Professional Documents
Culture Documents
Jaundice: in Older Children and Adolescents
Uploaded by
hectorOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jaundice: in Older Children and Adolescents
Uploaded by
hectorCopyright:
Available Formats
Article gastroenterology
Jaundice in Older Children and
Adolescents
Dinesh Pashankar, MD,*
Objectives After completing this article, readers should be able to:
and Richard A. Schreiber,
MD† 1. Describe the basic physiology of bilirubin metabolism, the two standard laboratory
methods for its fractionation, and the classification of jaundice.
2. Characterize the features of Gilbert disease.
3. Identify the leading infectious cause of acute jaundice in older children and
adolescents.
4. Delineate the clinical and biochemical features of Wilson disease and autoimmune
hepatitis.
5. Compare and contrast liver function tests and tests of liver function.
6. Describe the “worrisome” clinical and laboratory signs of hepatic synthetic dysfunction
in jaundiced patients that should prompt an immediate referral to a center where liver
Additional media transplantation is available.
illustrating features of
the disease processes
discussed are available Introduction
in the online version
Jaundice is defined as the presence of a yellow or yellow-greenish hue to the skin, sclera,
of this article at
and mucous membranes due to an elevation of serum bilirubin. In healthy individuals, the
www.pedsinreview.org.
total serum bilirubin is less than 1 mg/dL (17 mcmol/L). Jaundice can be readily detected
clinically when the total serum bilirubin is greater than 5 mg/dL (85 mcmol/L). Clinical
jaundice occurs much less frequently in older children and adolescents than in neonates.
Moreover, the differential diagnosis in this older age group differs markedly from that in
newborns and young infants. This review provides a practical approach to the clinical
evaluation of jaundice in the older child or adolescent. Because jaundice may be the
presenting feature of life-threatening conditions such as ful-
minant liver failure, a prompt and logical evaluation is nec-
essary to identify the more serious disorders that require
urgent management.
Abbreviations
ALP: alkaline phosphatase Bilirubin Metabolism
ALT: alanine aminotransferase Bilirubin is a product of heme metabolism. Heme is con-
ANA: antinuclear antibody verted in the reticuloendothelial (RE) system to biliverdin
ASMA: anti-smooth muscle antibody and then to bilirubin by heme oxygenase and biliverdin
AST: aspartate aminotransferase reductase, respectively. Bilirubin is lipophylic and is bound to
CNS: central nervous system serum albumin in circulation from the RE system to the liver.
EBV: Epstein-Barr virus The liver takes up the bilirubin-albumin complex through an
GGT: gamma glutamyltransferase albumin receptor. Bilirubin, but not albumin, is transferred
HAV: hepatitis A virus across the hepatocyte membrane and transported through
HBV: hepatitis B virus the cytoplasm to the smooth endoplasmic reticulum bound
HCV: hepatitis C virus primarily to ligandin or Y protein, a member of the glutathi-
KF: Kayser-Fleischer one S-transferase gene family of proteins. There, the water-
PT: prothrombin time insoluble bilirubin is conjugated to water-soluble bilirubin
RE: reticuloendothelial monoglucuronide and diglucuronide by UDP-glucuronosyl
transferase. The bilirubin conjugates are excreted through
*Clinical Assistant Professor of Pediatrics, Division of Gastroenterology, Children’s Hospital of Iowa, Iowa City, IA.
†
Clinical Associate Professor of Pediatrics, University of British Columbia, Division of Gastroenterology, British Columbia’s
Children’s Hospital, Vancouver, BC, Canada.
Pediatrics in Review Vol.22 No.7 July 2001 219
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
gastroenterology jaundice in children
Table 1. Fractionation of Bilirubin Causes of
Table 2.
Diazo® Method Hyperbilirubinemia in Older
Total bilirubin ⴝ Direct bilirubinm ⴙ Indirect bilirubinm Children
Ektachem® Slide Method Unconjugated Hyperbilirubinemia
Total bilirubinm ⴝ Conjugated bilirubinm ⴙ Hemolytic anemias
Unconjugated bilirubinm ⴙ Delta bilirubin Gilbert syndrome
The Diazo method measures the direct and indirect Crigler-Najjar syndrome
bilirubin and calculates the total. In the Ektachem Conjugated Hyperbilirubinemia
slide method, the total, conjugated, and
unconjugated bilirubin fractions are measured and Viral Infections
the delta bilirubin is calculated. m ⴝ measured. Hepatitis viruses A, B, C, D, E
Epstein-Barr virus
Cytomegalovirus
Herpes simplex
the canalicular membrane into the bile duct system by an Metabolic Liver Disease
energy-dependent process. Conjugated bilirubin flows in Wilson disease
the bile to the intestine, where it is broken down by gut Alpha-1-antitrypsin deficiency
flora to urobilinogen and stercobilin. Cystic fibrosis
Biliary Tract Disorders
Total serum bilirubin consists of an unconjugated Cholelithiasis
fraction and conjugated fraction of bilirubin and a frac- Cholecystitis
tion of bilirubin glucuronide that is bound covalently to Choledochal cyst
albumin known as delta-bilirubin. The newer Ektachem威 Sclerosing cholangitis
slide method for bilirubin fractionation accurately mea- Autoimmune Liver Disease
Type 1 (anti-smoooth muscle antibody)
sures the levels of unconjugated, conjugated, and total Type 2 (anti-liver-kidney-microsomal antibody)
serum bilirubin. Delta-bilirubin concentration can be Hepatotoxins
calculated from these figures (Table 1). With the tradi- Drugs: Acetaminophen
tional Diazo威 method for bilirubin fractionation, indirect Anticonvulsants
and direct bilirubin are measured and the total bilirubin Anesthetics
Antituberculous agents
is calculated. Unconjugated or indirect hyperbiliru- Chemotherapeutic agents
binemia is defined biochemically by an increased total Antibiotics
serum bilirubin level with less than 15% of the bilirubin in Oral contraceptives
the direct or conjugated form. Conjugated or direct Other: Alcohol, insecticides, organophosphates
hyperbilirubinemia is characterized by the conjugated or Vascular Causes
Budd-Chiari syndrome
direct fraction being greater than 20% of the total serum Veno-occlusive disease
bilirubin.
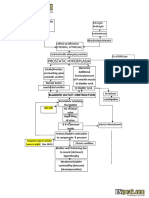
Differential Diagnosis phosphate dehydrogenase, or a hemoglobinopathy
The differential diagnosis of jaundice in an older child is (eg, sickle cell anemia and thalassemia). In these condi-
extensive, encompassing some common conditions and tions, significant hemolysis leads to excess heme produc-
many rare disorders (Table 2). A key practical first step is tion and consequent increased circulating unconjugated
to classify the jaundice as unconjugated (indirect) or bilirubin load.
conjugated (direct) hyperbilirubinemia by using the pre- Gilbert syndrome, an autosomal recessive disorder
viously noted Diazo or Ektachem method. seen in 5% of the population, is another important cause
of unconjugated hyperbilirubinemia in this age group.
