferentialDocument6 pagesGuidance For Storing Blood Samples in Laboratories Performingcomplete Blood Count With Differentialimran ahmed siddiquiNo ratings yet
- Study 2Document7 pagesStudy 2Suyash BagdeNo ratings yet
- 2 Ijmpsapr20172Document6 pages2 Ijmpsapr20172TJPRC PublicationsNo ratings yet
- Lmy 030Document7 pagesLmy 030Tuan NguyenNo ratings yet
- TechTalk HemolysisDocument2 pagesTechTalk HemolysisARIF AHAMMED P0% (1)
- Comparison of Point-of-Care Measurement of Electrolyte Concentrations On Calculations of The Anion Gap and The Strong Ion DifferenceDocument8 pagesComparison of Point-of-Care Measurement of Electrolyte Concentrations On Calculations of The Anion Gap and The Strong Ion DifferenceMuhammad DaffaNo ratings yet
- HemaDocument5 pagesHemaAra Christine AnchetaNo ratings yet
- Hematologia Del RatónDocument17 pagesHematologia Del RatónRodrigo Ignacio Gacitúa OpazoNo ratings yet
- Stability Whole Blood SamplesDocument2 pagesStability Whole Blood Samplessabin shaikNo ratings yet
- IndianJPatholOncol 7 4 625 630Document6 pagesIndianJPatholOncol 7 4 625 630Yaser MNo ratings yet
- Peripheral Blood Smear Pathologist ToolDocument3 pagesPeripheral Blood Smear Pathologist ToolSimon HafeniNo ratings yet
- Jurnal Alin Poct Dipstk UrineDocument9 pagesJurnal Alin Poct Dipstk Urineherlina armarianiNo ratings yet
- Cost Analysis of A Neonatal Point-of-Care MonitorDocument10 pagesCost Analysis of A Neonatal Point-of-Care MonitorMARIO LOPEZ VILLAMILNo ratings yet
- Cornes 2016Document5 pagesCornes 2016servicio kendalNo ratings yet
- Autologous Blood Salvage in Cardiac Surgery: Clinical Evaluation, Efficacy and Levels of Residual HeparinDocument8 pagesAutologous Blood Salvage in Cardiac Surgery: Clinical Evaluation, Efficacy and Levels of Residual HeparinjavelezhNo ratings yet
- Clinical Laboratory Quality Practices When Hemolysis OccursDocument6 pagesClinical Laboratory Quality Practices When Hemolysis OccursFelia AkasehNo ratings yet
- AARC Clinical Practice Guideline Blood Gas Analysis and Hemoximetry 2013.Document14 pagesAARC Clinical Practice Guideline Blood Gas Analysis and Hemoximetry 2013.Madalina TalpauNo ratings yet
- Namrata Bhutani-I-Mar 9Document4 pagesNamrata Bhutani-I-Mar 9Hedo HidayatNo ratings yet
- Use of Fresh Blood For Quality Control: Erythrocyte Sedimentation RateDocument6 pagesUse of Fresh Blood For Quality Control: Erythrocyte Sedimentation RateTriana AmaliaNo ratings yet
- 179-Article Text-723-2-10-20200606Document7 pages179-Article Text-723-2-10-20200606Laboratorium RS BELLANo ratings yet
- 10 0000@www Jrheum Org@32@5@828Document5 pages10 0000@www Jrheum Org@32@5@828Yasser AlghrafyNo ratings yet
- Impact of Hemodialysis On Bleeding Tendency in End Stage Renal DiseaseDocument7 pagesImpact of Hemodialysis On Bleeding Tendency in End Stage Renal DiseasedrosabryNo ratings yet
- Hasanin 2021Document8 pagesHasanin 2021Ammon10famNo ratings yet
- 02.99.055 (PDF Library)Document3 pages02.99.055 (PDF Library)Muthu KumarNo ratings yet
