Professional Documents
Culture Documents
Urine Reagent Strips Package Insert
Uploaded by
geraldineCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Urine Reagent Strips Package Insert
Uploaded by
geraldineCopyright:
Available Formats
results should be interpreted qualitatively. For yellow-green for negative results and green to within manufacturing tolerances.
within manufacturing tolerances. The following
semi-quantitative results, read at 30 seconds green-blue for positive results. 1-14 mg/dL of table below indicates read times and performance
only. protein may be excreted by a normal kidney.9 A characteristics fo r each parameter:
Ketone: This test is based on ketones reacting color matching any block greater than trace
with nitroprusside and acetoacetic acid to indicates significant proteinuria. For urine with REAGENTS AND PERFORMANCE CHARACTERISTICS
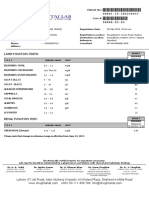
produce a color change ranging from light pink high specific gravity, the test area may most Read
Reagent Composition Description
Urine Reagent Strips for negative results to a darker pink or purple closely match the trace color block even though Time
(11 Parameters ) color for positive results. Ketones are normally only normal concentrations of protein are 1.5% w/w Detects glucose as
not present in urine. Detectable ketone levels present. Clinical judgment is required to evaluate glucose oxidase; low as
may occur in urine during physiological stress the significance of trace results. 0.5% w/w 25-50 mg/dL
For rapid detection of multiple analytes in conditions such as fasting, pregnancy and Urobilinogen: This test is based on a modified peroxidase; (1.4~2.8 mmol/L).
human urine. frequent strenuous exercise. In starvation diets, Ehrlich reaction between
Glucose 30
10.0% w/w Results may be
or in other abnormal carbohydrate metabolism p-diethylaminobenzaldehyde and urobobilinogen potassium read at 20 seconds
For in vitro diagnostic use only (GLU) seconds
situations, ketones appear in the urine in acid in strongly acidic medium to produce a pink iodide . 75.0% for qualitative
excessively high concentration before serum color. Urobilinogen is one of the major w/w buffer; results or at 45
Store at 15-30C ketones are elevated. compounds produced in heme synthesis and is a 13.0% w/w seconds for
INTENDED USE Bilirubin: This test is based on azo-coupling normal substance in urine. The expected range non-reactive semi-quantitative
Urine Reagent Strips are firm plastic strips onto which several reaction of bilirubin with diazotized for normal urine with this test is 0.2-1.0 mg/dL ingredients results.
separate reagent areas are affixed. The test is for the dichloroaniline in a strongly acidic medium. (3.5-17 mol/L). A result of 2.0 mg/dL (35 mol/L) Detects acetoacetic
detection of one or more of the following analytes in urine: 5% w/w sodium
Varying bilirubin levels will produce a pinkish-tan may be of clinical significance, and the patient Ketone 40 acid as low as
Leukocytes, Glucose, Ketone (Acetoacetic acid), Bilirubin, nitroprusside;
color proportional to its concentration in urine. specimen should be further evaluated. (KET) seconds 2.5-5 mg/dL
Blood, Specific Gravity, Protein, Urobilinogen, Nitrite, 95% w/w buffer
In normal urine, no bilirubin is detectable by Nitrite: This test depends upon the conversion of (0.25-0.5 mmol/L).
Ascorbic Acid, and pH. even the most sensitive methods. Even trace nitrate to nitrite by the action of Gram negative 0.5 % w/w 2,
amounts of bilirubin require further investigation. bacteria in the urine. In an acidic medium, nitrite 4-dichloroaniline
INTRODUCTION Atypical results (colors different from the Detects bilirubin as
in the urine reacts with p-arsanilic acid to form a diazonium salt;
Urine undergoes many changes during states of disease or negative or positive color blocks shown on the Bilirubin 30 low as 0.4- 0.8
diazonium compound. The diazonium compound 99.5% w/w
body dysfunction before blood composition is altered to a color chart) may indicate that bilirubin-derived in turn couples with 1 N-(1-naphthyl)- (BIL) seconds mg/dL
buffer and
significant extent. Urinalysis is a useful procedure as an bile pigments are present in the urine specimen, (6.8-13.6 µmol/L).
