Professional Documents
Culture Documents
Aquerreta2002 Farmakodinamik
Uploaded by
Adkhiatul MuslihatinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aquerreta2002 Farmakodinamik
Uploaded by
Adkhiatul MuslihatinCopyright:
Available Formats
Oncology
Pharmacodynamics of High-Dose Methotrexate
in Pediatric Patients
Irene Aquerreta, Azucena Aldaz, Joaquín Giráldez, and Luis Sierrasesúmaga
OBJECTIVE: To establish a relationship between the pharmacokinetics of high-dose methotrexate (MTX) and toxicity in children of a
pediatric oncology department and to reassess MTX concentrations at which the patients would be at high risk for toxic effects.
METHODS: This study included 37 patients (227 treatment courses) who received a median dose of 4.87 g/m2 of MTX in a 4-hour
infusion. The population pharmacokinetic parameters of MTX were estimated by parametric (IT2B) and nonparametric methods
(NPEM). Gastrointestinal, renal, and hematologic toxicity were evaluated. The relationship between pharmacokinetic parameters
and toxicity was analyzed by logistic regression and multiple linear regression.
RESULTS: Equations to predict hematologic and nonhematologic toxicity were obtained. An increase of 100 µmol/L in the MTX peak
concentration meant a 12% (p = 0.03) higher risk of vomiting; a significant delay in MTX elimination implied a 5.76-fold higher risk of
mucositis (p < 0.001). An increase of 1 µmol/L in the MTX concentration 24 hours after the end of the infusion (Cp24h) led to a 43%
increase in the risk of renal toxicity (p < 0.001). Hematologic toxicity was significantly conditioned by the baseline leukocyte count
and Cp24h (p < 0.001).
CONCLUSIONS: The analysis of high-dose MTX pharmacokinetic/pharmacodynamic relationship to toxicity has led to equations able
to predict toxicity that are easily applicable to daily practice. Cp24h >3.5 µmol/L was confirmed as an indicator of high risk of toxicity.
KEY WORDS: high-dose methotrexate, toxicity.
Ann Pharmacother 2002;36:1344-50.
igh-dose methotrexate (MTX) is useful therapy for a reduce the severity of the toxic effects. Clinical monitoring
H diverse range of pediatric tumors such as osteosarco-
1,2 3,4
ma, acute lymphocytic leukemia, and non-Hodgkin’s
is necessary to determine the period over which leucovorin
rescue must be maintained, as it has to be continued until
5,6
lymphoma. Clinical monitoring, hydration, and urine al- an MTX serum concentration of 0.05 µmol/L has been
kalinization have helped to reduce the mortality rate associ- reached.7 To our knowledge, quantitative methods to pre-
ated with high-dose MTX therapy from 5–6% to <0.1%.7 dict MTX-induced toxicity based on pharmacokinetic pa-
Monitoring the serum concentrations of high-dose MTX is rameters are limited.11-14 The objective of this study was to
a well-accepted method to identify patients who are at high derive predictive equations based on the analysis of phar-
risk for severe toxic effects of the drug.8 macokinetic/pharmacodynamic relationships in terms of
Criteria for risk assessment vary from one institution to toxicity to be used in daily clinical practice to help opti-
another. Concentrations of MTX that are likely to produce mize high-dose MTX therapy in pediatric patients.
a high risk for toxic effects have been defined9,10 at selected
times after the end of the infusion (24, 48, or 72 h). Once a Methods
high-risk concentration has been detected, appropriate
measures, such as leucovorin rescue, must be adopted to PATIENTS
Thirty-seven children (19 boys, 18 girls) who received high-dose
MTX therapy between 1986 and 1993 were studied. The total number of
Author information provided at the end of the text. MTX courses administered was 227 in patients diagnosed with osteosar-
1344 ■ The Annals of Pharmacotherapy ■ 2002 September, Volume 36 www.theannals.com
Downloaded from aop.sagepub.com at OhioLink on August 13, 2014
Research Reports
coma (n = 27), non-Hodgkin’s lymphoma (9), and medulloblastoma (1). traindividual variability to be applied on NPEM. The assay error pattern
The inclusion criterion was the availability of the relevant data in the pa- was determined by the Jelliffe and Tahani19 method. The pharmacokinet-
tients’ medical charts. ic parameters obtained by NPEM were chosen for their lower value of
the log-likelihood and their similar predictive performance when com-
pared with that obtained by IT2B. Pharmacokinetic parameters estimat-
DATA COLLECTION ed were elimination rate constant (kel), rate constants for MTX’s move-
ment from the central to peripheral compartment (kcp) and peripheral to
The following clinical data were collected by retrospective chart re- central compartment (kpc), and volume of distribution for the central
view: age; gender; height; weight; lean body weight; body surface area; compartment (Vc). MTX systemic clearance (Cl) and AUC were esti-
diagnosis; subtype of tumor; location of the tumor; presence of distant mated according to the following equations1:
metastases; creatinine clearance (Clcr) estimated by the Schwartz formu-
la15; significant delay in MTX elimination, defined in a previous unpub- Cl = kel × Vc
lished work done in our hospital as MTX concentration at 24 hours after
the end of the infusion (Cp24h) >3.5 µmol/L and plasma half-life for the AUC = dose
initial elimination phase (t1/2α) >3.5 hours, or MTX concentration 48 Cl
hours after the end of the infusion (Cp48h) ≥0.35 µmol/L and plasma t1/2
for the terminal elimination phase (t1/2β) >12.5 hours; baseline serum cre- The pharmacokinetic variables analyzed for each MTX course were
atinine (SCr); maximum SCr; baseline leukocyte count; minimum dose, peak plasma concentrations, Cp24h and Cp48h after the end of the in-
leukocyte count; volume of hydration; lowest recorded urine pH; and the fusion, Cl, Vc, kel, kcp, kpc, and AUC.
concurrent use of other drugs that could potentially interact with MTX In our previous, unpublished work, patient’s age was found to have a
(trimethoprim/sulfamethoxazole, penicillins, aminoglycosides, nons- profound influence on MTX pharmacokinetics. Therefore, relationships
teroidal antiinflammatory drugs [NSAIDs], diuretics, cisplatin, carbo- between pharmacokinetics and the incidence of the different toxicities
platin, vancomycin). were analyzed in different age groups (<8, 8–12, >12 y).
MTX ADMINISTRATION TOXICITY ANALYSIS
2
The dose of MTX ranged from 1.2 to 12.3 g/m (median 4.87, and in- MTX toxicity was evaluated as gastrointestinal toxicity defined as
terquartile range [IQR] 2.90). Hydration consisted of 3 L/m2/24 h of dex- vomiting after MTX administration (yes/no) or mucositis scored accord-
trose 5% in water with 300 mEq of NaHCO3 and 60 mEq of KCl per ing to the World Health Organization (WHO) scale20 (grade 0 = no reac-
liter. Hydration was begun 12 hours before MTX administration and tion; grade 1 = painless ulcers, erythema, or mild soreness; grade 2 =
maintained for 3 days. Urine pH was checked throughout the hydration painful erythema, edema, or ulcers but can eat solids; grade 3 = painful
period. MTX administration was performed when urine pH was between erythema, edema, or ulcers and cannot eat solids; grade 4 = requires par-
7 and 8 in 2 consecutive voids and urine flow was at least 120 mL/min. enteral or enteral support for alimentation); renal toxicity was assessed
If necessary, the NaHCO3 dose was adjusted to obtain a urine pH be- by the percentage of increase in SCr21 (grade 0 = <25%, grade 1 =
tween 7 and 8. The MTX dose was diluted in 500 mL of NaCl 0.9% and 25– 49%, grade 2 = 50 –74%, grade 3 = 75–100%, grade 4 = >100%);
infused over a 4-hour period. As this was a retrospective study, it was and hematologic toxicity was evaluated by the minimum leukocyte
not possible to confirm in every MTX course the exact length of the in- count per cubic millimeter according to the WHO scale20 (grade 0 =
fusion. We assumed that they all were 4-hour infusions, which is the >4000, grade 1 = 3000 –3900, grade 2 = 2000 –2900, grade 3 =
usual practice in our institution. The standard leucovorin rescue dose was 1000–1900, grade 4 = <1000). When mucositis plus renal and hemato-
15 mg/m2 every 6 hours for 3 days, beginning 12 hours after the end of logic toxicity were considered as binary variables, they were defined as
MTX administration. The chemotherapy regimen in patients with os- absent (grade 0) or present (grade >1).
