Professional Documents
Culture Documents
Jacob Unit V Pharma
Jacob Unit V Pharma
Uploaded by
Nikky Rossel Flores0 ratings0% found this document useful (0 votes)
11 views4 pagesOriginal Title
jacob Unit v pharma.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views4 pagesJacob Unit V Pharma
Jacob Unit V Pharma
Uploaded by
Nikky Rossel FloresCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
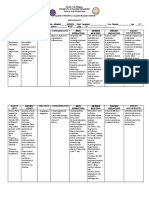
NON-STEROIDAL • Allergy to ASA
ANTI-INFLAMMATORY AGENTS • Children and pregnant women
• Strong anti-inflammatory and analgesic effects but very little antipyretic • PONSTAN, DOLFENAL
effects • Piroxicam – 20 mg as single or divided dose daily
• Inhibit prostaglandin synthesis by inhibiting the enzyme cyclooxygenase • RA and OA, GA, dysmenorrhea
(Cox-1 and Cox-2) • Effects of therapy seen in two weeks
Uses • Better compliance
• Mild to moderate pain • Take with food
• Dysmenorhea • Report abdominal pain, bruising, change in color of stools
• Discomfort from minor surgery • FELDENE
• Inflammatory processes • Tinoxicam – 20 mg
• Arthritis • RA,OA,GA, tendonitis, bursitis
Classifications • Se: edddema, wt gain, inc BUN, volume depletion
• Proprionic Acid derivatives; • ASA: inc GI symtos
– Ibuprofen (Alaxan,Muskelax, Advil) • Don’t give with anti-coag & pot. Sparing diuretics
– Naproxen – (Naprosyn, Flanax) • Take with meals
– Flubiprofen (Ansaid) • TILCOTIL
– Ketoprofen (Orudis • Indomethacin 25 mg BID or TID, max 150-200mg per day
– Oxaprozin (Daypro) • Not for routine use
Classifications • GA, OA, pre-term labor
• Acetic Acids: • CI: angioedema, PUD, pregnancy , asthma
– Diclofenac (Volotaren • GI: life threatening: thrombocytopenia, aplastic anemia,
– Etodolac (Lodine) hypokalemia
– Ketorolac (Torodal) • DI: decreases effect of antihypertensives
– Nabumetone (Relafen • Tke with food, blood tests
– sulindac (Clinoril) • INDOCIN
– Tolmetin (Tolectin) COX-2 INHIBITORS
• Fenamates: Action: decreases pain and inflammation by blocking only COX-2, which keeps the
– Mefenamic acid ( Ponstan, Dolfenal stomach lining intact, hence bleeding and gastric discomfort
– meclofenamate Therapeutic uses:
• Oxicams – Osteoarthritis
– Piroxicam (Feldene) – Rheumatoid arthritis
– Tinoxicam (Tilcotil) – Acute pain and dysmenorrhea
• Indoles Advantages: decreased gastric irritation, better compliance with single daily doses
– indomethacin Disadvantages: contraindicated in patients allergic to ASA and sulfonamides, may
Contraindications impair bone healing, more expensive, and increase the risk of cardiovascular events
• Allergies to NSAIAs including MI.
• Salicylates CI :in patients prone to stroke & heart attacks
• Peptic ulcer Preparations:
• Known GI bleeding celecoxib (Celebrex) 200 mg OD or 100mg Bid.