ethylenediamine to produce a pink color. Nitrite non-reactive
indicator of health or disease, and as such, is a part of and are possibly masking the bilirubin reaction. is not detectable in normal urine. The nitrite area ingredients
routine health screening. Urine Reagent Strips can be Blood: This test is based on the peroxidase-like will be positive in some cases of infection, Detects free
used in general evaluation of health, and aids in the diagnosis 4% w/w
activity of hemoglobin which catalyzes the depending on how long the urine specimens hemoglobin as low
and monitoring of metabolic or systemic diseases that affect reaction of cumene-hydroperoxide and were retained in the bladder prior to collection. 3,3’,5,5’-tetramet
as
kidney function, endocrine disorders and diseases or 3,3',5,5'-tetramethylbenzidine. The resulting Retrieval of positive cases with the nitrite test hylbenzidine
0.015-0.062 mg/dL
disorders of the urinary tract. color ranges from orange to green to dark blue. ranges from as low as 40% in cases where little (TMB); 6% w/w
60 or
Any green spots or green color development on bladder incubation occurred, to as high as Blood cumene
seconds 5-10 Ery/µL in
PRINCIPLE AND EXPECTED VALUES the reagent area within 60 seconds is significant approximately 80% in cases where bladder (BLO) hydroperoxide;
urine specimens
Leukocytes: This test reveals the presence of and the urine specimen should be examined incubation took place for at least 4 hours. 90% w/w buffer
with ascorbic acid
granulocyte esterases. The esterases cleave a further. Blood is often, but not invariably, found Ascorbic acid: This test involves decolorization of and non-reactive
content of
derivatized pyrazole amino acid ester to liberate in the urine of menstruating females. Tillmann’s reagent. The presence of ascorbic acid ingredients
<50 mg/dL.
derivatized hydroxy pyrazole. This pyrazole then
Specific Gravity: This test is based on the causes the color of the test field to change from 2.5% w/w
reacts with a diazonium salt to produce a
apparent pKa change of certain pretreated blue-green to orange. bromthymol blue
beige-pink to purple color. Normal urine Determines urine
polyelectrolytes in relation to ionic concentration. pH: This test is based on a double indicator indicator; 17.5%
specimens generally yield negative results. Trace In the presence of an indicator, colors range from specific gravity
system which gives a broad range of colors w/w buffer and
results may be of questionable clinical between 1.000 and
deep blue-green in urine of low ionic covering the entire urinary pH range. Colors range non-reactive
significance. When trace results occur, it is concentration to green and yellow-green in urine Specific 1.030. Results
from orange to yellow and green to blue. The 45 ingredients; 55%
recommended to retest using a fresh specimen of increasing ionic concentration. Randomly Gravity correlate with
expected range for normal urine specimens from seconds poly (methyl
from the same patient. Repeated trace and collected urine may vary in specific gravity from (SG) values obtained by
newborns is pH 5-7. The expected range for other vinyl
positive results are of clinical significance. refractive index
1.003-1.040. Twenty-four hour urine from normal urine specimens is pH 4.5-8, with an ether/maleic
Glucose: This test is based on the enzymatic healthy adults with normal diets and fluid intake average result of pH 6. method within
anhydride); 25%
reaction that occurs between glucose oxidase, will have a specific gravity of 1.016-1.022. In ±0.005.
sodium
peroxidase and chromogen. Glucose is first cases of severe renal damage, the specific gravity MATERIALS hydroxide
oxidized to produce gluconic acid and hydrogen is fixed at 1.010, the value of the glomerular MATERIALS PROVIDED 0.3% w/w
peroxide in the presence of glucose oxidase. The filtrate. Strips. tetrabromophen Detects albumin as
hydrogen peroxide reacts with potassium iodide Protein: This reaction is based on the Package insert. Protein 60 ol blue; 99.7% low as
chromogen in the presence of peroxidase. The phenomenon known as the "protein error” of pH MATERIALS NEEDED BUT NOT PROVIDED (PRO) seconds w/w buffer and 7.5-20 mg/dL
extent to which the chromogen is oxidized indicators where an indicator that is highly Specimen collection container. non-reactive (0.075-0.2 g/L).
