Professional Documents
Culture Documents
Diuretics
Uploaded by
Lee Ann Almeria0 ratings0% found this document useful (0 votes)
10 views4 pagesPCOL
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPCOL
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views4 pagesDiuretics
Uploaded by
Lee Ann AlmeriaPCOL
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
Diuretics & Other Drugs That Act on the Kidney
Diuretic - is an agent that increases urine volume
Natriuretic - causes an increase in renal sodium excretion
Aquaretic - increases excretion of solute-free water
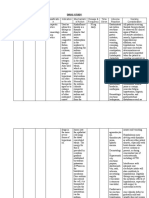
DRUG CLASS Member Drug PK PD Indication Toxicity Contraindication
THIAZIDE Chlorothiazide • not very lipid- • inhibit NaCl reabsorption • Hypertension 1. Hypokalemic Metabolic • Hepatic cirrhosis
soluble from the luminal side of • Heart failure Alkalosis and • Borderline renal
• must be given in epithelial cells in the DCT • Nephrolithiasis due to Hyperuricemia failure
relatively large by blocking the Na+/Cl− idiopathic hypercalciuria 2. Impaired Carbohydrate • Heart failure
doses • Nephrogenic diabetes Tolerance
transporter (NCC)
• only thiazide • enhance Ca2+ insipidus • Hyperglycemia
available for reabsorption from effects 3. Hyperlipidemia
parenteral in both the proximal and 4. Hyponatremia
administration 5. Allergic Reactions
distal convoluted tubules
• • Photosensitivity or
Hydrochlorothiazide more potent • Action depends in part on
(HCTZ) • should be used in generalized
renal prostaglandin
much lower doses dermatitis occurs
production
rarely
Chlorthalidone • slowly absorbed • inhibited by NSAIDs under
• Hemolytic anemia
• has a longer certain conditions
• useful in the treatment of • Thrombocytopenia
duration of action
• Acute necrotizing
Indapamide • excreted primarily kidney stones caused by
pancreatitis
by the biliary system hypercalciuria
• enough of the active
form is cleared by
the kidney to exert
its diuretic effect in
the DCT
POTASSIUM- Spironolactone • Onset and duration • Spironolactone & 1. states of 1. Hyperkalemia 1. Patients with
SPARING of action are Eplerenone mineralocorticoid excess 2. Hyperchloremic chronic renal
DIURETICS determined by the Inhibition by direct or hyperaldosteronism Metabolic Acidosis insufficiency
kinetics of the pharmacologic primary 3. Gynecomastia 2. Patients with liver
aldosterone antagonism of hypersecretion (Conn Spironolactone disease
response mineralocorticoid ’s syndrome, ectopic 4. Acute Renal Failure 3. Concomitant use of
• Substantial receptors Triamterene + other agents that
adrenocorticotropic
inactivation occurs • Amiloride & Triamterene Indomethacin blunt the renin-
hormone production)
in the liver inhibition of Na+ influx 5. Kidney Stones angiotensin system
secondary
• slow onset of action through ion channels in Triamterene is only 4. Strong CYP3A4
hyperaldosteronism
Eplerenone • greater selectivity the luminal membrane slightly soluble and inhibitors (eg,
(evoked by heart
for the • Ularitide (recombinant may precipitate in erythromycin,
failure, hepatic
mineralocorticoid urodilatin) the urine fluconazole,
cirrhosis, nephrotic
receptor blunts Na+ uptake and syndrome, or other
diltiazem, and
• less active on Na+/K+ -ATPase in grapefruit juice) can
conditions associated