- Hemolysis Area: A New Parameter of Erythrocyte Osmotic Fragility For Screening of Thalassemia TraitDocument9 pagesHemolysis Area: A New Parameter of Erythrocyte Osmotic Fragility For Screening of Thalassemia Traitjunita abbasNo ratings yet
- Haematologist-Reviewed Peripheral Blood Smear in PDocument6 pagesHaematologist-Reviewed Peripheral Blood Smear in PElba AlvarezNo ratings yet
- Effect of Squeezing On The Fingertip During Capillary Blood Collection To The Laboratory Analysis ResultsDocument8 pagesEffect of Squeezing On The Fingertip During Capillary Blood Collection To The Laboratory Analysis Resultsfardiah tilawatiNo ratings yet
- Hanif - Feqah - IbadahDocument4 pagesHanif - Feqah - IbadahmuhammadhanifmohdfahmiNo ratings yet
- Laisal GhareebDocument4 pagesLaisal GhareebmuhammadhanifmohdfahmiNo ratings yet
- As A PHD Examiner My Top 25 Tips For PHD StudentsDocument16 pagesAs A PHD Examiner My Top 25 Tips For PHD StudentsmuhammadhanifmohdfahmiNo ratings yet
- Peppa With Mummy Coloring Page - Free Printable Coloring PagesDocument1 pagePeppa With Mummy Coloring Page - Free Printable Coloring PagesmuhammadhanifmohdfahmiNo ratings yet
- As A PHD Examiner My Top 25 Tips For PHD StudentsDocument16 pagesAs A PHD Examiner My Top 25 Tips For PHD StudentsmuhammadhanifmohdfahmiNo ratings yet
- Topic 1 PDFDocument18 pagesTopic 1 PDFmuhammadhanifmohdfahmiNo ratings yet
- Trizol InfographicsDocument1 pageTrizol InfographicsmuhammadhanifmohdfahmiNo ratings yet
- Prepositions of Time (At - in - On) - Print - QuizizzDocument4 pagesPrepositions of Time (At - in - On) - Print - QuizizzmuhammadhanifmohdfahmiNo ratings yet
- New ZDocument131 pagesNew ZmuhammadhanifmohdfahmiNo ratings yet
- Guidelines HFMD 2007 PDFDocument135 pagesGuidelines HFMD 2007 PDFnght7942No ratings yet
- Guidelines HFMD 2007 PDFDocument135 pagesGuidelines HFMD 2007 PDFnght7942No ratings yet
- ALUMNI Poster 2Document1 pageALUMNI Poster 2muhammadhanifmohdfahmiNo ratings yet
- Capillary Blood CollectionDocument8 pagesCapillary Blood CollectionARIF AHAMMED P100% (1)
- 10 Tips For Reviewing Scientific Manuscripts - and 5 Red FlagsDocument2 pages10 Tips For Reviewing Scientific Manuscripts - and 5 Red FlagsmuhammadhanifmohdfahmiNo ratings yet
- Direct IndirectDocument5 pagesDirect IndirectmuhammadhanifmohdfahmiNo ratings yet
- Phlebotomy Tourniquets - Vectors For Bacterial Pathogens - Kane Et AlDocument2 pagesPhlebotomy Tourniquets - Vectors For Bacterial Pathogens - Kane Et AlmuhammadhanifmohdfahmiNo ratings yet
- 3 - Poster Phlebotomy Workshop-1Document1 page3 - Poster Phlebotomy Workshop-1muhammadhanifmohdfahmiNo ratings yet
- Purdue Owl - Apa StyleDocument53 pagesPurdue Owl - Apa StylemuhammadhanifmohdfahmiNo ratings yet
- Final Ichase17 Tentative ProgrammeDocument1 pageFinal Ichase17 Tentative ProgrammemuhammadhanifmohdfahmiNo ratings yet
- Logo For Ichase17Document5 pagesLogo For Ichase17muhammadhanifmohdfahmiNo ratings yet
- First Steps Improv PhlebotomyDocument44 pagesFirst Steps Improv PhlebotomymuhammadhanifmohdfahmiNo ratings yet
- Participant: Parking Lot Beside Fsk6 BuildingDocument1 pageParticipant: Parking Lot Beside Fsk6 BuildingmuhammadhanifmohdfahmiNo ratings yet