determines the color which is produced, ranging
buffered will change color in the presence of Timer. ingredients
from green to brown. Low amounts of glucose proteins (anions) as the indicator releases
are normally excreted in urine. Glucose 2.5% w/w Detects
hydrogen ions to the protein. At a constant pH, Urobilinog
concentrations as low as 100 mg/dL, read at RAEGENTS AND PERFORMANCE CHARACTERISTICS 60 p-diethylaminob urobilinogen as
the development of any green color is due to the en
either 10 or 30 seconds, may be considered Based on the dry weight at the time of seconds enzaldehyde; low as 0.2-1.0
presence of protein. Colors range from yellow to (URO)
abnormal if results are consistent. At 10 seconds, impregnation, the concentrations given may vary 97.5% w/w mg/dL (3.5-17
buffer and µmol/L). deteriorated. 3. Compare the reagent areas to the corresponding to and including trace (+).
non-reactive All specimens should be considered potentially color blocks on the canister label at the specified Bilirubin: Bilirubin is absent in normal urine, so
ingredients hazardous and handled in the same manner as an times. Hold the strip close to the color blocks and any positive result, including a trace positive,
Detects sodium infectious agent. match carefully. See illustration 3 below. indicates an underlying pathological condition
4.5% w/w nitrite as low as The used strip should be discarded according to Note: and requires further investigation. Reactions may
p-arsanilic acid; 0.05-0.1 mg/dL in local regulations after testing. Results may be read up to 2 minutes after the specified occur with urine containing large doses of
Nitrite 60 times.
95.5% w/w urine with a low chlorpromazine or rifampen that might be
(NIT) seconds
non-reactive specific gravity and STORAGE AND STABILITY mistaken for positive bilirubin.The presence of
1 2 3
ingredients less than 30 mg/dL Store as packaged in the closed canister either at bilirubin-derived bile pigments may mask the
ascorbic acid. room temperature (15-30°C). bilirubin reaction. This phenomenon is
0.5% w/w methyl Keep out of direct sunlight. characterized by color development on the test
red sodium salt; The strip is stable through the expiration date patch that does not correlate with the colors on
Permits the the color chart. Large concentrations of ascorbic
5% w/w printed on the canister label.
quantitative acid may decrease sensitivity.
pH
60 bromthymol
differentiation of Do not remove the desiccant. Remove only
seconds blue; enough strips for immediate use. Blood: A uniform blue color indicates the
pH values within
94.5% w/w non-r Replace cap immediately and tightly. presence of myoglobin, hemoglobin or
the range of 5- 9.
eactive Do not freeze. hemolyzed erythrocytes. Scattered or compacted
ingredients Do not use beyond the expiration date. blue spots indicate intact erythrocytes. To
0.5% w/w INTERPRETATION OF RESULTS enhance accuracy, separate color scales are
derivatized Note: Results are obtained by direct comparison of the provided for hemoglobin and for erythrocytes.
pyrrole amino Detects leukocytes Once the canister has been opened, the remaining strips color blocks printed on the canister label. Positive results with this test are often seen with
acid ester; 0.4% as low as are stable for up to 3 months. Stability may be reduced in The color blocks represent nominal values; actual urine from menstruating females. It has been
Leukocytes 120 values will vary close to the nominal values. reported that urine of high pH reduces sensitivity,
w/w diazonium 10-25 white blood high humidity conditions.
(LEU) seconds
salt; 32% w/w cells Leu/L in In the event of unexpected or questionable while moderate to high concentration of ascorbic
buffer; 67.1% clinical urine. SPECIMEN COLLECTION AND PREPARATION results, the following steps are recommended; acid may inhibit color formation. Microbial
w/w non-reactive A urine specimen must be collected in a clean Confirm that the specimens have been peroxidase, associated with urinary tract
ingredients and dry container and tested as soon as possible. tested within the expiration date printed infection, may cause a false positive reaction. The
0.3% w/w Do not centrifuge. on the canister label. test is slightly more sensitive to free hemoglobin
2,6-dichlorophen Detects ascorbic The use of urine preservatives is not Compare results with known positive and myoglobin than to intact erythrocytes.