Unconjugated Hyperbilirubinemia This inherited disorder of bilirubin metabolism is char-
Older children and adolescents who present with acterized by a mild unconjugated hyperbilirubinemia
jaundice due to unconjugated hyperbilirubinemia are (usually 5 mg/dL [⬍85 mcmol/L]) due to a UGT1
most likely to have a disorder associated with excessive gene mutation that impairs the function of the UDP
hemolysis, such as hereditary spherocytosis, a red blood glucuronosyl transferase enzyme. In affected adolescents
cell enzyme defect of pyruvate kinase or glucose-6- or young adults, jaundice appears most often in associa-
220 Pediatrics in Review Vol.22 No.7 July 2001
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
gastroenterology jaundice in children
tion with an intercurrent mild infectious illness, fasting, aminotransferase (ALT) as well as a conjugated hyperbi-
or physical stress. Other than the modest elevation in lirubinemia. Clinical symptoms and biochemical abnor-
unconjugated bilirubin, patients who have Gilbert syn- malities completely resolve within 4 weeks in most pa-
drome are healthy and have no clinical or laboratory tients. In rare cases, HAV can cause relapsing or
evidence of liver disease or hemolysis. An associated persistent jaundice for months. However, HAV infection
family history, although not always present, is diagnostic never leads to a chronic hepatitis, defined as hepatitis
for the condition. There are no specific diagnostic labo- lasting for more than 6 months. Fulminant HAV infec-
ratory tests. The prognosis is excellent, with no long- tion, heralded by encephalopathy and significant hepatic
term sequelae. dysfunction (ie, coagulopathy), is distinctly unusual, oc-
The Crigler-Najjar syndromes types 1 and 2 are ex- curring in fewer than 1% of cases. Indeed, although viral
tremely rare autosomal recessive diseases that result from or presumed viral hepatitis accounts for 75% to 80% of all
a complete absence (type 1) or limited activity (type 2) of cases of fulminant liver failure in children, most of these
the UDP-glucuronosyl transferase enzyme. Both condi- are the result of non-A through G hepatitis viruses.
tions typically manifest as an unconjugated hyperbiliru- The majority of pediatric patients who have hepatitis
binemia in the first few days of life, although exceptional B virus (HBV) infection are asymptomatic. However,
cases of Crigler-Najjar type 2 presenting at an older age jaundice may occur in acutely infected older children.
have been reported. Without the ability to conjugate The most important routes for acquiring acute HBV
and excrete bilirubin, patients who have type 1 disease infection in adolescence are horizontal—from highly in-
exhibit markedly elevated serum bilirubin levels (25 to fectious family members, from improperly sterilized sy-
35 mg/dL) [425 to 600 mcmol/L]), are at high risk ringes, or when adolescents practice high-risk sexual
to develop kernicterus, and require aggressive photo- behavior with multiple partners and infrequent use of
therapy. In contrast, patients who have type 2 disease condoms. Many older children and adolescents chroni-
usually have total serum bilirubin levels below 20 mg/dL cally infected with HBV are foreign immigrants from
(350 mcmol/L) because of the partially functioning endemic regions who had acquired infection through
UDP-glucuronosyl transferase enzyme, whose activity perinatal transmission. Older children who have chronic
can be induced by phenobarbital. Indeed, the two types HBV infection are often asymptomatic carriers or they
of Crigler-Najjar syndrome may be distinguished by may have a limited, subclinical, biochemical hepatitis,
treatment with phenobarbital. Patients who have type 1 evidenced by increased hepatic transaminase levels. Jaun-
disease show no response; those who have type 2 disease dice is an unusual manifestation in children who have
exhibit a dramatic decrease in serum bili rubin levels chronic HBV infection, except in the rare instance of
following the administration of phenobarbital. fulminant liver failure or end-stage liver disease and
cirrhosis developing at a young age.
Conjugated Hyperbilirubinemia Most children who have hepatitis C virus (HCV)
INFECTIONS infection are older than 8 years of age and have con-
Infection with any of the hepatotropic viruses (A, B, C, tracted the infection through contaminated blood and
D, or E) may cause jaundice in older children and ado- blood products prior to 1992. With improved processing
lescents. In these instances, the jaundice is due to conju- of blood and blood products, the chance of contracting
gated hyperbilirubinemia resulting from intrahepatic HCV through these sources is now low, estimated at 1
cholestasis. Hepatitis A virus (HAV) infection, a self- per 100,000 units transfused. The more important
limited illness induced by an RNA virus, is the most source for pediatric HCV infection is through maternal-
common infectious cause of acute jaundice in this age infant transmission. This indolent disease takes many
group. Young infants rarely develop jaundice when in- decades to progress to end-stage liver disease. Thus, the
fected with HAV. Infants and young children who have vast majority of older children infected with this virus are
HAV infection are usually asymptomatic or simply man- asymptomatic. However, as with chronic HBV infection,
ifest signs and symptoms of viral gastroenteritis without jaundice may manifest in those very rare patients who
icterus. In contrast, older children and adolescents have a have HCV infection and develop cirrhosis at an early age.
prodrome of fever, headache, and general malaise fol- Hepatitis D virus infection is uncommon in the United
lowed by the onset of jaundice, abdominal pain, nausea, States, occurring only in patients already infected with
vomiting, and anorexia. There is biochemical evidence of HBV. Hepatitis E virus is prevalent in developing coun-
a profound hepatitis characterized by significant eleva- tries and typically presents acutely with jaundice, in a
tions in aspartate aminotransferase (AST) and alanine manner similar to HAV infection.