• Pregancy or lactation rofecoxib (Vioxx) 12.5– 25 mg po
Adverse reactions & side effects
• GI irritation Non-Opiate
• Diarhea, n/V, abdominal pain (Non- Narcotic)
• Vomiting, flatulence Analgesics-Antipyretics
• Bleeding
• Dizziness, lightheadedness SALICYLATES
• rash analgesic, antipyretic, anti-inflammatory, decreased platelet aggregation
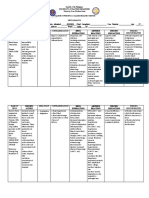
• Ibuprofen -300 mg 4x daily PO or 400-800 mg 3-4x daily • Acetylsalicylic acid (ASA, Aspirin),
• Monitor for gastric iritation & visual changes • choline magnesium trisilicate,
• Take with meals, • choline salicylate,
• MIDOL, ALAXAN, MUSKELAX • salsalate
• Naproxen – 250-500 mg 2x daily PO Actions
• Do not give with ASA, give with meals • Relieve pain by inhibiting prostaglandin through the inhibition of
• May prolong bleeding time, monitor CBC cyclooxygenase an enzyme needed for its production
• Observe for development of black stools Cox -1 protects stomach lining & regulates
• Periodic eye exam blood platelets, Inhibition decreases
• - FLANAX, NAPROSYN stomach protection hence bleeding may occur
• Diclofenac – 50-75 mg 2-3x /day PO Cox 2 – triggers pain and inflammation. When
• Use in pregnancy may cause miscarriage inhibited pain is reduced and inflammation
• VOLTAREN
• Ketorolac • Anti-pyretic effect by blocking of a prostaglandin mediator of pyrogens that
• IM 30-60 mg, then 15-30 q 6h can increase body temperature at the thermoregulating center of the
• Oral: 10 mg q 4-6h hypothalamus
• IV 15-30 mg q 6h not to exceed 120 mg/day • Inhibit platelet aggregation by inhibiting thromboxane A synthesis
• Use only for less than 1 week
• Administer round the clock for best effect Therapeutic Uses
• TORODAL • Mild to moderate pin
• Mefenamic acid – 500 mg q 4-6h PO, max of 1 week • Fever of bacterial and viral origin
• CTBT, ( agranulocytosis, aplastic anemia) • arthritis and muscular pains
• give with food, • prophylaxis for myocardial infarction
• do not use for more than 1 week Contraindications…
• Enhances effect of oral coagulants • Child with varicella and influenza
• CI: PUD, IBD, hepatic & renal ds • Hemophilia and other bleeding disorders
• Peptic ulcer – Hepatic and renal function tests
• Children with viral fevers – Administer with a full glass of water
Drug Interactions… – Assess type and intensity of pain
• Anticoagulants and Thrombolytics [ increases risk of bleeding – Assess patient’s temperature
• NSAIA and corticosteroids - increased risk for GI bleeding – Avoid alcohol as it increases liver toxicity
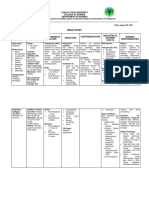
Usual dosage… – Avoid combination with ASA, NSAIA
• Fever, mild to moderate musculoskeletal pain: – do not use for more than 5 days in children and 10 days in
– 325-650 mg PO q 3-4h for pain adults
• Dysmennorrhea: 650 mg PO q 4-6 h • Report signs of toxicity: N/V, abdominal pain,
• Rheumatic fever 975-1300 mg PO 4-6x daily • Methemoglobinemia: SOB, weakness, headache, dizziness
• Rheumatoid arthritis: 3.6-5.4 g PO daily in divided doses • Hemolytic anemia: paleness, weakness, skipped heart beats
• Prevent TIAs; 325 mgPO qid or 650 mg PO bid • Chronic poisoning: SOB, fast weak pulse, cold extremeties, unexplained
• Prevent recurrent MI: 325 mg PO daily bleeding, bruising,sore throat, fatigue
Adverse effects… • Liver toxicity: jaundice, dark urine, clay colored stools
• GI: nausea, vomiting, diarrhea, epigastric pain and GI bleeding are most • PREPARATIONS:
common. Give with food. – Anadol
• CNS: salicylsm at overdose levels – Panadol
• Allergic reactions are also common – Tylenol
• Respiatory: alkalosis – Biogesic
• Prolonged use – bilateral hearing loss – D/c drug – Calpol
Salicylism (overdose toxicity) – Tempra
• Occurs with high doses of ASA Drugs to Treat Pain, Inflammation and Fever: Analgesics & Antipyretics
• Mild: N/V, hyperventilation, headache, mental confusion, dizziness, tinnitus PAIN
• Severe: restlessness, delirium, hallucinations, convulsions, coma, • UNPLEASANT SENSATION
respiratory and metabolic acidosis, death from respiratory failure • CAUSES DISCOMFORT,
Treatment… • DISTURBS SLEEP
• Gastric lavage • INTERFERES WITH NORMAL DAILY ACTIVITIES
• Activated charcoal through NGT • SYMPTOM OF AN UNDERLYINF DISEAS PROCESS.