Ascorbic olindophenol; acid as low as recommended. and negative controls and repeat the Specific Gravity: Ketoacidosis or protein higher
30 more than 100 mg/dL may cause elevated results.
Acid 99.7% w/w 5-10 mg/dL If testing cannot be done within an hour after test using a new strip.
seconds
(ASC) buffer and (0.28-0.56 voiding, refrigerate the specimen immediately If the problem persists, discontinue Results are not affected by non-ionic urine
non-reactive mmol/L). using the strip immediately and contact components such as glucose. If the urine has a
and let it return to room temperature before
ingredients your local distributor. pH of 7 or greater, add 0.005 to the specific
testing.
The performance characteristics of the Urine gravity reading indicated on the color chart.
Prolonged storage of unpreserved urine at room
Reagent Strips have been determined in both QUALITY CONTROL Protein: Any green color indicates the presence
temperature may result in microbial proliferation
laboratory and clinical tests. Parameters of For best results, performance of reagent strips should be of protein in the urine. This test is highly sensitive
with resultant changes in pH. A shift to alkaline
importance to the user are sensitivity, specificity, confirmed by testing known positive and negative for albumin, and less sensitive to hemoglobin,
pH may cause false positive results with the
accuracy and precision. Generally, this test has specimens/controls whenever a new test is performed, or globulin and mucoprotein. A negative result does
protein test area.
been developed to be specific for the parameters whenever a new canister is first opened. Each laboratory not rule out the presence of these other proteins.
Urine containing glucose may decrease in pH as
to be measured with the exceptions of the should establish its own goals for adequate standards of False positive results may be obtained with highly
organisms metabolize the glucose.
interferences listed. performance. buffered or alkaline urine. Contamination of
Contamination of the urine specimen with skin
Please refer to the Limitations section in this urine specimens with quaternary ammonium
cleansers containing chlorhexidine may affect
package insert. LIMITATIONS compounds or skin cleansers containing
protein (and to a lesser extent, specific gravity
Interpretation of visual results is dependent on and bilirubin) test results. As with all diagnostic and therapeutic tests, all chlorhexidine produce false positive results. The
several factors: results must be considered with other clinical urine specimens with high specific gravity may
The variability of color perception, information available to the physician. give false negative results.
PROCEDURE
The presence or absence of inhibitory Glucose: This test is highly specific for glucose. Urobilinogen: All results lower than 1 mg/dL
1. Remove the strip from the closed canister and
factors, No substance excreted in urine other than urobilinogen should be interpreted as normal. A
use it as soon as possible. Immediately close the
The lighting conditions when the strip is glucose is known to give a positive result. The negative result does not at any time preclude the
canister tightly after removing the required
read. reagent area does not react with ketones, lactose, absence of urobilinogen. The reagent area may
number of strip(s). Completely immerse the
galactose, fructose or other metabolic substances, react with interfering substances known to react
Each color block on the chart corresponds reagent areas of the strip in fresh, well-mixed
to a range of analyte concentrations. nor with reducing metabolites of drugs (e.g. with Ehrlich’s reagent, such as p-aminosalicylic
urine and immediately remove the strip to avoid
salicylates and nalidixic acid). Sensitivity may be acid and sulfonamides. False negative results may
dissolving the reagents. See illustration 1 below.
decreased in specimens with high specific gravity be obtained if formalin is present. The test
PRECAUTIONS 2. While removing the strip from the urine, run the
(>1.025) and with ascorbic acid concentrations of cannot be used to detect porphobilinogen.
