Professional Documents
Culture Documents
Effects of Aromatherapy On Sleep Quality and Anxiety of Patients
Uploaded by
fraldyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effects of Aromatherapy On Sleep Quality and Anxiety of Patients
Uploaded by
fraldyCopyright:
Available Formats
RESEARCH
doi: 10.1111/nicc.12198
Effects of aromatherapy on sleep
quality and anxiety of patients
Ezgi Karadag, Sevgin Samancioglu, Dilek Ozden and Ercan Bakir
ABSTRACT
Background: In intensive care units (ICUs), patients cannot sleep well. Aromatherapy is used for depression, anxiety, relaxation and disorders
related with sleep and stress.
Aim: This study aimed to investigate the effect of lavender essential oil on the sleep quality and anxiety level of patients in coronary ICU.
Participants: A total of 60 patients in coronary ICU participated in this study.
Design: A randomized controlled study was conducted with 60 patients in a province located in the southeast of Turkey.
Methods: After informing the patients in both groups about the study, they were administered a questionnaire, Pittsburgh Sleep Quality Index
(PSQI) and the Beck Anxiety Inventory (BAI) scale. The patients in the intervention group were given 2% lavender essential oil via inhalation for
15 days after which they were administered the same scales again to evaluate the sleep quality and anxiety. As for the control group, they were
administered the same scales again after 15 days without the inhalation of lavender essential oil.
Results: Comparison of the PSQI and BAI scores of the patients in the control and intervention groups before and after the intervention
showed statistically significant differences in the change in favour of the intervention group (p < 0⋅05).
Conclusion: Lavender essential oil increased quality of sleep and reduced level of anxiety in patients with coronary artery disease.
Relevance to clinical practice: As a non-invasive, cheap, easily applicable, cost-effective, independent nursing intervention and
appropriate for cardiac patients, lavender essential oil could be applied in ICUs.
Key words: Anxiety • Coronary artery disease • Lavender oil • Nursing • Sleep quality
BACKGROUND lives because of cardiovascular diseases (WHO, 2015).
Coronary artery disease (CAD) is the most common This figure is expected to rise up to 25 million in the
cardiovascular system disease (World Health Organi- year 2020. Not only worldwide, but CAD also draws
zation (WHO), 2015). Because of its high mortality attention in Turkey as a major cause of mortality and
and morbidity rate, prevalence in the productive age morbidity with increasing prevalence. It is estimated
group, highs costs of treatment and potential to cause that there are 2 million patients with CAD in Turkey
severe complications, it is a major public health prob- and 160 000 people die because of CAD (Turkish Soci-
lem (Badır and Demir Korkmaz, 2010). ety of Cardiology (TSC), 2013; İnangil and Şendir,
According to WHO reports, coronary heart diseases 2014). According to the latest statistical data, CAD mor-
have the highest mortality rates. Among the clinical tality rate has been determined to be 7⋅5 per thou-
symptoms of CAD are angina pectoris, which is caused sand for men and 3⋅7 per thousand for women in the
by an atherosclerotic process affecting the arteries feed- 45–74 years age group (Onat et al., 2014).
ing the heart, acute myocardial infarction and sud- Sleep, which is one of the vital necessities, is crucial
den death. Every year, 16⋅7 million people lose their in sustaining the physiological and psychological
welfare of individuals (Akça Ay, 2012). Patients hos-
pitalized in intensive care units, especially those in
Authors: E Karadag, PhD, RN, Assistant Professor, Faculty of Nursing, coronary intensive care units, frequently experience
Dokuz Eylül University, Turkey; S Samancioglu, PhD, RN, Assistant
sleep disorders for many reasons such as pain, physical
Professor, Health Science Faculty, Gaziantep University, Gaziantep, Turkey;
D Ozden, PhD, RN, Associate Professor, Faculty of Nursing, Dokuz Eylül condition, medication, fear of death, light, environ-
University, Izmir, Turkey; E Bakir, MSc, RN, Nurse, Gaziantep University mental noise, unpleasant odours, foreign instruments,
Medical Hospital, Gaziantep, Turkey nursing interventions, invasive procedures, complica-
Address for correspondence: E Karadag, Assistant Professor, tions of disease, loss of privacy and staying away from
Department of Oncology Nursing, Faculty of Nursing, Dokuz Eylül
University, 35340 İnciraltı/İzmir, Turkey
family (Dedeli and Durmaz Akyol, 2008; Wenham and
E-mail: ezgikaradag44@gmail.com Pittard, 2009; Kurt and Enç, 2013; Hajibagheri et al.,
2014). Research has shown that the sleep quality and
© 2015 British Association of Critical Care Nurses 1
Effects of aromatherapy on sleep quality and anxiety of patients
duration of patients hospitalized in intensive care units et al., 2014). Studies on the benefits of lavender’s aroma
are inversely related (Mui So and Chan, 2004; Tunçay showed that linalool and linalyl acetate present in this
and Uçar, 2010). As these patients stay awake for a sig- plant can stimulate parasympathetic system. In addi-
nificant amount of time, they cannot benefit from the tion, linalyl acetate has narcotic effects and linalool
therapeutic effects of sleep. Inadequate and unsatisfac- acts as a sedative. This herb improves the heart func-
tory sleep precludes healing by having negative effects tion and as a circulatory stimulant, it has beneficial
on the immune system, wound healing process and effects on coronary blood flow (Fayazi et al., 2011;
cognitive functions of individuals as well as increasing Bikmoradi et al., 2014).
their level of stress and anxiety (Mui So and Chan, Essential oils from plants are used with three
2004; Kurt and Enç, 2013; Lytle et al., 2014). The anx- methods; via inhalation, massage and orally. In the
iety level of patients who experience sleep disorders study conducted by Gedney et al. (2004), five drops
increases, or patients suffer from sleep deprivation of lavender essential oil to be inhaled was applied to
because of anxiety; in other words, sleep disorder and a cotton gauze and placed in front of the patients. In
anxiety mutually affect each other (Cho et al., 2013). this way, its effect was observed in a short time via
Wenham and Pittard (2009) reported that in inten- inhalation (Gedney et al., 2004). Moeini et al. (2010)
sive care units, patients cannot sleep well and may stay applied aromatherapy with lavender essential oil to
awake for about 30–40% of their sleep time. Sleep dis- ischaemic heart disease patients in intensive care units
orders can be associated with increased sympathetic via inhalation and found that the quality of sleep
activity and subsequent increased blood pressure and after the intervention was significantly different. In
heart rate, raising the risk for developing cardiovas- the study conducted by Cho et al. (2013) with patients
cular problems among patients hospitalized in coro- diagnosed with CAD, it was determined that lavender
nary care units (Hajibagheri et al., 2014). Thus, avoiding essential oil had a positive effect on the quality of sleep
sleep disorder in patients with cardiac diseases is also and anxiety. Lytle et al. (2014) found that lavender
crucial in terms of reducing anxiety (Hajibagheri et al., essential oil increased the quality of sleep.