androgen and markedly increase
progesterone collecting tubules and with diminished blood levels of
receptors increases GFR through effective eplerenone
Amiloride • direct inhibitors of its vascular effects intravascular volume
Na + influx in the • Nesiritide 2. blunt the K+ secretory
CCT (cortical commercially available response in enhanced
collecting tubule for intravenous use only mineralocorticoid
Triamterene • metabolized in the increases GFR and secretion and excessive
liver blunts Na+ delivery of Na+ to distal
• renal excretion is a reabsorption in both nephron sites
major route of proximal and collecting 3. slow the progression of
elimination for the tubules albuminuria in diabetic
active form and the patients
metabolites 4. reduce myocardial
• shorter half-life perfusion defects after
myocardial infarction
OSMOTIC Mannitol poorly absorbed by • major effect in the 1. Increase of Urine 1. Extracellular Volume
DIURETICS the GI tract, proximal tubule and the Volume Expansion
Orally; causes descending limb of Henle’ 2. Reduction of Intracranial • complicate heart
osmotic diarrhea and Intraocular Pressure failure
s loop
rather than diuresis • may produce florid
• oppose the action of ADH
must be given in the collecting tubule
pulmonary edema
intravenously • Headache, nausea,
• prevents the normal
not metabolized and absorption of water by
and vomiting
is excreted by 2. Dehydration,
interposing a
glomerular filtration Hyperkalemia, and
countervailing osmotic
within 30–60 force; urine volume Hypernatremia
minutes, without 3. Hyponatremia
increases
any important • In patients with
• urine flow rate: the
tubular severe renal
contact time between
reabsorption or impairment,
fluid and the tubular
secretion parenterally
epithelium
administered
reducing Na+ and water
mannitol cannot be
reabsorption
excreted and is
• resulting natriuresis is of
retained
lesser magnitude than the
intravenously
water diuresis
excessive water loss and
hypernatremia
ANTIDIURETIC Conivaptan 5–10 hours half-life • inhibit the effects of ADH 1. Syndrome of 1. Nephrogenic Diabetes
HORMONE Demeclocycline in the collecting tubule Inappropriate ADH Insipidus
ANTAGONISTS Tolvaptan • Conivaptan and tolvaptan Secretion 2. Renal Failure
Lithium 12–24 hours half-life are direct ADH receptor • Demeclocycline • Lithium and
Demeclocycline antagonists (600–1200 mg/d) Demeclocycline
• lithium and 3. Chronic interstitial
demeclocycline reduce • tolvaptan (15–60 nephritis
ADH-induced cAMP by mg/d) • Long-term
mechanisms that are not 2. Other Causes of lithium therapy
yet completely clarified Elevated Antidiuretic 4. Dry mouth and thirst
Hormone 5. Hypotension
• Patients with heart • Tolvaptan
failure - blockade of 6. Demeclocycline should
V1a receptors by be avoided in patients
conivaptan leads to with liver disease and in
decreased children younger than
peripheral vascular 12 years
resistance and
increased cardiac
output
You might also like
- Diuretics Module - Promote Excretion of Water and ElectrolytesDocument7 pagesDiuretics Module - Promote Excretion of Water and ElectrolytesBenzy Anne MermalNo ratings yet
- Taking The Long View of Canine Hypoadrenocorticism OutlineDocument4 pagesTaking The Long View of Canine Hypoadrenocorticism OutlineJuniClaudia13No ratings yet