Pediatrics in Review Vol.22 No.7 July 2001 221
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
gastroenterology jaundice in children
Epstein-Barr virus (EBV) infection can cause acute Skeletal manifestations resulting from bone demineral-
hepatitis and jaundice in older children and adolescents ization are not uncommon.
as a part of the infectious mononucleosis syndrome. Any Alpha-1-antitrypsin deficiency, an autosomal codomi-
child or adolescent who presents acutely with jaundice, nantly inherited disease, can present with a conjugated
especially in association with lymphadenopathy, sore hyperbilirubinemia at any age. Approximately 20% of
throat, and mild splenomegaly, should be evaluated for patients who have the ZZ protease inhibitor phenotype
EBV infection. In immunocompromised hosts, infection will have liver disease. Although neonatal cholestasis is a
with herpes simplex virus, cytomegalovirus, or rare op- more common presentation for this disorder, older chil-
portunistic agents can cause hepatobiliary disease with dren may have new-onset jaundice in association with
clinical jaundice, but a discussion of these is beyond the alpha-1-antitrypsin deficiency, chronic hepatitis, or
scope of this article. Jaundice with hepatic dysfunction as cirrhosis.
a result of gram-negative bacterial infections and sepsis is Hepatobiliary disease may occur in up to two thirds of
much more common in infants and young children than patients who have cystic fibrosis. Pancreatic insufficiency
in older children and adolescents. and pulmonary disease used to be the dominant features
of cystic fibrosis, which was associated with high morbid-
METABOLIC LIVER DISEASE ity and mortality at a young age. With improved treat-
A variety of metabolic diseases of the liver may present ments and longer life expectancy, liver disease has as-
with jaundice in older children. Wilson disease is an sumed greater importance, especially for older children
autosomal recessive disorder of copper metabolism, char- and adolescents. The spectrum of hepatobiliary disorders
acterized by excess accumulation of copper in the liver, in cystic fibrosis includes steatohepatitis, focal biliary and
central nervous system (CNS), kidney, cornea, and other multilobular cirrhosis, cholelithiasis and cholecystitis,
organs. The hepatic manifestations are protean, ranging sclerosing cholangitis, and common bile duct stenosis.
from an acute hepatitis to fulminant hepatic failure with Any of these complications may be heralded by a conju-
coagulopathy, ascites, and hepatic encephalopathy or a gated hyperbilirubinemia.
more indolent course with chronic hepatitis and cirrho-
sis. Wilson disease must be considered in the differential BILIARY TRACT DISORDERS
diagnosis of every older child or adolescent who presents Extrahepatic biliary tract disorders may cause an obstruc-
with conjugated hyperbilirubinemia. Neuropsychiatric tive type of jaundice that is manifested by icterus, dark
features may be dramatic, including motor system distur- urine, acholic stools, and pruritus in association with a
bances such as tremor, incoordination, and dysarthria, conjugated hyperbilirubinemia. Cholelithiasis can occur
along with poor school performance, depression, neuro- in older children, albeit infrequently. Gallstones in this
sis, or psychosis. The CNS manifestations may present in age group may be idiopathic or may develop due to
concert with or independent of the hepatic symptoms. hemolytic disorders, cystic fibrosis, obesity, ileal resec-
Kayser-Fleischer (KF) rings, a golden brown discolora- tion, or long-term use of total parenteral nutrition. Al-
tion in the zone of the Descemet membrane of the though many children who have gallstones are asymp-
cornea, is virtually always present when neurologic or tomatic, jaundice, periumbilical or right upper quadrant
psychiatric symptoms develop. However, KF rings may abdominal pain, vomiting, and fever may develop in cases
be absent in patients who have Wilson disease without of acute cholecystitis, choledocholithiasis, or pancreati-
neurologic involvement but who present with hepatic tis. Ultrasonography is the safest, most sensitive, and
symptoms. Renal involvement is characterized by proxi- most specific method of identifying gallstones.
mal tubular dysfunction, decreased glomerular filtration Choledochal cysts are congenital cystic dilatations of
rate, and decreased renal plasma flow. Patients may man- the intrahepatic or extrahepatic biliary ducts. At least five
ifest proteinuria, glucosuria, phosphaturia, uricosuria, subtypes have been described based on the anatomic site
aminoaciduria, renal tubular acidosis, and microscopic of cystic dilation along the biliary tree. Patients may
hematuria. Severe renal insufficiency may occur in pa- present at any age with epigastric pain, fever, and jaun-
tients who have fulminant or end-stage liver disease. dice. The most useful diagnostic study is abdominal
Intravascular hemolysis with a Coombs-negative hemo- ultrasonography. In older children, acute jaundice may
lytic anemia may develop because of the oxidative injury develop in cases of intrahepatic cystic duct lesions that are
to red blood cell membranes induced by excess copper. associated with congenital hepatic fibrosis and autosomal
Cardiac involvement, including ventricular hypertrophy recessive polycystic kidney disease.
and arrhythmias, has been reported in Wilson disease. Primary sclerosing cholangitis is a chronic fibro-
222 Pediatrics in Review Vol.22 No.7 July 2001
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
gastroenterology jaundice in children
obliterative disease of unknown etiology that involves can cause jaundice include erythromycin, sulfonamides,
the extrahepatic and intrahepatic bile ducts. In older halothane, methotrexate, chemotherapy, anticonvul-
children, this condition occurs most often in association sants such as valproate and phenytoin, the antitubercu-
with inflammatory bowel disease, although it may lous drug isoniazid, and oral contraceptives.
present rarely in otherwise healthy teenagers or in pa-
tients who have congenital or acquired immunodefi- VASCULAR DISEASES
ciency. Clinical features include jaundice, anorexia, fa- Vascular diseases of the liver may present with jaundice in
tigue, abdominal pain, and pruritus. The diagnosis is older children. Veno-occlusive disease causing hepatic
confirmed by cholangiography that shows a characteris- congestion and jaundice may be seen in children in the
tic beading and stenosis of the common or intrahepatic first few weeks following bone marrow transplantation.
bile ducts in the absence of choledocholithiasis.
Clinical Evaluation
AUTOIMMUNE HEPATITIS Distinguishing between conjugated and unconjugated
Autoimmune hepatitis is a chronic progressive inflamma- hyperbilirubinemia is a most important first step in diag-
tory liver disease of unknown etiology. Two major sub- nosis. Whereas the presence of dark urine, pale stools,
types have been identified based on circulating autoanti- or pruritus in a jaundiced patient suggests hepatobiliary
bodies. Type 1 disease, defined by the presence of anti- disease with a conjugated hyperbilirubinemia, the ab-
smooth muscle antibodies (ASMAs) and antinuclear sence of these symptoms does not specify the underlying
type of jaundice, and laboratory
studies are required. If the jaun-
dice is associated with abdominal
. . . the acute onset of jaundice in any pain, it is important to document
the nature, site, and severity of the
child may be an initial clinical manifestation pain. Cholecystitis or chole-
of previously unrecognized chronic liver docholithiasis due to gallstone
disease. disease usually presents with se-
vere epigastric or right upper
quadrant pain, often accompanied
by vomiting. For acute viral hepa-
antibodies (ANAs), typically presents in adolescent fe- titis, the abdominal pain characteristically is a dull ache in
males as an acute hepatitis with symptoms of malaise, the right upper quadrant. Personality changes, inappro-
nausea, anorexia, fatigue, abdominal pain, and jaundice. priate behavior, and disturbed sleep-wake cycle or wors-
Type 2 autoimmune liver disease, associated with the ening school performance in a child who has jaundice
liver-kidney microsomal antibody, is a more rapidly pro- may indicate hepatic encephalopathy, suggesting fulmi-
gressive form that usually presents with similar symptoms nant hepatitis, or may represent features of the CNS
in younger children and infants. complications of Wilson disease.