2014; Lytle et al., 2014). Intensive care nurses have major roles and responsi-
In coronary intensive care units, sleep dis- bilities such as early diagnosis, assessment of sleep dis-
oders are treated using both pharmacological and orders and anxiety as well as reducing present stressors
non-pharmacological methods. Sedative-hypnotic and arranging a therapeutic environment. It is seen
agents used in pharmacological treatments can that nurses, especially in Turkey, do not pay enough
increase the quality of sleep significantly; however, it is attention to non-pharmacological approaches although
stated that these drugs have side effects, cause addic- they have competence in using them for promoting
tion and do not provide adequate sleep (Kurt and Enç, and maintaining health. As health care team members
2013; Hajibagheri et al., 2014). Therefore, it is essential who spend most of the time with patients, it is cru-
to employ and implement non-pharmacological meth- cial for nurses to be aware of their problems and gen-
ods that are safer and have fewer side effects than the erate evidence-based solutions. Therefore, this study
pharmacological methods. aimed to produce evidence-based data for nurses in
One of the non-pharmacological approaches used Turkey to practise their independent nursing inter-
for sleep disorders is aromatherapy, which is prac- ventions. Furthermore, it is of significance that no
tised with essential oils from plants via both direct other study was conducted to investigate the effects
intervention to the skin and inhalation, which is a of lavender essential oil on sleep quality and anxi-
more effective method (Moeini et al., 2010; Özdemir ety in Turkey, which indicates the necessity of such a
and Öztunç, 2013; Bikmoradi et al., 2014). Aromather- research.
apy is used for pain, depression, anxiety, relaxation
and disorders related with sleep and stress (Abuham-
dah and Chazot, 2008; Lytle et al., 2014). Among the Aim and hypotheses
claims made for lavender essential oil, which is com- In this study, the aim was to investigate the effect of
monly used in aromatherapy, are its impact on amyg- lavender essential oil on the sleep quality and anxi-
dala and its relaxing, sedative effects and carminative ety level of patients hospitalized in coronary intensive
(smooth muscle relaxing) qualities, thus affecting sleep care unit.
quality, as well as its antibacterial, antifungal, antide-
pressive and stress-reducing qualities. It is also claimed Hypothesis 1: There is a significant difference
to be the least toxic and allergenic among essential oils between the Pittsburgh Sleep Quality Scale pretest
(Gedney et al., 2004; Lemon, 2004; Jimbo et al., 2009; and post-test mean scores of patients who received an
van der Ploeg et al., 2010; Cho et al., 2013; Bikmoradi aromatherapy of lavender essential oil.
2 © 2015 British Association of Critical Care Nurses
Effects of aromatherapy on sleep quality and anxiety of patients
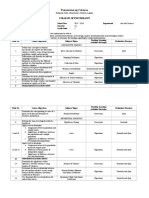
Hypothesis 2: There is a significant difference between in the control group randomly (Figure 1). The same
the Beck Anxiety Inventory pretest and post-test procedure continued with the following patients until
mean scores of patients who received an aromatherapy 30 patients were obtained in each group. In order
of lavender essential oil. not to allow an interaction of lavender inhalation
between patients in the intervention and control
groups, patients from different rooms were included
DESIGN AND METHODS within the scope of the study. There was no interac-
This study was designed as a randomized controlled tion between the researcher who implemented the
study. randomization and the researcher who conducted
the intervention; the blinding method was used. The
Setting and sampling patients in the intervention group were applied laven-
The study population consisted of patients hospital- der essential oil while no intervention was conducted
ized in the Coronary Intensive Care Unit of Şahinbey on the control group patients.
Research Hospital, Gaziantep Universty. The sample Drawing on the facts regarding lavender essential
size for this study was calculated using G*Power anal- oil in the literature that it is the least toxic and aller-
ysis. Using a significance level (𝛼) of 0⋅05, a statistical genic among other essential oils and that it provides
power (1-𝛽) of 0⋅80 and effect size of 0⋅74, as calculated effective relaxation as well as positive impacts on sleep
from previous studies, 30 aromatherapy and 30 control and anxiety, lavender essential oil was preferred to
subjects were needed for this study (Cho et al., 2013; be used in the study (Lemon, 2004; Jimbo et al., 2009;
Lytle et al., 2014). Of those who were receiving treat- Bikmoradi et al., 2014). Relevant literature was anal-
ment in the coronary intensive care unit and who were ysed to decide on the intervention method (inhalation)
eligible for the study, 60 patients were included within (Chien et al., 2012; Seifi et al., 2014) concentration 2 cc
the scope of the research. lavender essential oil + 100 cc water (2%) (Chien et al.,
The inclusion criteria were as follows: (a) 65 years 2012) intervention time (20 min) number of drops (two
of age or below, (b) diagnosed with CAD and passed drops) (Moeini et al., 2010; Chien et al., 2012; Cho et al.,
the first stage of disease (the first 24–48 h of the dis- 2013; Seifi et al., 2014). The intervention group were
ease), (c) no risk of heart failure and cardiogenic shock applied lavender essential oil for 15 days in total, which
(class III and IV), (d) no history of asthma, eczema was determined based on the average intensive care
and allergies to flowers and plants, (e) not allergic duration of patients hospitalized in the unit where the
to lavender, (f) communicative, no severe hearing or study was conducted, 5–15 days in average).
speech impairment, (g) no use of antidepressants, anti-
histamines, diuretics, hypnotics, benzodiazepines and
Intervention protocol
narcotic derivatives that affect the quality of sleep and
(A) Intervention Group: On the first day, the patients
(h) willingness to participate in the research.
were asked to fill in a questionnaire form regarding
their sociodemographic characteristics and diseases,
Data collection PSQI and BAI. For a period of 15 days, the patients
Before applying lavender oil, pretest data of the inter- were asked to inhale 2% lavender essential oil every
vention group were collected using a questionnaire on night before they went to sleep (21⋅00–24⋅00). Treat-
sociodemographic and disease characteristics, the BAI ment consisted of application of two drops of lavender
and PSQI. At the end of the intervention (day 15), the essential oil to a 2 × 2 cm cotton gauze, attached to the
BAI and PSQI scales were completed for all the patients front of the patients’ scrubs, approximately 12 inches
again. The control group patients were administered below their nose. Patients were directed to breathe
only the questionnaire for sociodemographic and dis- normally while they waited for 20 min (Gedney et al.,
ease characteristics, and the BAI and PSQI scales with- 2004). At the end of the 15th day, they were asked to fill
out administering any lavender oil. The same scales in the PSQI and BAI again and their sleep quality and
were repeated for each patient after 15 days. anxiety were evaluated.