teosarcoma included administration of cisplatin, doxorubicin, bleomycin,
dactinomycin, and ifosfamide. Patients with non-Hodgkin’s lymphoma
received M-BACOD and ICAVP chemotherapy regimens (Appendix I). STATISTICAL ANALYSIS
The relationship between the pharmacokinetic parameters and toxici-
PLASMA SAMPLES ty was analyzed by logistic regression and by multiple linear regression.
The best logistic regression model was selected by the p value associated
MTX concentrations were measured at specific times to determine to the Wald χ2. The frequencies of an event such as toxicity were com-
adequate leucovorin rescue therapy or supportive care. High-risk con- pared using a χ2 test. The criterion used to select the best model by mul-
centrations of MTX had been determined in our hospital in a preliminary tiple linear regression was the adjusted R2 (R2adj). The method used in
study in pediatric patients: Cp24h ≥3.5 µmol/L or Cp48h ≥0.35 µmol/L. logistic and multiple linear regression was forward stepwise. The corre-
Therefore, in most cases, MTX plasma concentrations were determined lations between variables were evaluated using a Pearson or Spearman
at the end of the MTX infusion and at 24 and 48 hours. Crom and correlation coefficient depending on the distribution of the variable. The
Evans’7 guidelines for modification of leucovorin dosage were followed program used for statistical analyses was Statistica edition ’99.22 In all
in patients with high-risk MTX concentrations ≥42 hours after the begin- cases, the significance level chosen was p < 0.05.
ning of the MTX infusion.
Results
SAMPLE ANALYSIS
PATIENTS
MTX plasma concentrations were measured by fluorescence polar-
ization immunoassay (FPIA) with a TDxFLx analyzer.16
Demographic and clinical data on the 37 subjects are
shown in Table 1.
PHARMACOKINETIC ANALYSIS
Pharmacokinetic parameters of MTX were estimated by parametric PHARMACOKINETIC ANALYSIS
(IT2B, iterative two-stage Bayesian)17 and nonparametric (NPEM, non-
parametric expectation maximization)18 methods using the software MTX plasma concentrations expressed as median (IQR)
package USC*PACK 10.7a (University of Southern California, Los An-
geles, CA) and assuming a 2-compartment pharmacokinetic model.
were peak 450 (320) µmol/L, Cp24h 0.85 (1.09) µmol/L,
First, pharmacokinetic parameters were estimated by IT2B to obtain a and Cp48h 0.14 (0.14) µmol/L. A significant delay in MTX
range of variability of the parameters and estimate the value of σ or in- elimination (Cp24h >3.5 µmol/L and t1/2α >3.5 h, or Cp48h
www.theannals.com The Annals of Pharmacotherapy ■ 2002 September, Volume 36 ■ 1345
Downloaded from aop.sagepub.com at OhioLink on August 13, 2014
I Aquerreta et al.
≥0.35 µmol/L and t1/2β >12.5 h) was observed in 37 cours- an increase of 1 µmol/L increased the risk of vomiting by
es (16.30%). The dose of leucovorin administered was 0.11%. When considering an increase of 100 µmol/L, the
177.20 (71.14) mg/m2. Urine pH <7 was detected in only 4 OR increases to 1.12 (95% CI 1.01 to 1.24). Thus, an in-
MTX courses. In 3 of these cases, the acid urine pH crease of 100 µmol/L in peak concentration means a 12%
(5–6.5) resulted in a significant delay in MTX elimination. greater risk of vomiting after MTX administration. The fol-
Pharmacokinetic parameters estimated by NPEM present- lowing equation can be used to determine the risk of devel-
ed an optimal predictive performance (determination coef- oping vomiting that is associated with an increase in the
ficient between observed and predicted plasma concentra- peak (Table 2):
tions R2 = 0.98). MTX Cl was 6.25 (2.80) L/h and AUC
OR = e(0.00112 × ∆peak)
was 2392.64 (1777.74) µmol/L/h.
The only variable significantly related to mucositis (p <
TOXICITY
0.05) was the delay in MTX elimination (Wald p < 0.001;
Table 2). The OR obtained shows that patients who experi-
Different types of toxicity were observed: emesis 24 enced significant delay in MTX elimination had a 5.76-
hours after MTX administration was reported in 55 treat-
ment courses, mucositis 1 week after administration of
MTX in 8 courses, renal toxicity between grades 1 and 4 Table 1. Anthropometric and Clinical Variablesa
in 65 courses, and hematologic toxicity between grades 1
Variable Mean SD CV (%) Range
and 4 in 52 courses. Not all the clinical charts included an-
alytical data of renal and hematologic information after ad- BSA (m2) 1.40 0.33 23.48 0.67–2.28
ministration of MTX. Indeed, only 180 and 81 MTX Weight (kg) 46.67 15.99 34.38 15.32–96.43
courses presented renal and hematologic information to as- LBW (kg) 38.32 12.34 32.30 13.87–75.79
sess toxicity, respectively. WBC (x 103/mm3)
baseline 5.17 2.29 44.24 1.24–16.0
minimum 3.64 1.61 44.29 8.0–9.1
RELATIONSHIP BETWEEN MTX PHARMACOKINETICS AND Clcr (mL/min) 120.8 46.23 38.27 46.23–216.69
TOXICITY Median IQR
Age (y) 14 7 37.88 4–21
The dose of MTX, its peak concentration, and concur-
Height (cm) 158 30 14.38 105–192
rent administration of penicillins were identified by logistic
SCr (mg/dL)
regression as significant related to delay in MTX elimina- baseline 0.6 0.2 25.25 0.3–1.50
tion (p < 0.05). These variables were included in multivari- maximum 0.7 0.3 32.47 0.3–3.0
ate analysis; the best model selected was the one that in- BSA = body surface area; Clcr = creatinine clearance estimated by the
cluded the MTX peak concentration considering the value Schwartz formula; IQR = interquartile range; LBW = lean body weight;
of p associated to Wald χ2 (p < 0.001) (Table 2). The odds SCr = serum creatinine; WBC = white blood cell.
a
37 patients; 227 courses of high-dose methotrexate.