In reviewing the past history, it is important to inquire
HEPATOTOXINS about risk factors for viral hepatitis, such as maternal-
A variety of drugs or environmental agents may be hep- infant transmission, transfusion of contaminated blood
atotoxic and cause jaundice in older children and adoles- products, intravenous drug abuse, high-risk sexual activ-
cents. Acetaminophen overdose is a leading cause of ity, travel history, or a history of infectious contacts.
fulminant hepatic failure in these age groups. Hepato- A detailed review of all medications is essential to search
toxicity develops in the face of glutathione depletion, for potential hepatotoxic agents, especially acetamino-
after which any excess acetaminophen is metabolized phen abuse or misuse. Consanguinity or a family history
by the hepatic P450 pathway to produce the hepato- for jaundice may suggest inherited metabolic conditions
toxic product NAPQI (N-acetyl-p-benzoquinoneimine). such as Wilson disease, alpha-1-antitrypsin deficiency,
A distinct clinical course ensues, with initial nausea and cystic fibrosis, or Gilbert syndrome.
vomiting, followed progressively by a quiescent period The physical examination should focus on signs of
and acute liver dysfunction with jaundice and coagulopa- chronic liver disease; the acute onset of jaundice in any
thy. Hepatic failure may develop with progressive en- child may be an initial clinical manifestation of previously
cephalopathy and coma. Other hepatotoxic agents that unrecognized chronic liver disease. Pallor may suggest an
Pediatrics in Review Vol.22 No.7 July 2001 223
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
gastroenterology jaundice in children
acute hemolytic anemia or chronic liver disease. Malnu-
trition, palmar erythema, and spider nevi on the chest or Laboratory Evaluation of
Table 3.
upper extremities suggest chronic liver disease. General-
ized lymphadenopathy and pharyngitis point to an EBV
Hyperbilirubinemia in Older
infection. The finding of KF rings on opthalmologic Children
slitlamp examination suggests Wilson disease. The liver
must be carefully palpated and percussed to assess its Unconjugated Hyperbilirubinemia
texture and measure its size and span. The normal liver ● Complete blood count
● Reticulocyte count
span is approximately 9 to 12 cm in early adolescence.
● Blood smear
A nodular hard surface or a shrunken liver suggests ● Serum haptoglobins
cirrhosis. Sharp-edged, tender hepatomegaly typifies ● Direct and indirect Coombs test
acute hepatitis. Splenomegaly may be present because of ● Hemoglobin electrophoresis
a hemolytic disease or acute EBV infection or it may be ● Red cell enzyme assay
● Test for spherocytosis
the singular sign for chronic liver disease with cirrhosis
and portal hypertension. Abdominal distension or shift- Conjugated Hyperbilirubinemia
ing dullness on percussion in the flanks may indicate ● Liver function tests (AST, ALT, ALP, and GGT)
ascites formation. Neurologic abnormalities, includ- ● Synthetic liver function (prothrombin time, total
ing confusion and delirium, asterixis, hyperreflexia, or protein, albumin, glucose, cholesterol, ammonia)
decorticate or decerebrate posturing, are all features of ● Abdominal ultrasonography
● HAV IgM, HBsAg, IgM-antiHBcore, antiHCV,
hepatic encephalopathy. Early onset of encephalopathy Monospot姞/EBV titers
in a patient who has newly diagnosed liver disease defines ● Serum ceruloplasmin, 24-hour urinary copper
fulminant liver failure and portends a poor prognosis. excretion
● Serum IgG, autoantibodies (ANA, ASMA, anti-liver-
Laboratory Evaluation and Diagnosis kidney-microsomal antibody)
● Serum alpha-1-antitrypsin level and phenotype
Bilirubin fractionation by the Ektachem or Diazo ● Liver biopsy
method is a necessary first step in the laboratory evalua-
tion of any older child or adolescent who has jaundice
(Table 3). Unconjugated hyperbilirubinemia in this age albumin. Of these, the most sensitive test for synthetic
group is due most often to hemolytic disease. A complete liver function is the PT. Prolongation of the PT despite
blood count, reticulocyte count, direct and indirect administration of vitamin K suggests significant hepatic
Coombs tests, measurement of serum haptoglobins, and dysfunction. Patients who have acute hepatitis and a
hemoglobin electrophoresis should be requested. Excep- marked coagulopathy that is not responsive to vitamin K
tionally, a Coombs-negative hemolytic anemia may be or who manifest other “worrisome signs” (Table 4)
the sole presenting feature of Wilson disease. In the should be referred promptly to a center that has expertise
absence of hemolysis or elevated liver enzyme levels, in the management of children who have advanced liver
Gilbert syndrome should be considered in the adolescent disease and where liver transplantation is readily avail-
who has mild unconjugated hyperbilirubinemia. able. For these more urgent cases, intensive supportive
Conjugated hyperbilirubinemia suggests hepatobili- care and liver transplantation hold the greatest potential
ary disease. The initial laboratory investigations should for survival.
include a complete blood count, liver function tests Further laboratory investigations are directed toward
(AST, ALT, alkaline phosphatase [ALP], gamma- establishing a diagnosis. Every patient who presents with
glutamyltransferase [GGT]), total protein, serum albu- conjugated hyperbilirubinemia should undergo abdom-
min, and a prothrombin time (PT). Although there is inal ultrasonography to examine the hepatic architecture
considerable overlap, predominant elevation of the AST and to exclude biliary tract disease. Screening for the viral
and ALT suggests hepatocellular injury, and a prevailing hepatitides should include serology for hepatitis A im-
elevation in the ALP and GGT suggests biliary tract munoglobulin M (IgM), hepatitis B surface antigen,
disease. It is important to remember that the so-called IgM antibody to hepatitis B core antigen, and anti-HCV.