• Forced alkaline diuresis PAIN CONCEPTS
• Hemodialysis • COMPONENTS:
• Treat hyperthermia and convulsions – PHYSICAL – SENSATION OF PAIN
• correct acid-base balance – PSYCHOLOGICAL – EMOTIONAL RESPONSE
Nursing responsibilities… Sources of Pain
• Take medicines with a full glass of water, peferrably with food • Illness
• Monitor history of GI disorder, bleeding • Medical or surgical procedures
• Assess pt for reactions to salicylate and signs of overdosage • Injury/trauma
• Report hearing loss • Immobility
• Do not use below 18 y.o – linked Reye’s syndrome in children • Nursing procedures
• Discard tabs with a vinegar-like odor • Movement
• Do not crush or chew • Dressing change
• Wound care
NON-SALICYLATES Types of Pain
• Acetaminophen/paracetamol • Acute vs Chronic
– ACTION: hypothalamic effect sweating and vasodilation; – Acute –needed upon request, parenteral
inhibit CNS prostaglandin synthesis – Chronic – regular schedule, oral
– Antipyretic-analgesic with less GI effects • Mild, Moderate vs Severe
– no Reye’s syndrome, • Superficial, Visceral and Somatic
– does not alter blood clotting or respiration – superficial – skin, mucus membranes*
– no significant anti-inflammatory effect – Visceral – smooth muscles, organ systems*
– DOSE: 325-260 mg q 4-6 hours – Somatic – skeletal muscles, joints, ligaments
• Therapeutic Uses * narcotics
– Fever in bacterial or viral infections Pain Measurement
– myalgia, musculoskeletal pain, immunization • Pain Threshold – level of stimulus resulting in the perception of pain
• Adverse effects • Pain Tolerance – amount of pain an individual can withstand without
– Hepatoxicity , jaundice, nephrotoxicity, disrupting normal function and without requiring an analgesic.
– allergy, Pain Theories
– hemolytic anemia • Gate Theory
• Precautions – PAINFUL STIMULI CAUSES RELEASE PF HISTAMINE
– C/I in malnourished clients and chronic ROH abuse SEROTONIN
– Overdose in acute hepatic failure can cause death BRADYKININ
– Adminsister antidote within 8-10 hours of overdose: PROSTAGLANDIN
acetylcysteine IV to reduce liver damag - STIMULI INITIATE ACTION POTENTIALS ALONG A
– Do not take with alcohol SENSOY NERVE
• Drug interactions - SENSITIZE PAIN RECEPTORS
– Alcohol increases toxicity] Gate Theory
– Loop diuretics – decreases plasma renin activity • A Fibers
– NSAIDS – increases risk of hypertension – Large covered with myelin sheath
– Oral contraceptives – increase liver breakdown of – Alpha, beta, gamma and delta fibers
acetaminophen – Alpha – largest, rapid transmission, sharp well localized pain
– Rifampin – increased hepatoxicity from peripheral areas
– Isoniazid – increased risk of hepatotoxicity – Delta – smaller
– Smoking – decrease serum acetaminophen levels and increased • C Fibers
liver breakdown of acetaminophen – Small, unmyelinated
• NURSING RESPONSIBILITIES: – Slow transmission of impulses
– Dull, nonlocalized pain • constipation, nausea & vomiting, lightheadedness, constipation, confusion,
Gate Theory disorientation, orthostatic hypotension itching
• Pain and other sensory fibers enter SC and ascend to the brain (spinal gate) • Adverse effects (Reportable)
• respiratory depression (morphine, fentanyl
• Cells in substantia geltinosa (Dorsal horn) – acts as a gate to regulate flow of
• and hydromorphone – c/I labor,
impulses • lactating and children)
– Alters sensation of pain from peripheral nerve fibers to the • euphoria and dependence
brain • laryngospasm, apnes
PAIN STIMULI Morphine
– Moderate to severe pain, post-op
A Fibers C Fibers – Acute MI
– Cancer (liquid morphine –Roxanol)
Closes dorsal Horn gate opens gate in dorsal horn – Severe pain in terminally ill patients
– Dosage: oral 10-30 mg q 4h
• SC 5-20 mg q 4h, IV: 1.5-2.5 mt
Decrease Transmission of impulses
• Children –IV, SC IM .1-.2 mg/kg q 1-2 h
transmission of impulses cortex
• Rectal: 10-20 mg q 4