ratio (OR) associated with the peak concentra-
tion was 1.0041, implying that an increase of 1
µmol/L increases the risk of presenting signifi-
cant delay (0.41%) in MTX elimination. An in- Table 2. Logistic Regression Models for Significant Delay in MTX
crease of 100 µmol/L in the peak MTX con- Elimination, Vomiting, Mucositis, and Renal Toxicity
centration raises the OR to 1.50 (95% CI 1.31
Parameter β SE Wald p OR OR 95% CI
to 1.72), implying a 50% higher risk of devel-
oping significant delay in MTX elimination. Delay in MTX
elimination
The following equation can be used to deter- intercept –4.21 0.53 <0.001 0.015 0.0052 to 0.043
mine the risk of developing significant delay in peak concen- 0.0041 0.00070 <0.001 1.0041 1.0027 to 1.0055
tration
MTX elimination that is associated with an in-
Vomiting
crease in peak concentration (∆peak) (Table 2): intercept –1.76 0.34 <0.001 0.17 0.089 to 0.33
OR = e(0.00406 × ∆peak) peak concen- 0.0011 0.00051 0.030 1.0011 1.00011 to 1.0021
tration
Logistic regression led to the identification Mucositis
of 3 variables as significant determinants of the intercept –3.83 0.51 <0.001 0.022 0.00803 to 0.059
risk of developing vomiting (p < 0.05). They delay in MTX 1.72 0.73 0.020 5.76 1.32 to 23.59
elimination
were concomitant administration of NSAIDs,
Renal toxicity
total leucovorin dose (mg/m2), and peak con- intercept 1.17 0.77 0.13 3.23 0.70 to 14.92
centration of MTX. By multiple logistic regres- Cp24h (µmol/L) 0.36 0.13 0.0075 1.43 1.10 to 1.86
sion, the best model selected was the one that SCr (mg/dL) –3.71 1.31 0.0055 0.025 0.0018 to 0.33
included MTX peak concentration (Wald p = Cp24h = MTX plasma concentration at 24 hours after the end of the infusion; MTX =
0.030; Table 2). The OR associated with the methotrexate; peak concentration = MTX plasma concentration at the end of the
infusion; SCr = baseline serum creatinine.
peak concentration was 1.0011, meaning that
1346 ■ The Annals of Pharmacotherapy ■ 2002 September, Volume 36 www.theannals.com
Downloaded from aop.sagepub.com at OhioLink on August 13, 2014
Research Reports
fold higher risk of presenting mucositis than those who able to develop equations that may predict toxicity. Some
eliminated MTX at a normal rate. of the limitations of our study were the relatively low num-
By simple logistic regression, the variables significantly ber of patients included, the retrospective design, and the
related to renal toxicity were Cp24h, baseline SCr, Clcr, kcp, relatively large number of correlative factors analyzed.
kpc, AUC, and MTX Cl (p < 0.05). The model selected by Different authors have described the mechanism by
multiple logistic regression included the variable Cp24h and which renal toxicity and consequent delay in MTX elimina-
baseline SCr (Wald p = 0.00064; Table 2). The Cp24h OR tion is produced. MTX and its metabolite, 7-hydroxy-
obtained shows that an increase of 1 µmol/L in Cp24h was methotrexate (7-OH-MTX), precipitate in distal tubules, in-
reflected in an increase of 43% in the risk of renal toxicity ducing renal dysfunction as well as having a direct nephro-
(95% CI 10% to 86%). The equation to predict the risk of toxic action on distal tubule cells.23 This leads to a decrease
nephrotoxicity that is associated with an increase in Cp24h in the renal elimination of MTX, causing an increase in the
(∆Cp24h) is: concentration of MTX and, consequently, a higher inci-
OR = e(0.359 × ∆Cp24h) dence of adverse events such as hematologic and gastroin-
testinal toxicity. Thus, renal toxicity induced by MTX in-
(Table 2). When renal toxicity was analyzed as percentage
hibits its own renal excretion.11,24 Indeed, high-dose MTX
of the increase in SCr by multiple linear regression, the
therapy has been shown23 to produce a decrease in glom-
variables that explain renal toxicity were Cp24h and base-
erular filtration even in otherwise nontoxic courses.
line SCr. Both variables were able to explain a 44.39%
Logistic regression analysis shows that an increase of
variability in the percentage increase of SCr (R2adj = 0.44;
100 µmol/L in the peak concentration of MTX increases
p < 0.001). The regression equation obtained was:
the risk of developing significant delay in the elimination
increase of SCr (%) = 38.91– 45.82 × baseline SCr of MTX by 50%. The strong correlation observed between
(mg/dL) + 7.15 × Cp24h (µmol/L) the peak concentration and the dose of MTX (Spearman R
The Cp24h at which significant differences in renal toxicity = 0.83; p < 0.001; Figure 1) indicates that the main factor
were detected was evaluated. Significant differences were responsible for delay of MTX elimination is its dose.
detected by the χ2 test at Cp24h 3.5 µmol/L (p = 0.018), with a Many other factors have been described that increase
sensitivity of 20% and specificity of 94.19%. The OR ob- the risk of MTX toxicity including inadequate hydration,25
tained was 2.09, which means that patients whose Cp24h ex- acidic urine pH,11 presence of extravascular third spaces,7
ceeded 3.5 µmol/L presented a double risk of nephrotoxicity. concomitant administration of other drugs (e.g., NSAIDs,26
The only significant variable associated with hemato- nephrotoxic agents27), low concentration of plasma pro-
logic toxicity by logistic regression was the baseline leuko- teins,28 emesis,11 or poor nutritional status.7 Nevertheless, in
cyte count (p < 0.001). A decrease of 1000 leukocytes per many cases, delayed MTX elimination cannot be related to
cubic millimeter in baseline leukocyte count leads to a four any of these risk factors. Given the high incidence of un-
fold increase in the risk of developing hematologic toxici- predictable delays in MTX elimination, it is useful to mon-
ty. When the minimum leukocyte count was
considered the dependent variable in multiple
linear regression, the explanatory variables
were the baseline leukocyte count and Cp24h (p
< 0.001; R2adj = 0.64). The regression equa-
tion obtained was:
minimum leukocyte count/mm3 = 735.36 +
0.65 × baseline leukocyte count – 80.92 ×
Cp24h (µmol/L)
Significant differences were obtained in the in-
cidence of hematologic toxicity at Cp24h above
or below 3.5 µmol/L by the Mann–Whitney
U-test (p = 0.034).
It seems that hematologic toxicity increases
with age; however, no significant differences
were detected in hematologic or renal toxicity
between the different age groups analyzed. No
significant influence of age was identified for
gastrointestinal toxicity.
Discussion
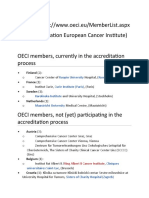
Figure 1. Correlation between MTX dose and peak concentration. The regression equa-
In analyzing the relationship between high- tion obtained was as follows: peak concentration (µmol/L) = –61.75 + 107.06 × dose (g/m2);
dose MTX and toxicity in children, we were Spearman rank order correlation (p < 0.001). MTX = methotrexate.
www.theannals.com The Annals of Pharmacotherapy ■ 2002 September, Volume 36 ■ 1347
Downloaded from aop.sagepub.com at OhioLink on August 13, 2014
I Aquerreta et al.
itor its concentrations in all high-dose courses10,29 and to in osteosarcoma patients and 20% in those with non-
define high-risk MTX concentrations at specific times. Re- Hodgkin’s lymphoma. Similarly, nephrotoxicity was 30%
nal dysfunction as the result of the MTX administration versus 28%, respectively. Mucositis was detected only in
appears to be the main factor involved in significant delay patients with osteosarcoma.
of elimination. Hematologic toxicity appears to increase with age. How-
Vomiting was related to the peak concentration of MTX ever, no significant differences were detected between the
by logistic regression analysis (p < 0.001). An increase in different age groups. Some investigators30,31 have found that
the peak concentration of 100 µmol/L increases the risk of toxicity caused by high-dose MTX is milder and more tol-
vomiting by 12%, which can be considered slightly rele- erable in younger patients, probably because of the higher
vant. As was the case for delayed MTX elimination, the values of MTX Cl and Vc in that population that determine
close correlation observed between peak concentration and lower MTX exposure.32 Wang and Fujimoto33 found that
dose (R = 0.83) indicates that the main factor involved in the incidence of moderate or severe toxicity was signifi-
vomiting was the dose. cantly lower in patients <15 years old,33 and Rask et al.14
The incidence of mucositis was related to the delay in observed a significant increase in liver toxicity with age.
