Professional Documents
Culture Documents
Principles For All Medication
Uploaded by
Belle Makinano0 ratings0% found this document useful (0 votes)
43 views6 pagespppp
Original Title
Pharmacology Notes
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpppp
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
43 views6 pagesPrinciples For All Medication
Uploaded by
Belle Makinanopppp
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 6
PRINCIPLES FOR ALL MEDICATION 3rd: Check bed tag (this is least reliable method
14. Provide privacy if needed.
1. Verify all new or questionable orders. 15. Inform client of medication, any procedure, technique, purposes,
2. Prepare medications in a quiet environment. and client teaching as applicable.
3. Perform hand hygiene. Observe standard precautions as 16. Stay with the client until medication is taken. Do not leave
appropriate. medication at bedside.
4. Collect all necessary equipment including straws, juice, water or 17. Give the medication within 30mins of prescribed time.
stethoscope. 18. Assist client if needed and leave in a comfortable position.
5. Review the medication administration record carefully to ensure 19. Chart administration immediately in ink, marking your initials in
safety, note: the appropriate space.
Medication dosage 20. Document the rationale if the drug is not administered.
Route 21. Report any errors immediately and complete appropriate
Expiration date institutional document.
Frequency 22. Liquid medications (all routes of administration) MUST NOT be
6. Research drug incompatibilities, action, purpose, mixed together unless of compatibility is verified.
contraindications, side effects and appropriate routes. 23. Prepare drugs for administration in a quiet, well-lit area.
7. Calculate the dosage accurately. Confirm normal range of dose, 24. Never remove a drug from an unlabeled container or from a
particularly in pediatrics. container whose label is illegible.
8. Check expiration date. Look for changes that indicate for 25. Do not let hands touch capsules or tablets.
decomposition (color, odor, clarity) 26. Always observe aseptic technique when handling syringes and
9. Compare label three times with the medication to decrease risk needles.
for error: 27. Be alert for drugs with similar names.
1st: When removing package from the drawer. 28. Replace the caps of drug containers immediately after the drug is
2nd: Before preparing the medication removed.
3rd: After preparing medication 29. Return drugs requiring special storage to the storage area
10. Check need for pm medications. immediately after they are prepared for administration.
11. Be sure medications are identified for each client. 30. Evaluate patient’s response to the drug. Document both negative
12. Check for any allergies and perform all special assessment before and positive reactions.
administration 31. Observe the ten rights in drug administration.
13. Confirm identity by checking at least two of the three possible 32. To ensure safety, do not give a medication that someone else
mechanism for identification. prepared.
1st: Ask client his name 33. When using a unit dose system:
2nd: Check client’s identity-band
Do not remove the wrappings of the unit dose until the Iron – have client use straw to prevent staining of the
drug reaches the bedside of the patient who is to receive teeth.
it. 8. Use gloves if you place your finger in client’s mouth.
After administering the drug, the nurse charts
immediately on the unit dose drug form. Special Concerns
1. Use a calibrated dropper, or syringe to give medications to infant.
Keep infant at 45 degree angle.
1. Special assessment: diet status, level of knowledge, oral cavity See if medication is available in liquid form if child is
and ability to swallow. unable to swallow.
2. Use mortar and pestle to crush tablets, if appropriate. Be sure not to use child’s favorite food as this may result
Enteric coated tables should not be crushed. Only scored in distrust.
tablets can be broken. 2. For rectal suppository
3. Capsule content may be mixed with food, except time-release Insert suppository, tapered end first (approximately 2
capsules. inches)
4. Give medication with 60-100 ml of water or juice, unless Hold buttocks together
contraindicated (e.g. cough syrup) Encourage to retain suppository for 15-20 minutes to
5. Preparation of liquid medications: allow suppository to melt.
Shake to mix.
Pour away from bottle label Administration of Nasal Medication
Read liquid amount at meniscus (eye level) 1. Have client blow nose to clear mucus
Do not administer alcohol-based products (e.g elixirs) to 2. Position client so that head can be tilted back to aid a
alcohol-dependent persons gravitational flow
6. Sit client upright to ensure swallowing 3. Push up on tip of nostril
7. Have client swallow medication except: 4. Place dropper or atomizer angled slightly upward just inside
Sublingual route – DO NOT swallow fluid for 30mins nostril (careful not to touch nose with applicator)
following administration 5. Remind client to keep head tilted for 5mins.