(B) Control Group: On the first day, the patients were
Intervention and intervention protocol asked to fill in a questionnaire form regarding their
The patients were evaluated according to the eligibility sociodemographic characteristics and diseases, PSQI
criteria for the sample and were informed about the and BAI. The patients in this group were not applied
written consents. Of the patients who agreed to partic- lavender aromatherapy and at the end of the 15th day,
ipate in the research, the first patient was included in they were asked to fill in the PSQI and BAI again for
the intervention group while the second was included the evaluation of their sleep quality and anxiety.
© 2015 British Association of Critical Care Nurses 3
Effects of aromatherapy on sleep quality and anxiety of patients
Assessed for eligibility (n=300)
Enrollment
Excluded n=240
*Not meeting inclusion criteria (n=210)
*Declined to participate (n=30)
Randomization (n=60 )
Allocated
Allocated to intervention (n=30) Allocated to control (n=30)
Follow up
Lost to follow up (n=0) Lost to follow up (n=0)
Discontunied intervention (n=0) Discontunied cotrol (n=0)
Analysis
Analyzed (n=30) Analyzed (n=30)
Excluded from analyzed (n=0) Excluded from analyzed (n=0)
Figure 1 Consort flow diagram.
Instruments for evaluation sleep disturbances, use of sleeping medications and
Questionnaire for sociodemographic and disease daytime dysfunction, and are grouped into seven com-
characteristics ponents. Each item received a value ranging from 0 (no
This form was prepared by the researchers in accor- difficulty) to 3 (severe difficulty) and the score of each
dance with the literature (Chien et al., 2012; Cho et al., component ranged between 0 and 3. The seven com-
2013; Seifi et al., 2014). While the sociodemographic ponent scores are then summed to yield a global PSQI
data were collected using questions on age, sex, mar- score, which has a range of 0–21. Those receiving a total
ital status, educational level and social security, data score ≤ 5 are considered to have a ‘good’ sleep qual-
regarding health condition were collected using ques- ity (Buysse et al., 1989). PSQI has forms assessing the
tions on blood pressure, heart rate, use of alcohol and past month and week (In the forms, all the expressions
cigarette, daily activities, presence of chronic diseases, are the same except for the words ‘week’ and ‘month’.).
evaluation of health condition and sleep disorder. As we evaluated the sleep quality of the individual in
the past week, we used the weekly form of the PSQI.
Therefore, 15-day use of the tool is appropriate. Previ-
Pittsburgh Sleep Quality Index (PSQI) ous studies have also shown that PSQI could be used
Developed by Buysse et al. (1989), PSQI is an instru- for assessing sleep quality for a 1-week period or more
ment that provides information on the type and sever- (Lewith et al., 2005; Barbosa Neto et al., 2014).
ity of sleep disorders and sleep quality over a 1-month The validity and reliability of the instrument with
period. The instrument consists of a total of 24 ques- regard to Turkish patients were assessed by Ağargün
tions; 19 of which are self-rated while 5 are rated (1996), who reported the internal consistency coeffi-
by the bed partner or roommate. While the self-rated cient to be 0⋅80 (Ağargün, 1996). In this study, the Cron-
questions are included in the assessment, the other bach’s 𝛼 was found to be 0⋅94.
five questions are not tabulated in the scoring. The Beck Anxiety Inventory (BAI): It is a self-report instru-
19 self-rated questions assess subjective sleep quality, ment developed by Beck et al. (1988) that measures
sleep latency, sleep duration, habitual sleep efficiency, the frequency of anxiety individuals experience using
4 © 2015 British Association of Critical Care Nurses
Effects of aromatherapy on sleep quality and anxiety of patients
Table 1 Baseline characteristics at pretest between intervention and control groups
Groups n (%)
Variable Total sample (n = 60) N (%) Intervention group (n = 30) Control group (n = 30) Significance test (p)
Age (mean ± SD) 50⋅33 ± 12⋅44 53⋅30 ± 11⋅92 47⋅36 ± 11⋅82 1⋅936; 0⋅058∗
Time for diagnosis of CAD (years) (mean ± SD) 2⋅55 ± 1⋅24 2⋅80 ± 1⋅21 2⋅30 ± 1⋅23 1⋅580; 0⋅119∗
Sex
Female 20 (33⋅3) 10 33⋅3 10 33⋅3 3⋅333; 0⋅068†
Male 40 (66⋅7) 20 66⋅7 20 66⋅7
Educational level
Illiterate 9 (15⋅0) 7 23⋅3 2 6⋅7 9⋅500; 0⋅050†
Literate 10 (16⋅7) 5 16⋅7 5 16⋅7
Primary education 16 (26⋅7) 10 33⋅3 6 20⋅0
Secondary education 19 (31⋅7) 4 13⋅3 15 50⋅0
University 6 (10⋅0) 4 13⋅3 2 6⋅7
Presence of other chronic diseases
Yes 26 (43⋅3) 14 46⋅7 12 40⋅0 1⋅067; 0⋅302†
No 34 (56⋅7) 16 53⋅3 18 60⋅0
The presence of sleep problems
Yes 28 (46⋅7) 14 (46⋅7) 14 (46⋅7) 0⋅267; 0⋅606†
No 32 (53⋅3) 16 (53⋅3) 16 (53⋅3)
CAD, coronary artery disease.
∗ Independent t-test.
† 𝜒 2 analyses.
a 4-point Likert-type scale. The validity and reliabil- RESULTS
ity of the Turkish version was conducted by Ulu- Sample characteristics
soy et al. (1998) and the Cronbach’s 𝛼 coefficient was A total of 60 patients, 30 for intervention and 30 for
found to be 0⋅93. The score obtained from the instru- control group, were included in this study. Of the
ment ranges between 0 and 63. As for the items, 13 of study patients, 66⋅7% were males and 33⋅3% were
them measure physiological symptoms while 5 mea- females, with a mean age of 50⋅33 ± 12⋅14 years. Pri-
sure cognition and 3 refer to both somatic and cognitive mary school graduates comprised 26⋅7%, and 43⋅3%
symptoms. In this study, the Cronbach’s 𝛼 was found to had no accompanying chronic diseases other than
be 0⋅98. CAD. The average time for diagnosis of CAD was
2⋅55 ± 1⋅24 years and 31⋅7% of the patients had sleep
Data analysis problems (Table 1). Although not shown in the table,
Data were evaluated using SPSS software (SPSS, all the patients were married and 86⋅7% had social
Chicago, IL, USA) using numbers or percentages. The security.