For in vitro diagnostic use only. Do not use after edge of the strip against the rim of the urine
≥ 10 mg/dL. Nitrite: The test is specific for nitrite and will not
the expiration date. container to remove excess urine. Hold the strip
The strip should remain in the closed canister in a horizontal position and bring the edge of the Ketone: The test does not react with acetone or react with any other substance normally excreted
β-hydroxybutyrate. Urine specimens of high in urine. Any degree of uniform pink to red color
until use. strip into contact with an absorbent material (e.g.
pigment, and other substances containing should be interpreted as a positive result,
Do not touch the reagent areas of the strip. a paper towel) to avoid soiling hands with urine.
sulfhydryl groups occasionally give reactions up suggesting the presence of nitrite. Color intensity
Discard any discolored strips that may have See illustration 2 below.
is not proportional to the number of bacteria Serum, Plasma and Milk. Clin. Chem. Acta II:
present in the urine specimen. Pink spots or pink 372-378, 1965.
edges should not be interpreted as a positive 8. Henry JB, et al. Clinical Diagnosis and
result. Comparing the reacted reagent area on a Management by Laboratory Methods, 18th Ed.
white background may aid in the detection of low Philadelphia. Saunders. 396-397, 415, 1991.
nitrite levels, which might otherwise be missed. 9. Burtis CA, Ashwood ER. Tietz Textbook of Clinical
Ascorbic acid above 30 mg/dL may cause false Chemistry 2nd Ed. 2205, 1994.
negatives in urine containing less than 0.05 10. Tietz NW. Clinical Guide to Laboratory Tests. W.B.
mg/dL nitrite ions. The sensitivity of this test is Saunders Company. 1976.
reduced for urine specimens with highly buffered
alkaline urine. For accurate results, antibiotics
should be discontinued for at least 3 days before
the test is performed. A negative result does not ATLAS MEDICAL
at any time preclude the possibility of bacteruria. William James House, Cowley Rd,
Negative results may occur in urinary tract Cambridge, CB4 0WX
infections from organisms that do not contain Tel: ++44 (0) 1223 858 910
reductase to convert nitrate to nitrite; when Fax: ++44 (0) 1223 858 524
urine has not been retained in the bladder for a
sufficient length of time (at least 4 hours) for PPI587A01 Rev C (18.02.2010)
reduction of nitrate to nitrite to occur; or when
Product Store at 15 -
dietary nitrate is absent.
Reference No. 30°C.
pH: pH readings are not affected by variations in
urinary buffer concentration. For in-vitro
Leukocytes: The result should be read between Caution
diagnostic use.
60-120 seconds to allow for complete color
development. The intensity of the color that Number of Read product
develops is proportional to the number of tests in the insert before
leukocytes present in the urine specimen. High pack. use.
specific gravity or elevated glucose Lot (batch)
concentrations (≥ 500 mg/dL) may cause test Manufacturer.
number.
results to be artificially low. The presence of
cephalexin, cephalothin, or high concentrations Manufacturer
of oxalic acid may also cause test results to be telephone Expiry date.
artificially low. Tetracycline may cause decreased number.
reactivity, and high levels of the drug may cause a Manufacturer
false negative reaction. High urinary protein (≥ fax number.
500 mg/dL) may diminish the intensity of the
reaction color. This test will not react with
erythrocytes or bacteria common in urine.
REFERENCES
1. Free AH, Free HM. Urinalysis, Critical Discipline of
Clinical Science. CRC Crit. Rev. Clin. Lab. Sci. 3(4):
481-531, 1972.
2. Yoder J, Adams EC, Free, AH. Simultaneous
Screening for Urinary Occult Blood, Protein,
Glucose, and pH. Amer. J. Med Tech. 31:285,
1965.
3. Shchersten B, Fritz H. Subnormal Levels of
Glucose in Urine. JAMA 201:129-132, 1967.
4. McGarry JD, Lilly. Lecture, 1978: New
Perspectives in the Regulation of Ketogenesis.
Diabetes 28: 517-523 May, 1978.
5. Williamson DH. Physiological Ketoses, or Why
Ketone Bodies? Postgrad. Med. J. (June Suppl.):
372-375, 1971.
6. Paterson P, et al. Maternal and Fetal Ketone
Concentrations in Plasma and Urine. Lancet:
862-865; April 22, 1967.