• Fentanyl citrate (Sublimaze)
Endorphins & Enkephalins
• Brain peptides found to have opiate like activity – epidural anesthesia and analgesia
• Act as neurotransmitters/neuromodulators – Cancer
• Pain stimuli release of endorphins/enkephalins bind to opiate receptors – Monitor closely for respiratory depression
in CNS inhibit impulse transmission – Dosage IM,IV Adults: .02-.1 mg
Basis for Pain Management • Children 2-12 y: 2-3 mcg/kg
• Treatment of cause • Transdermal patch: one patch q 48-72 h, 25
• Safest and most effective analgesic
mcg/hr
• Psychological support
• Use of other measures, position change, back rubs, etc. • Hydromorphone (Dilaudid)
Analgesics – moderate to severe pain with tolerance to morphine
– Long term analgesia as in cancer
Drugs that relieve pain without causing loss of consciousness – Terminal diseases
Non-narcotics and Narcotics – Dose – 5-10 mg q 4-6 h
Opiods – Administer round the clock in severe pain
Opiod agonists – Respiratory depression more common than in morphine
Opiod Antagonists • Methadone
Non-opiods
– severe pain in end stage cancer, HIV, chronic surgical pain
– Less sedation unless after repeated doses
Selecting the Proper Analgesic
• Effectiveness of the agent – Common SE: constipation
• Duration of Action – Dose
• Desired duration of therapy • A: 2.5-10 mg q 3-4 h
• Ability to cause drug interactions • C: .1 mg/kg q 6-8 h
• Hypersensitivity of the client • Meperidine (demerol)
• Available routes of administration – Kappa receptors
Mechanisms of Action
– Shorter action than morphine
• Opiod & Opiod-like – bind to opiod receptors in the CNS act as agonists
– Metabolized in the liver
of endogenously occuring peptides decrease permeability of cell
– Potentiate CNS depressants
membrane to Sodium diminished transmission of pain impulses
– Monitor respirator depression and liver dysfunction
• Opiod antagonists – bind with opiod receptors, block the binding of opiod
– 50-150 mg q 4h po/IM/SC (A)
and opiod-like drugs, endorphins and enkephalins
– 1.1-1.8 mg/kg bw q3-4h not to exceed 100 mg
Therapeutic effects:
• Codeine – 15-60 mg PO IM SC
analgesia, cough suppression, decrease GI motility, adjunct to anesthesia – Analgesic antitussive, antidiarrheal effects, mild to moderate
• Common SE: sedation, nausea, vomiting pain
• Monitor: orthostatic hypotension, respiratory depression, urinary retention – Fluid hydration
Mechanisms of Action – Administer with food or milk to reduce gi distress
• Non-opiods: • Tramadol (Tramal)
– Salicylates – affect hypothalamus, inhibits prostaglandin – 50 mg cap 3-4x /day max 400 mg
synthesis preventing sensitization of pain receptors • Levorphanol (Levo-Dromoran)
– Non-steroidal anti-inflammatory agents – inhibit prostaglandin
– Oderate to severe pain, visceral pain assoc with terminal CA,
synthesis renal & biliary colic< MI, tauma, post-op pain
OPIODS • (Dolophine)
• Opium – poppy plant, produces euphoria – Primarily to treat withdrawal syndrome in heroine or morphine
• Morphine – active component isolated from Opium
dependence
• Uses:
• Oxymorphone ( Numorphan)
– moderate to severe pain from visceral sources (GIT, internal
– Similar to morphine, except:causes more N/V and psychic
organs)
effects, less constipating and less cough suppression
– Cough suppressant
– Moderate to severe pain, pre-op med. OB analgesia,
– Suppression of GI motility and secretions – 1-1.5 mg IM or Sc q 6 h, .5mg IV, 5 mg q 4-6h rectally
– General anesthetic adjunct – Give with milk or meals
• Specific mechanism: • Propoxyphene (Darvon)
– Act on mu, kappa and sigma receptors
– Mild analgesic, may be combined with ASA or acetaminophen
• Mu- control morphine-like effects – analgesia,
– Used in patients with history of alcohol intake
euphoria and respiratory depression
• Mixtures
• Kappa – analgesia, sedation miosis • Brompton’s cocktail