“liver function tests” are a misnomer; they do not reveal A Monospot威 test or serology for EBV is also highly
anything about the synthetic function of the liver. Tests recommended for the adolescent who presents with con-
for liver function include a coagulation screen and mea- jugated hyperbilirubinemia. Measurement of serum
surements of serum glucose, cholesterol, ammonia, and alpha-1-antitrypsin levels and protease inhibitor pheno-
224 Pediatrics in Review Vol.22 No.7 July 2001
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
gastroenterology jaundice in children
each individual disease state is beyond the scope of this
“Worrisome” Signs and
Table 4. article. In general, acute hemolytic crises require hyper-
hydration and close monitoring of renal function. Immu-
Symptoms in the Jaundiced nosuppressive agents, such as prednisone, azathioprine,
Older Child or Adolescent who or cyclosporine, are used to treat autoimmune hepatitis.
has Acute Hepatitis Penicillamine is the drug of choice for Wilson disease,
although zinc replacement and trientine also have been
● Onset of hepatic encephalopathy prescribed. N-acetyl-cysteine is recommended for the
● Vitamin K-resistant prolongation of the prothrombin treatment of acetaminophen overdose. Patients who
time have acute viral hepatitis, especially hepatitis A, are prone
● Cerebral edema
to dehydration and require adequate fluid support.
● Serum bilirubin 18 mg/dL (>300 mcmol/L)
● Rising serum bilirubin with decreasing ALT/AST Passive immunoprophylaxis should be administered to
● Rising serum creatinine all close family contacts of patients who have acute
● Hypoglycemia hepatitis A.
● Sepsis Any child who has conjugated hyperbilirubinemia and
● Ascites
encephalopathy or biochemical features of hepatic syn-
● pH<7.3 in acetaminophen overdose
thetic dysfunction, best evidenced by a prolonged PT, is
at high risk to develop a more fulminant course that has
typing should be requested to exclude alpha-1- a fatal outcome. Close supervision and intensive support-
antitrypsin deficiency. Patients who have autoimmune ive care are required, preferably by physicians who have
hepatitis, jaundice, and an elevated ALT usually exhibit expertise in the management of advanced pediatric liver
a high serum total protein relative to the albumin, re- disease.
flecting an increased globulin fraction. This is a result of
the significant hypergammaglobulinemia often found Summary
in association with autoimmune hepatitis. Aside from The spectrum of diseases causing jaundice in older chil-
measuring the serum IgG, other tests for autoimmune dren and adolescents differs from that in the neonate and
hepatitis should include an ANA, ASMA, and anti-liver- young infant. A sound knowledge of the differential
kidney-microsomal antibody. A liver biopsy is recom- diagnosis of unconjugated and conjugated hyperbiliru-
mended to confirm the diagnosis. binemia in this age group provides the framework for a
Serum ceruloplasmin is a valuable screening test for sensible approach to the clinical evaluation and labora-
Wilson disease. A decreased serum ceruloplasmin level is tory investigation of these children. For patients who
found in up to 80% of affected patients. Another useful have acute hepatitis, a careful assessment of liver function
diagnostic test is the 24-hour urinary copper excretion. is of critical importance. Signs and symptoms of liver
In Wilson disease, the urinary copper excretion is typi- dysfunction in a jaundiced patient should prompt an
cally greater than 100 mcg/24 h. Serum copper levels are immediate referral to a tertiary center where expertise in
not helpful in diagnosing Wilson disease except for those the management of pediatric liver disease and hepatic
rare patients presenting with fulminant liver failure, in transplantation is readily available.
whom serum copper levels are significantly elevated.
Other laboratory abnormalities often seen in Wilson
disease include a low serum ALP, particularly when ful- Suggested Reading
minant hepatic failure is present, and low serum phos- D’Agata ID, Balistreri WF. Evaluation of liver disease in the pedi-
atric patient. Pediatr Rev. 1999;20:376 –389
phate and uric acid due to the associated Fanconi syn-
Gourley GR. Disorders of bilirubin metabolism. In: Suchy F, ed.
drome. Quantification of hepatic copper concentration Liver Disease in Children. St. Louis, Mo: Mosby; 1994:
in a liver biopsy tissue specimen (⬎250 mcg/g of dry 401– 413
weight liver) remains the gold standard for diagnosing Jonas M. Viral hepatitis. In: Walker WA, Durie PR, Hamilton JR,
Wilson disease. Walker-Smith JA, Watkins JB, eds. Pediatric Gastrointestinal
Disease. St. Louis, Mo: Mosby; 1996:1028 –1051
Mews C, Sinatra F. Chronic liver disease in children. Pediatr Rev.
Treatment 1993;14:436 – 443
Specific treatment of the hyperbilirubinemia depends on Roberts EA, Cox DW. Wilson disease. Baillieres Clin Gastroenterol.
the precise etiology. A detailed discussion of therapy for 1998:12:237–256
Pediatrics in Review Vol.22 No.7 July 2001 225
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
gastroenterology jaundice in children
PIR Quiz
Quiz also available online at www.pedsinreview.org.
1. You are seeing a 13-year-old girl who has acute onset of jaundice. She previously has been healthy, but
had a mild viral illness 1 week ago. She appears well and has mild scleral icterus. Laboratory testing reveals
a total bilirubin of 4 mg/dL (68.4 mcmol/L) that is all unconjugated. There is no evidence of hemolysis on a
peripheral smear. Which of the following is the most likely diagnosis?
A. Autoimmune hepatitis.
B. Crigler-Najjar syndrome.
C. Gilbert syndrome.
D. Hepatitis A.
E. Wilson disease.
2. A 10-year-old boy comes to your office with a 4-day history of abdominal pain, nausea, and jaundice.
He appears mildly ill and is notably jaundiced. His laboratory values are as follows: conjugated bilirubin,
10.5 mg/dL (179.6 mcmol/L); aspartate aminotransferase, 800 U/L; and alanine aminotransferase, 950 U/L.
Which of the following is the most likely diagnosis?
A. Alpha-1-antitrypsin deficiency.
B. Cholelithiasis.
C. Epstein-Barr virus infection.
D. Hepatitis A.
E. Hepatitis B.
3. Which of the following statements about Wilson disease in adolescents is true?
A. Central nervous system symptoms are always present with hepatic insufficiency.
B. Elevated serum copper levels are pathognomonic of the disease.
C. Kayser-Fleischer rings are almost always present with neurologic involvement.
D. Patients typically are asymptomatic at the time of diagnosis.
E. The gold standard for diagnosis is an elevated ceruloplasmin level.
4. Which of the following laboratory tests is the most sensitive indicator of liver function?
A. Alanine aminotransferase.
B. Albumin.
C. Alkaline phosphatase.
D. Prothrombin time.
E. Total bilirubin level.
5. You are evaluating a 15-year-old patient who has had a 2-week history of worsening jaundice. She shows
signs of depression. You are concerned about the possibility of fulminant liver failure. Which of the
following is most likely to prompt you to refer her to a liver transplant center immediately?