SL; from the Latin for “under the 6. Inform that drops may produce an unpleasant taste.
tongue” by which substances 7. Instruct just to wipe nose not blow
diffuse into the blood through 8. If client aspirates and begins to cough, let the client sit upright.
tissues under the tongue. 9. If client is an infant, lay infant on his/her back.
Buccal route – medication between cheek and gum. No
fluid after administration.
Administration of Ophthalmic Solution 2. Cleanse area of old medication using gauze pads with soap and
warm water.
1. Check solution for color and clarity 3. Use gloves and gauze, tongue depressors or sterile applicator if
2. Warm solution in hands before administration integument is broken.
3. Have client lie on back or sit with head turn to affected side. 4. Spread medication over the site evenly and thinly
4. Cleanse eyelid and eyelashes with sterile gauze pad soaked with 5. If necessary, cover area loosely with a dressing
physiologic saline.
5. Have client look up Special Concerns
6. Keep eye open by gently pulling down the skin below the eye to
expose the lower conjunctival sac. 1. When applying nitroglycerin ointment, take client’s blood
7. Place drops into lower conjunctiva near outer canthus (less pressure 5 minutes before and after application
sensitive than cornea) 2. Wash hands after applications to prevent self-absorption
8. If using ointment, squeeze into lower conjunctiva (from inner to 3. When using transdermal patches, use glove to avoid inadvertent
outer canthus) drug absorption. Place patch in area with little hair.
Let client blink 2-3 times.
Parenteral Route
Ophthalmic medications are for individual clients only.
Angles for inserting injections:
Administration of Otic Medications
a. Intramuscular – 90 degrees
1. Warm medication in hands before administering. b. Subcutaneous – 45 degrees
2. Have client slightly tilt head at unaffected side to aid gravitational c. Intravenous – 25 degrees
flow
d. Intradermal – 10-15 degrees
3. Clean outer ear using a wet gauze pad
4. Straighten ear canal by pulling pinna Subcutaneous Route
Up and back for adults
Down and back for infants and children under 3 years old 1. Use size 25-27 G, ½ - 1 inch needle, maximum volume is 1.5
5. Maintain position of ear for 5-10 minutes until medication has ml
totally reached inner ear. 2. Pinch skin to form SC fold
3. Insert needle at 45 degree angle in thigh or arm (to avoid
Administration of Topical Agents entering muscle)
4. 90 degree angle in the abdomen
1. Provide privacy and expose only appropriate area to provide
comfort
Possible sites: d. Deltoid – only for small volumes (0.5 – 1ml); use for
immunizations in toddles, older children and adults but NOT for
a. Lateral aspects of upper arm infants; check site carefully, axillary nerve lies beneath deltoid
b. Anterior thigh muscle
c. Abdomen: 2 inches away from umbilicus e. Dorsogluteal – not preferred due to proximity to sciatic nerve
d. Back, in scapular area
Z-track Technique
Intradermal Route
1. For irritating solutions; needle size 20-22 G
1. Use size 26-27 G 1-inch needle on a 1 ml or tuberculin syringe 2. Pull away skin away from the site laterally with non-dominant
(volume will be approximately 0.1 ml) hand to ensure medication enters muscle
2. Stretch skin taut 3. Wait 10 seconds after injecting medication before withdrawing
3. Insert needle 10-15 degrees angle needle
4. Release skin; do not massage (seals needle track)
Possible sites:
5. Encourage physical activity
a. Ventral mid-forearm
Possible sites:
b. Scapula
c. Upper chest a. Gluteus medius: Best but may use other sites except deltoid.
When wheal appears, remove the needle, and do not
massage it
Intramuscular Route
1. Needle size 18-23 G, 1-2 inches needle; maximum volume is 5ml.
Sites for IM injections:
a. Ventrogluteal – anterior-superior iliac spine, iliac crest, greater
trochanter of the femur
b. Vastus Lateralis – preferred site for immunization of infants.
