Professional Documents
Culture Documents
Ciy1111 5
Uploaded by
inesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ciy1111 5
Uploaded by
inesCopyright:
Available Formats
Clinical Infectious Diseases
SUPPLEMENT ARTICLE
Antibiotic Resistance and Typhoid
Zoe A. Dyson,1,a Elizabeth J. Klemm,1,2,a Sophie Palmer,1 and Gordon Dougan1,2
1
Department of Medicine, University of Cambridge, and 2Wellcome Sanger Institute, Wellcome Genome Campus, Hinxton, Cambridge, United Kingdom
Multiple drug (antibiotic) resistance (MDR) has become a major threat to the treatment of typhoid and other infectious diseases.
Since the 1970s, this threat has increased in Salmonella enterica serovar Typhi, driven in part by the emergence of successful genetic
clades, such as haplotype H58, associated with the MDR phenotype. H58 S. Typhi can express multiple antibiotic resistance determi-
Downloaded from https://academic.oup.com/cid/article-abstract/68/Supplement_2/S165/5371231 by guest on 14 April 2019
nants while retaining the ability to efficiently transmit and persist within the human population. The recent identification of exten-
sively drug resistant S. Typhi only highlights the dangers of ignoring this threat. Here we discuss the evolution of the S. Typhi MDR
phenotype and consider options for management.
Keywords. multiple drug resistance; MDR; S. Typhi; H58; typhoid.
Since the introduction of antibiotics in the middle of the last Salmonella enterica serovar Typhi (S. Typhi) is a subtype
century, there has been an increasing appreciation of the threat of the Gram-negative enteric pathogen Salmonella enterica.
of antibiotic resistance [1, 2]. Following the first clinical use of Unlike many other S. enterica serovars, S. Typhi is a human
penicillin, many other antibiotics have been introduced and, in restricted pathogen that, as far as we know, is propagated by
each case, resistance has followed at some level. The threat of human to human spread with no zoonotic reservoir and with a
resistance has been compounded by a dramatic reduction in the limited ability to survive longer term in the environment [4]. S.
rate of introduction of novel classes of antibiotics and an associ- Typhi can persist in water and food contaminated with human
ated drop in investment in the area (https://amr-review.org). We fecal material, but there is no environmentally adapted stage of
are now in an era where the levels of circulating virulent, multi- the bacterial life-cycle such as the formation of spores. The per-
ple drug-resistant (MDR) bacteria threatens healthcare efficacy sistence of S. Typhi in human populations is influenced by clin-
globally. Typhoid treatment was one of the key areas that imme- ically silent carriage within certain individuals (carriers) that
diately benefited from antibiotic usage. This chronic infection can be infected for months and even years with periodic shed-
with the potential for relapse, carriage, and complications was ding of S. Typhi into the environment in contaminated feces.
enormously challenging in terms of clinical management prior Thus, antibiotic usage can influence both acute typhoid disease
to antibiotics. Indeed, antibiotic treatment transformed the and the carrier state. In both states the emergence of antibiotic
clinical management of the disease and the public’s percep- resistance is theoretically possible. Unlike other enteric bacte-
tion of the threat the disease posed. Antibiotics, together with ria, genetic and phenotypic analysis (eg, through the controlled
improved water treatment and better public health manage- challenge of human volunteers) has indicated that S. Typhi is
ment, led to the control of the disease, at least in economically relatively poorly adapted for growth in the human intestine
developed settings. However, typhoid remains in economically [5]. Indeed, many genes, for example, shdA associated with
deprived areas where poverty and poor infrastructure persisted persistence in the intestine are inactivated in S. Typhi and are
[3]. In these same resource-limited settings, the indiscriminate consequently known as pseudogenes [6]. S. Typhi also shows
use of antibiotics has encouraged resistance and selected for vir- limited evidence of recombination with other bacteria, sug-
ulent MDR clades. Thus, antibiotic resistance in typhoid is now gesting the global population of S. Typhi is relatively isolated
a clinical and economic challenge. compared to other enteric bacteria that live free in the intes-
tine or environment [7]. This, theoretically, limits their relative
ability to horizontally acquire genes, including those that are
a
encoded on genetically mobile elements. Nevertheless, over
Z. A. D. and E. J. K. contributed equally.
the past 70 years, multiple antibiotic resistance in S. Typhi has
Correspondence: G. Dougan, Department of Medicine, University of Cambridge, 5th Fl,
Addenbrooke’s Hospital, Hills Rd, Cambridge CB2 0SP, United Kingdom (gd312@medschl.cam. emerged as a global threat.
ac.uk).
Clinical Infectious Diseases® 2019;68(S2):S165–70 THE EARLY EMERGENCE OF ANTIBIOTIC
© The Author(s) 2019. Published by Oxford University Press for the Infectious Diseases Society
RESISTANCE IN S. TYPHI
of America. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted
reuse, distribution, and reproduction in any medium, provided the original work is properly cited.