A. Increasing conjugated bilirubin and liver enzyme levels.
B. Persistently elevated prothrombin time despite administration of vitamin K.
C. Presence of ascites.
D. Presence of splenomegaly.
E. Rising levels of ammonia.
226 Pediatrics in Review Vol.22 No.7 July 2001
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
Jaundice in Older Children and Adolescents
Dinesh Pashankar and Richard A. Schreiber
Pediatrics in Review 2001;22;219
DOI: 10.1542/pir.22-7-219
Updated Information & including high resolution figures, can be found at:
Services http://pedsinreview.aappublications.org/content/22/7/219
Supplementary Material Supplementary material can be found at:
http://pedsinreview.aappublications.org/content/suppl/2001/06/27/22.
7.219.DC1
http://pedsinreview.aappublications.org/content/suppl/2005/01/27/22.
7.219.DC2
References This article cites 3 articles, 2 of which you can access for free at:
http://pedsinreview.aappublications.org/content/22/7/219.full#ref-list
-1
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Fetus/Newborn Infant
http://classic.pedsinreview.aappublications.org/cgi/collection/fetus:n
ewborn_infant_sub
Hyperbilirubinemia
http://classic.pedsinreview.aappublications.org/cgi/collection/hyperbi
lirubinemia_sub
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
https://shop.aap.org/licensing-permissions/
Reprints Information about ordering reprints can be found online:
http://classic.pedsinreview.aappublications.org/content/reprints
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
Jaundice in Older Children and Adolescents
Dinesh Pashankar and Richard A. Schreiber
Pediatrics in Review 2001;22;219
DOI: 10.1542/pir.22-7-219
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pedsinreview.aappublications.org/content/22/7/219
Pediatrics in Review is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1979. Pediatrics in Review is owned,
published, and trademarked by the American Academy of Pediatrics, 345 Park Avenue, Itasca,
Illinois, 60143. Copyright © 2001 by the American Academy of Pediatrics. All rights reserved.
Print ISSN: 0191-9601.
Downloaded from http://pedsinreview.aappublications.org/ by 1476414 on May 11, 2019
You might also like
- Jaundice: in Older Children and AdolescentsDocument10 pagesJaundice: in Older Children and AdolescentsjoslinmtggmailcomNo ratings yet
- Jaundice in The Adult PatientDocument6 pagesJaundice in The Adult Patientrbatjun576No ratings yet
- Jaundice Newborn - 2Document15 pagesJaundice Newborn - 2Miratunnisa AzzahrahNo ratings yet
- Jaundice: Newborn To Age 2 Months: Education GapDocument14 pagesJaundice: Newborn To Age 2 Months: Education GapRaul VillacresNo ratings yet
- Liver DiseasesDocument10 pagesLiver DiseasesDaniel HikaNo ratings yet
- Conjugated Hyperbilirubinemia:: Screening and Treatment in Older Infants and ChildrenDocument11 pagesConjugated Hyperbilirubinemia:: Screening and Treatment in Older Infants and ChildrendjebrutNo ratings yet
- Neonatal Indirect HyperbilirubinemiaDocument14 pagesNeonatal Indirect HyperbilirubinemiaValen CadenaNo ratings yet
- Hiperbilirrubinemia DirectaDocument9 pagesHiperbilirrubinemia DirectaRonal Cadillo MedinaNo ratings yet
- Evaluation of Jaundice in Adults: Patient InformationDocument5 pagesEvaluation of Jaundice in Adults: Patient InformationCarlos CalvacheNo ratings yet
- Clase 3 HepatogramaDocument9 pagesClase 3 HepatogramajuanpbagurNo ratings yet
- Pediatrics in Review33 (7) 291Document14 pagesPediatrics in Review33 (7) 291Barbara Helen Stanley100% (1)
- Neonatal Jaundice: Aetiology, Diagnosis and Treatment: Current Issues in Neonatal CareDocument6 pagesNeonatal Jaundice: Aetiology, Diagnosis and Treatment: Current Issues in Neonatal CareLaila AzizahNo ratings yet
- Jaundice Clinical Manifestation and Pathophysiology A Review ArticleDocument3 pagesJaundice Clinical Manifestation and Pathophysiology A Review ArticleHany ZutanNo ratings yet
- Neonatal JaundiceDocument48 pagesNeonatal JaundiceRemy MartinsNo ratings yet
- Research ProposalDocument5 pagesResearch ProposalZablon KodilaNo ratings yet
- Core Concepts Bilirrubin MetabolismDocument9 pagesCore Concepts Bilirrubin MetabolismAngelina ChunNo ratings yet
- Neonatal Jaundice Bilirubin Physiology and ClinicaDocument13 pagesNeonatal Jaundice Bilirubin Physiology and ClinicaNURUL NADIA BINTI MOHD NAZIR / UPMNo ratings yet
- Nej M 200102223440807Document10 pagesNej M 200102223440807fajriNo ratings yet
- Health Education On NEONATAL JAUNDICEDocument23 pagesHealth Education On NEONATAL JAUNDICEAsha jilu100% (2)
- Daftar-IsiDocument2 pagesDaftar-Isi'RahmaT' ANdesjer Lcgs CuyyNo ratings yet
- HyperbilirubinemiaDocument48 pagesHyperbilirubinemiaEdrik Luke Pialago100% (2)
- 1 Core Concepts Bilirubin MetabolismDocument9 pages1 Core Concepts Bilirubin Metabolismlink0105No ratings yet
- Neonatal JaundiceDocument4 pagesNeonatal JaundiceChristian Eduard de DiosNo ratings yet
- Neonatal Jaundice Cme 3Document56 pagesNeonatal Jaundice Cme 3Arief NorddinNo ratings yet
- Newborn Jaundice Guide: Causes, Symptoms and TreatmentDocument5 pagesNewborn Jaundice Guide: Causes, Symptoms and TreatmentArinaManaSikanaNo ratings yet
- Monorafia SP BryanDocument45 pagesMonorafia SP BryanBryan SanchezNo ratings yet
- Neonatal Anemia: Revisiting The Enigmatic PyknocyteDocument5 pagesNeonatal Anemia: Revisiting The Enigmatic PyknocyteDavid MerchánNo ratings yet
- Jaundice - StatPearls - NCBI BookshelfDocument11 pagesJaundice - StatPearls - NCBI BookshelfCONSTANTIUS AUGUSTONo ratings yet