𝜒 2 test and independent Student’s t-test were used There were no statistically significant differences
when comparing whether there was any difference between the intervention and control groups in
between the intervention and control groups in terms terms of age, gender, educational level, presence
of basic characteristics. Differences between the PSQI of accompanying disease and sleep disorder (p > 0⋅05)
and BAI scores obtained from the intervention and (Table 1). These findings gave homogeneity to the
control groups were analysed by using the indepen- groups.
dent student’s t-test. Paired sample student’s t-test
was used to assess the differences before and after
intervention within the same group. Difference of the PSQI and BAI scores between
intervention and control group
Ethical consideration When the PSQI and BAI scores of the patients in
Written consent was received from the ethics commit- the control and intervention groups before and after
tee (No: 24.03.2014/105) of Gaziantep University, Fac- the intervention were compared, the differences in
ulty of Medicine. Additionally, informed consents were the change were found to be statistically signifi-
obtained from all patients in line with the Declaration cant in favour of the intervention group (p < 0⋅05;
of Helsinki. Table 2).
© 2015 British Association of Critical Care Nurses 5
Effects of aromatherapy on sleep quality and anxiety of patients
Table 2 Difference of PSQI and BAI scores between intervention and control group at pretest and post-test
Intervention group Control group
Variable Mean (SD) Mean (SD) Significance test (p)
PSQI
Pretest 8⋅68 ± 2⋅96 9⋅44 ± 2⋅75 t ∗= −1⋅009 (0⋅318)
Post-test 7⋅60 ± 2⋅83 9⋅38 ± 2⋅60 t ∗= −2⋅420 (0⋅019)
Significance test (p) t †= 2⋅962, p = 0⋅006 t †= 0⋅694, p = 0⋅493
BAI
Pretest 16⋅00 ± 9⋅48 12⋅23 ± 6⋅12 t ∗= 1⋅827 (0⋅074)
Post-test 12⋅93 ± 7⋅70 13⋅00 ± 6⋅54 t ∗= −0⋅036 (0⋅971)
Significance test (p) t †= 4⋅850, p = 0⋅001 t †= −1⋅588, p = 0⋅123
BAI, Beck Anxiety Inventory; PSQI, Pittsburgh Sleep Quality Index.
∗ The score difference between intervention and control groups has been evaluated using independent sample t-test.
† The score difference between the pretest and post-test of the same group was evaluated using the paired sample t-test.
In the intervention group, a significant difference effective in preventing sleep disorders. By acting on
was found between the pretest and post-test scores of the lymbic system, lavender essential oil induces sleep
PSQI (t = 2⋅962, p = 0⋅006) and BAI (t = 4⋅850, p = 0⋅001). by producing 𝛾-aminobutyric acid effect especially
Following the aromatherapy intervention, the PSQI in the amygdala. Furthermore, lavender essential oil
and BAI mean scores decreased significantly; in other facilitates sleep by producing a sedative effect and
words, the anxiety level decreased (Table 2). inhibiting the release of acetylcholine (Peng et al.,
In the control group, no significant difference was 2009). Cho et al. (2013) found that lavender essential
found between the pretest and post-test scores of PSQI oil increased the quality of sleep in their study con-
(t = 0⋅694, p = 0⋅493) and BAI (t = −1⋅588, p = 0⋅123) ducted in a coronary intensive care unit. Chien et al.
(Table 2). (2012) also found that lavender aromatherapy led to a
significant improvement in sleep quality when women
had a 20-min exposure twice a week during a 12-week
DISCUSSION period. Moeini et al. (2010) found that the sleep qual-
The essential oils used in aromatherapy are extracted ity of cardiac patients in the intervention group
from aromatic plants (lavender, rose, jasemine, etc.) increased after the application of lavender essential
generally by steam distillation method (Köse et al., oil. Hajibagheri et al. (2014) investigated the effect of
2007; Özdemir and Öztunç, 2013). The vapourized Rosa damascene aromatherapy on the sleep quality of
essential oils are inhaled that result in various effects cardiac patients and found that the intervention signif-
by connecting to many centres from the hypothalamus icantly reduced sleep latency and sleep disturbances
and hippocampus to the lymbic system through the while it significantly improved the efficiency, the sub-
olfactory bulb (Köse et al., 2007). Sleep is an essential jective quality and the duration of sleep. The positive
component of health and is related to physical and effect of aromatherapy on improving sleep quality in
psychological well-being. Inadequate quality and haemodialysis patients has also been reported (Najafi
quantity of sleep in hospitalized patients are common et al., 2014). These findings support the results of
problems, particularly in intensive care or interme- our study.
diate care units (IMCUs), and they may have serious Anxiety is a complex phenomenon experienced very
detrimental effects on health and recovery from illness frequently by patients hospitalized in intensive care
(Lytle et al., 2014). units (Mui So and Chan, 2004; Wenham and Pittard,
In this study, which aimed to investigate the effect 2009). Aromatherapy is a therapy to promote physical,
of aromatherapy on the the sleep quality and anxi- mental and psychological health, to maintain health
ety level of patients in coronary intensive care unit, and to enhance vitality with therapeutic components
it was found that the quality of sleep increased in of refined essential oil extracted from various plants.
patients who received aromatherapy. In parallel with Inhalation aromatherapy is a technique in which essen-
our finding, Moeini et al. (2010) also stated that the tial oils are used in inhalation, which can decrease pain,
quality of sleep increased in cardiac patients after anxiety and depression and improve the vital signs
aromatherapy. Similarly, Goel et al. (2005), Lewith (Seifi et al., 2014). In this study, it was observed that
et al. (2005) and Kasper et al. (2010) found that aro- the anxiety level of patients decreased significantly
matherapy conducted with lavender essential oil was in the intervention group, whereas it increased in the
6 © 2015 British Association of Critical Care Nurses
Effects of aromatherapy on sleep quality and anxiety of patients
control group. These results are consistent with the IMPLICATIONS AND
anxiety-decreasing effects of aromatherapy in patients RECOMMENDATIONS FOR PRACTICE
before surgery (Oh and Jung, 2002), before percuta- Drawing on the fact that the effects of lavender essen-
neous coronary intervention (Cho et al., 2013), during tial oil have not been researched in Turkey, it is essential
menstruation (Kim et al., 2011), in haemodialysis that lavender aromatherapy be experimented with dif-
patients (Kim et al., 2007) and during colonoscopy ferent and larger samples and that the evidence data be
(Lee and Ahn, 2010). In the study conducted by Woelk transferred to nursing practices. For this reason, there
and Schläfke (2010), the impacts of medical treatment is a need for a greater number of research studies to be
and lavender essential oil inhalation on anxiety were conducted in this field.
compared and it was found that lavender oil was as
effective as medical treatment in reducing anxiety. On
the other hand, Seifi et al. (2014) and Bikmoradi et al. CONCLUSION
(2014) stated that lavender essential oil application by This study found that lavender essential oil increased
way of inhalation was not effective on mental stress the quality of sleep and reduced the level of anx-
and anxiety of patients who had undergone coronary iety in patients with CAD. In coronary care units,
bypass surgery. sleep disorders and anxiety are important factors influ-
encing the well-being of patients. Nurses have major
responsibilities because they spend long time with
LIMITATIONS patients. As a non-invasive, inexpensive, easily appli-
In this study, the short-term effect of lavender essential cable, cost-effective, independent nursing intervention
oil has been evaluated. Therefore, the findings obtained and appropriate for cardiac patients, lavender essential
are valid for the short-term effect of lavender essential oil could be applied in intensive care units.
oil on sleep quality and anxiety.