7. Fraser J, et al. Studies with a Simplified
Nitroprusside Test for Ketone Bodies in Urine,
You might also like
- Urine parameters(1)Document2 pagesUrine parameters(1)earldioborrinagaNo ratings yet
- Us Vis13Document2 pagesUs Vis13Nghi NguyenNo ratings yet
- Putri Wulandari 024Document8 pagesPutri Wulandari 024Septi Wulandari AnwarNo ratings yet
- Urine StripsDocument4 pagesUrine StripsABUAC CYSSELLE DAWN KNo ratings yet
- 171 CT10350Document2 pages171 CT10350thureinwinnNo ratings yet
- CT - Urine Strips - 20141101bDocument2 pagesCT - Urine Strips - 20141101bAliNo ratings yet
- FRUCTOSAMINEDocument1 pageFRUCTOSAMINERisqon Anjahiranda AdiputraNo ratings yet
- Detect liver and kidney issues with urine testsDocument5 pagesDetect liver and kidney issues with urine testsMargaret Nicole AboNo ratings yet
- Yazz Bilirrubina DirectaDocument2 pagesYazz Bilirrubina DirectaFlorence ToroNo ratings yet
- CT10382Document4 pagesCT10382Nguyễn HuynhNo ratings yet
- Albumin Package InsertDocument2 pagesAlbumin Package InsertjairajNo ratings yet
- Clinical Chemistry Review 1 110Document6 pagesClinical Chemistry Review 1 110DELLNo ratings yet
- Glucose (Mono Reagent) (GOD/POD Method) : For in Vitro Diagnostic Use OnlyDocument2 pagesGlucose (Mono Reagent) (GOD/POD Method) : For in Vitro Diagnostic Use OnlySourav MondalNo ratings yet
- Fluitest U/Csf: Ultrasensitive ProteinDocument4 pagesFluitest U/Csf: Ultrasensitive ProteinDarko MaksimovicNo ratings yet
- Albumin & Total Protein: (Page 1 - ALBUMIN) 4 X 50 ML 11002001Document2 pagesAlbumin & Total Protein: (Page 1 - ALBUMIN) 4 X 50 ML 11002001N. K. MandilNo ratings yet
- Fluitest Urea: BiolyzerDocument4 pagesFluitest Urea: BiolyzerLhiyvind PaoNo ratings yet
- Urea (Vitro)Document2 pagesUrea (Vitro)m sdNo ratings yet
- AUBF LAB - Exams and QuizzesDocument18 pagesAUBF LAB - Exams and QuizzesLUALHATI VILLASNo ratings yet
- Tanner Scientific 10SG Reagent Test StripsDocument2 pagesTanner Scientific 10SG Reagent Test Stripssaifulmangopo123No ratings yet
- NotesDocument9 pagesNotesLyudmyla GillegoNo ratings yet
- Mod 9 CC of Proteins Part 2Document5 pagesMod 9 CC of Proteins Part 2Benson PaglinawanNo ratings yet
- Albumin: Quantitative Determination of AlbuminDocument2 pagesAlbumin: Quantitative Determination of AlbuminNguyễn Ngọc TuyếnNo ratings yet
- CA NotesDocument6 pagesCA NotesJean Calubag CatalanNo ratings yet
- Multistix Reagent StripDocument3 pagesMultistix Reagent StripFrancis TorresNo ratings yet
- Métodos de Reactivos Marca Jas para Equipo Metrolab-2300 PlusDocument2 pagesMétodos de Reactivos Marca Jas para Equipo Metrolab-2300 PlusInversiones Llanolab, c.a. LlanolabNo ratings yet
- EN Albumin PDFDocument1 pageEN Albumin PDFDharmesh PatelNo ratings yet
- Urinalysis System Line enDocument4 pagesUrinalysis System Line enNghi NguyenNo ratings yet
- Catalog # URS-10: 100 Strips Per BoxDocument4 pagesCatalog # URS-10: 100 Strips Per BoxLey100% (1)
- Albumin: N.S. Bio-TecDocument2 pagesAlbumin: N.S. Bio-Tecكن مع اللهNo ratings yet
- Bilirubin Stability and Interference FactorsDocument2 pagesBilirubin Stability and Interference FactorsKian Andrei VinluanNo ratings yet