Shortly after the introduction of chloramphenicol for the treat-
DOI: 10.1093/cid/ciy1111 ment of typhoid, reports of resistance in S. Typhi began to
Antibiotic Resistance and Typhoid • CID 2019:68 (Suppl 2) • S165
emerge [8]. These tended to be reports of sporadic resistance resistance to quinolones (nalidixic acid) and intermediate lev-
associated with clinical failures and because new antibiotics els of resistance to ofloxacin were reported in the same region
were being introduced on a regular basis, particularly in the [14]. The targets of fluoroquinolones are the DNA gyrase
1950–70s, this was largely regarded as a nuisance rather than subunits encoded by genes gyrA and gyrB, as well as DNA
a crisis. As S. Typhi has an unusual fastidious intracellular life- topoisomerase IV components parC and parE. “Signature”
style in vivo, some antibiotics worked much better than oth- mutations including those at codon positions 83 and 87 in the
ers, and chloramphenicol became one of the “go to” antibiotics gyrA gene sequence are associated with resistance. These sig-
for this disease. The potential side effects of chloramphenicol nature mutations were identified in the nalidixic acid resistant
dampened this enthusiasm to some extent, but cheaper antibi- derivatives of S. Typhi in Vietnam [15].
otics continued to be favored in resource-poor settings. Over the next decade, the use of ciprofloxacin for the treat-
During the 1960s, resistance to 3 or more first-line (mul- ment of typhoid, and indeed other infections, became wide-
Downloaded from https://academic.oup.com/cid/article-abstract/68/Supplement_2/S165/5371231 by guest on 14 April 2019
tiple) antibiotics including ampicillin, trimethoprim-sulfa- spread across parts of Asia, and the reports of resistance began
methoxazole, and chloramphenicol, known as MDR, became to increase in general frequency.
more common, and MDR S. Typhi began to be reported more
frequently. In 1972 a large MDR typhoid epidemic, with over THE EMERGENCE OF MDR CLADES OF S. TYPHI
10 000 reported cases, occurred in Mexico City and other parts
As part of the studies on MDR S. Typhi in Vietnam, work was
of Mexico [9, 10]. The epidemic S. Typhi commonly exhibited
initiated to use molecular approaches including pulse field gel
resistance to chloramphenicol, tetracycline, streptomycin, and
electrophoresis (PFGE) to characterize the S. Typhi and start to
sulphonamides and encoded an R factor plasmid that was trans-
understand the population structure of the pathogen. An aim
ferable to Escherichia coli. Some S. Typhi isolates from the epi-
here was to try to track transmission and identify outbreaks in
demic also encoded resistance to ampicillin and/or kanamycin,
a region with a high level of endemic disease. It was quickly
but fortunately these never became dominant. Eventually, this
noted that the PFGE patterns of S. Typhi isolated before 1990
epidemic subsided and remained a local phenomenon confined
were diverse, but those isolated after this time onward became
largely within Mexico. Other sporadic cases of MDR S. Typhi
increasingly conserved as one PFGE type [16]. S. Typhi itself
were reported in different countries over the next 2 decades, but
is highly clonal compared to many other pathogens, and this
these also did not become dominant.
characteristic confounded the epidemiological investigations.
This observation remained of interest, but the limitations of
MDR S. TYPHI BECAME A THREAT TO TREATMENT the techniques meant that this phenomenon remained unex-
plained. However, it was noted that all MDR S. Typhi harbored
During this period (1970–90) typhoid frequently occurred in
a large, transferrable R factor of incompatibility group IncHI1,
regions with limited facilities for culturing S. Typhi and con-
the same group as the plasmid identified in Mexico in 1970 [17].
sequently the levels of MDR remained largely unreported and
Over the next years, the interest in bacterial population
likely underappreciated. However, the Wellcome Trust and
structures increased as the technologies advanced. Techniques
Oxford University established a Clinical Unit in Ho Chi Minh
such as multi locus sequence typing (MLST) were invented, but
City in Vietnam in conjunction with the Vietnamese govern-
they were not sufficiently discriminatory to provide further res-
ment, and a local program of typhoid surveillance involving
olution of the population structure of S. Typhi, which is largely a
blood culture and antibiotic susceptibility testing was estab-
single MLST type. Further advances into molecular typing using
lished. It quickly became clear that MDR was associated with
rare single nucleotide polymorphisms in the bacterial genome
up to 90% of the typhoid cases in Ho Chi Minh City and in
were eventually developed and applied to a global collection
a rural study area in the Mekong Delta [11]. This, in part,
of S. Typhi [7]. These studies identified an emerging subtype,
explained a high level of clinical relapse, intestinal perforation,
known as a haplotype, of S. Typhi designated H58 that was as-
and poor response to treatment. Other reports coming in from
sociated with both MDR and fluoroquinolone resistance signa-
elsewhere, including India [12], resulted in a rethink about the
ture mutations in gyrA. Importantly, S. Typhi H58 were found
treatment of typhoid, and the use of fluoroquinolones in the
in many countries in Asia and were becoming more common
form of ciprofloxacin was advocated [13]. To that point, the
in more recent isolates. The conserved PFGE MDR clade found
use of fluoroquinolones in children was not common due to
in Vietnam was identified as haplotype H58. S. Typhi H58 fre-
reported side effects associated with joint/cartilage damage.
quently harbored MDR plasmids of IncHI1 type.