WHAT IS KNOWN ABOUT THIS TOPIC
• Intensive care unit patients cannot sleep well and may stay awake for about 30–40% of their sleep time.
• Aromatherapy is used for pain, depression, anxiety, relaxation and disorders related with sleep and stress.
WHAT THIS PAPER ADDS
• Lavender essential oil increased the quality of sleep and reduced the level of anxiety in patients with coronary artery disease.
• As a non-invasive, inexpensive, easily applicable, cost-effective, independent nursing intervention and appropriate for cardiac patients,
lavender essential oil could be applied in intensive care units.
REFERENCES lavender essential oil on stress and vital signs inpatients
undergone coronary artery bypass surgery: a single blinded
Abuhamdah S, Chazot PL. (2008). Lemon balm and lavender
randomized clinical trial. Complementary Therapies in Medicine.
herbal essential oils: old and new ways to treat emotional
23:331–338. DOI: 10.1016/j.ctim.2014.12.001.
disorders? Current Anaesthesia & Critical Care; 19: 221–226.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DC.
Ağargün MY. (1996). Validity and reliability of Turkish version
(1989). The Pittsburgh Sleep Quality Index: a new instrument
of Pittsburgh Sleep Quality Index. Türk Psikiyatri Dergisi; 7:
107–115. for psychiatric practice and research. Psychiatry Research; 28:
Akça Ay F. (2012). Basic Concepts and Skills in Health Practice. 4th 193–213.
edn. Nobel Bookstore, Istanbul. Chien LW, Cheng SL, Liu CF. (2012). The effect of lavender aro-
Badır A, Demir Korkmaz F. (2010). Coronary artery disease. In: matherapy on autonomic nervous system in midlife women
Karadakovan A, Eti Aslan F, (eds), Care in the Medical and with insomnia. Evidence-Based Complementary and Alterna-
Surgical Diseases. Vol. 2. Adana: Nobel. tive Medicine; 2012;2012:740813, 8 pages. doi:10.1155/2012/
Barbosa Neto JB, Germain A, Mattos PF, Serafim PM, Santos 740813.
RCM, Martini LC, Suchecki D, Mello MF. (2014). Psychometric Cho MY, Min ES, Hur MH, Lee MS. (2013). Effects of aromather-
properties of the Brazilian version of the Pittsburgh Sleep apy on the anxiety, vital signs, and sleep quality of percuta-
Quality Index Addendum for PTSD (PSQI-A). Revista Brasileira neous coronary intervention patients in intensive care units.
de Psiquiatria; 36: 330–335. Evidence-Based Complementary and Alternative Medicine; 2013;
Beck AT, Epstein N, Brown G, Steer RA. (1988). An inventory for 2013:381381. doi:10.1155/2013/381381.
measuring clinical anxiety: psychometric properties. Journal of Dedeli Ö, Durmaz Akyol A. (2008). Psychosocial issues in inten-
Consulting and Clinical Psychology; 56: 893–897. sive care patients. Journal of Critical Care Nursing; 12: 26–32.
Bikmoradi A, Seifi Z, Poorolajal J, Araghchian M, Safiaryan R, Fayazi S, Babashahi M, Rezaei M. (2011). The effect of inhalation
Oshvandi K. (2014). Effect of inhalation aromatherapy with aromatherapy on anxiety level of patients in preoperative
© 2015 British Association of Critical Care Nurses 7
Effects of aromatherapy on sleep quality and anxiety of patients
period. Iranian Journal of Nursing and Midwifery Research; 16: Moeini M, Khadibi M, Bekhradi R, Ahmad Mahmoudian S, Nazari
278–283. F. (2010). Effect of aromatherapy on the quality of sleep in
Gedney JJ, Glover LT, Fillingim BR. (2004). Sensory and affective ischemic heart disease patients hospitalized in intensive care
pain discrimination after inhalation of essential oils. Psychoso- units of heart hospitals of the Isfahan University of Medical
matic Medicine; 66: 599–606. Sciences. Iranian Journal of Nursing and Midwifery Research; 15:
Goel N, Kim H, Lao RP. (2005). An olfactory stimulus modifies 234–239.
nighttime sleep in young men and women. Chronobiology Inter- Mui So H, Chan DSK. (2004). Perception of stresssors by patients
national; 22: 889–904. and nurses of critical care units in Hong Kong. International
Hajibagheri A, Babaii A, Adib-Hajbaghery M. (2014). Effect of Journal of Nursing Studies; 41: 77–84.
Rosa damascene aromatherapy on sleep quality in cardiac Najafi Z, Tagharrobi Z, Shahriyari-Kale-Masihi M. (2014). Effect of
patients: a randomized controlled trial. Complementary Thera- aromatherapy with lavender on sleep quality among patients
pies in Clinical Practice; 20: 159–163. under going hemodialysis. Feyz Journal of Kashan University of
İnangil D, Şendir M. (2014). Nurse’s role in the development of Medical Sciences; 18: 145–150.
health behavior of coronary artery disease. Journal of Acibadem Oh YH, Jung HM. (2002). The effects of inhalation method using
University Health Sciences; 5: 96–101. essential oils on the preoperative anxiety of hystrectomy
Jimbo D, Kimura Y, Taniguchi M, Inoue M, Urakami K. (2009). patients. Korean Academic Society of Rehabilitation Nursing; 5:
Effect of aromatherapy on patients with Alzheimer’s disease. 18–26.
Psychogeriatrics; 9: 173–179. Onat A, Çakır H, Karadeniz Y, Dönmez İ, Karagöz A, Yüksel M,
Kasper S, Gastpar M, Müller WE, Volz HP, Möller HJ, Dienel A, Can G. (2014). Turkish adult risk factor survey 2013: rapid rise
Schläfke S. (2010). Silexan, an orally administered Lavandula in the prevalence of diabetes [Article in Turkish]. Turk Kardiyol
oil preparation, is effective in the treatment of ‘subsyndro- Dern Ars; 42: 511–516.
mal’ anxiety disorder: a randomized, double-blind, placebo Özdemir H, Öztunç G. (2013). Aromatherapy in Nursing Practice:
controlled trial. International Clinical Psychopharmacology; 25: Review. Journal of Turkey Clinical Nursing Science. 5: 98–104.