- Drug Study On Emergency Drugs Final - )Document12 pagesDrug Study On Emergency Drugs Final - )wen_pil100% (3)
- Diabetes in Hospital: A Practical Approach for Healthcare ProfessionalsFrom EverandDiabetes in Hospital: A Practical Approach for Healthcare ProfessionalsNo ratings yet
- Agent For Treating Heart FailureDocument26 pagesAgent For Treating Heart FailureClarisse SuanNo ratings yet
- Anti Hypertensive DrugsDocument113 pagesAnti Hypertensive DrugsRobert DowneyNo ratings yet
- Drug StudyDocument3 pagesDrug StudyCyril_Cybernat_1553No ratings yet
- ENDOCRINE 1.3 Incidentallomas, Conn's SyndromeDocument5 pagesENDOCRINE 1.3 Incidentallomas, Conn's SyndromeJem QuintoNo ratings yet
- Chapter 6 - Endocrine System 2Document12 pagesChapter 6 - Endocrine System 2AyeshaNo ratings yet
- FMBularan-Urinary-Drug StudyDocument3 pagesFMBularan-Urinary-Drug StudyfransmallarebularanNo ratings yet
- Drug Study: SaluronDocument4 pagesDrug Study: Saluronunkown userNo ratings yet
- Drug Study: SaluronDocument4 pagesDrug Study: Saluronunkown userNo ratings yet
- Renal PharmacologyDocument7 pagesRenal PharmacologywanichysonlyNo ratings yet
- Levodopa Management Side EffectsDocument6 pagesLevodopa Management Side EffectsMajo Coronel100% (1)
- PEDIA2 2.01b Fluids Electrolytes Summary TablesDocument4 pagesPEDIA2 2.01b Fluids Electrolytes Summary TablesVon HippoNo ratings yet
- Toxicology Toxidromes and TreatmentsDocument40 pagesToxicology Toxidromes and TreatmentsTan Geok EngNo ratings yet
- KidneyDocument19 pagesKidneySridharNo ratings yet
- Pharmacology Final TermDocument19 pagesPharmacology Final TermDWIGHT LESTER O. MANGILANo ratings yet
- Drug NameDocument31 pagesDrug Namelawha.chaand02No ratings yet
- DiureticsDocument5 pagesDiureticsUsmanNo ratings yet
- Anaesthesia For Ect March 2020Document120 pagesAnaesthesia For Ect March 2020Sangkaran KumarNo ratings yet
- HPNDocument32 pagesHPNkaren GoNo ratings yet
- Drugstudy PotassiumchlorideDocument3 pagesDrugstudy Potassiumchloridetrina412No ratings yet
- Drug Study About Carbamazepine Used For Down Syndrome Patients With Seizure PDFDocument4 pagesDrug Study About Carbamazepine Used For Down Syndrome Patients With Seizure PDFAlexander Miguel M. AbasNo ratings yet
- Carbamazepine drug study for Down syndrome patientsDocument4 pagesCarbamazepine drug study for Down syndrome patientsAlexander Miguel M. AbasNo ratings yet
- Carbamazepine drug study for seizures in Down syndrome patientsDocument4 pagesCarbamazepine drug study for seizures in Down syndrome patientsAlexander Miguel M. AbasNo ratings yet
- Furosemide Drug StudyDocument2 pagesFurosemide Drug StudyCrisha Ann Billones BacutaNo ratings yet
- Drug Study 2Document4 pagesDrug Study 2EARL GERALD RICAFRANCANo ratings yet
- Psychiatric Drugs - ZarinaDocument25 pagesPsychiatric Drugs - Zarinaszarina_7No ratings yet
- Diclogen Drug GuideDocument9 pagesDiclogen Drug GuideRasco, Allen jayNo ratings yet
- Drugs For Diabetes PDFDocument4 pagesDrugs For Diabetes PDFDylan RastoNo ratings yet
- Pemicu 2 KGD SherDocument175 pagesPemicu 2 KGD SherSheren ReginaNo ratings yet
- Drug Study-Ibekwe Njideka VanessaDocument2 pagesDrug Study-Ibekwe Njideka VanessaFavor ColaNo ratings yet
- Laranang, Mica Joy R. Drug Study: BSN 123 Group 90Document5 pagesLaranang, Mica Joy R. Drug Study: BSN 123 Group 90Gerard Louise Esmao RNNo ratings yet