• Sigma – control hallucinatory activity, respiratory – Mixture of morphine, cocaine, dextroamphetamine and alcohol
and vasomotor stimulation – Given to terminally ill clients for relief of sever cancer pain
– Medullary cough center suppression –codeine
CONTRAINDICATIONS
– Suppression of gi motility
– Drug allergies
• Common side effects – Increased ICP
– Acute asthma, chronic airway problems – Abdominal cramps
– Elderly with renal ds. Pulmonary ds. CHF, liver ds, – Tachycardia,
– alcoholism – hypertension
– Headache
Drug interactions
– Reversal of analgesia and return of pain
• ROH , antihistamines, anesthetics, CNS depressants, Sedatives, Important drugs
Phenothiazines – potentiation, additive depression and drowsiness, • Naloxone (Narcan)
coma – Therapeutic effects occur within 1-2 IV and 2-5 mins (IM/SC)
• Cimetidine – increased CNS toxicity, disorientation, confusion, depression minutes and last for 1-2 hours
and seizures. – Assess level of pain
Nursing Responsibilities – Resuscitation equipment ready
– Assess BP, RR, PR. Notify MD for HR above 120 bpm and BP
• Assess character of pain
over 140/90
• Obtain SBP – withold if RR below 12 and SBP belo 90 – Monitor for signs of withdrawal
• Admin before pain peaks
• Monotor for RD
• Turn to sides q two hours
• Monitor for hypotension – suppine position
• Fluids and fiber for constipation
• Anti-emetics for nausea and vomiting
• Monitory mental status- safety
• Palpate abdomen for retention
• PO – snacks to decrease GI irritation
• Health teachings
• Naloxone for morphine overdosage
• Institute after pain relief measures
Opiate Agonists-Antagonists
• Stimulates some receptors but antagonizes others
• Suppress CNS and alter patients perception and responses to pain
• Antagonistic effects reduces potential for narcotic abuse
• No antitussive effects
• Fewer gastrointestinal side effects
General uses: moderate to severe pain
Adverse :
• Similar to morphine
• Withdrawal symptoms in patients addicted to narcotics: anorexia, nausea,
vomiting, intestinal cramps, fever syncope or lightheadedness
• Pentazocine (Talwin) can cause life threatening effects when given as
injection to patients addicted to narcotics
Important Drugs
• Pentazocine – (Talwin)
o Moderate to severe pain
o Control pain during labor
o SE: more frequent- sedation, euphoria, N/V
o Less freq- dryness of mouth, headache, visual disturbance,
flushing, constipation, urinary frequency. Increased anxiety
o Adverse: tachycardia, skin rash, facial edema, hypertension,
respiratory difficulty
• Nalbuphine (Nubain)
o Analgesia equivalent to morphine
• Brupenorphine (Buprenex)
o 30x more potent than morphine but low potential for abuse
• Butorphanol (Stadol)
o 3-5x more potent than morphine
o Moderate to severe pain
o Adjunct to anesthesia
Nursing Responsibilities
• Mental status assessment – dizziness confusion
• Provide for safety. Avoid hazardous activities and those that need
mental concentration
• Assess for RD
• Stool softeners, laxatives, high fiber diet
• Do not discontinue abruptly
Opioid Antagonists
• Drugs that block the effect of agonists by competing for receptor sites
• Block objective and subjective effects of opioids
• Will precipitate withdrawal symptoms in patients physically dependent on
opiods
• Indicated for emergency treatment of opioid overdose
Uses:
– Diagnose opioid toxicity
– Reverse CNS and respiratory depression caused by narcotics
– Treat babies born to addicted mothers
Prec: contraindicated in clients addicted to narcotics
Adverse effects
– Withdrawal symptoms
– N/V
You might also like
- Passive Aggressive PersonalityDocument14 pagesPassive Aggressive PersonalityNikky Rossel Flores100% (2)
- Advanced Fast NutritionDocument24 pagesAdvanced Fast NutritionRich Galindo-Mela100% (5)
- English Workbook For SSC & BANK PODocument129 pagesEnglish Workbook For SSC & BANK PODevanand MishraNo ratings yet