Nevertheless, the present threat of MDR encouraged ethically
supported trials of ciprofloxacin in the treatment of typhoid,
WHOLE GENOME SEQUENCING OF S. TYPHI
and this was reported as being very effective with a low level
of clinical relapse. However, within a few years of the intro- In 2000, the first complete genome sequence of an MDR S. Typhi
duction of ofloxacin treatment, S. Typhi exhibiting significant known as CT18 from Vietnam was reported [6]. S. Typhi CT18
S166 • CID 2019:68 (Suppl 2) • Dyson et al
is not H58, but it does harbor a classical S. Typhi-associated dominant in West Africa. Interestingly, IncHI1 plasmids are not
transferrable R plasmid named pHCM1. pHCM1 encodes resis- always present in newer S. Typhi isolates that express the MDR
tance genes for all first-line antibiotics used for the treatment of phenotype. Instead, regions of the composite transposon pres-
typhoid fever and is highly related to R27, an IncHI1 plasmid ent on the IncHI1 plasmids have integrated into the S. Typhi
that was first isolated in the 1960s from S. enterica. pHCM1 chromosome, into at least 2 different genetic loci on multiple
has acquired additional genes compared to R27, predominantly occasions. This was concerning in that chromosomally inte-
at 2 points with 18 genes encoding resistance to antibiotics grated DNA tends to be more stable and is less likely to be lost
and heavy metals. Multiple transposon-like and integrases/ compared to a plasmid. Additionally, this highly fluid genetic
transposases are encoded around these 2 regions suggesting a region could act as a hot spot for sampling other genetic mate-
recombination hotspot. Antibiotic resistance genes encoded on rial taken up from the environment. Fluoroquinolone signature
pHCM1 include dhfr1b (trimethoprim), sul2 (sulphonamide), mutations are less common in S. Typhi from Africa than Asia,
Downloaded from https://academic.oup.com/cid/article-abstract/68/Supplement_2/S165/5371231 by guest on 14 April 2019
catI (chloramphenicol), bla (TEM-1; ampicillin), tetA/tetC More recently a S. Typhi H58 “triple mutant” clade possessing
(tetracyclines), and strAB (streptomycin). Further comparative 2 signature mutations in gyrA (codon 83 and 87) and a third in
analysis of IncHI1 plasmids showed that these plasmids were parC (codon 80) has been observed in Nepal as well as India
highly conserved in their broad framework but showed some and has been associated with a lack of fluoroquiolone efficacy
variation at these two recombinatorial hotspots. [22, 23]. The reduced frequency of these mutations in Africa
With the introduction of next generation sequencing the may be a reflection of the use of this class of antibiotics on the
analysis of thousands of S. Typhi at the whole genome level different continents [19].
rapidly became feasible and currently several thousand S. Interestingly in West Africa, the evolution of MDR in S.
Typhi have been sequenced [18–21]. These data provide an Typhi appears to have taken a different path as H58 isolates
enormous expanding database that has been used to define the have not become established there [24, 25]. Instead S. Typhi of
global S. Typhi population structure and to analyze the antibi- haplotype H56 (3.1.1) that harbor a range of different R factor
otic resistance signatures of individual isolates and clades. All types, including some of IncHI1 type, have become established,
currently circulating S. Typhi have a common ancestor and can for example, in Nigeria and Ghana. The genomic evidence indi-
be regarded as a monophyletic clade that entered the human cates that several of these West African MDR clades have spread
population from an unknown source several thousand years extensively in the region, crossing into multiple countries and
ago. MDR isolates can be found around the phylogenetic tree, causing sustained outbreaks. Similar clades have also been
but over 50% of recent isolates belong to clade H58 with a sig- found in the Republic of Congo suggesting widespread typhoid
nificant proportion of these harboring MDR and fluoroquino- in the region [26].
lone resistance alleles [19].
However, clear evolutionary patterns can be detected. S. Typhi THE EMERGENCE OF EXTENSIVELY RESISTANT
S. TYPHI
H58 isolates are widely distributed in Asia and the Middle East
region. In addition, there have been at least 3 recent indepen- In 2017, reports emerged of a large outbreak in Sindh, Pakistan,
dent introductions of S. Typhi H58 into the African continent of a S. Typhi expressing resistance to classical first-line antibiotics
that have become established. These 3 “waves” are currently (chloramphenicol, ampicillin, and trimethoprim-sulfamethox-
still present in Kenya, and the H58 introductions have spread azole), as well as to both fluoroquinolones and third-generation
across East Africa through several countries including Uganda, cephalosporins. These infections can only be resolved with azi-
Tanzania, Zaire, and Malawi. S. Typhi H58 isolates have also thromycin, carbapenems (meropenem) and tigecycline (Table
entered Zimbabwe and South Africa but have not become 1). Because only one of these remaining antibiotics can be
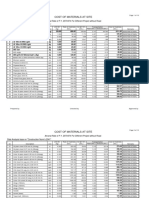
Table 1. Treatment Options for Different Resistance Classes of S. Typhi
Antibiotic Route of Administration MDR Pakistan XDR
Chloramphenicol Oral, intravenous X X
Co-trimoxazole Oral, intravenous X X
Ampicillin Oral, intramuscular, intravenous X X
Ciprofloxacin Oral, intravenous X
Ceftriaxone Intramuscular, intravenous X
Azithromycin Oral
Meropenem Intravenous
Tigecycline Intravenous
Abbreviations: MDR, multiple drug resistance; XDR, extensively drug resistant.