- Purdue Owl - Apa StyleDocument53 pagesPurdue Owl - Apa StylemuhammadhanifmohdfahmiNo ratings yet
- APA Referencing 6th Ed Quick GuideDocument2 pagesAPA Referencing 6th Ed Quick GuidehartymNo ratings yet
- FSK Infographic 2016 - Page 1Document1 pageFSK Infographic 2016 - Page 1muhammadhanifmohdfahmiNo ratings yet
- Abnormal RbcsDocument1 pageAbnormal RbcsmuhammadhanifmohdfahmiNo ratings yet
- Hub ColourDocument1 pageHub ColourmuhammadhanifmohdfahmiNo ratings yet
- Policy Phlebotomy Blood CollectionDocument6 pagesPolicy Phlebotomy Blood CollectionmuhammadhanifmohdfahmiNo ratings yet
- FSK Infographic 2016 - Page 2Document1 pageFSK Infographic 2016 - Page 2muhammadhanifmohdfahmiNo ratings yet
- A Grammar of Power in Psychotherapy Exploring The Dynamics of Privilege (Malin Fors)Document220 pagesA Grammar of Power in Psychotherapy Exploring The Dynamics of Privilege (Malin Fors)Andrea A. Ortiz Vázquez100% (1)
- Internship-Plan BSBA FInalDocument2 pagesInternship-Plan BSBA FInalMark Altre100% (1)
- Cognitive Behavioral Therapy - 7 Ways To Freedom From Anxiety, Depression, and Intrusive Thoughts (Happiness Is A Trainable, Attainable Skill! Book 1)Document105 pagesCognitive Behavioral Therapy - 7 Ways To Freedom From Anxiety, Depression, and Intrusive Thoughts (Happiness Is A Trainable, Attainable Skill! Book 1)SOUFIANE RACHID100% (8)
- Khalifa NagwaDocument111 pagesKhalifa NagwajokonudiNo ratings yet
- Is 228 (Part 1) : 1987 Methods For Chemical Analysis Of: (Reaffirmed 2008)Document5 pagesIs 228 (Part 1) : 1987 Methods For Chemical Analysis Of: (Reaffirmed 2008)Indira BanerjeeNo ratings yet
- Princess Joy Placement and General Services vs. BinallaDocument2 pagesPrincess Joy Placement and General Services vs. Binallaapple_doctoleroNo ratings yet
- The European Board of Anaesthesiology.2Document4 pagesThe European Board of Anaesthesiology.2readririNo ratings yet
- RPLB NewDocument22 pagesRPLB NewMeta learnNo ratings yet
- Magat, Jescel-Anne Janea D. MED-2B A B C BDocument3 pagesMagat, Jescel-Anne Janea D. MED-2B A B C BJescel-Anne Janea MagatNo ratings yet
- Year Test - Ii: (Batch - A)Document11 pagesYear Test - Ii: (Batch - A)sachin sakuNo ratings yet
- (Nikolaj Wolfson, Alexander Lerner, Leonid Roshal (B-Ok - CC)Document589 pages(Nikolaj Wolfson, Alexander Lerner, Leonid Roshal (B-Ok - CC)Andi sutandi100% (1)
- Jeremiah's Law, Introduced by Assemblywoman Rodneyse BichotteDocument2 pagesJeremiah's Law, Introduced by Assemblywoman Rodneyse BichotteCity & State NYNo ratings yet
- Initial Data Base FormatDocument7 pagesInitial Data Base FormatrhamhonaNo ratings yet
- Self Esteem and AdjustmentDocument22 pagesSelf Esteem and AdjustmentJan IrishNo ratings yet
- Inquiries Research Titles SOP ExamplesDocument10 pagesInquiries Research Titles SOP ExamplesEunice Pineza ManlunasNo ratings yet
- DS 1 CatDocument38 pagesDS 1 CatMuhammad Bilal Khattak100% (1)
- May 2 Homework Solutions: S M X CDocument3 pagesMay 2 Homework Solutions: S M X CClerry SamuelNo ratings yet
- PT3 Practices EssayDocument61 pagesPT3 Practices EssayGolden Fingers100% (3)
- The Thermal ConductivityDocument6 pagesThe Thermal ConductivityLuc LeNo ratings yet