Muscle is well developed and not located near major nerves or
blood vessels.
c. Rectus Femoris (medial thigh) – a handbreath above knee and
below greater trochanter; good site for infants and self-injection
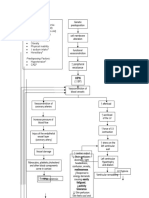
PHASES OF DRUG ACTIVITY To decrease the effects of the stomach’s acid barrier, and the
direct effects of certain foods, ORAL drugs ideally should be given
Dose Disintergration of dose from dissolution of drug 1 hour before or 2 hours after a meal.
(Pharmaceutical Phase)
Drug Absorption of Various Dosage Forms
Oral Preparations: (fastest to slowest)
Absorption, Distribution, Metabolism, Elimination (Pharmacokinetic Phase)
a. Liquid, elixirs, syrups f. coated tablets
b. Suspension solutions g. enteric - coated
c. Powders
Drug receptor interaction (Pharmacodynamic Phase)
d. Capsules
e. Tablets
Effect Bioavailability
Pharmaceutics A term used to express the extent of drug absorption
Refers to the percentage of the administered drug that reaches
The study of how various drugs form influence pharmacokinetic the systemic circulation and eventually its site of action
and pharmacodynamic activities Significance: differences in bioavailability leads to variable drug
Pharmaceutic phase or dissolution refers to the reduction of drugs responses
in slid form into smaller particles and their dissolution into a liquid Dangers of Drugs with a Narrow Therapeutic Range: a relatively
to facilitate absorption. small change in the drug level in those type of drugs can produce
After ingestion, solid drug (tablet or capsule) must first a significant change in the response.
disintegrate into smaller particles A small decline in drug level = Therapeutic failure; A small
Smaller particles are dissolved into liquid, ready for absorption in increase in drug level = Toxicity
the gastrointestinal tract
Bioequivalent
Always remember that…
If two medications have the same bioavailability and the same
Drugs in liquid form are more rapidly available for GIT absorption concentration of active ingredient.
than solids. Examples: Paracetamol & Biogesic
Food in the GIT may interfere pharmaceutics Furosemide & Lasix
Milk, alcohol, and protein speed up the breakdown of many drugs Captopril & Capoten
Others may chemically bind drugs or block their absorption.
Factors Influencing Drug Effects
a. Weight:
Recommended dosage of a drug is based on drug evaluation
studies:
Targeted at a 150 pound person
Doses are adjusted by patient’s weight
Toxic effects may occur at the recommended dosage if
the person is very small
b. Age
Children have immature systems for handling drugs
Older adults undergo many physical changes that are part
of aging process
Bodies may respond differently in all aspects of
pharmacokinetics
Pediatric Dosages
Fried’s Rule:
Infant’s dose (<1 year) = infant’s age (in months)
150 months x average adult dose
Young’s Rule:
Child’s dose (1-12 years) = child’s age (in years)
Child’s age (in years) + 12 x average adult dose
You might also like
- Basic Pharmacology HandoutsDocument16 pagesBasic Pharmacology HandoutsRS BuenavistaNo ratings yet
- InsulinsDocument1 pageInsulinsReymart Waitforit DulayNo ratings yet
- Intermediate Math For Nurses NAME - WorkbookDocument7 pagesIntermediate Math For Nurses NAME - WorkbookRaniela MaeNo ratings yet
- Pharma NotesDocument8 pagesPharma NotesKylahNo ratings yet
- Vital Sign Na (1) by ZWBDocument52 pagesVital Sign Na (1) by ZWBAshraf Ali100% (1)
- Pharm Exam Ii NotesDocument24 pagesPharm Exam Ii Noteskatiana louisNo ratings yet
- Med Admin Practice QuestionsDocument5 pagesMed Admin Practice QuestionsArmelle DelvaNo ratings yet