Antibiotic Resistance and Typhoid • CID 2019:68 (Suppl 2) • S167
administered orally, this presents a difficult and costly treatment Subsequent genome analysis showed the clade harbored a very
practice, which is especially challenging in resource-limited set- large pool of resistance determinants, with the chromosomally
tings. This outbreak stimulated an emergency response involving integrated composite resistance loci and an additional novel IncY
public health management and a typhoid vaccination campaign. plasmid encoding a blaCTX-M-15 extended-spectrum β-lactamase
The isolates were eventually classified as being “extensively drug gene and a qnrS fluoroquinolone resistance gene (Figure 1).
resistant”[XDR] [27, 28]. Whole-genome sequencing of represen- It is concerning that the blaCTX-M-15 and qnrS are encoded on the
tative XDR isolates confirmed that this was indeed an outbreak same plasmid raising the potential that treatment with one of
involving a highly conserved subclade of the H58 haplotype. the target antibiotic may favor the retention of both genes. The
Downloaded from https://academic.oup.com/cid/article-abstract/68/Supplement_2/S165/5371231 by guest on 14 April 2019
Figure 1. Outline genetic structure of XDR S. Typhi in Pakistan. A, Oval outlines represent individual bacteria harboring chromosome (wiggly, green) and plasmid (red and
blue circles) elements. Red and blue triangles represent acquired resistance loci. Small purple triangles represent SNPs in the chromosome associated with resistance. B,
Detailed structures with color codes as per A of the different acquired resistance elements on plasmid and chromosome. Abbreviations: AMR, antimicrobial resistance; MDR,
multiple drug resistance; SNP, single nucleotide polymorphism; XDR, extensively drug resistant.
S168 • CID 2019:68 (Suppl 2) • Dyson et al
IncY plasmid was highly homologous to a similar plasmid group the National Institute for Health Research (NIHR), or the Department of
Health and Social Care.
reported widely in other enteric bacteria around the globe, sug-
Financial support. This publication is based on research funded in
gesting that the IncY plasmid may have been acquired by conjuga- part by a grant from the Bill & Melinda Gates Foundation [OPP1151153].
tion from an E. coli cohabiting the intestine of an individual [27]. In addition, this work was supported by The Wellcome Trust (grants
Further genetic analysis showed that the H58 subclade associated STRATAA, 106158 and 098051) and by the NIHR (Cambridge Biomedical
Research Centre at the Cambridge University Hospitals NHS Foundation
with XDR was quite widely spread in Pakistan and other coun- Trust).
tries in the Middle East before the IncY plasmid was acquired Supplement sponsorship. This supplement is sponsored by the Center
in Sindh. Worryingly, the same XDR S. Typhi clade was isolated for Vaccine Development and Global Health (CVD) at the University of
Maryland School of Medicine.
from a traveler returning from Pakistan to the United Kingdom
Potential conflicts of interest. All authors: No reported conflicts.
and United States, indicating the clade is capable of interconti- All authors have submitted the ICMJE Form for Disclosure of Potential
nental spread [27]. There have been other reports of sporadic Conflicts of Interest. Conflicts that the editors consider relevant to the con-
Downloaded from https://academic.oup.com/cid/article-abstract/68/Supplement_2/S165/5371231 by guest on 14 April 2019
tent of the manuscript have been disclosed.
cases of XDR S. Typhi involving non-H58 isolates and different
plasmids [28].
References
1. O’Neill J. Tackling drug-resistant infections globally: final report and recom-
WHAT NEXT? mendations. Review of antimicrobial resistance. London: HM Government and
Wellcome trust; 2016.
These recent developments involving XDR isolates highlights 2. World Health Organization. Antimicrobial resistance: global report on surveil-
the evolving threat of antibiotic resistance in S. Typhi and the lance. Geneva: World Health Organization; 2014.
3. Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World
value of antibiotic susceptibility testing linked to genomic Health Organ 2004; 82:346–53.
analysis. Thus, we need to develop further low-cost diag- 4. Dougan G, Baker S. Salmonella enterica serovar Typhi and the pathogenesis of
typhoid fever. Annu Rev Microbiol 2014; 68:317–36.
nostic tools and kits that can be used in the field to rapidly 5. Waddington CS, Darton TC, Jones C, et al. An outpatient, ambulant-design, con-
detect such strains. Such tools should be linked to an open trolled human infection model using escalating doses of Salmonella Typhi chal-
lenge delivered in sodium bicarbonate solution. Clin Infect Dis 2014; 58:1230–40.
access, global database of whole genome-based sequences of 6. Parkhill J, Dougan G, James KD, et al. Complete genome sequence of a multiple
S. Typhi. Such databases do exist in various DNA sequence drug resistant Salmonella enterica serovar Typhi CT18. Nature 2001; 413:848–52.
7. Roumagnac P, Weill FX, Dolecek C, et al. Evolutionary history of Salmonella
repositories, but they are not readily accessible to groups
Typhi. Science 2006; 314:1301–4.
or organizations not well trained in the genomic sciences. 8. Murti BR, Rajyalakshmi K, Bhaskaran CS. Resistance of Salmonella Typhi to
We need to develop simple software that can be used to chloramphenicol. I. A preliminary report. J Clin Pathol 1962; 15:544–51.