- Blood Stasis and What Does That MeanDocument2 pagesBlood Stasis and What Does That MeanCarl MacCordNo ratings yet
- Ryder Funeral Home Ex Parte MotionDocument22 pagesRyder Funeral Home Ex Parte MotionJim KinneyNo ratings yet
- CyberPunk 2020 - Unofficial - Reference Book - Ammo and Add-OnsDocument6 pagesCyberPunk 2020 - Unofficial - Reference Book - Ammo and Add-Onsllokuniyahooes100% (1)
- Nasoalveolar Moulding Seminar at MalakkaraDocument54 pagesNasoalveolar Moulding Seminar at MalakkaraAshwin100% (1)
- IOC CoachingResearchStudiesList PDFDocument87 pagesIOC CoachingResearchStudiesList PDFJeane LucenaNo ratings yet
- Ccii Proposal EssayDocument4 pagesCcii Proposal Essayapi-456307983No ratings yet
- Comparative Study For Determination of Atracurium Besilate in Presence of Its Toxic Degradant (Laudanosine) by Reversed Phase HPLC and by TLC DensitometryDocument11 pagesComparative Study For Determination of Atracurium Besilate in Presence of Its Toxic Degradant (Laudanosine) by Reversed Phase HPLC and by TLC DensitometrySabrina JonesNo ratings yet
- Manual Fritadeira PDFDocument136 pagesManual Fritadeira PDFtherasiaNo ratings yet
- Elecsys T4: Cobas e 411 Cobas e 601 Cobas e 602 English System InformationDocument5 pagesElecsys T4: Cobas e 411 Cobas e 601 Cobas e 602 English System InformationIsmael CulquiNo ratings yet
- Spoilage of Frozen Chicken Nuggets by Toxigenic Psycrophilic FungiDocument16 pagesSpoilage of Frozen Chicken Nuggets by Toxigenic Psycrophilic FungiNIDHI BARINo ratings yet
- Book Review - Black Skin, White MasksDocument9 pagesBook Review - Black Skin, White MasksKaren A. LloydNo ratings yet
- Alex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessFrom EverandAlex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessNo ratings yet
- The Other End of the Leash: Why We Do What We Do Around DogsFrom EverandThe Other End of the Leash: Why We Do What We Do Around DogsRating: 5 out of 5 stars5/5 (64)
- Show Dog: The Charmed Life and Trying Times of a Near-Perfect PurebredFrom EverandShow Dog: The Charmed Life and Trying Times of a Near-Perfect PurebredRating: 3.5 out of 5 stars3.5/5 (13)
- The Dog Listener: Learn How to Communicate with Your Dog for Willing CooperationFrom EverandThe Dog Listener: Learn How to Communicate with Your Dog for Willing CooperationRating: 4 out of 5 stars4/5 (37)
- An Eagle Named Freedom: My True Story of a Remarkable FriendshipFrom EverandAn Eagle Named Freedom: My True Story of a Remarkable FriendshipNo ratings yet
- Merle's Door: Lessons from a Freethinking DogFrom EverandMerle's Door: Lessons from a Freethinking DogRating: 4 out of 5 stars4/5 (326)
- Roxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueFrom EverandRoxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueRating: 5 out of 5 stars5/5 (3)
- Roxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueFrom EverandRoxane Gay & Everand Originals Presents: Good Girl: Notes on Dog RescueRating: 4.5 out of 5 stars4.5/5 (22)
- Dogland: Passion, Glory, and Lots of Slobber at the Westminster Dog ShowFrom EverandDogland: Passion, Glory, and Lots of Slobber at the Westminster Dog ShowNo ratings yet