MTX elimination, with the risk being 5.76 times higher in
patients who experienced significant delay in elimination. Summary
Rask et al12,14 also found a significant correlation between
mucositis and low systemic clearance of MTX and high We have been able to obtain predictive equations of gas-
plasma concentration 28 hours after starting the infusion.14 trointestinal and renal toxicity by high-dose MTX in a
The incidence of mucositis that we observed was lower population of pediatric patients. The MTX peak concentra-
(3.52%) than that reported10,12,20 by other authors (33– tion is the main factor that affects the significant delay in
52%). This difference can be explained by the delayed ap- elimination and emesis. This delay is unpredictable; conse-
pearance of mucositis, an effect that appears ≥1 week after quently, all high-dose MTX courses should be closely
MTX administration. Within that time, if the drug has been monitored. Cp24h >3.5 µmol/L is an MTX concentration
adequately eliminated, the patient has been discharged; in associated with a high-risk toxicity. MTX concentrations
addition, mucositis is not always recorded in the medical and supportive measures should be adopted if this level of
records. Other authors have probably performed a closer exposure is reached. We found no significant correlation
monitoring over a longer period of time after MTX admin- between Cp48h and toxicity, and the Cp48h toxicity criteria
istration and so were able to detect late toxic events. Mean obtained in our preliminary study could not be confirmed.
length of stay of our patients was 3 days, and no clinical The predictive equations derived from our observations
data were collected after they were discharged. could be useful in the evaluation of MTX toxicity in pa-
The variables related to renal toxicity were baseline SCr tients whose clinical data were above the toxicity level in
and Cp24h. Baseline SCr was included in the model as a order to adopt the adequate supportive and treatment mea-
corrective factor of how renal toxicity was evaluated (per- sures.
centage increase in SCr related to baseline value). At a
Cp24h >3.5 µmol/L, the incidence of renal toxicity was Irene Aquerreta PharmD PhD, Staff Pharmacist, Pharmacy De-
twofold greater than normal. This group of patients exhib- partment, University Hospital of Navarra, Pamplona, Spain
ited a mean t1/2α >3.5 hours. These results corroborate the Azucena Aldaz PharmD PhD, Staff Pharmacist, Pharmacy De-
partment, University Hospital of Navarra
high-risk MTX concentration and t1/2 obtained in a prelimi-
Joaquín Giráldez PharmD PhD, Director, Pharmacy Department,
nary study conducted in our department and show that the University Hospital of Navarra
Cp24h is important in detecting patients with a high risk of Luis Sierrasesúmaga MD PhD, Director, Pediatrics Department,
developing toxic effects. University Hospital of Navarra
The only variable significantly related by logistic re- Reprints: Irene Aquerreta PharmD PhD, Pharmacy Department,
University Hospital of Navarra, Avda. Pío XII 36, 31008 Pamplona,
gression to hematologic toxicity was the baseline leuko- Spain, FAX 34 948 175278, E-mail iaquerreta@unav.es
cyte count; however, multiple linear regression showed
that Cp24h also has a significant influence. Other authors14
References
have found a significant correlation between hematologic
toxicity and long exposure to MTX measured as AUC. 1. Delepine N, Delepine G, Bacci G, Rosen G, Desbois JC. Influence of
The Cp24h seems to be an indicator of the risk of develop- methotrexate dose intensity on outcome of patients with high grade os-
teogenic osteosarcoma. Analysis of the literature. Cancer 1996;78:2127-
ing both renal and hematologic toxicity. 35.
No significant influence of other chemotherapy agents 2. Kawai A, Sugihara S, Kunisada T, Hamada M, Inoue H. The importance
was detected in the incidence of toxic effects. Despite the of doxorubicin and methotrexate dose intensity in the chemotherapy of
osteosarcoma. Arch Orthop Trauma Surg 1996;115:68-70.
different MTX doses administered, no significant differ- 3. Evans WE, Crom WR, Abromowitch M, Dodge R, Look T, Bowman P,
ences were detected in the incidence of toxic effects be- et al. Clinical pharmacodynamics of high-dose methotrexate in acute
tween the patients diagnosed with osteosarcoma and non- lymphocytic leukemia. Identification of a relation between concentration
and effect. N Engl J Med 1986;314:471-7.
Hodgkin’s lymphoma, although it tended to be higher in
4. Evans WE, Relling MV, Rodman JH, Crom WR, Boyett JM, Pui CH.
patients with osteosarcoma. The percentage of MTX treat- Conventional compared with individualized chemotherapy for childhood
ment courses that were associated with vomiting was 25% acute lymphoblastic leukemia. N Engl J Med 1998;338:499-505.
1348 ■ The Annals of Pharmacotherapy ■ 2002 September, Volume 36 www.theannals.com
Downloaded from aop.sagepub.com at OhioLink on August 13, 2014
Research Reports
5. Skarin AT, Canellos GP, Rosenthal DS. Improved prognosis of diffuse his- 28. Kumar RV, Gokhale SV, Ambaye RY, Shetty PA. Pharmacokinetics of
tiocytic and undifferentiated lymphoma by use of high dose methotrexate methotrexate in Indian children and its relationship to nutritional status.
alternating with standard agents (M-BACOD). J Clin Oncol 1983;1:91-7. Chemotherapy 1987;33:234-9.
6. Shipp MA, Yong YB, Harrington DP. The m-BACOD combination che- 29. Graf N, Winkler K, Betlemovic M, Fuchs N, Bode U. Methotrexate
motherapy regimen in large-cell lymphoma: analysis of the completed pharmacokinetics and prognosis in osteosarcoma. J Clin Oncol 1994;12:
trial and comparison with the M-BACOD regimen. J Clin Oncol 1990; 1443-51.
8:84-93. 30. Hande KR, Oldman RH, Fer MF, Richardson RL, Greco FA. Random-
7. Crom WR, Evans WE. Methotrexate. In: Evans WE, Schentag JJ, Jusko ized study of high-dose versus low-dose methotrexate in the treatment of
WJ, eds. Applied pharmacokinetics. Principles of therapeutic drug moni- extensive small cell lung cancer. Am J Med 1982;73:413-9.
toring. 3rd ed. Spokane WA:1992:29-31. 31. Brouwers P, Moss H, Reaman G, McGuire T, Trupin E, Libow J. Central
8. Moore MJ, Erlichman C. Therapeutic drug monitoring in oncology. nervous system preventive therapy with systemic high-dose methotrex-
Problems and potential in antineoplastic therapy. Clin Pharmacokinet ate versus cranial irradiation and intrathecal methotrexate: longitudinal
1987;13:205-27. comparison of effects of treatment on intellectual function of children
9. Raude E, Oellerich M, Weinel P, Freund M, Schrappe M, Riehm H, et al. with ALL (abstract). Proc Am Soc Clin Oncol 1987;6:158.
High-dose methotrexate: pharmacokinetics in children and young adults. 32. Borsi JD, Moe PJ. A comparative study on the pharmacokinetics of
Int J Clin Pharmacol Ther Toxicol 1988;26:364-70. methotrexate in a dose range of 0.5 to 33.6 g/m2 in children with acute
10. Reggev A, Djerassi I. The safety of administration of massive doses of lymphoblastic leukemia. Cancer 1987;60:5-13.
methotrexate (50 g) with equimolar citrovorum factor rescue in adult pa- 33. Wang YM, Fujimoto T. Clinical pharmacokinetics of methotrexate in
tients. Cancer 1988;61:2423-8. children. Clin Pharmacokinet 1984;9:335-48.
11. Relling MV, Fairclough D, Ayers D, Crom WR, Rodman JH, Pui CH, et
al. Patient characteristics associated with high-risk methotrexate concen-
trations and toxicity. J Clin Oncol 1994;12:1667-72.