- Top 200 Drug Study Reference RLPDocument31 pagesTop 200 Drug Study Reference RLPYathrika YathrikaNo ratings yet
- Dance History: Prepared By: Ferry Ann MontesDocument28 pagesDance History: Prepared By: Ferry Ann MontesNikky Rossel Flores100% (1)
- Amh Summary 2019 İn One FileDocument220 pagesAmh Summary 2019 İn One FileTatenda BrunoNo ratings yet
- Gout 131015051453 Phpapp01 PDFDocument26 pagesGout 131015051453 Phpapp01 PDFReny Rony BersaudaraNo ratings yet
- Employee Nda 353Document4 pagesEmployee Nda 353Rajiv SharmaNo ratings yet
- Adjuvants DrugsDocument38 pagesAdjuvants DrugsIppank F SjNo ratings yet
- Skateboarding: Design and Development Guidance For SkateboardingDocument52 pagesSkateboarding: Design and Development Guidance For SkateboardingAlejandro GaonaNo ratings yet
- SLMG6Q1W4-6 Filtration and SievingDocument15 pagesSLMG6Q1W4-6 Filtration and SievingSalve Serrano80% (5)
- PDF Installment Sales Reviewer Problems - CompressDocument43 pagesPDF Installment Sales Reviewer Problems - CompressMischievous Mae0% (1)
- (Women and Religion in The World) Sylvia Marcos (Editor) - Women and Indigenous Religions (Women and Religion in The World) - Praeger (2010) PDFDocument267 pages(Women and Religion in The World) Sylvia Marcos (Editor) - Women and Indigenous Religions (Women and Religion in The World) - Praeger (2010) PDFAnonymous QNu8I48100% (1)
- ReportDocument60 pagesReportNikky Rossel Flores100% (1)
- NDSAID Pan MangementDocument91 pagesNDSAID Pan MangementEslam EzzatNo ratings yet
- Therapeutics in Endo-2Document67 pagesTherapeutics in Endo-2mahmoudNo ratings yet
- Drug StudyDocument1 pageDrug Study049851No ratings yet
- Pain and Mobility Medication CardsDocument8 pagesPain and Mobility Medication CardsJamie O.No ratings yet
- Pharma Midterm CNS and ANS Drugs ReviewerDocument9 pagesPharma Midterm CNS and ANS Drugs ReviewerChesca LayosaNo ratings yet
- Mat Lecture Otc Meds2Document56 pagesMat Lecture Otc Meds2api-586369243No ratings yet
- Nsaid GuidelineDocument62 pagesNsaid GuidelineraffellaNo ratings yet
- MCH Unit5NonsteroidalantiinflammatoryagentsDocument40 pagesMCH Unit5Nonsteroidalantiinflammatoryagentsdottommohamedi.120411No ratings yet
- Analgesics: Non-Steroidal Anti-Inflammatory Drugs andDocument8 pagesAnalgesics: Non-Steroidal Anti-Inflammatory Drugs andWilliam C ChishaNo ratings yet
- Drug NameDocument31 pagesDrug Namelawha.chaand02No ratings yet
- IX. Drug StudyDocument4 pagesIX. Drug StudykingpinNo ratings yet
- Drug Ana Gin Amoxicillin DiclofenacDocument2 pagesDrug Ana Gin Amoxicillin DiclofenacmarohunkNo ratings yet
- Antacid Drug AnalysisDocument2 pagesAntacid Drug AnalysisJosef Angelo PoldoNo ratings yet
- Republic of The Philippines University Town, Northern SamarDocument2 pagesRepublic of The Philippines University Town, Northern SamarJosef Angelo PoldoNo ratings yet
- Antiinflammatory Antirheumatic Antigout DrugsDocument22 pagesAntiinflammatory Antirheumatic Antigout DrugsGracia Dela CruzNo ratings yet
- Local Media3752320764393916540Document22 pagesLocal Media3752320764393916540Hazea AwasNo ratings yet
- Non-Steroidal Anti-Inflammatory Drugs (Nsaids) : Dr. Nishant B. BhansaliDocument24 pagesNon-Steroidal Anti-Inflammatory Drugs (Nsaids) : Dr. Nishant B. Bhansaliankit ahirNo ratings yet
- Ferl Drug Study PDFDocument40 pagesFerl Drug Study PDFFERL KAILA SANTOSNo ratings yet
- NSAIDSDocument19 pagesNSAIDSDonna Kelly DuranNo ratings yet
- Rheumatology PADocument30 pagesRheumatology PAAlupoaie SilviuNo ratings yet
- Analgesic and Nsaids: Dr. Budhi Setiawan, M.Kes PharmacologyDocument25 pagesAnalgesic and Nsaids: Dr. Budhi Setiawan, M.Kes PharmacologyAyuNo ratings yet
- Endocrine DrugsDocument42 pagesEndocrine DrugsSolaNo ratings yet
- Pud Drug StudyDocument6 pagesPud Drug StudyLolcoma15 JaymsNo ratings yet
- Naproxen Drug StudyDocument4 pagesNaproxen Drug StudyTimz GatdulaNo ratings yet