- Will's Red Coat: The Story of One Old Dog Who Chose to Live AgainFrom EverandWill's Red Coat: The Story of One Old Dog Who Chose to Live AgainRating: 4.5 out of 5 stars4.5/5 (18)
- Inside of a Dog: What Dogs See, Smell, and KnowFrom EverandInside of a Dog: What Dogs See, Smell, and KnowRating: 4 out of 5 stars4/5 (390)
- The Dog Who Couldn't Stop Loving: How Dogs Have Captured Our Hearts for Thousands of YearsFrom EverandThe Dog Who Couldn't Stop Loving: How Dogs Have Captured Our Hearts for Thousands of YearsNo ratings yet
- Come Back, Como: Winning the Heart of a Reluctant DogFrom EverandCome Back, Como: Winning the Heart of a Reluctant DogRating: 3.5 out of 5 stars3.5/5 (10)
- The Wrong Dog: An Unlikely Tale of Unconditional LoveFrom EverandThe Wrong Dog: An Unlikely Tale of Unconditional LoveRating: 4.5 out of 5 stars4.5/5 (26)
- Decoding Your Cat: The Ultimate Experts Explain Common Cat Behaviors and Reveal How to Prevent or Change Unwanted OnesFrom EverandDecoding Your Cat: The Ultimate Experts Explain Common Cat Behaviors and Reveal How to Prevent or Change Unwanted OnesRating: 4 out of 5 stars4/5 (6)
- Puppy Training 101: How to Train a Puppy, Training Your Own Psychiatric Service Dog, A Step-By-Step Program so your Pup Will Understand You!From EverandPuppy Training 101: How to Train a Puppy, Training Your Own Psychiatric Service Dog, A Step-By-Step Program so your Pup Will Understand You!Rating: 5 out of 5 stars5/5 (85)
- Arthur: The Dog Who Crossed the Jungle to Find a HomeFrom EverandArthur: The Dog Who Crossed the Jungle to Find a HomeRating: 4.5 out of 5 stars4.5/5 (19)
- Your Dog Is Your Mirror: The Emotional Capacity of Our Dogs and OurselvesFrom EverandYour Dog Is Your Mirror: The Emotional Capacity of Our Dogs and OurselvesRating: 4 out of 5 stars4/5 (31)
- Lessons from Tara: Life Advice from the World's Most Brilliant DogFrom EverandLessons from Tara: Life Advice from the World's Most Brilliant DogRating: 4.5 out of 5 stars4.5/5 (42)
- For the Love of a Dog: Understanding Emotion in You and Your Best FriendFrom EverandFor the Love of a Dog: Understanding Emotion in You and Your Best FriendRating: 4 out of 5 stars4/5 (100)
- Meet Your Dog: The Game-Changing Guide to Understanding Your Dog's BehaviorFrom EverandMeet Your Dog: The Game-Changing Guide to Understanding Your Dog's BehaviorRating: 5 out of 5 stars5/5 (34)
- How To Speak Dog: Mastering the Art of Dog-Human CommunicationFrom EverandHow To Speak Dog: Mastering the Art of Dog-Human CommunicationRating: 4 out of 5 stars4/5 (66)
- Edward's Menagerie: Dogs: 50 canine crochet patternsFrom EverandEdward's Menagerie: Dogs: 50 canine crochet patternsRating: 3 out of 5 stars3/5 (5)
- Meet Your Dog: The Game-Changing Guide to Understanding Your Dog's BehaviorFrom EverandMeet Your Dog: The Game-Changing Guide to Understanding Your Dog's BehaviorRating: 5 out of 5 stars5/5 (1)
- Arthur: The Dog who Crossed the Jungle to Find a HomeFrom EverandArthur: The Dog who Crossed the Jungle to Find a HomeRating: 4.5 out of 5 stars4.5/5 (16)