12. Rask C, Albertoni F, Schroder H, Peterson C. Oral mucositis in children
with acute lymphoblastic leukemia after high-dose methotrexate treat- EXTRACTO
ment without delayed elimination of methotrexate: relation to pharma- OBJETIVO: El objetivo de este estudio retrospectivo consistió en
cokinetic parameters of methotrexate. Pediatr Hematol Oncol 1996;13: establecer una relación entre la farmacocinética de altas dosis de
313-4. methotrexate (MTX) y la toxicidad en niños del departamento de
13. Albertoni F, Rask C, Schroeder H, Peterson C. Monitoring of methotrex- Oncología Pediátrica y establecer las concentraciones de MTX a las que
ate and 7-hydroxymethotrexate in saliva from children with acute lym- los pacientes presentaban riesgo de sufrir toxicidad.
phoblastic leukemia receiving high-dose consolidation treatment: rela-
MÉTODOS: Este estudio incluyó 37 pacientes (227 ciclos de tratamiento)
tion to oral mucositis. Anticancer Drugs 1997;8:119-24.
que recibieron una mediana de dosis de 4.87 g/m2 de MTX en una
14. Rask C, Albertoni F, Bentzen SM, Schroeder H, Peterson C. Clinical and
pharmacokinetic risk factors for high-dose methotrexate-induced toxici- infusión de 4 horas. Los parámetros farmacocinéticos de MTX fueron
ty in children with acute lymphoblastic leukemia: a logistic regression estimados mediante métodos paramétricos (IT2B) y no paramétricos
analysis. Acta Oncol 1998;37:277-84. (NPEM). Se evaluó la toxicidad gastrointestinal, renal, y hematológica.
15. Schwartz GJ, Haycock GB, Edelman CM. A simple estimate of La relación entre los parámetros farmacocinéticos y la toxicidad se
glomerular filtration rate in children derived from body length and plas- analizó mediante regresión logística y regresión lineal múltiple.
ma creatinine. Pediatrics 1976;58:259-63.
16. TDx assays manual. Abbott Park, IL: Abbott Laboratories, 1991.
17. Jelliffe RW, Schumitzky A, Van Guilder M. Making parametric popula-
tion pharmacokinetic/pharmacodynamic models: the Iterative Bayesian
(IT2B) algorithm. Technical report. Laboratory of Applied Pharmacoki- Appendix I. Chemotherapy Regimens
netics, University of Southern California, Los Angeles, 1999.
18. Jelliffe RW, Schumitzky A, Van Guilder M. Making nonparametric pop- Osteosarcoma
ulation pharmacokinetic/pharmacodynamic models: the NPEM algo- Before surgery
rithm. Technical report. Laboratory of Applied Pharmacokinetics, Uni- cisplatin 40 mg/m2/d ia, days 1, 2, 3, 21, 22, and 23
versity of Southern California, Los Angeles, 1999. doxorubicin 30 mg/m2/d iv, days 1, 2, 22, 23
19. Jelliffe RW, Tahani B. A library of serum drug assay error patterns, and MTX 6 g/m2 iv, days 7, 14, 29, 36
some suggestions for improved modeling and simulation of pharmacoki- cisplatin 40 mg/m2/d ia, days 43, 44, 45
netic behaviour. Technical report: 92-5. Laboratory of Applied Pharma- 2 wk after surgery
cokinetics, University of Southern California, Los Angeles, 1992. (A) MTX 6 g/m2 iv
20. Miller AB, Hougstraten B, Staquet M, Winkler A. Reporting results of (B) cisplatin 40 mg/m2/d iv for 3 d
cancer treatment. Cancer 1981;47:207-14. doxorubicin 25 mg/m2/d iv for 3 d
(C) bleomycin 10 mg/m2/d iv for 3 d
21. Parker RI, Forman EN, Krumm KF, Abeel MJ, Martin HF. Pharmacoki-
dactinomycin 0.5 mg/m2/d iv for 3 d
netics and toxicity of frequent intermediate dose methotrexate infusions.
ifosfamide 1.5 g/m2/d iv for 3 d, with Mesna 300 mg/m2 adminis-
Ther Drug Monitor 1986;8:393-9.
tered before and 4 and 8 h after ifosfamide
22. Statistica. Volumes I–IV. Tulsa, OK: Stat Soft, Inc., 1994. cycles B and C repeated every 21 d; cycle A administered be-
23. Widemann BC, Balis FM, Murphy RF, Sorensen JM, Montello MJ, tween cycles B and C, days 7 and 14
O’Brien M, et al. Carboxypeptidase-G2, thymidine and leucovorin res- NHL
cue in cancer patients with methotrexate-induced renal dysfunction. J M-BACOD
Clin Oncol 1997;15:2125-34. bleomycin 4 mg/m2 im, day 1
24. Abelson HT, Fosburg MT, Beardsley GP, Goorin AM, Gorka C, Link C, doxorubicin 45 mg/m2 im, day 1
et al. Methotrexate-induced renal impairment: clinical studies and rescue cyclophosphamide 600 mg/m2 iv, day 1
from systemic toxicity with high-dose leucovorin and thymidine. J Clin vincristine 1 mg/m2 iv, day 1
Oncol 1983;1:208-16. dexamethasone 6 mg/m2 po, days 1–5
25. Treon SP, Chabner BA. Concepts in use of high-dose methotrexate ther- methotrexate 3 g/m2 iv, day 14
apy. Clin Chem 1996;42(8B):1322-9. ICAVP
26. Kremer JM, Hamilton RA. The effects of nonsteroidal antiinflammatory ifosfamide 3 g/m2 iv, day 21
drugs on methotrexate (MTX) pharmacokinetics: impairment of renal cisplatin 50 mg/m2 iv, day 21
clearance of MTX at weekly maintenance doses but not at 7.5 mg. J etoposide 60 mg/m2 iv, days 21–23
Rheumatol 1995;22:2072-7. cytarabine 20 mg/m2 iv for 12 doses, days 21–23
27. Spector GB, Wang YM, Gleiser CA, Chan RC, Van Eys J. Effect of gen- prednisone 60 mg/m2/d po, days 21–25
tamicin and irradiation on the toxicity of high-dose methotrexate in rats. MTX = methotrexate.
Cancer Treat Rep 1980;64:989-91.
www.theannals.com The Annals of Pharmacotherapy ■ 2002 September, Volume 36 ■ 1349
Downloaded from aop.sagepub.com at OhioLink on August 13, 2014
I Aquerreta et al.
RESULTADOS: Se obtuvieron ecuaciones para predecir la toxicidad MÉTHODOLOGIE: Cette étude comprenait 37 patients (227 cycles) ayant
hematológica y no hematológica. Un incremento de 100 µmol/L en la reçu 1 dose médiane de 4.87 g/m2 de MTX en perfusion de 4 heures. Les
concentración de MTX al final de la infusión supuso un aumento del paramètres pharmacocinétiques du MTX pour cette population ont été
12% (p = 0.03) en el riesgo de presentar vómitos, mientras que los estimés par des tests paramétriques et non-paramétriques. Les toxicités
pacientes con retraso en la eliminación de MTX presentaron un riesgo gastro-intestinale, rénale, et hématologique ont été évaluées. Les
de desarrollar mucositis 5.76 veces superior (p < 0.001). Un aumento en relations entre les paramètres pharmacocinétiques et la toxicité ont été
1 µmol/L en la concentración de MTX 24 horas tras el fin de la infusión analysées par régression logistique et par régression multiple linéaire.