- AnalgesicsDocument36 pagesAnalgesicsTakale BuloNo ratings yet
- Adjuvant AnalgesicDocument19 pagesAdjuvant AnalgesicKyra KhalidNo ratings yet
- M5 Lesson 2 - AnalgesicsDocument72 pagesM5 Lesson 2 - AnalgesicsClaire Marie AlvaranNo ratings yet
- RenalPalliativeCarefinal Mar 2011Document5 pagesRenalPalliativeCarefinal Mar 2011Nexi anessaNo ratings yet
- Pain MedicationsDocument2 pagesPain MedicationsimirelaNo ratings yet
- Nsaids: On Teroidal Nti Nflammatory RugDocument61 pagesNsaids: On Teroidal Nti Nflammatory RugNdayishimiye ErnestNo ratings yet
- 2020 Drugs On Pain (Analgesics) - DENTISTRYDocument28 pages2020 Drugs On Pain (Analgesics) - DENTISTRYVisayan Alliah GailNo ratings yet
- UntitledDocument4 pagesUntitledALYSSA MARIE MATANo ratings yet
- Unit 16 AnalgesicsDocument19 pagesUnit 16 AnalgesicsSante MunguyaNo ratings yet
- Anti-Inflammatory, Anti-Arthritis, and Related AgentsDocument22 pagesAnti-Inflammatory, Anti-Arthritis, and Related AgentsMarjolene PudaderaNo ratings yet
- IbuprofenDocument2 pagesIbuprofenAnreezahy GnoihcNo ratings yet
- Anti Inflammatory Analgesics Immunosuppresants Vaccines SeraDocument10 pagesAnti Inflammatory Analgesics Immunosuppresants Vaccines SeraShaira Dinamling BernabeNo ratings yet
- Antiamoebic Drugs & AnthelminthsDocument29 pagesAntiamoebic Drugs & Anthelminthsjeevan ghimireNo ratings yet
- Pain MedicationsDocument3 pagesPain Medicationsapi-3739910100% (1)
- Common Orofacial Pain Disorders - KN 3.24.18 IAEGDDocument99 pagesCommon Orofacial Pain Disorders - KN 3.24.18 IAEGDTayyuba AslamNo ratings yet
- AntipyreticsDocument14 pagesAntipyreticsRadianty Haengbog Daeng FrederichaNo ratings yet
- Jyane ReubenDocument35 pagesJyane ReubenAmr El-RefaeyNo ratings yet
- AcetazolamideDocument3 pagesAcetazolamideGwyn RosalesNo ratings yet
- Gout Presentation Group 2Document10 pagesGout Presentation Group 2Von Valentine MhuteNo ratings yet
- DRUG CelecoxibDocument2 pagesDRUG CelecoxibrholiboiNo ratings yet
- Analgesik: Chenny, Dr. Bagian Farmakologi Fakultas Kedokteran Universitas Wijaya Kusuma SurabayaDocument37 pagesAnalgesik: Chenny, Dr. Bagian Farmakologi Fakultas Kedokteran Universitas Wijaya Kusuma SurabayaWanda Puspita SariNo ratings yet
- Pain Medication (SALICYLATES ASPIRIN)Document2 pagesPain Medication (SALICYLATES ASPIRIN)KyrrielJimenoCeladaNo ratings yet
- Non Steroid Antiinflammatory Drugs & Drugs Use in The Treatment of GoutDocument28 pagesNon Steroid Antiinflammatory Drugs & Drugs Use in The Treatment of GoutVevi VarcetyNo ratings yet
- Pharmacotherapy 1 GIS Self CarepdfDocument40 pagesPharmacotherapy 1 GIS Self Carepdfelifuygur09No ratings yet
- Drug Study FormatDocument3 pagesDrug Study FormatMeryl MarcosNo ratings yet
- Antiinflammation DrugsDocument64 pagesAntiinflammation DrugsSusy MariyatiNo ratings yet
- SUMMARY Drugs Used Primarily For Gastrointestinal ConditionsDocument3 pagesSUMMARY Drugs Used Primarily For Gastrointestinal ConditionsXylex Dave AndresNo ratings yet
- 7endocrine DrugsDocument2 pages7endocrine DrugsSOFIA ALYSSA MARIE ABUDENo ratings yet
- Gastroesophageal Reflux Disease (GERD) : Types of HeartburnDocument12 pagesGastroesophageal Reflux Disease (GERD) : Types of HeartburnSara Al-FerkhNo ratings yet
- Laranang, Mica Joy R. Drug Study: BSN 123 Group 90Document5 pagesLaranang, Mica Joy R. Drug Study: BSN 123 Group 90Gerard Louise Esmao RNNo ratings yet
- Family Lifeline Hospice Group ADocument4 pagesFamily Lifeline Hospice Group ANikky Rossel FloresNo ratings yet
- Pathophysiology of Colon CancerDocument1 pagePathophysiology of Colon CancerNikky Rossel FloresNo ratings yet
- Health Assessment ChristianDocument23 pagesHealth Assessment ChristianNikky Rossel FloresNo ratings yet
- Problem in OxygenationDocument11 pagesProblem in OxygenationNikky Rossel FloresNo ratings yet