277–287. Peng SM, Koo M, Yu ZR. (2009). Effects of music and essential oil
Kim YJ, Lee MS, Yang YS, Hur MH. (2011). Self aromather- inhalation on cardiac autonomic balance in healthy individu-
apy massage of the abdomen for the reduction of men- als. The Journal of Alternative and Complementary Medicine; 15:
strual pain and anxiety during menstruation ın nurses: a 53–57.
placebo-controlled clinical trial. European Journal of Integrative Seifi Z, Beikmoradi A, Oshvandi K, Poorolajal J, Araghchian M,
Medicine; 3: 165–168. Safiaryan R. (2014). The effect of lavender essential oil on anx-
Kim OJ, Kim KH, Park KS. (2007). The effect of aroma inhalation iety level in patients undergoing coronary artery bypass graft
on stress, anxiety and sleep pattern in patients with hemo- surgery: a double-blinded randomized clinical trial. Iranian
dialysis. Journal of the Korean Clinical Nursing Research; 13: Journal of Nursing and Midwifery Research; 19: 574–580.
99–111. Tunçay GY, Uçar H. (2010). Opinions of patients on physical envi-
Köse E, Sarsılmaz M, Ögetürk M, Kuş İ, Kavaklı A, Zararsız İ. ronmental features of ıntensive care units. Hacettepe University
(2007). The role of rose essential oil aroma on the learning Faculty of Health Sciences Nursing Journal; 17: 33–46.
behaviours: an experimental study. Firat Medical Journal; 12: Turkish Society of Cardiology. (2013). National heart health
159–162. policy basic principles. http://www.tkd-online.org (accessed
Kurt S, Enç N. (2013). Sleep problems ın critical care patients 12/12/14).
and nursing care. Turkish Journal of Cardiovascular Nursing; 4: Ulusoy M, Şahin NH, Erkmen H. (1998). Turkish version of the
1–8. Beck anxiety inventory: psychometric properties. Journal of
Lee YM, Ahn HY. (2010). Effect of the aromatherapy on anxi- Cognitive Psychotherapy; 12: 163–172.
ety and discomfort in patients having colonoscopy. Journalof Van der Ploeg E, Eppingstall B, Connor D. (2010). The study
Korean Academy of Fundamentals of Nursing; 17: 539–547. protocol of a blinded randomised controlled cross-over trial
Lemon K. (2004). An assesment of treating depression and anxiety of lavender oil as a treatment of behavioural symptoms in
with aromatherapy. The International Journal of Aromatherapy; dementia. BMC Geriatrics; 10: 1–5.
14: 63–69. Wenham T, Pittard A. (2009). Intensive care unit environment.
Lewith G, Godfrey A, Prescott PA. (2005). Single-blinded, random- Continuning Education in Anaesthesia Critical Care Pain; 9:
ized pilot study evaluating the aroma of Lavandula augustifolia 178–183.
as a treatment for mild insomnia. The Journal of Alternative and WHO. (2015). Cardiovasculer diseases (CVDs). http://www.who.
Complementary Medicine; 11: 631–637. int/mediacentre/factsheets/fs317/en/ (accessed 12/05/15).
Lytle J, Mwatha C, Davis K. (2014). Effect of lavender aromather- Woelk H, Schläfke S. (2010). A multi-center, double-blind, ran-
apy on vital signs and perceived quality of sleep in the domised study of the Lavender oil preparation Silexan in
intermediate care unit: a pilot study. American Journal of Critical comparison to Lorazepam for generalized anxiety disorder.
Care; 23: 24–29. Phytomedicine; 17: 94–99.
8 © 2015 British Association of Critical Care Nurses
You might also like
- Artikel 8 PDFDocument8 pagesArtikel 8 PDFapryani lumban gaolNo ratings yet
- 154943-404874-1-SM MassDocument6 pages154943-404874-1-SM MassSyarief NurseNo ratings yet
- Applied Nursing Research: Gamze Muz, Sultan Ta ŞcıDocument8 pagesApplied Nursing Research: Gamze Muz, Sultan Ta ŞcıMonyet...No ratings yet
- The Effect of Music On Comfort, Anxiety and Pain in The Intensive Care Unit: A Case in TurkeyDocument9 pagesThe Effect of Music On Comfort, Anxiety and Pain in The Intensive Care Unit: A Case in Turkeyandra kurniaNo ratings yet
- Efektifitas Aroma Terapiessensial Oil Rose Dalammenurunkanskalanyeripadapasienkanker Stadium IiDocument10 pagesEfektifitas Aroma Terapiessensial Oil Rose Dalammenurunkanskalanyeripadapasienkanker Stadium IiKyaruuNo ratings yet
- The Effect of Massage Therapy On Sleep Quality in Cardiac Care Unit PatientsDocument7 pagesThe Effect of Massage Therapy On Sleep Quality in Cardiac Care Unit Patientsayu purnamaNo ratings yet
- The Effect of Lavender Oil Application Via Inhalation Pathway On Hemodialysis Patients' Anxiety Level and Sleep QualityDocument12 pagesThe Effect of Lavender Oil Application Via Inhalation Pathway On Hemodialysis Patients' Anxiety Level and Sleep QualityRoberta PraxedesNo ratings yet
- Back Massage Intervention For Improving Health and Sleep Quality Among Intensive Care Unit PatientsDocument7 pagesBack Massage Intervention For Improving Health and Sleep Quality Among Intensive Care Unit PatientsيوكيNo ratings yet
- Complementary Therapies To Improve The Quality of Sleep in The Elderly: A Systematic ReviewDocument6 pagesComplementary Therapies To Improve The Quality of Sleep in The Elderly: A Systematic ReviewSavitriNo ratings yet
- Akman 2015Document7 pagesAkman 2015Ariwati Anggita PutriNo ratings yet
- CEJNM - CJN 201704 0003Document6 pagesCEJNM - CJN 201704 0003Yuliaa SaputriNo ratings yet
- Effects of eye masks and earplugs on sleep quality and anxiety in hospitalized patientsDocument9 pagesEffects of eye masks and earplugs on sleep quality and anxiety in hospitalized patientsjayaNo ratings yet
- The Effects of Massage Therapy On SleepDocument5 pagesThe Effects of Massage Therapy On SleepraniNo ratings yet
- The Influence of Gayatri Mantra and EmotDocument8 pagesThe Influence of Gayatri Mantra and EmotOrlando HernándezNo ratings yet