9. Olarte J, Galindo E. Salmonella Typhi resistant to chloramphenicol, ampicillin,
rapidly select diagnostic signatures from these data that and other antimicrobial agents: strains isolated during an extensive typhoid fever
can be quickly used to modify and update diagnostic tools. epidemic in Mexico. Antimicrob Agents Chemother 1973; 4:597–601.
10. Watanabe T. Infectious drug resistance in enteric bacteria. N Engl J Med 1966;
Isothermal polymerase chain reaction technologies are being 275:888–94.
developed that are relatively inexpensive and can work on 11. Wain J, Hien TT, Connerton P, et al. Molecular typing of multiple-antibiotic-re-
sistant Salmonella enterica serovar Typhi from Vietnam: application to acute and
simple platforms such as dipsticks and these will be vital, relapse cases of typhoid fever. J Clin Microbiol 1999; 37:2466–72.
potentially along with better serological and culture-based 12. Kumar R, Aneja KR, Punia AK, Roy P, Sharma M, Gupta R, Ram S. Changing pat-
tern of biotypes, phage types and drug resistance of Salmonella Typhi in Ludhiana
technologies for typhoid. These diagnostic approaches will be
during 1980–1999. Indian J Med Res 2001; 113:175–80.
used in conjunction with the implementation of better public 13. Smith MD, Duong NM, Hoa NT, et al. Comparison of ofloxacin and ceftriaxone
health management approaches including vaccine campaigns for short-course treatment of enteric fever. Antimicrob Agents Chemother 1994;
38:1716–20.
to bring typhoid under control in endemic regions. However, 14. Parry C, Wain J, Chinh NT, Vinh H, Farrar JJ. Quinolone-resistant Salmonella
it should be noted that vaccination would likely not specif- typhi in Vietnam. Lancet 1998; 351:1289.
15. Wain J, Hoa NT, Chinh NT, et al. Quinolone-resistant Salmonella Typhi in Viet
ically target resistant oversensitive isolates, but it would at Nam: molecular basis of resistance and clinical response to treatment. Clin Infect
least reduce the overall typhoid disease burden. Dis 1997; 25:1404–10.
16. Connerton P, Wain J, Hien TT, et al. Epidemic typhoid in Vietnam: molecular
Finally, it should be noted that the incidence of MDR in typing of multiple-antibiotic-resistant Salmonella enterica serotype Typhi from
typhoid is variable over time. As antibiotic treatment prac- four outbreaks. J Clin Microbiol 2000; 38:895–7.
17. Phan MD, Kidgell C, Nair S, et al. Variation in Salmonella enterica serovar Typhi
tices change, the selective pressure profile is altered, and the
IncHI1 plasmids during the global spread of resistant typhoid fever. Antimicrob
incidence of MDR typhoid has been observed to increase and Agents Chemother 2009; 53:716–27.
decrease over time in a particular geographical region. This 18. Holt KE, Parkhill J, Mazzoni CJ, et al. High-throughput sequencing provides
insights into genome variation and evolution in Salmonella Typhi. Nat Genet
suggests that selection is playing a significant role in the main- 2008; 40:987–93.
tenance of the resistance phenotype and that better antibiotic 19. Wong VK, Baker S, Pickard DJ, et al. Phylogeographical analysis of the dominant
multidrug-resistant H58 clade of Salmonella Typhi identifies inter- and intracon-
stewardship could have a beneficial impact. tinental transmission events. Nat Genet 2015; 47:632–9.
20. Feasey NA, Gaskell K, Wong V, et al. Rapid emergence of multidrug resistant, H58-
Notes lineage Salmonella Typhi in Blantyre, Malawi. PLoS Negl Trop Dis 2015; 9:e0003748.
21. Kuijpers LMF, Phe T, Veng CH, et al. The clinical and microbiological characteristics
Disclaimer. The findings and conclusions contained within are those of enteric fever in Cambodia, 2008–2015. PLoS Negl Trop Dis 2017; 11:e0005964.
of the authors and do not necessarily reflect positions or policies of the 22. Pham Thanh D, Karkey A, Dongol S, et al. A novel ciprofloxacin-resistant sub-
Bill & Melinda Gates Foundation. The views expressed are those of the clade of H58 Salmonella Typhi is associated with fluoroquinolone treatment fail-
authors and not necessarily those of the National Health Service (NHS), ure. Elife 2016; 5:e14003.
Antibiotic Resistance and Typhoid • CID 2019:68 (Suppl 2) • S169
23. Britto CD, Dyson ZA, Duchene S, et al. Laboratory and molecular surveillance of 26. Phoba MF, Barbé B, Lunguya O, et al. Salmonella enterica serovar Typhi produc-
paediatric typhoidal Salmonella in Nepal: Antimicrobial resistance and implica- ing CTX-M-15 extended spectrum β-lactamase in the Democratic Republic of
tions for vaccine policy. PLoS Negl Trop Dis 2018; 12:e0006408. the Congo. Clin Infect Dis 2017; 65:1229–31.
24. Wong VK, Holt KE, Okoro C, et al. Molecular surveillance identifies mul- 27. Klemm EJ, Shakoor S, Page AJ, et al. Emergence of an extensively drug-resistant
tiple transmissions of typhoid in West Africa. PLoS Negl Trop Dis 2016; Salmonella enterica serovar Typhi clone harboring a promiscuous plasmid encod-
10:e0004781. ing resistance to fluoroquinolones and third-generation cephalosporins. MBio
25. Park SE, Pham DT, Boinett C, et al. The phylogeography and incidence of 2018; 9:e00105–18.
multi-drug resistant typhoid fever in Sub-Saharan Africa. Nat Commun 2018; 28. Levine MM, Simon R. The gathering storm: is untreatable typhoid fever on the
9:5094. way? MBio 2018; 9:pii: e00482-18.