- Sensory Deficits in The Elderly: Their Implications and ManagementDocument41 pagesSensory Deficits in The Elderly: Their Implications and ManagementNikky Rossel FloresNo ratings yet
- Web Causation of MalnutritionDocument1 pageWeb Causation of MalnutritionNikky Rossel FloresNo ratings yet
- Unit II-D (Nursing Interventions On Mental Health)Document68 pagesUnit II-D (Nursing Interventions On Mental Health)Nikky Rossel FloresNo ratings yet
- Ernestine WiedenbachDocument22 pagesErnestine WiedenbachNikky Rossel FloresNo ratings yet
- Dance Steps, Step Patterns, Time Signature and Counting: Prepared By: Karl Jacon Ferolino Judy Ann UyDocument25 pagesDance Steps, Step Patterns, Time Signature and Counting: Prepared By: Karl Jacon Ferolino Judy Ann UyNikky Rossel FloresNo ratings yet
- The Psychosocial Aspects OF Aging: A. Normal Changes in The Older PersonsDocument17 pagesThe Psychosocial Aspects OF Aging: A. Normal Changes in The Older PersonsNikky Rossel FloresNo ratings yet
- Likes and Dislikes: Late AdulthoodDocument4 pagesLikes and Dislikes: Late AdulthoodNikky Rossel FloresNo ratings yet
- Chitoran Et AlDocument5 pagesChitoran Et AlCristina TomaNo ratings yet
- Chasing Atlas DragonsDocument9 pagesChasing Atlas DragonsCarles JiménezNo ratings yet
- Assigment BBM Finacial AccountingDocument6 pagesAssigment BBM Finacial Accountingtripathi_indramani5185No ratings yet
- BANK OF COMMERCE and STEPHEN Z. TAALA vs. SPOUSES ANDRES and ELIZA FLORESDocument6 pagesBANK OF COMMERCE and STEPHEN Z. TAALA vs. SPOUSES ANDRES and ELIZA FLORESKatherine OlidanNo ratings yet
- Gato BarbieriDocument1 pageGato Barbierireihuno0% (1)
- RismaAnisa-Tabel Pilihan Jurnal Timeline Final Progress Per MingguDocument22 pagesRismaAnisa-Tabel Pilihan Jurnal Timeline Final Progress Per MingguRisma AnisaNo ratings yet
- The Purpose and Goals of A Call Center Audit Colin TaylorDocument102 pagesThe Purpose and Goals of A Call Center Audit Colin TaylorMarius AngaraNo ratings yet
- The Influence of Brand Recognition On Retail Store ImageDocument15 pagesThe Influence of Brand Recognition On Retail Store ImageCiobanu MarianNo ratings yet
- Area A ProprofsDocument10 pagesArea A ProprofsClyde Micole FelipeNo ratings yet
- Bai Tap Tieng Anh Lop 7 Unit 3 Community ServiceDocument6 pagesBai Tap Tieng Anh Lop 7 Unit 3 Community ServiceHưng NguyễnNo ratings yet
- MT 107 General Direct Debit MessageDocument33 pagesMT 107 General Direct Debit MessageVladimirNo ratings yet
- A Final Project Report On Customer Loyalty Study of Hero Honda BikeDocument10 pagesA Final Project Report On Customer Loyalty Study of Hero Honda Bikejoshirohit100% (5)
- Good Fences Make Good Neighbors: Background For TeachersDocument4 pagesGood Fences Make Good Neighbors: Background For TeachersMuhammad Furqan Aslam AwanNo ratings yet
- Uji Lab Hazmat TIGER HEAD (QUALIS) PDFDocument5 pagesUji Lab Hazmat TIGER HEAD (QUALIS) PDFMHUA GroupNo ratings yet
- Memo On Equal Access Act and First AmendmentDocument13 pagesMemo On Equal Access Act and First AmendmentStudentsforlifeHQNo ratings yet
- Bland-Altman Plot and AnalysisDocument25 pagesBland-Altman Plot and AnalysisRachmi FadillahNo ratings yet
- Science 6 - Q3Document4 pagesScience 6 - Q3CHRISTINE ROSE ESPIRITUNo ratings yet
- SupplierDocument18 pagesSupplierFaisal KhanNo ratings yet
- GovernorDocument9 pagesGovernorAqsa Riaz SoomroNo ratings yet
- Latihan Mid Semester 1 B Ing Kelas 8Document5 pagesLatihan Mid Semester 1 B Ing Kelas 8ipung miranti sariNo ratings yet
- Idx Monthly StatsticsDocument113 pagesIdx Monthly StatsticsemmaryanaNo ratings yet
- User Exit Real Time Business Example SAP - Enhancements in SAP - SapnutsDocument6 pagesUser Exit Real Time Business Example SAP - Enhancements in SAP - SapnutsDeepakNo ratings yet
- Basic Education Curriculum 3Document241 pagesBasic Education Curriculum 3MICHELLE DE LOS REYESNo ratings yet