- Aromatherapy Massage For Neuro PDFDocument11 pagesAromatherapy Massage For Neuro PDFTitin JuherniNo ratings yet
- 22 The Effects of Noise Levels On Nurses inDocument7 pages22 The Effects of Noise Levels On Nurses inLeonardoMartínezNo ratings yet
- Jurnal Akupresur Kelompok 5Document25 pagesJurnal Akupresur Kelompok 5Balkis 13No ratings yet
- Comparing The Effects of Music and Exercise With Music For Older Adults With InsomniaDocument7 pagesComparing The Effects of Music and Exercise With Music For Older Adults With InsomniaConsuelo VelandiaNo ratings yet
- Foot BathDocument10 pagesFoot BathAfnizar WAhyu RamadhanNo ratings yet
- Jurnal GGL JNTG WahyuDocument11 pagesJurnal GGL JNTG WahyuWahyu SusilowatiNo ratings yet
- Musik Terapi NeuropatiDocument10 pagesMusik Terapi NeuropatiAdihypno PurnomoNo ratings yet
- 18 Bicer Original 10 1Document8 pages18 Bicer Original 10 1Nurul HafizaNo ratings yet
- Palliative Care: The Practice of End of Life CareDocument10 pagesPalliative Care: The Practice of End of Life CareAnonymous CwJeBCAXpNo ratings yet
- Ircmj 16 15485Document7 pagesIrcmj 16 15485pangaribuansantaNo ratings yet
- Jurnal SpiritualDocument6 pagesJurnal SpiritualQodri DewiNo ratings yet
- Effects of Back Massage On Chemotherapy-Related Fatigue and Anxiety: Supportive Care and Therapeutic Touch in Cancer NursingDocument8 pagesEffects of Back Massage On Chemotherapy-Related Fatigue and Anxiety: Supportive Care and Therapeutic Touch in Cancer NursingFauzul AzhimahNo ratings yet
- Pengaruh Terapi Posisi Lateral Kanan Terhadap Kualitas Tidur Pasien Gagal Jantung Di Rsup M Djamil PadangDocument9 pagesPengaruh Terapi Posisi Lateral Kanan Terhadap Kualitas Tidur Pasien Gagal Jantung Di Rsup M Djamil PadangKholisatun NisaNo ratings yet
- NYERI DistractionDocument6 pagesNYERI DistractionHandayaniNo ratings yet
- Vital Signs: Valid Indicators To Assess Pain in Intensive Care Unit Patients? An Observational, Descriptive StudyDocument7 pagesVital Signs: Valid Indicators To Assess Pain in Intensive Care Unit Patients? An Observational, Descriptive Studybardah wasalamahNo ratings yet
- 4 AbaDocument7 pages4 AbaGabrielle Ann SalazarNo ratings yet
- ContentServer 2Document12 pagesContentServer 2Meined19No ratings yet
- Murottal Al-Qur'An Stimulation For Reducing Anxiety Level On Acute Coronary Syndrome Patient: A Practice Based On EvidenceDocument9 pagesMurottal Al-Qur'An Stimulation For Reducing Anxiety Level On Acute Coronary Syndrome Patient: A Practice Based On EvidenceDesi Ratna SariNo ratings yet
- Effect of Accupressure On Quality of Sleep and Pulse Rate in Patients With Acute Myocardial InfarctionDocument10 pagesEffect of Accupressure On Quality of Sleep and Pulse Rate in Patients With Acute Myocardial InfarctionErnaNo ratings yet
- JJCDC 21796Document6 pagesJJCDC 21796agung MaulanaNo ratings yet
- Effect of Acupressure On Quality of Sleep and Pulse Rate in Patients With Acute Myocardial InfarctionDocument10 pagesEffect of Acupressure On Quality of Sleep and Pulse Rate in Patients With Acute Myocardial InfarctionAri PutraNo ratings yet
- Spiritual EFT's Influence on Anxiety and Sleep Quality in Breast Cancer PatientsDocument6 pagesSpiritual EFT's Influence on Anxiety and Sleep Quality in Breast Cancer PatientsApril LiasariNo ratings yet
- 12 Ustundag Orignial 9 3Document8 pages12 Ustundag Orignial 9 3Sanjivi GovekarNo ratings yet
- San Vera Materi ADocument13 pagesSan Vera Materi Aendah desfindaNo ratings yet
- Oamjms 11f 180Document16 pagesOamjms 11f 180clinichafshahNo ratings yet
- A Study On Assessment of Frequency, Intensity, Disability and Severity Associated With Primary HeadachesDocument7 pagesA Study On Assessment of Frequency, Intensity, Disability and Severity Associated With Primary HeadachesDhEg LieShh WowhNo ratings yet
- Nurse-Led CBT Therapy for InsomniaDocument6 pagesNurse-Led CBT Therapy for InsomniaWita AnggraeniNo ratings yet
- Lim R (2018) Benefits of Quiet Time Interventions in The Intensive Care Unit - A Literature Review. Nursing Standard. 32, 30, 41-48.Document8 pagesLim R (2018) Benefits of Quiet Time Interventions in The Intensive Care Unit - A Literature Review. Nursing Standard. 32, 30, 41-48.Neesha MNo ratings yet
- Journal of Affective Disorders: Yueheng Tang, Minmin Gong, Xin Qin, Hao Su, Zhi Wang, Hui DongDocument9 pagesJournal of Affective Disorders: Yueheng Tang, Minmin Gong, Xin Qin, Hao Su, Zhi Wang, Hui DongmirahutamidewiNo ratings yet
- Pengaruh Musik Instrumental Kitaro Terhadap Kualitas Tidur Pasien Rawat Inap Yang Mengalami Gangguan Tidur Di Rsud UngaranDocument12 pagesPengaruh Musik Instrumental Kitaro Terhadap Kualitas Tidur Pasien Rawat Inap Yang Mengalami Gangguan Tidur Di Rsud UngaranIndah sbNo ratings yet
- Effectiveness of Back Massage in Promoting Sleep Pattern of Patients With Congestive Cardiac Failure PDFDocument8 pagesEffectiveness of Back Massage in Promoting Sleep Pattern of Patients With Congestive Cardiac Failure PDFArio Raafsan Anugrah PutraNo ratings yet
- Improving Sleep QualityDocument10 pagesImproving Sleep Qualityapi-349689592No ratings yet
- Effect of Progressive Muscle Relaxation With Analgesic On Anxiety Status and Pain in Surgical PatientsDocument5 pagesEffect of Progressive Muscle Relaxation With Analgesic On Anxiety Status and Pain in Surgical PatientsAzza SintaNo ratings yet
- Unal 2016Document21 pagesUnal 2016Deni MalikNo ratings yet
- Pijat Punngung Kemo WordDocument8 pagesPijat Punngung Kemo WordefielyarizaNo ratings yet
- Narsum 2. Gangguan Tidur Narsum DR - Apt Ika PuspitasariDocument33 pagesNarsum 2. Gangguan Tidur Narsum DR - Apt Ika PuspitasariKariEm uLLahNo ratings yet
- Jurnal UtamaDocument8 pagesJurnal UtamaUhti JahrotunisaNo ratings yet