- Managing Breast Milk JaundiceDocument7 pagesManaging Breast Milk JaundiceJéssica MorenoNo ratings yet
- Liver Chemistry and Function Tests: Daniel S. PrattDocument11 pagesLiver Chemistry and Function Tests: Daniel S. PrattAnişoara FrunzeNo ratings yet
- Final Jaundice1Document43 pagesFinal Jaundice1ahmad solehinNo ratings yet
- Neonatal Hyperbilirubinemia: Mahlet Abayneh Assistant Professor of PediatricsDocument41 pagesNeonatal Hyperbilirubinemia: Mahlet Abayneh Assistant Professor of PediatricsBegashawNo ratings yet
- Applied Physiology of Bilirubin MetabolismDocument6 pagesApplied Physiology of Bilirubin MetabolismRenata SetyariantikaNo ratings yet
- Oj 2 PDFDocument6 pagesOj 2 PDFAnisah Maryam DianahNo ratings yet
- Neonatal Hyperbilirubinemia and JaundiceDocument8 pagesNeonatal Hyperbilirubinemia and JaundiceAndreea GeorgianaNo ratings yet
- PathologyDocument19 pagesPathologyAfrin AkhtarNo ratings yet
- Assessment of jaundice causes and evaluationDocument16 pagesAssessment of jaundice causes and evaluationlaura canoNo ratings yet
- Pediatrics - Neonatal Jaundice PDFDocument2 pagesPediatrics - Neonatal Jaundice PDFJasmine KangNo ratings yet
- Bac GroundDocument6 pagesBac GroundRitu Ayu PutriNo ratings yet
- Neonatal Jaundice: Understanding and Preventing KernicterusDocument12 pagesNeonatal Jaundice: Understanding and Preventing Kernicterusn_akash3977No ratings yet
- Core Concepts:: Bilirubin MetabolismDocument9 pagesCore Concepts:: Bilirubin MetabolismManasye AlanNo ratings yet
- TAYLOR 1984 AnaesthesiaDocument3 pagesTAYLOR 1984 Anaesthesiapolly91No ratings yet
- Peadiatrics Assignment - Mr. KangwaDocument11 pagesPeadiatrics Assignment - Mr. KangwaTahpehs PhiriNo ratings yet
- Neonatal Jaundice 2023Document31 pagesNeonatal Jaundice 2023Demelash SolomonNo ratings yet
- PPPPDocument6 pagesPPPPChristy Ada IjeomaNo ratings yet
- HyperbilirubinemiaDocument10 pagesHyperbilirubinemiachiboogs456100% (1)
- J Mpsur 2017 09 012Document7 pagesJ Mpsur 2017 09 012riffarsyad100% (1)
- Jaundice and Ascites Group ProjectDocument15 pagesJaundice and Ascites Group ProjectJosiah Noella BrizNo ratings yet
- Jaundice 160318164012Document47 pagesJaundice 160318164012Ritik MishraNo ratings yet
- Understanding and Managing Breast Milk JaundiceDocument7 pagesUnderstanding and Managing Breast Milk JaundiceJulian RiveraNo ratings yet
- Hyperbilirubinemia: West Visayas State University College of Medicine Neonatal Intensive Care UnitDocument49 pagesHyperbilirubinemia: West Visayas State University College of Medicine Neonatal Intensive Care UnitDonna LabaniegoNo ratings yet
- Neonatal Jaundice: Bilirubin MetabolismDocument2 pagesNeonatal Jaundice: Bilirubin MetabolismghsNo ratings yet
- 73 Liver Chemistry and Function TestsDocument11 pages73 Liver Chemistry and Function TestsPaola PizanoNo ratings yet
- IctericiaDocument19 pagesIctericiadavid pinedaNo ratings yet
- T15 - Neonatal JaundiceDocument38 pagesT15 - Neonatal JaundiceMawuliNo ratings yet
- ) Jaundice PDFDocument4 pages) Jaundice PDFAzzNo ratings yet
- 10 NNJ 1Document22 pages10 NNJ 1ahmed shorshNo ratings yet
- Nelson JaundiceDocument7 pagesNelson JaundiceJesly CharliesNo ratings yet
- Liver Disorders in Childhood: Postgraduate Paediatrics SeriesFrom EverandLiver Disorders in Childhood: Postgraduate Paediatrics SeriesNo ratings yet
- Metabolism With Triphasic Oral Contraceptive Formulations Containing Norgestimate or LevonorgestrelDocument6 pagesMetabolism With Triphasic Oral Contraceptive Formulations Containing Norgestimate or LevonorgestrelhectorNo ratings yet
- English LessonDocument2 pagesEnglish LessonhectorNo ratings yet
- Comprehensive Medical Education PodcastsDocument25 pagesComprehensive Medical Education PodcastshectorNo ratings yet
- Endocrinology In-Training ObjectivesDocument12 pagesEndocrinology In-Training ObjectiveshectorNo ratings yet
- Sample Diabetic Ketoacidosis (Dka) Clinical Order Set: AdultDocument2 pagesSample Diabetic Ketoacidosis (Dka) Clinical Order Set: AdulthectorNo ratings yet
- U.S. Contraceptive Use Recommendations 2016Document60 pagesU.S. Contraceptive Use Recommendations 2016hectorNo ratings yet
- A Comparative Analysis of Three Methods of Contraception: Effects On Blood Glucose and Serum Lipid ProfilesDocument4 pagesA Comparative Analysis of Three Methods of Contraception: Effects On Blood Glucose and Serum Lipid ProfileshectorNo ratings yet
- Blood Pressure Log 02Document1 pageBlood Pressure Log 02hectorNo ratings yet
- 60 Affirmations For PeaceDocument21 pages60 Affirmations For PeacehectorNo ratings yet
- Example Abstract ItemDocument2 pagesExample Abstract ItemhectorNo ratings yet
- Glasgow Coma Scale (With Explanations)Document1 pageGlasgow Coma Scale (With Explanations)hectorNo ratings yet
- Gauthier 1992Document6 pagesGauthier 1992hectorNo ratings yet
- Clinical Reasoning Guide FormDocument3 pagesClinical Reasoning Guide FormhectorNo ratings yet
- Mental Status ExamDocument4 pagesMental Status Examscootaccess100% (1)
- Internal Medicine Progress Note TemplateDocument2 pagesInternal Medicine Progress Note Templatehector100% (1)
- ACGMECLERNational Report Findings 2019Document132 pagesACGMECLERNational Report Findings 2019hectorNo ratings yet
- Paradigm Shift - Gratitude PadDocument1 pageParadigm Shift - Gratitude PadElmer GarchitorenaNo ratings yet
- GYN History Physical PDFDocument2 pagesGYN History Physical PDFMariam A. KarimNo ratings yet