- Clinical Parasitology OutlineDocument5 pagesClinical Parasitology OutlineLynneth Mae Beranda CorpusNo ratings yet
- Poison & Antidote Chart IWK Regional Poison Cen PDFDocument1 pagePoison & Antidote Chart IWK Regional Poison Cen PDFdeeptiNo ratings yet
- Pharm ReviewDocument5 pagesPharm ReviewChelsea ChanceNo ratings yet
- Vital Signs: Aurora Roslin Samosa, Man RNDocument57 pagesVital Signs: Aurora Roslin Samosa, Man RNAlexander DontonNo ratings yet
- Mechanisms of Drug Interactions: A. AbsorptionDocument4 pagesMechanisms of Drug Interactions: A. AbsorptionAnne Geleen BraganzaNo ratings yet
- Diabetes Management ATIDocument15 pagesDiabetes Management ATIJessica ChirinoNo ratings yet
- Female Reproductive SystemDocument7 pagesFemale Reproductive SystemyannieNo ratings yet
- Gestational DiabetesDocument51 pagesGestational Diabeteskhadzx100% (2)
- Hytension For 16 Years Men (64 Years Old) Cigarette Smoking (32 Pack Years) Alcoholic Drinker For 32 Years Fond of Eating Fatty Foods Physical Inability Sodium Intake HereditaryDocument3 pagesHytension For 16 Years Men (64 Years Old) Cigarette Smoking (32 Pack Years) Alcoholic Drinker For 32 Years Fond of Eating Fatty Foods Physical Inability Sodium Intake HereditaryJohn Paulo CatacutanNo ratings yet
- Anatomy: Blood Is A Specialized Bodily Fluid in Animals That Delivers Necessary Substances SuchDocument5 pagesAnatomy: Blood Is A Specialized Bodily Fluid in Animals That Delivers Necessary Substances Suchjeoffrey_castroNo ratings yet
- PharmaDocument12 pagesPharmaPamela Reinn SulpaNo ratings yet
- Concept Map Diagnosis and InterventionsDocument3 pagesConcept Map Diagnosis and Interventionsmenickel3No ratings yet
- Reproductive SystemDocument6 pagesReproductive SystemDara BMNo ratings yet
- Pharmacology by DoctorDocument3 pagesPharmacology by DoctorLae DujonNo ratings yet
- Ection I. The Female Reproductive System 1-1. GENERALDocument9 pagesEction I. The Female Reproductive System 1-1. GENERALNheil_Christop_4211No ratings yet
- Anaphysio of The HeartDocument6 pagesAnaphysio of The HeartChamCham AquinoNo ratings yet
- Foundations of Pharmacology NotesDocument5 pagesFoundations of Pharmacology NotesSheril MarekNo ratings yet
- The Cardiovascular SystemDocument5 pagesThe Cardiovascular Systemjuly3ciaNo ratings yet
- Case Study Cerebrovascular Accident TRIXIEDocument10 pagesCase Study Cerebrovascular Accident TRIXIETrixie Marie Shebel AbdullaNo ratings yet
- PharmacologyDocument9 pagesPharmacologyRPh Krishna Chandra JagritNo ratings yet
- Pathophysiology CHFDocument3 pagesPathophysiology CHFKit LaraNo ratings yet
- Insulin ChartDocument1 pageInsulin ChartGabriel TaylorNo ratings yet
- Drug Calculation WorksheetDocument3 pagesDrug Calculation WorksheetUmaru DomaNo ratings yet
- Nasal Cavity. The Nasal Cavity, Also Known As TheDocument11 pagesNasal Cavity. The Nasal Cavity, Also Known As TheWilly Chandra HermawanNo ratings yet
- Chapter 1 - The Nursing Process and Drug TherapyDocument3 pagesChapter 1 - The Nursing Process and Drug TherapyHaleyNo ratings yet
- Chapter 45-Antiarrhythmic AgentsDocument13 pagesChapter 45-Antiarrhythmic AgentsMelanie RodriguezNo ratings yet
- Notes Human EyeDocument9 pagesNotes Human EyeGeetanshi OberoiNo ratings yet
- Nasal CavityDocument4 pagesNasal Cavitykep1313No ratings yet
- Inorganic Compounds and SolutionsDocument22 pagesInorganic Compounds and SolutionsSophia RoseNo ratings yet
- Head and NeckkkkkkDocument7 pagesHead and NeckkkkkkJoey A. RumbaoaNo ratings yet
- CPR of NewbornDocument6 pagesCPR of NewbornChandu RajNo ratings yet