(Cp24h) supuso un aumento del 43% en el riesgo de presentar toxicidad RESULTATS: Pour prédire la toxicité hématologique et non-
renal (p < 0.001). La toxicidad hematológica estaba relacionada hématologique, les cliniciens ont développé des équations. Ainsi, une
significativamente con el recuento basal de leucocitos y con la Cp24h (p augmentation de 100 µmol/L du pic plasmatique de MTX signifiait un
< 0.001). risque de 12% (p = 0.03) plus élevé de développer des vomissements
CONCLUSIONES: Mediante el análisis de la relación entre farmacocinética tandis qu’un délai significatif dans l’élimination du MTX impliquait un
y farmacodinamica de altas dosis de MTX en términos de toxicidad risque 5.76 fois plus élevé de développer des mucosites (p inf. à 0.001).
permitió obtener ecuaciones para predecir la toxicidad que son Une hausse de 1 µmol/L de la concentration de MTX 24 heures après la
fácilmente aplicables a la práctica clínica. La Cp24h > 3.5 µmol/L se fin de la perfusion (Cp24h) a occasionné une augmentation de 43% du
confirmó como un indicador de riesgo elevado de presentar toxicidad. risque de développer de la néphrotoxicité (p inf. à 0.001). La toxicité
hématologique était influencée significativement par le décompte initial
Irene Aquerreta des leucocytes et par la Cp24h (p inf. à 0.001).
CONCLUSIONS: L’analyse de cette étude sur les hautes doses de MTX a
RÉSUMÉ permis d’élaborer des équations facilement applicables dans notre
OBJECTIF: Le but de cette étude rétrospective consistait à établir une pratique quotidienne pour prédire la toxicité du MTX. Une CP24h
relation entre la pharmacocinétique du méthotrexate (MTX) et la supérieure à 3.5 µmol/L est un indicateur imporant de haut risque de
toxicité chez les enfants d’un département d’oncologie pédiatrique et à toxicité.
déterminer à quelles concentrations de MTX les malades présenteraient Louise Gagnon
plus de risques au niveau des effets toxiques.
Finding Strength in Weakness:
A Study of Tribulation and Our Appropriate Response
By William D Black MD
ISBN 1-57921-3580-8 / Paperbound / xxii + 256 pp. / 2001 / $13.99
Dr. Black writes, “God allows [human suffering] in order to bring about a
more ultimate good in our lives. Any response to tribulation that moves us
farther away from God should be considered sin.
“The key to successfully moving through difficult circumstances lies within
the human spirit. There is nothing that quite satisfies the longings of our spir-
its like the God who created them. In this life, we may never completely un-
derstand why we are undergoing tribulation, but we have ample evidence of how we are to handle it.
Jesus is our example, and we are supposed to walk as He did.”
“Dr Black writes from the pathos of the examination room…From a lifetime of immersion in Holy
Scripture, intermixed with his own multiplex of personal setbacks and devastating family illnesses, he
brings us a book that the anguished and heartbroken will turn to again and again for solid help.”
— Rev. Ronald L Siegenthaler, Coral Ridge Presbyterian Church, Ft. Lauderdale, FL
“It is a fine book, bringing together a great deal of biblical wisdom that to my knowledge is not to be
found between any other two book covers. It is a powerful piece of writing, and will surely do its read-
ers a great deal of good.”
— JI Packer, Regent College, Vancouver, BC, Canada
For more information, visit www.FindingStrength.com or call toll-free 877-421-7323
1350 ■ The Annals of Pharmacotherapy ■ 2002 September, Volume 36 www.theannals.com
Downloaded from aop.sagepub.com at OhioLink on August 13, 2014
You might also like
- WHO Classification of Tumours of The Central Nervous System 4th EdDocument313 pagesWHO Classification of Tumours of The Central Nervous System 4th EdRandy UlloaNo ratings yet
- Use of MTHFR C677T Polymorphism and Plasma Pharmacokinetics To Predict Methotrexate Toxicity in Patients With Acute Lymphoblastic LeukemiaDocument8 pagesUse of MTHFR C677T Polymorphism and Plasma Pharmacokinetics To Predict Methotrexate Toxicity in Patients With Acute Lymphoblastic LeukemiaFaMe TanapornNo ratings yet
- JGM 2990Document7 pagesJGM 2990FaMe TanapornNo ratings yet
- Leucovorin (Folinic Acid) Rescue For High-Dose MethotrexateDocument10 pagesLeucovorin (Folinic Acid) Rescue For High-Dose Methotrexateanton.neonatusNo ratings yet
- Pharmaco DynamicsDocument2 pagesPharmaco DynamicsSunil DeshpandeNo ratings yet
- PIII-74 Pro-76: Society For Clinical Pharmacology and TherapeuticsDocument1 pagePIII-74 Pro-76: Society For Clinical Pharmacology and Therapeuticsdev darma karinggaNo ratings yet
- Pharmacokinetics, PharmacodynamicsDocument18 pagesPharmacokinetics, PharmacodynamicspinkbutterNo ratings yet
- PK ProblemsDocument18 pagesPK ProblemsJosephine Valsa JoseNo ratings yet
- The PK/PD Index (C /mic) For Ciprofloxacin in Patients With Cystic FibrosisDocument7 pagesThe PK/PD Index (C /mic) For Ciprofloxacin in Patients With Cystic Fibrosisefra maneNo ratings yet
- Influence of Mechanical Ventilation On Vancomycin Pharmacokinetics Administered by Continuous Infusion in Critically Ill PatientsDocument32 pagesInfluence of Mechanical Ventilation On Vancomycin Pharmacokinetics Administered by Continuous Infusion in Critically Ill PatientsNguyễn LongNo ratings yet
- MixDocument3 pagesMixranievadewiNo ratings yet
- Rodvold 1988Document5 pagesRodvold 1988Fernando ToroNo ratings yet
- Shungo Imai Bs Takehiro Yamada PHD Kumiko Kasashi PHD Masaki Kobayashi PHD Ken Iseki PHDDocument7 pagesShungo Imai Bs Takehiro Yamada PHD Kumiko Kasashi PHD Masaki Kobayashi PHD Ken Iseki PHDMutiara SeptianiNo ratings yet
- Application of Neural Networks To Population Pharmacokinetic Data AnalysisDocument6 pagesApplication of Neural Networks To Population Pharmacokinetic Data AnalysisHoda HosnyNo ratings yet
- Dosing Guidance For Intravenous Colistin in Critically Ill Patients PDFDocument7 pagesDosing Guidance For Intravenous Colistin in Critically Ill Patients PDFJukapun YoodeeNo ratings yet
- KetoconazoleDocument5 pagesKetoconazoleadisty maharaniNo ratings yet
- A Short Introduction To Pharmacokinetics: R. Urso, P. Blardi, G. GiorgiDocument12 pagesA Short Introduction To Pharmacokinetics: R. Urso, P. Blardi, G. GiorgiMirlitha LopezNo ratings yet
- Compartmental & Non-Compartmental PharmacokineticsDocument21 pagesCompartmental & Non-Compartmental PharmacokineticsVikas JhawatNo ratings yet