- Drug Induced Liver DisordersDocument19 pagesDrug Induced Liver Disorders22 Prem PatelNo ratings yet
- Drug Induced Liver Diseases HamidDocument57 pagesDrug Induced Liver Diseases HamidKhadija KamranNo ratings yet
- HYPONATREMIA Final HandoutsDocument2 pagesHYPONATREMIA Final HandoutsSahata BOHARINo ratings yet
- Institute of Nursing BSN110-GROUP 39 S.Y. 2010-2011: Lab Test Considerations: MonitorDocument5 pagesInstitute of Nursing BSN110-GROUP 39 S.Y. 2010-2011: Lab Test Considerations: MonitorIvy Grace LimNo ratings yet
- Hypertermia CrisisDocument1 pageHypertermia CrisislisaNo ratings yet
- Epoetin Drug Study GuideDocument5 pagesEpoetin Drug Study Guidejasper pachingelNo ratings yet
- IV Fluid Replacement TherapyDocument12 pagesIV Fluid Replacement TherapyKamran Sheraz100% (1)
- MS Drug Study 1Document6 pagesMS Drug Study 1Elijah MarfilNo ratings yet
- NCM 112 - Renal System-Pharma-Tubes and DrainsDocument2 pagesNCM 112 - Renal System-Pharma-Tubes and DrainsCailah Sofia SelausoNo ratings yet
- Hypermagnesemia Handouts Group 9Document3 pagesHypermagnesemia Handouts Group 9Risha Ethel BerondoNo ratings yet
- PHS CVSDocument25 pagesPHS CVStewogbadeomobuwajo005No ratings yet
- ANTI-GOUT DRUGS New11Document31 pagesANTI-GOUT DRUGS New11Ghina RizwanNo ratings yet
- Compensated Vs Decompensated CirrhosisDocument4 pagesCompensated Vs Decompensated CirrhosisMary Rose EstradaNo ratings yet
- Furosemide Mechanism, Uses, Side Effects & Nursing CareDocument2 pagesFurosemide Mechanism, Uses, Side Effects & Nursing CareFavor ColaNo ratings yet
- ANTIPSYCHOTICSDocument25 pagesANTIPSYCHOTICSCheetahboi Shopee100% (4)
- Ekg en HiperkalemiaDocument18 pagesEkg en HiperkalemiaMariana SgNo ratings yet
- Medical ManagementDocument15 pagesMedical ManagementDana RuizNo ratings yet
- Drug Study FinalDocument8 pagesDrug Study FinalWendy EscalanteNo ratings yet
- Print MeDocument4 pagesPrint MeDoneva Lyn MedinaNo ratings yet
- Drug Study Potassium ChlorideDocument5 pagesDrug Study Potassium ChlorideKenneth Mark B. TevesNo ratings yet
- Adverse Drug ReactionsDocument5 pagesAdverse Drug ReactionsfouzaNo ratings yet
- DRUGS in E-CARTDocument8 pagesDRUGS in E-CARTRagual Mica100% (1)
- Drug StudyDocument3 pagesDrug Studysinister17No ratings yet
- PhIT 002Document1 pagePhIT 002Lee Ann AlmeriaNo ratings yet
- Chapter 34 CoagulationDocument4 pagesChapter 34 CoagulationLee Ann AlmeriaNo ratings yet
- Chapter 4 Saponin GlycosidesDocument5 pagesChapter 4 Saponin GlycosidesLee Ann AlmeriaNo ratings yet
- Chapter 4 GlycosidesDocument1 pageChapter 4 GlycosidesLee Ann AlmeriaNo ratings yet
- Chapter 4 Saponin GlycosidesDocument5 pagesChapter 4 Saponin GlycosidesLee Ann AlmeriaNo ratings yet
- Assignment in Hospital Pharmacy: Submitted By: Almeria, Lee Ann T. MW 9:00 - 10:00Document3 pagesAssignment in Hospital Pharmacy: Submitted By: Almeria, Lee Ann T. MW 9:00 - 10:00Lee Ann AlmeriaNo ratings yet
- Chapter 3 HeteroglycansDocument6 pagesChapter 3 HeteroglycansLee Ann AlmeriaNo ratings yet
- Pharmacist VenturesDocument3 pagesPharmacist VenturesLee Ann AlmeriaNo ratings yet
- Pricing Strategies for Drugstore Outlets and ClientsDocument1 pagePricing Strategies for Drugstore Outlets and ClientsLee Ann AlmeriaNo ratings yet