- Physiology NotesDocument4 pagesPhysiology NotesGizem OsmanogluNo ratings yet
- Introduction To PharmacologyDocument119 pagesIntroduction To PharmacologyYzel Vasquez AdavanNo ratings yet
- Antidotes To Commn MedicationDocument1 pageAntidotes To Commn Medicationjosephabram051590No ratings yet
- Dialyzable MedsDocument2 pagesDialyzable MedsMerry Janne RebolesNo ratings yet
- DrugmedsDocument52 pagesDrugmedsshirleyNo ratings yet
- Neonatal Resuscitation: BY DR Babatunde O.TDocument20 pagesNeonatal Resuscitation: BY DR Babatunde O.Tijojo elizabethNo ratings yet
- Sources Hormone FunctionDocument2 pagesSources Hormone FunctionKatherine Joy MaderajeNo ratings yet
- Chapter 10 Endocrine SystemDocument8 pagesChapter 10 Endocrine SystemCriscia Lene OlatNo ratings yet
- Physiology of ThyroidDocument9 pagesPhysiology of ThyroidAbby EvangelistaNo ratings yet
- Anatomy of The Female Reproductive SystemDocument9 pagesAnatomy of The Female Reproductive SystemPinkeyinthecityNo ratings yet
- Chapter25 Urinary SystemDocument9 pagesChapter25 Urinary Systemkikajet23No ratings yet
- Endocrine SystemDocument21 pagesEndocrine SystemMark DimarucutNo ratings yet
- BiologyDocument30 pagesBiologyChristel Ramos100% (1)
- Pharmacology Notes #1 DRUG ACTIONDocument4 pagesPharmacology Notes #1 DRUG ACTIONAyumi StarNo ratings yet
- 21 - Peripheral Nervous SystemDocument16 pages21 - Peripheral Nervous Systembhavikrao7605No ratings yet
- Mantoux Test: Pirquet Test, or PPD Test For Purified Protein Derivative) Is A Diagnostic Tool ForDocument5 pagesMantoux Test: Pirquet Test, or PPD Test For Purified Protein Derivative) Is A Diagnostic Tool ForGurmeet SinghNo ratings yet
- Pharmacology Notes CH 1 IntroductionDocument4 pagesPharmacology Notes CH 1 Introductionridley45No ratings yet
- Impulses Which Are Rapid and Specific and CauseDocument9 pagesImpulses Which Are Rapid and Specific and CauseCellina De LeonNo ratings yet
- Anatomy of The Urinary SystemDocument24 pagesAnatomy of The Urinary Systemgaylmm100% (2)
- Medication Calculation - Docx..... BDocument14 pagesMedication Calculation - Docx..... BKaren Ruste Villaluna-AbulenciaNo ratings yet
- Oral MedicationDocument8 pagesOral Medicationrea bentayaoNo ratings yet
- Medication AdministrationDocument26 pagesMedication AdministrationTuTit100% (2)
- Drug Study AmbroxolDocument2 pagesDrug Study AmbroxolBelle MakinanoNo ratings yet
- Care of Patients With Asthma: Peak Flow MonitoringDocument2 pagesCare of Patients With Asthma: Peak Flow MonitoringBelle MakinanoNo ratings yet
- Care of Women and Families During PostpartumDocument3 pagesCare of Women and Families During PostpartumBelle MakinanoNo ratings yet
- Homeostatic Imbalances in The SkinDocument1 pageHomeostatic Imbalances in The SkinBelle MakinanoNo ratings yet
- Cardiovascular Drugs: D. Hormone DeliveryDocument8 pagesCardiovascular Drugs: D. Hormone DeliveryBelle MakinanoNo ratings yet
- A. Osteoarthritis: UnderstandingDocument4 pagesA. Osteoarthritis: UnderstandingBelle MakinanoNo ratings yet
- Common Drugs in The Labor Room and Delivery RoomDocument4 pagesCommon Drugs in The Labor Room and Delivery RoomBelle MakinanoNo ratings yet
- Continuation Sa PregnancyDocument3 pagesContinuation Sa PregnancyBelle MakinanoNo ratings yet
- Concept of Family & Family Nursing ProcessDocument3 pagesConcept of Family & Family Nursing ProcessBelle MakinanoNo ratings yet
- Human Capital ManagementDocument16 pagesHuman Capital ManagementDavid Mason100% (1)
- Lesson 1 INTRO Research WritingDocument4 pagesLesson 1 INTRO Research WritingMary Joyce GaliguerNo ratings yet
- QueuingDocument32 pagesQueuingSasana SanNo ratings yet