- TetrodotoxinDocument9 pagesTetrodotoxinNguyen thanhNo ratings yet
- Analytical Validation of A Novel UHPLC-MS MS Method For 19 Antibiotics Quantification in Plasma Implementation in A LC-MS MS KitDocument14 pagesAnalytical Validation of A Novel UHPLC-MS MS Method For 19 Antibiotics Quantification in Plasma Implementation in A LC-MS MS KitngobaochanNo ratings yet
- PIIS0007091217320603Document10 pagesPIIS0007091217320603amjedsenoussiNo ratings yet
- Frid Lund 2016Document20 pagesFrid Lund 2016DoyoxNo ratings yet
- Therapeutic Drug MonitoringDocument50 pagesTherapeutic Drug MonitoringKapusetti Vanaja0% (1)
- Oxidant Stress in Primary Nephrotic Syndrome: Does It Modulate The Response To Corticosteroids?Document6 pagesOxidant Stress in Primary Nephrotic Syndrome: Does It Modulate The Response To Corticosteroids?galihrahman51No ratings yet
- TCI Propofol ClearanceDocument9 pagesTCI Propofol ClearanceJoanna GlezNo ratings yet
- Reduced Dose Folinic Acid Rescue After Rapid High-Dose Methotrexate Clearance Is Not Associated With Increased Toxicity in A Pediatric CohortDocument8 pagesReduced Dose Folinic Acid Rescue After Rapid High-Dose Methotrexate Clearance Is Not Associated With Increased Toxicity in A Pediatric Cohortanton.neonatusNo ratings yet
- Reuter 2010Document8 pagesReuter 2010Hector Javier BurgosNo ratings yet
- Pharmacokinetics & Compartment ModelingDocument50 pagesPharmacokinetics & Compartment ModelingPrathamesh PatilNo ratings yet
- The Pharmacodynamics and Pharmacokinetics of Mivacurium in ChildrenDocument7 pagesThe Pharmacodynamics and Pharmacokinetics of Mivacurium in ChildrenluyawinNo ratings yet
- Patient Experience in The Treatment of Metastatic Castration-Resistant Prostate Cancer: State of The ScienceDocument11 pagesPatient Experience in The Treatment of Metastatic Castration-Resistant Prostate Cancer: State of The ScienceLuis ReyNo ratings yet
- Bioequivalence of 250 MG Lysine ClonixinDocument6 pagesBioequivalence of 250 MG Lysine ClonixinMax Marcial JavierNo ratings yet
- Tse 2014Document5 pagesTse 2014Ke XuNo ratings yet
- Clinical Efficacy of Therapeutic Drug Monitoring in Patients Receiving VancomycinDocument4 pagesClinical Efficacy of Therapeutic Drug Monitoring in Patients Receiving VancomycinAprilia SyafraniNo ratings yet
- Mikkelsen 2013Document5 pagesMikkelsen 2013Maria Carolina CoutoNo ratings yet
- 10.3324 Haematol.2014.104133Document9 pages10.3324 Haematol.2014.104133Jess silvaNo ratings yet
- Pharmacokinetic Modeling Simulation and Development of A Limited Sampling Strategy of Cycloserine in Patients With Multidrug Extensively Drug Resistant TuberculosisDocument13 pagesPharmacokinetic Modeling Simulation and Development of A Limited Sampling Strategy of Cycloserine in Patients With Multidrug Extensively Drug Resistant TuberculosisTejas EditNo ratings yet
- Farmakologi KlinikDocument23 pagesFarmakologi KlinikAmir ShafiqNo ratings yet
- Regular ArticleDocument8 pagesRegular ArticleFaMe TanapornNo ratings yet
- Antimicrobial Agents and Chemotherapy-2010-Pea-4605.fullDocument6 pagesAntimicrobial Agents and Chemotherapy-2010-Pea-4605.fullGül BaktırNo ratings yet
- Systemic Methotrexate Treatment in Childhood Psoriasis: Further Experience in 24 Children From IndiaDocument5 pagesSystemic Methotrexate Treatment in Childhood Psoriasis: Further Experience in 24 Children From IndiaNana AdistyNo ratings yet
- Babalik. Serum Drug Concentration Turkey. IJTLD Dec 13Document7 pagesBabalik. Serum Drug Concentration Turkey. IJTLD Dec 13Vigilancia EpidemiologicaNo ratings yet
- Abstract Early IdentificationDocument4 pagesAbstract Early IdentificationrhezagiovNo ratings yet
- MEtka M 1994Document4 pagesMEtka M 1994joana curadoNo ratings yet
- Pharmacokinetics & Compartment ModelingDocument50 pagesPharmacokinetics & Compartment ModelingPrathamesh PatilNo ratings yet
- Jurding AulDocument5 pagesJurding AulRizky AuliaNo ratings yet
- Asam Traneksamat MelasmaDocument14 pagesAsam Traneksamat MelasmaFitrianidilaNo ratings yet
- 6.toxicokinetics in Animal Toxicology Studies.01Document18 pages6.toxicokinetics in Animal Toxicology Studies.01Manu m rNo ratings yet
- Ansefar 2Document8 pagesAnsefar 2NATASYA NOOR FADILLA -No ratings yet
- Artritis ReumatoideDocument5 pagesArtritis ReumatoideAdrian CarranzaNo ratings yet
- Pharmacokinetic Interaction Between High-Dose Methotrexate and OxacillinDocument3 pagesPharmacokinetic Interaction Between High-Dose Methotrexate and Oxacillindds (TMU)No ratings yet
- Bmri2018 1683414Document13 pagesBmri2018 1683414Pande Agung MahariskiNo ratings yet
- Review Article: Tranexamic Acid For Adults With Melasma: A Systematic Review and Meta-AnalysisDocument14 pagesReview Article: Tranexamic Acid For Adults With Melasma: A Systematic Review and Meta-Analysismiak miakNo ratings yet
- JurnalDocument5 pagesJurnalkadekNo ratings yet
- Nimas 1929Document21 pagesNimas 1929Gabriel NguyenNo ratings yet
- The Influence of CYP2D6 Phenotype On The Pharmacokinetic Profile of Atomoxetine in Caucasian Healthy SubjectsDocument8 pagesThe Influence of CYP2D6 Phenotype On The Pharmacokinetic Profile of Atomoxetine in Caucasian Healthy SubjectsAlina RotariNo ratings yet
- Article 4Document13 pagesArticle 4ירדן לויןNo ratings yet
- Articulo OooDocument7 pagesArticulo OooPaola M. TrianaNo ratings yet
- st03 PDFDocument8 pagesst03 PDFLutfi HidiyaningtyasNo ratings yet
- Pharmacokinetics of Moxi Oxacin, A Novel 8-Methoxy-Quinolone, in Patients With Renal DysfunctionDocument6 pagesPharmacokinetics of Moxi Oxacin, A Novel 8-Methoxy-Quinolone, in Patients With Renal DysfunctionAuliyaa Zahra SupriyatnaNo ratings yet
- Antibacterial Therapeutic Drug Monitoring in CerebrospinalDocument5 pagesAntibacterial Therapeutic Drug Monitoring in CerebrospinalaNo ratings yet
- Pharmacology in Drug Discovery: Understanding Drug ResponseFrom EverandPharmacology in Drug Discovery: Understanding Drug ResponseNo ratings yet
- Abebe2010 Bab4goodDocument14 pagesAbebe2010 Bab4goodAdkhiatul MuslihatinNo ratings yet
- Krabbe DiseaseDocument5 pagesKrabbe DiseaseAdkhiatul MuslihatinNo ratings yet
- 2013 Ozougwuetal2013JPAPDocument13 pages2013 Ozougwuetal2013JPAPAdkhiatul MuslihatinNo ratings yet
- Aly PDFDocument6 pagesAly PDFAdkhiatul MuslihatinNo ratings yet
- Krabbe DiseaseDocument5 pagesKrabbe DiseaseAdkhiatul MuslihatinNo ratings yet
- 1Document9 pages1Adkhiatul MuslihatinNo ratings yet
- AIH2010Document31 pagesAIH2010Irina GîrleanuNo ratings yet