- Assignments Report - Surgery ProgramsDocument16 pagesAssignments Report - Surgery ProgramshectorNo ratings yet
- Step 2 Clinical Knowledge (CK) : Content Description and General InformationDocument12 pagesStep 2 Clinical Knowledge (CK) : Content Description and General InformationAleezay ZaharaNo ratings yet
- AOAStudy 2018Document26 pagesAOAStudy 2018Gerardo Lerma100% (1)
- Soapwhat To WriteDocument1 pageSoapwhat To WriteJoriza TamayoNo ratings yet
- Leadership PlenaryDocument1 pageLeadership PlenaryhectorNo ratings yet
- SketchyIM Check List PDFDocument5 pagesSketchyIM Check List PDFhectorNo ratings yet
- Example Note 1Document2 pagesExample Note 1naimNo ratings yet
- Serenity Tri-Fold PDFDocument2 pagesSerenity Tri-Fold PDFFynneganNo ratings yet
- NBME Subject Exam Content Outlines and Sample ItemsDocument144 pagesNBME Subject Exam Content Outlines and Sample ItemshectorNo ratings yet
- CS Blue Sheet Mnemonics - USMLE Step 2 CS - WWW - MedicalDocument1 pageCS Blue Sheet Mnemonics - USMLE Step 2 CS - WWW - MedicalRavi Parhar75% (4)
- The AOA Guide:: How To Succeed in The Third-Year ClerkshipsDocument25 pagesThe AOA Guide:: How To Succeed in The Third-Year Clerkshipshector100% (1)
- Primer2ndEd PDFDocument37 pagesPrimer2ndEd PDFhectorNo ratings yet
- ECHO MASTERCLASS: A GUIDE TO ACCURATELY ASSESSING HEART VALVE DISEASEDocument136 pagesECHO MASTERCLASS: A GUIDE TO ACCURATELY ASSESSING HEART VALVE DISEASEVladlena Cucoș-CaraimanNo ratings yet
- Introduction to Public Health NursingDocument37 pagesIntroduction to Public Health NursingKailash NagarNo ratings yet
- Stool Exam Guide - Key Tests, Colors, Consistencies in 40 CharactersDocument8 pagesStool Exam Guide - Key Tests, Colors, Consistencies in 40 CharactersLester John HilarioNo ratings yet
- Vegetable Kingdom Continued: SciaticDocument14 pagesVegetable Kingdom Continued: SciaticSatyendra RawatNo ratings yet
- Thyroid DiseasesDocument44 pagesThyroid DiseasesPLDT HOMENo ratings yet
- Osteoporosis Clinical Case by SlidesgoDocument30 pagesOsteoporosis Clinical Case by SlidesgoHussein Al-jmrawiNo ratings yet
- General Stress Level of SHS ABM Students in Their Specialized SubjectDocument4 pagesGeneral Stress Level of SHS ABM Students in Their Specialized SubjectThons Nacu LisingNo ratings yet
- Philippine College of Physicians Daily Census Ward Hospital de Los Santos-Sti Medical CenterDocument22 pagesPhilippine College of Physicians Daily Census Ward Hospital de Los Santos-Sti Medical Centercruz_johnraymondNo ratings yet
- HematologyDocument6 pagesHematologyRian CopperNo ratings yet
- Antenatal CareDocument12 pagesAntenatal CarefiramnNo ratings yet
- PhenobarbitalDocument2 pagesPhenobarbitalhahahahaaaaaaaNo ratings yet
- CV Abdul HafeezDocument7 pagesCV Abdul HafeezAbdul Hafeez KandhroNo ratings yet
- Test Bank For Pharmacology For Nurses A Pathophysiologic Approach 5th EditionDocument36 pagesTest Bank For Pharmacology For Nurses A Pathophysiologic Approach 5th Editiontipsterchegoe.t8rlzv100% (41)
- Questions from the Ministry of Health for Residency and Fellowship Programs (2013-2018Document68 pagesQuestions from the Ministry of Health for Residency and Fellowship Programs (2013-2018Ahmad HamdanNo ratings yet
- Daftar Harga Ethical Per April'22 (Khus Riau)Document8 pagesDaftar Harga Ethical Per April'22 (Khus Riau)iraNo ratings yet
- Guide For History Taking, Physical Exam and Diagnosis of Pediatric PatientsDocument19 pagesGuide For History Taking, Physical Exam and Diagnosis of Pediatric PatientsKendall Marie BuenavistaNo ratings yet
- Evaluating The Airway for Difficult Intubation (LEMON MethodDocument7 pagesEvaluating The Airway for Difficult Intubation (LEMON Methodtri-edge 8No ratings yet
- The Heart, Part 1 - Under Pressure: Crash Course A&P # 25Document5 pagesThe Heart, Part 1 - Under Pressure: Crash Course A&P # 25Jordan TorresNo ratings yet
- Prevalence of Cardiovascular Risk Factors in Two Brazilian Quilombola Communities in Southwest Bahia StateDocument7 pagesPrevalence of Cardiovascular Risk Factors in Two Brazilian Quilombola Communities in Southwest Bahia StateIJAERS JOURNALNo ratings yet
- Movement Disorders Types - Mayo ClinicDocument1 pageMovement Disorders Types - Mayo ClinicdrrajmptnNo ratings yet
- Cues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationDocument3 pagesCues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationVher SisonNo ratings yet
- Tracheo-Oesophageal FistulaDocument23 pagesTracheo-Oesophageal FistulaAhmad KhanNo ratings yet
- EMR Implementation Readiness Assessment and Patient Satisfaction ReportDocument20 pagesEMR Implementation Readiness Assessment and Patient Satisfaction ReportAbidi HichemNo ratings yet
- Pathologt of The HeartDocument40 pagesPathologt of The HeartJudithNo ratings yet
- Benign Prostatic Hyperplasia - BPH - Pathophysiology - Schematic DiagramDocument2 pagesBenign Prostatic Hyperplasia - BPH - Pathophysiology - Schematic DiagramSimran JosanNo ratings yet
- Free Modern Neuromuscular Techniques PDFDocument6 pagesFree Modern Neuromuscular Techniques PDFStiven FloresNo ratings yet
- Food Poisoning and IntoxicationsDocument26 pagesFood Poisoning and IntoxicationslakshmijayasriNo ratings yet
- PREBORD NLE8part1Document671 pagesPREBORD NLE8part1Bryan NorwayneNo ratings yet
- REBOZETDocument28 pagesREBOZETAndronikus DharmawanNo ratings yet
- L5 - Nature of Clinical Lab - PMLS1Document98 pagesL5 - Nature of Clinical Lab - PMLS1John Daniel AriasNo ratings yet