- BILIRUBIN TOTAL TEST RESULTS AND PROCEDUREDocument4 pagesBILIRUBIN TOTAL TEST RESULTS AND PROCEDUREMatibar RahmanNo ratings yet
- Low Serum Bicarbonate in A Patient With Diabetes&#Document3 pagesLow Serum Bicarbonate in A Patient With Diabetes&#ayaz ahmadNo ratings yet
- Microprotein Reagent Precautions and UseDocument2 pagesMicroprotein Reagent Precautions and UseJuan Sánchez100% (1)
- QUANTITATIVE ALBUMIN TESTDocument2 pagesQUANTITATIVE ALBUMIN TESTrichardNo ratings yet
- Total Protein Reagent KitDocument1 pageTotal Protein Reagent KitJohnmar AquinoNo ratings yet
- Bilirrubinas PDFDocument2 pagesBilirrubinas PDFWilmer Cruzado CarrascoNo ratings yet
- EN GGT BAOSR6x19 USDocument2 pagesEN GGT BAOSR6x19 USDharmesh PatelNo ratings yet
- COD reagents measure protein concentrationDocument1 pageCOD reagents measure protein concentrationNisa Javadd100% (2)
- Total ProteinDocument2 pagesTotal ProteinMina MouradNo ratings yet
- Urine Test Strip AnalysisDocument4 pagesUrine Test Strip AnalysisAurian TormesNo ratings yet
- LabStripU11 GL Instructions For UseDocument4 pagesLabStripU11 GL Instructions For UseAurian TormesNo ratings yet
- Albumin: Intended Use MethodDocument2 pagesAlbumin: Intended Use MethodForhadur RezaNo ratings yet
- Iiquicolor: Photometric Test For Calcium CPC MethodDocument1 pageIiquicolor: Photometric Test For Calcium CPC MethodMaherNo ratings yet
- Transes Act 7 CC LabDocument7 pagesTranses Act 7 CC LabCiara PamonagNo ratings yet
- Mission Urinalysis Strips InsertDocument1 pageMission Urinalysis Strips Insertquirmche70No ratings yet
- PI - TPROT e 6Document1 pagePI - TPROT e 6NawelNo ratings yet
- Urea Color 2r en PDFDocument3 pagesUrea Color 2r en PDFKmo mastnNo ratings yet
- Randox ..... BilirubinDocument4 pagesRandox ..... BilirubinJohn SenufaNo ratings yet
- MLS-111B-LABORATORY-ENDTERM-very-finalDocument6 pagesMLS-111B-LABORATORY-ENDTERM-very-finalJohanna MarieNo ratings yet
- Alb2.Js02 (1) AlbuminaDocument2 pagesAlb2.Js02 (1) AlbuminaJuan SánchezNo ratings yet
- Pamyl Ifcc B GB D 21 001Document4 pagesPamyl Ifcc B GB D 21 001Cristian LaraNo ratings yet
- Examination Done Date Results Normal Values Significance or Relevance To Patient's Condition UrinalysisDocument10 pagesExamination Done Date Results Normal Values Significance or Relevance To Patient's Condition UrinalysisStephanie Libo-onNo ratings yet
- Proteins Lab Methods ExplainedDocument36 pagesProteins Lab Methods ExplainedDawlat Salama100% (1)
- Post Lab QuestionDocument3 pagesPost Lab QuestionJoshua DividinaNo ratings yet
- EN - TOTAL PROTEIN - BAOSR6x32 - USDocument3 pagesEN - TOTAL PROTEIN - BAOSR6x32 - USDharmesh PatelNo ratings yet
- TRIGLYCERIDES PROCEDUREDocument2 pagesTRIGLYCERIDES PROCEDUREMarj MendezNo ratings yet
- Stanbio BUN PDFDocument2 pagesStanbio BUN PDFKian Andrei VinluanNo ratings yet
- FructosamineDocument3 pagesFructosaminetuan vănNo ratings yet
- Total ProteinDocument2 pagesTotal ProteinBEA PETILNo ratings yet
- 219 D4 - PhototherapyDocument2 pages219 D4 - PhototherapyAngelina Mei BenitezNo ratings yet