- Clinical Pharmacokinetics of Methotrexate: D.O. Shen and DL AzarnoffDocument2 pagesClinical Pharmacokinetics of Methotrexate: D.O. Shen and DL AzarnoffAdkhiatul MuslihatinNo ratings yet
- Ka Math 2004Document6 pagesKa Math 2004Adkhiatul MuslihatinNo ratings yet
- Ka Math 2004Document6 pagesKa Math 2004Adkhiatul MuslihatinNo ratings yet
- Ab StewardshipDocument10 pagesAb StewardshipAdkhiatul MuslihatinNo ratings yet
- Ka Math 2004Document6 pagesKa Math 2004Adkhiatul MuslihatinNo ratings yet
- Pathogenesis of Obesity: Josanne VassalloDocument4 pagesPathogenesis of Obesity: Josanne VassalloAdkhiatul MuslihatinNo ratings yet
- Quantitative Assessment of Combination Bathing and Moisturizing Regimens On Skin Hydration in Atopic DermatitisDocument6 pagesQuantitative Assessment of Combination Bathing and Moisturizing Regimens On Skin Hydration in Atopic DermatitisAdkhiatul MuslihatinNo ratings yet
- Jann 2006Document11 pagesJann 2006Adkhiatul MuslihatinNo ratings yet
- Analisis Kadar Kreatinin Pada Anak Dengan Leukemia Limfoblastik Akut Di Pusat Kanker Anak Estella Blu Rsup Prof DR RD KandouDocument5 pagesAnalisis Kadar Kreatinin Pada Anak Dengan Leukemia Limfoblastik Akut Di Pusat Kanker Anak Estella Blu Rsup Prof DR RD KandouAdkhiatul MuslihatinNo ratings yet
- Aquerreta2002 FarmakodinamikDocument7 pagesAquerreta2002 FarmakodinamikAdkhiatul MuslihatinNo ratings yet
- Analisis Kadar Kreatinin Pada Anak Dengan Leukemia Limfoblastik Akut Di Pusat Kanker Anak Estella Blu Rsup Prof DR RD KandouDocument5 pagesAnalisis Kadar Kreatinin Pada Anak Dengan Leukemia Limfoblastik Akut Di Pusat Kanker Anak Estella Blu Rsup Prof DR RD KandouAdkhiatul MuslihatinNo ratings yet
- Treatment of Atopic Dermatitis (Eczema) William2019 PDFDocument60 pagesTreatment of Atopic Dermatitis (Eczema) William2019 PDFAdkhiatul MuslihatinNo ratings yet
- Analisis Kadar KreatininDocument13 pagesAnalisis Kadar KreatininAdkhiatul MuslihatinNo ratings yet
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument25 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsAdkhiatul MuslihatinNo ratings yet
- 194 265 1 SMDocument5 pages194 265 1 SMAdkhiatul MuslihatinNo ratings yet
- Malignant Fungating Wounds EducationDocument4 pagesMalignant Fungating Wounds Education郭品君No ratings yet
- Breast Cancer in Women - A Narrative Literature ReviewDocument7 pagesBreast Cancer in Women - A Narrative Literature ReviewAnnie McSolsticeNo ratings yet
- Current Management of Cerebral GliomasDocument6 pagesCurrent Management of Cerebral GliomasResiden BedahNo ratings yet
- Final EssayDocument12 pagesFinal Essayapi-609569585No ratings yet
- Cancer Research AssignmentDocument5 pagesCancer Research Assignmentapi-212901753No ratings yet
- Metabolic Solutions Report: Should You Get A Biopsy of That Lump?Document11 pagesMetabolic Solutions Report: Should You Get A Biopsy of That Lump?Ilona Gunawan100% (1)
- InformationFeb19 ABOUT ROHTAKDocument20 pagesInformationFeb19 ABOUT ROHTAKsushmita singhNo ratings yet
- Abstract - Big Data Analytics and Evaluation For Cancer Prognosis and Diagnosis - Abdullahi Kabiru - PHD (IT)Document2 pagesAbstract - Big Data Analytics and Evaluation For Cancer Prognosis and Diagnosis - Abdullahi Kabiru - PHD (IT)abunishanNo ratings yet
- Care of Clients With Cellular Aberrations: NCM 106/ NCM 112Document4 pagesCare of Clients With Cellular Aberrations: NCM 106/ NCM 112evaNo ratings yet
- Environmental Carcinogens and Cancer RiskDocument3 pagesEnvironmental Carcinogens and Cancer RiskJessica MalijanNo ratings yet
- NURSING CARE PLAN For Acute LeukemiaDocument2 pagesNURSING CARE PLAN For Acute LeukemiaJadeNo ratings yet
- Tre 295Document4 pagesTre 295Ahmed Ben BellaNo ratings yet
- Adi Wasis Prakosa - Poster AbstractDocument2 pagesAdi Wasis Prakosa - Poster AbstractAdi Wasis PrakosaNo ratings yet
- Benign Breast Papilloma: Is Surgical Excision Necessary?: Original ArticleDocument6 pagesBenign Breast Papilloma: Is Surgical Excision Necessary?: Original Articleyongky sugandaNo ratings yet
- Pediatric Blood Cancer - 2022 - Mader - Social Emotional and Behavioral Functioning in Young Childhood Cancer SurvivorsDocument11 pagesPediatric Blood Cancer - 2022 - Mader - Social Emotional and Behavioral Functioning in Young Childhood Cancer SurvivorsJuliana SoaresNo ratings yet
- Organisation of European Cancer InstitutesDocument4 pagesOrganisation of European Cancer InstitutesMazhar KayaNo ratings yet
- Invasive Micropapillary Breast Carcinoma Discovered During The Investigation of Acute Respiratory Distress in A Postpartum Woman: A Case ReportDocument7 pagesInvasive Micropapillary Breast Carcinoma Discovered During The Investigation of Acute Respiratory Distress in A Postpartum Woman: A Case ReportIJAR JOURNALNo ratings yet
- Pembrolizumab For Persistent, Recurrent, or Metastatic Carvical CancerDocument12 pagesPembrolizumab For Persistent, Recurrent, or Metastatic Carvical CancerluizaNo ratings yet
- Introduction To Word Parts: Speaker: Heidi JonesDocument8 pagesIntroduction To Word Parts: Speaker: Heidi JonesZoreenNo ratings yet
- Dermoscopy of Inflamed Seborrheic KeratosisDocument9 pagesDermoscopy of Inflamed Seborrheic KeratosisFreddy RojasNo ratings yet
- FINAL Gebbia PSA Script Breast Cancer-1Document2 pagesFINAL Gebbia PSA Script Breast Cancer-1Diana Marie NicoleNo ratings yet
- Cutaneous - Melanoma-Spanish Hasta 183Document233 pagesCutaneous - Melanoma-Spanish Hasta 183Ely SalazarNo ratings yet
- Cancer: Kendriya Vidyalaya AruvankaduDocument20 pagesCancer: Kendriya Vidyalaya AruvankaduGáMÍNG WÍTH ÁBHÍ GaMÍNG CHÁNNÉLNo ratings yet
- Advanced Prostate Cancer: Treatment Advances and Future DirectionsDocument14 pagesAdvanced Prostate Cancer: Treatment Advances and Future DirectionsMishel Rodriguez GuzmanNo ratings yet
- Bladder - Bx.turbt 4.1.0.0.rel CapcpDocument12 pagesBladder - Bx.turbt 4.1.0.0.rel CapcpkarimahihdaNo ratings yet
- Tumors of The KidneyDocument5 pagesTumors of The KidneyShivaniNo ratings yet
- L6-PATHO-Neoplasia (Sept2821)Document12 pagesL6-PATHO-Neoplasia (Sept2821)Erald PaderangaNo ratings yet
- Glimmers of Hope For Targeting Oncogenic KRAS-G12D: Cancer Gene TherapyDocument3 pagesGlimmers of Hope For Targeting Oncogenic KRAS-G12D: Cancer Gene Therapychato law officeNo ratings yet
- Osteokondroma Raksasa Pada Rami Pubis: Laporan KasusDocument6 pagesOsteokondroma Raksasa Pada Rami Pubis: Laporan KasusentannabilakasdyNo ratings yet