- Assessment Method 3 - Project: Instructions For StudentsDocument5 pagesAssessment Method 3 - Project: Instructions For StudentsJyoti Verma0% (2)
- Acknowledgement: The Influence of Family Dynamics and Social Conditions On Human DevelopmentDocument8 pagesAcknowledgement: The Influence of Family Dynamics and Social Conditions On Human DevelopmentRhea ChawlaNo ratings yet
- Chapter 14 Flash Profile MethodDocument21 pagesChapter 14 Flash Profile MethodTiến ThànhNo ratings yet
- Thesis SampleDocument22 pagesThesis SamplePatrick Vinuya100% (2)
- 11 Economics-Collection of Data-Notes and Video LinkDocument11 pages11 Economics-Collection of Data-Notes and Video Link2R CLASSESNo ratings yet
- The LAMP FrameworkDocument13 pagesThe LAMP FrameworkGrace RuthNo ratings yet
- Weekly Schedule of MBA 2016 SIIIA Week 1Document12 pagesWeekly Schedule of MBA 2016 SIIIA Week 1aadinNo ratings yet
- 1751 PDFDocument221 pages1751 PDFParag SharmaNo ratings yet
- Unit 5aDocument22 pagesUnit 5akanu_cNo ratings yet
- Rizal 203 BeedDocument14 pagesRizal 203 BeedJhonny Dela CruzNo ratings yet
- Effects of Technology in The Level of PeDocument41 pagesEffects of Technology in The Level of PeGabriel Cortez MercadoNo ratings yet
- Cause and Effect of AbsenteeismDocument17 pagesCause and Effect of Absenteeismlizechvria67% (3)
- Csir Net Exam 2024Document3 pagesCsir Net Exam 2024as1655647No ratings yet
- Choosing The Denture Occlusion - A Systematic ReviewDocument6 pagesChoosing The Denture Occlusion - A Systematic ReviewshraddhaNo ratings yet
- Management Information System: - by Group IDocument15 pagesManagement Information System: - by Group Iashwinishanbhag1987No ratings yet
- When Should Uniform Conditioning Be Applied PDFDocument10 pagesWhen Should Uniform Conditioning Be Applied PDFChrisCusackNo ratings yet
- Instant Download Ebook PDF Doing Research With Children A Practical Guide 3rd Edition PDF ScribdDocument41 pagesInstant Download Ebook PDF Doing Research With Children A Practical Guide 3rd Edition PDF Scribdemiko.johnson659100% (50)
- 2013 Book BayesianAndFrequentistRegressi PDFDocument700 pages2013 Book BayesianAndFrequentistRegressi PDFlore002No ratings yet
- Inua Jamii Senior Citizens' Scheme: Main Lessons LearnedDocument6 pagesInua Jamii Senior Citizens' Scheme: Main Lessons LearnedreaganNo ratings yet
- Internet Addiction and Associated Factors Among UndergraduatesDocument8 pagesInternet Addiction and Associated Factors Among UndergraduatesAdam ZiyyadNo ratings yet
- Prison Thesis 1Document25 pagesPrison Thesis 1Joseph Nathaniel MarmolNo ratings yet
- Assignment 2 (Marketing)Document18 pagesAssignment 2 (Marketing)MikealayNo ratings yet
- Barkley Deficits in Executive Functioning Scale (BDEFS) Validation in A Large Multisite College SampleDocument23 pagesBarkley Deficits in Executive Functioning Scale (BDEFS) Validation in A Large Multisite College Samples0919012心理系碩士No ratings yet
- United States House of Representatives Committee On Science, Space, and TechnologyDocument21 pagesUnited States House of Representatives Committee On Science, Space, and TechnologyChaoticEmoNo ratings yet
- Headquarters-Subsidiary Relationships in MNCS: Fifty Years of Evolving ResearchDocument9 pagesHeadquarters-Subsidiary Relationships in MNCS: Fifty Years of Evolving ResearchAssal NassabNo ratings yet
- Apa Style Research Paper Outline TemplateDocument6 pagesApa Style Research Paper Outline Templateyscgudvnd100% (1)
- Applied Math Unit1 Summary and Useful FormulasDocument4 pagesApplied Math Unit1 Summary and Useful FormulasEquitable BrownNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)