- Algoritmo IctericiaDocument18 pagesAlgoritmo IctericiaDiego RodriguezNo ratings yet
- Application and Optimization of Reference Change Values For Delta Checks in Clinical LaboratoryDocument8 pagesApplication and Optimization of Reference Change Values For Delta Checks in Clinical Laboratorymahmouda100No ratings yet
- Urinalysis Results InterpretationDocument21 pagesUrinalysis Results InterpretationSutjipto WijonoNo ratings yet
- Medicine Gi ModuleDocument11 pagesMedicine Gi ModuleBobet ReñaNo ratings yet
- Jaundice Biochemical ProfileDocument64 pagesJaundice Biochemical ProfileGhaidaa SadeqNo ratings yet
- BiliDocument63 pagesBiliFu Xiao ShanNo ratings yet
- Neonatal Jaundice and Prolonged Jaundice in Newborn InfantsDocument33 pagesNeonatal Jaundice and Prolonged Jaundice in Newborn InfantskeyRielleNo ratings yet
- Staining Techniques: Connective TissueDocument6 pagesStaining Techniques: Connective TissuePamela Dawn PornesoNo ratings yet
- Laboratory Correlation of Urine ColorDocument2 pagesLaboratory Correlation of Urine ColorKyle PicocNo ratings yet
- Newborn Case StudyDocument16 pagesNewborn Case StudyErl Joy Montaño Cañete0% (1)
- Med Surg 2 - 8 Malabsorption Syndromes and Nursing Care of Clients With Hepatic DisordersDocument8 pagesMed Surg 2 - 8 Malabsorption Syndromes and Nursing Care of Clients With Hepatic DisordersMaxinne RoseñoNo ratings yet
- Evidence Based PediatricDocument463 pagesEvidence Based Pediatricsetyo pranotoNo ratings yet
- High Risk PediatricsDocument207 pagesHigh Risk Pediatricsruby cubionaNo ratings yet
- Test #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyDocument47 pagesTest #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyJahangir AlamNo ratings yet
- 2.biochemistry OSPEDocument55 pages2.biochemistry OSPEmermaidshruti1524No ratings yet
- Bharath A PDocument103 pagesBharath A PSuman MondalNo ratings yet
- Laboratory Test Report: Male 25 YearsDocument5 pagesLaboratory Test Report: Male 25 Yearsom_prakash1986100% (1)
- Liver and kidney function test reportDocument4 pagesLiver and kidney function test reportMuhammad IshfaqNo ratings yet
- SerosisDocument41 pagesSerosistasya salsabilaNo ratings yet
- JaundiceDocument22 pagesJaundiceimanzurynn161No ratings yet
- Perinatal Asphyxia in Term and Late Preterm Infants - UpToDateDocument31 pagesPerinatal Asphyxia in Term and Late Preterm Infants - UpToDateRocio GNo ratings yet
- #16 - NCM 109 (Rle) - TransesDocument7 pages#16 - NCM 109 (Rle) - TransesJaimie BanaagNo ratings yet
- Neonatal JaundiveDocument15 pagesNeonatal JaundiveCarolyn CapisnonNo ratings yet
- Bilirubin Direct: ADL/V.01/110314Document1 pageBilirubin Direct: ADL/V.01/110314S MNo ratings yet
- JaundiceDocument20 pagesJaundicelourdesfercab_at_msnNo ratings yet
- Icteric Index and Its SignificanceDocument3 pagesIcteric Index and Its SignificanceJulius FrondaNo ratings yet
- BilirubinbeaconDocument2 pagesBilirubinbeaconMalou AndersenNo ratings yet
- LED PhototherapyDocument7 pagesLED PhototherapyAreef MuarifNo ratings yet
- Neonatal HyperbilirubinemiaDocument22 pagesNeonatal Hyperbilirubinemiajoza29No ratings yet