Downloaded from https://academic.oup.com/cid/article-abstract/68/Supplement_2/S165/5371231 by guest on 14 April 2019
S170 • CID 2019:68 (Suppl 2) • Dyson et al
You might also like
- Harriet Ugboko and Nandita deDocument16 pagesHarriet Ugboko and Nandita deChockalingam MeenakshisundaramNo ratings yet
- Host-Pathogen Interaction in Invasive Salmonellosis: ReviewDocument9 pagesHost-Pathogen Interaction in Invasive Salmonellosis: ReviewFabsscribNo ratings yet
- Ijms 22 00735Document28 pagesIjms 22 00735Nur AnisaNo ratings yet
- Typhoid Fever Current Concepts.5Document7 pagesTyphoid Fever Current Concepts.5pawitrajayaNo ratings yet
- Overview On Mechanisms of Antibacterial Resistance: Alemayehu Toma, Serawit DeynoDocument10 pagesOverview On Mechanisms of Antibacterial Resistance: Alemayehu Toma, Serawit DeynowaelNo ratings yet
- Microorganisms 10 02006 v2Document15 pagesMicroorganisms 10 02006 v2Novia khasanahNo ratings yet
- Host-Pathogen Interaction in Invasive Salmonellosis: Plos Pathogens October 2012Document10 pagesHost-Pathogen Interaction in Invasive Salmonellosis: Plos Pathogens October 2012Alif RahmanNo ratings yet
- Antimicrobial Resistance A Tale of The Past Becomes A Terrorfor The PresentDocument7 pagesAntimicrobial Resistance A Tale of The Past Becomes A Terrorfor The PresentdssgssNo ratings yet
- Viral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensFrom EverandViral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensNo ratings yet
- The Prevalence of Antibiotic-Resistant Clostridium Species in Iran: A Meta-AnalysisDocument9 pagesThe Prevalence of Antibiotic-Resistant Clostridium Species in Iran: A Meta-Analysisdokteradhit891438No ratings yet
- Typhoid Vaccines ReviewDocument10 pagesTyphoid Vaccines ReviewdragondostNo ratings yet
- Addressing Clinical Safety of AntimicrobialDocument17 pagesAddressing Clinical Safety of Antimicrobialluis chucasNo ratings yet
- Emerging Antibiotic Resistance in Bacteria With Special Reference To IndiaDocument11 pagesEmerging Antibiotic Resistance in Bacteria With Special Reference To IndiaDrSagar GrNo ratings yet
- Drug Resistance in Bacteria: An Emerging ThreatDocument18 pagesDrug Resistance in Bacteria: An Emerging Threatkumari astha rupaliNo ratings yet
- Antifungal Drugs - The Current Armamentarium and Development of New AgentsDocument20 pagesAntifungal Drugs - The Current Armamentarium and Development of New AgentssovalaxNo ratings yet
- Immunological, Cellular and Molecular Events in Typhoid FeverDocument12 pagesImmunological, Cellular and Molecular Events in Typhoid FeverAde RifkaNo ratings yet
- Enteric Fever 2013Document3 pagesEnteric Fever 2013aminceloNo ratings yet
- Mayoclinproc 86 4 014 PDFDocument14 pagesMayoclinproc 86 4 014 PDFAnisoara AvonNo ratings yet
- Jurnal 7Document8 pagesJurnal 7Fida NadhirNo ratings yet
- Coidi 31 449Document6 pagesCoidi 31 449Kavyarani RathodNo ratings yet
- Antibiotics: Relationship Between Virulence and Resistance Among Gram-Negative BacteriaDocument11 pagesAntibiotics: Relationship Between Virulence and Resistance Among Gram-Negative BacteriapfcabsNo ratings yet
- Ijms-22-00735 Id enDocument28 pagesIjms-22-00735 Id enNur AnisaNo ratings yet
- Biomedicine & Pharmacotherapy: ReviewDocument12 pagesBiomedicine & Pharmacotherapy: Reviewkorede juniorNo ratings yet
- The Treasure Called AntibioticsDocument2 pagesThe Treasure Called AntibioticsBenamrane MarwaNo ratings yet
- Resistencia em Fungos - Editorial 2019Document2 pagesResistencia em Fungos - Editorial 2019Dr EnéasNo ratings yet
- Ceftriaxone R Salmonella Typhi 02Document8 pagesCeftriaxone R Salmonella Typhi 02docsumitraiNo ratings yet
- HHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideDocument30 pagesHHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideicaeeNo ratings yet
- AMR - Current Scenario and ChallangesDocument37 pagesAMR - Current Scenario and ChallangesShonit SharmaNo ratings yet
- Typhoid Fever PDFDocument14 pagesTyphoid Fever PDFginstarNo ratings yet
- Antibiotic Resistance in MicrobesDocument13 pagesAntibiotic Resistance in MicrobesMaulida 04No ratings yet
- Antibiotic Resistance Genes in BacteriaDocument22 pagesAntibiotic Resistance Genes in BacteriaGabriel TrevisanNo ratings yet