- Applied Nursing Research: Original ArticleDocument8 pagesApplied Nursing Research: Original ArticleWahyonoNo ratings yet
- The Effect of Inhalation Aromatherapy With Lavender On Sleep Quality of The Elderly in Nursing Care Homes A Randomized Clinical TrialDocument7 pagesThe Effect of Inhalation Aromatherapy With Lavender On Sleep Quality of The Elderly in Nursing Care Homes A Randomized Clinical TrialSatria Yosi HernawanNo ratings yet
- Nursing Care For Stroke Patients: A Survey of Current Practice in Eleven European CountriesDocument22 pagesNursing Care For Stroke Patients: A Survey of Current Practice in Eleven European CountriesSiti Ariatus AyinaNo ratings yet
- Terapi Kombinasi Sugesti Dan Dzikir Dalam Peningkatan Kualitas Tidur PasienDocument12 pagesTerapi Kombinasi Sugesti Dan Dzikir Dalam Peningkatan Kualitas Tidur PasienRoby L HNo ratings yet
- The Application of Art Therapy To Reduce The Level of Depression in Patients With HemodialysisDocument7 pagesThe Application of Art Therapy To Reduce The Level of Depression in Patients With Hemodialysisbardah wasalamahNo ratings yet
- Decision To Choose Acupuncture Therapy For Degenerative 'LVHDVHV DPRQJ WKH (OGHUO/ DW - D Idu 0Hglnd +rvslwdo KaranganyarDocument11 pagesDecision To Choose Acupuncture Therapy For Degenerative 'LVHDVHV DPRQJ WKH (OGHUO/ DW - D Idu 0Hglnd +rvslwdo KaranganyarSitilestariNo ratings yet
- The Experience of Sleep Deprivation in Intensive Care Patients: Findings From A Larger Hermeneutic Phenomenological StudyDocument7 pagesThe Experience of Sleep Deprivation in Intensive Care Patients: Findings From A Larger Hermeneutic Phenomenological Studyrap 2treyNo ratings yet
- Effect of Psychoeducation On Anxiety in Patients With Coronary Heart DiseaseDocument7 pagesEffect of Psychoeducation On Anxiety in Patients With Coronary Heart DiseaseIsmunandar wahyu KNo ratings yet
- Clinical Synopsis of COVID-19: Evolving and ChallengingFrom EverandClinical Synopsis of COVID-19: Evolving and ChallengingHemanshu PrabhakarNo ratings yet
- Avery Sporting GoodsDocument15 pagesAvery Sporting GoodsKodem JohnsonNo ratings yet
- Chapter 4Document67 pagesChapter 4Minh Ngan NguyenNo ratings yet
- Statistics For Anal. Chem. - Lecture Notes - Xu Ly So LieuDocument157 pagesStatistics For Anal. Chem. - Lecture Notes - Xu Ly So LieuLiên Hương100% (1)
- DMAIC Six Sigma Guide 3MDocument162 pagesDMAIC Six Sigma Guide 3Mejedelmal100% (5)
- Psychological Statistics SyllabusDocument4 pagesPsychological Statistics SyllabusGrace Cadag100% (1)
- Statistics Without Maths For Psychology 7Th Edition by Christine Dancey PDF Full ChapterDocument41 pagesStatistics Without Maths For Psychology 7Th Edition by Christine Dancey PDF Full Chaptervirginia.carmona601100% (27)
- Choosing Between Parametric and Non-Parametric TestsDocument17 pagesChoosing Between Parametric and Non-Parametric TestsGB Sawey-OgnayonNo ratings yet
- SPE-124799-PA-Determining Wax Type Paraffin or NaphtheneDocument6 pagesSPE-124799-PA-Determining Wax Type Paraffin or NaphtheneJohn HastingNo ratings yet
- Credit Card AnalysisDocument19 pagesCredit Card Analysisar1304 bhatiaNo ratings yet
- Hyphothesis With Two Independent Sample Test - CompressedDocument14 pagesHyphothesis With Two Independent Sample Test - CompressedResiNo ratings yet
- SS 03 Quiz 1 AnswersDocument64 pagesSS 03 Quiz 1 AnswersjusNo ratings yet
- Defense Powerpoint 1-3Document96 pagesDefense Powerpoint 1-3Rose Dacles90% (20)
- Teachers' Perceptions of Effective Strategies For Teaching Literature To Enhance BEED Students' LearningDocument6 pagesTeachers' Perceptions of Effective Strategies For Teaching Literature To Enhance BEED Students' LearningnylanehrNo ratings yet
- Best Machine Learning Interview Questions and AnswersDocument38 pagesBest Machine Learning Interview Questions and AnswersabhishekNo ratings yet
- Impact of employee engagement on job satisfaction and motivationDocument11 pagesImpact of employee engagement on job satisfaction and motivationJeswin BennyNo ratings yet
- Research Plan in QuantitativeDocument8 pagesResearch Plan in QuantitativeNurur Risky AuliaNo ratings yet
- BSC Statistics Syllabus 01122015Document16 pagesBSC Statistics Syllabus 01122015sandhyaNo ratings yet
- Nyabwanga Et Al 2013Document16 pagesNyabwanga Et Al 2013Robert Nyamao NyabwangaNo ratings yet
- Business Statistics Final Exam SolutionsDocument10 pagesBusiness Statistics Final Exam SolutionsTesfsh Demis BitewNo ratings yet
- SUSS BSBA: BUS105 Jan 2021 TOA AnswersDocument9 pagesSUSS BSBA: BUS105 Jan 2021 TOA AnswersAzido AzideNo ratings yet
- Using Oral and Written Feedback To Improve Student Writing-LibreDocument60 pagesUsing Oral and Written Feedback To Improve Student Writing-LibreThanh LêNo ratings yet
- Victor Jupp The SAGE Dictionary of Social Research Methods 2006Document348 pagesVictor Jupp The SAGE Dictionary of Social Research Methods 2006TanaseAdrianaIoana100% (1)
- 3 IS Module 5Document11 pages3 IS Module 5Hiezeyl Ymana GuntangNo ratings yet
- CFA L1 SCHWSR FL Test Ques+Ans - NDocument52 pagesCFA L1 SCHWSR FL Test Ques+Ans - NAdamNo ratings yet
- Psych Stat Notes FinalDocument11 pagesPsych Stat Notes FinalKdrama SweetieNo ratings yet
- Epidemiology MCQsDocument4 pagesEpidemiology MCQsyooshlo78% (32)
- Writing A Protocol Mccrindle 20161.zp88724Document54 pagesWriting A Protocol Mccrindle 20161.zp88724Anonymous tBxCPAEX7SNo ratings yet
- Kreativitas SiswaDocument8 pagesKreativitas SiswaImanuelNo ratings yet
- A Study On Consumer Satisfaction Towards Jio NetworkDocument32 pagesA Study On Consumer Satisfaction Towards Jio NetworkAjmal Roshan100% (1)