- Manual de Intrucciones Oximag PDFDocument134 pagesManual de Intrucciones Oximag PDFJose Ivan Carvajal CortizosNo ratings yet
- PDA Points To Consider For Aseptic ProcessingDocument14 pagesPDA Points To Consider For Aseptic ProcessingKevin ZhaoNo ratings yet
- Congenital Adrenal HyperplasiaDocument5 pagesCongenital Adrenal HyperplasiaduapajNo ratings yet
- Devesh Mahajan ResumeDocument5 pagesDevesh Mahajan Resumejobs shahiNo ratings yet
- Study of Prevelance of Rhesus (RH) Blood Group Antigens Profiling Among Blood DonorsDocument7 pagesStudy of Prevelance of Rhesus (RH) Blood Group Antigens Profiling Among Blood Donorsindu mathiNo ratings yet
- UAE HospitalsDocument20 pagesUAE Hospitalsswati_progNo ratings yet
- ResuscitationDocument38 pagesResuscitationsonics issacNo ratings yet
- Out 7 PDFDocument8 pagesOut 7 PDFAfif Al FatihNo ratings yet
- Univan Maritime (H.K.) Limited: Rug and Alcohol Olicy EctionDocument1 pageUnivan Maritime (H.K.) Limited: Rug and Alcohol Olicy Ectionnavigator1977No ratings yet
- Computed Tomography (CT) - ChestDocument8 pagesComputed Tomography (CT) - ChestGloria Evasari RitongaNo ratings yet
- MCQ OphthalmoDocument62 pagesMCQ Ophthalmosafasayed100% (1)
- Fibrous Protein or ScleroproteinDocument4 pagesFibrous Protein or ScleroproteinMia DimagibaNo ratings yet
- Olimpus - System Guide EndosDocument100 pagesOlimpus - System Guide EndosAna Prisacariu100% (1)
- Aki & CKDDocument61 pagesAki & CKDChengzhi KhorNo ratings yet
- Cavernous Hemangioma of Mandible: A Rare Case ReportDocument5 pagesCavernous Hemangioma of Mandible: A Rare Case ReportAna CernaianuNo ratings yet
- Nasal Steroid Proven Effective Rhinitis TreatmentDocument80 pagesNasal Steroid Proven Effective Rhinitis TreatmentYuliastuti RahayuNo ratings yet
- Chapter Orofacial PainDocument34 pagesChapter Orofacial PainintanNo ratings yet
- Nama-Nama Obat PrekurDocument2 pagesNama-Nama Obat PrekurWatini Daiman Fii QolbyNo ratings yet
- 2012 Pittsburgh Black Business Directory PDFDocument104 pages2012 Pittsburgh Black Business Directory PDFMhacblink ManNo ratings yet
- Flutter and Other DeviceDocument39 pagesFlutter and Other DeviceEira LopezNo ratings yet
- Adoption of Plea Bargaining Framework in Drug CasesDocument10 pagesAdoption of Plea Bargaining Framework in Drug CasesMagtanggol HinirangNo ratings yet
- Value Guided Healthcare As A Platform For Industrial Development in Sweden - Feasibility StudyDocument85 pagesValue Guided Healthcare As A Platform For Industrial Development in Sweden - Feasibility StudyTorresLiangNo ratings yet
- HPLC Dad1Document13 pagesHPLC Dad1Siti HartinaNo ratings yet
- HVAC Systems for Health Care Facilities ConferenceDocument75 pagesHVAC Systems for Health Care Facilities ConferenceAhmed AbdelzaherNo ratings yet
- MCQ HemodynamicsDocument2 pagesMCQ HemodynamicsKehkashan Khan80% (5)
- Tests of SignificanceDocument111 pagesTests of SignificanceMeer100% (1)
- Hannah Dion Resume 2 PageDocument2 pagesHannah Dion Resume 2 Pageapi-449543796No ratings yet
- The Strategy of Preventive Medicine: Geoffrey RoseDocument8 pagesThe Strategy of Preventive Medicine: Geoffrey RosePaulNo ratings yet
- CV Dr. SM Safdar Ashraf Prin. Inv.Document13 pagesCV Dr. SM Safdar Ashraf Prin. Inv.Erin BlairNo ratings yet
- S - LANSS Questionnaire Polish VersionDocument4 pagesS - LANSS Questionnaire Polish VersionBartosz Zaczek100% (1)