- Dixit, 2009Document14 pagesDixit, 2009JuniClaudia13No ratings yet
- Infections in The Neutropenic Patient-2001Document27 pagesInfections in The Neutropenic Patient-2001Raisa_90No ratings yet
- The Extended Impact of Human Immunodeficiency Virus/ AIDS ResearchDocument4 pagesThe Extended Impact of Human Immunodeficiency Virus/ AIDS ResearchRNo ratings yet
- Overview:Globalandlocal Impactofantibiotic Resistance: Richard R. Watkins,, Robert A. BonomoDocument10 pagesOverview:Globalandlocal Impactofantibiotic Resistance: Richard R. Watkins,, Robert A. BonomoEduardo Moreira San MartinNo ratings yet
- Journal Pone 0212969Document13 pagesJournal Pone 0212969Indri RemetwaNo ratings yet
- Treatment and Prevention of Enteric (Typhoid and Paratyphoid) Fever - UpToDate 2020Document17 pagesTreatment and Prevention of Enteric (Typhoid and Paratyphoid) Fever - UpToDate 2020Zubair Mahmood KamalNo ratings yet
- ReferatDocument18 pagesReferatFannyNo ratings yet
- Ofy 064Document3 pagesOfy 064Robert StryjakNo ratings yet
- Pw. BiologyDocument18 pagesPw. BiologyARNAV ARYANo ratings yet
- Jurnal LagiDocument18 pagesJurnal LagiElva PatabangNo ratings yet
- Correspondence: Broad-And Narrow-Spectrum Antibiotics: A Different ApproachDocument2 pagesCorrespondence: Broad-And Narrow-Spectrum Antibiotics: A Different ApproachJulio Andro ArtamulandikaNo ratings yet
- Interactions Between Parasites and Human MicrobiotDocument6 pagesInteractions Between Parasites and Human MicrobiotGregorio De Las CasasNo ratings yet
- Tuberculosis - StatPearls - NCBI BookshelfDocument10 pagesTuberculosis - StatPearls - NCBI BookshelfDhany karubuyNo ratings yet
- (Articulo) Patobioma 1 - How Holobionts Get Sick, Toward A Unifying Scheme of Disease PDFDocument4 pages(Articulo) Patobioma 1 - How Holobionts Get Sick, Toward A Unifying Scheme of Disease PDFFernanda PenagosNo ratings yet
- Pseudomonas Baru 4-1Document29 pagesPseudomonas Baru 4-1Nadia Iriana DewiNo ratings yet
- SeminarDocument12 pagesSeminarSatt Michael Sobiono SantosNo ratings yet
- Typhoid FeverDocument14 pagesTyphoid FeverJames Cojab SacalNo ratings yet
- PAIR in Vitro Activity of Pandan Pandanus Amaryllifolius Leaves CrudeDocument23 pagesPAIR in Vitro Activity of Pandan Pandanus Amaryllifolius Leaves CrudeMiftahurrachmahNo ratings yet
- Nihms 940015Document50 pagesNihms 940015Maria Salome Olortegui AceroNo ratings yet
- DtifoDocument11 pagesDtifoDwi atikaNo ratings yet
- TB PaperDocument11 pagesTB PapergwapingMDNo ratings yet
- Shigella Review GuidelineDocument16 pagesShigella Review GuidelineAndi MuftyNo ratings yet
- 2019 Shigella Antibiotic Resistance Mechanism and New Horizons ForDocument31 pages2019 Shigella Antibiotic Resistance Mechanism and New Horizons FormiekekusumaNo ratings yet
- Literature Review SalmonellaDocument7 pagesLiterature Review Salmonellaafdtbwkhb100% (1)
- WHO - AMR - Key FactsDocument9 pagesWHO - AMR - Key Factstanishtarun06No ratings yet
- Antimicrobial Resistance. A Global ChallengeDocument30 pagesAntimicrobial Resistance. A Global Challengeluis sanchezNo ratings yet
- Blrincon - Blrincon - 2023 Nature ReviewsDocument20 pagesBlrincon - Blrincon - 2023 Nature ReviewsDavidf VillabonaNo ratings yet
- The Scourge of Antibiotic Resistance: The Important Role of The EnvironmentDocument7 pagesThe Scourge of Antibiotic Resistance: The Important Role of The EnvironmentMaulida 04No ratings yet
- Contagious Diseases: The Science, History, and Future of Epidemics. From Ancient Plagues to Modern Pandemics, How to Stay Ahead of a Global Health CrisisFrom EverandContagious Diseases: The Science, History, and Future of Epidemics. From Ancient Plagues to Modern Pandemics, How to Stay Ahead of a Global Health CrisisNo ratings yet
- Detection of Breast CancerDocument7 pagesDetection of Breast CancerNunkyRainandaNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakainesNo ratings yet
- AAMDHDHHDDocument6 pagesAAMDHDHHDinesNo ratings yet
- Treatment of Typhoid Fever in Children Comparison of Efficacy of Ciprofloxacin With Ceftriaxone PDFDocument10 pagesTreatment of Typhoid Fever in Children Comparison of Efficacy of Ciprofloxacin With Ceftriaxone PDFAtmayadi GunawanNo ratings yet
- Diagnosis and Staging of Lung Carcinoma With CT Scan and Its Histopathological CorrelationDocument7 pagesDiagnosis and Staging of Lung Carcinoma With CT Scan and Its Histopathological CorrelationinesNo ratings yet
- Aryansah Dwiiiiiiiii AkkandkhsjDocument1 pageAryansah Dwiiiiiiiii AkkandkhsjinesNo ratings yet
- BBB BBBBBBDocument1 pageBBB BBBBBBinesNo ratings yet
- Aryansah Dwiiiiiiiii AkkandkhsjDocument1 pageAryansah Dwiiiiiiiii AkkandkhsjinesNo ratings yet
- Captured Ammunition Bulletin No 1Document34 pagesCaptured Ammunition Bulletin No 1roberto porto100% (1)
- Foundation of EducationDocument31 pagesFoundation of EducationM T Ząřřąř100% (1)
- Imsa Catalog Imsa CatDocument16 pagesImsa Catalog Imsa CatDaniel TelloNo ratings yet
- The Following Functional Health Pattern Assessment Is Based On A 65 Year Old Scottish Woman Who Lives Independently With Her Husband in Their Home at Happy ValleyDocument9 pagesThe Following Functional Health Pattern Assessment Is Based On A 65 Year Old Scottish Woman Who Lives Independently With Her Husband in Their Home at Happy ValleyJajangNo ratings yet
- Module 2 Chem 1Document25 pagesModule 2 Chem 1melissa cabreraNo ratings yet
- Eric Gamalinda - Amigo WarfareDocument88 pagesEric Gamalinda - Amigo Warfareenstone100% (1)
- Altivar ATV61HU55N4 CatalogueDocument4 pagesAltivar ATV61HU55N4 CatalogueEugen Marius BadescuNo ratings yet
- MSDS 442 BulkDocument2 pagesMSDS 442 BulkEliasNo ratings yet
- Rotating Sharp Shooting Multi Target Mechanism Improves Military AimDocument13 pagesRotating Sharp Shooting Multi Target Mechanism Improves Military AimVishal GNo ratings yet
- Friends of Hursley School: Late Summer NewsletterDocument6 pagesFriends of Hursley School: Late Summer Newsletterapi-25947758No ratings yet
- DesignDocument2 pagesDesignAmr AbdalhNo ratings yet
- Financing of New EnterpriseDocument8 pagesFinancing of New EnterpriseSunil BhamuNo ratings yet
- Bandari 2015 Exact SER Expressions of GFDM in Nakagami-M and Rician Fading ChannelsDocument6 pagesBandari 2015 Exact SER Expressions of GFDM in Nakagami-M and Rician Fading Channelssameer khan100% (1)
- Theoretical Development of The Brooks-Corey CapillDocument7 pagesTheoretical Development of The Brooks-Corey CapillDiana Vanessa PedrazaNo ratings yet
- ON Code (Aci 318-77) : Commentary Building Requirements For Reinforced ConcreteDocument132 pagesON Code (Aci 318-77) : Commentary Building Requirements For Reinforced ConcreteAzmi BazazouNo ratings yet
- Physical Activity Guidelines Advisory Committee ReportDocument683 pagesPhysical Activity Guidelines Advisory Committee Reportyitz22100% (1)
- The Practical Welding EngineerDocument154 pagesThe Practical Welding EngineerMohamed Atef0% (1)
- Rational Use of AntibioticsDocument35 pagesRational Use of AntibioticsRahul SharmaNo ratings yet
- Rate Constant Determination 2Document8 pagesRate Constant Determination 2Divya UpadhyayNo ratings yet
- Nursing TheoriesDocument9 pagesNursing TheoriesMichelleneChenTadleNo ratings yet
- (New) Adjustable Voltage Power Supply 55 V - 20A High Power and Current - Automatic Fan On - OffDocument1 page(New) Adjustable Voltage Power Supply 55 V - 20A High Power and Current - Automatic Fan On - OffSek PyroNo ratings yet
- 05.G. Before Takeoff CheckDocument4 pages05.G. Before Takeoff CheckUDAYAPRAKASH RANGASAMYNo ratings yet
- CHAPT 12a PDFDocument2 pagesCHAPT 12a PDFindocode100% (1)
- SampleDocument8 pagesSampleAntônioNo ratings yet
- Rate Analysis-Norms 1Document10 pagesRate Analysis-Norms 1yamanta_rajNo ratings yet
- 3 Soal Ganjil Inggris MaritimDocument8 pages3 Soal Ganjil Inggris MaritimFikri Mu'izNo ratings yet
- Biomass and Bioenergy: Z.N. Akhlisah, R. Yunus, Z.Z. Abidin, B.Y. Lim, D. KaniaDocument20 pagesBiomass and Bioenergy: Z.N. Akhlisah, R. Yunus, Z.Z. Abidin, B.Y. Lim, D. KaniaPutri sinagaNo ratings yet
- K2N Final Internship ReportDocument55 pagesK2N Final Internship ReportAceZeta0% (1)
- Detailed Lesson Plan Boyle's LawDocument9 pagesDetailed Lesson Plan Boyle's LawTeacher Derick Daet86% (7)
- Surat Kecil Untuk TuhanDocument9 pagesSurat Kecil Untuk TuhanAsgarPurnamaNo ratings yet