Professional Documents
Culture Documents
Module 3: The Cardiovascular System
Uploaded by
koya patOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Module 3: The Cardiovascular System
Uploaded by
koya patCopyright:
Available Formats
NPHW Training Manual Module 3
Module 3: The Cardiovascular System
Module Aim
This module is an overall introduction to the cardiovascular system, its components, and
their functions and some related diseases. This will help you understand underlying causes
of risk factors outlined in Module 4 that lead to cardiovascular diseases. This module is
important to understand, as further modules will build on this basic knowledge.
This module contains the following sections:
Section 3.1: Structure and Function of the Cardiovascular System
Section 3.2: Diseases of the Cardiovascular System
Section 3.3: Burden of Cardiovascular Disease
Final 3.0 – 2015-September-17 Page 1 of 20
NPHW Training Manual Module 3
Contents
Module Aim................................................................................................................................................... 1
Module 3 Pre-test ......................................................................................................................................... 3
Section 3.1: Structure and Function of the Cardiovascular System.............................................................. 4
3.1.1. Introduction to the Cardiovascular System .................................................................................... 4
3.1.2. Blood ............................................................................................................................................... 5
I. Red blood cells (RBCs) ........................................................................................................................ 5
II. White blood cells (WBCs) .................................................................................................................. 5
III. Platelets............................................................................................................................................ 6
IV. Plasma .............................................................................................................................................. 6
Functions of Blood ................................................................................................................................ 6
3.1.3. Heart ............................................................................................................................................... 7
Chambers and Valves ............................................................................................................................ 7
Flow of Blood ........................................................................................................................................ 8
Beating of the Heart.............................................................................................................................. 8
The Cardiac Cycle .................................................................................................................................. 9
3.1.4. Blood Vessels .................................................................................................................................. 9
I. Arteries ............................................................................................................................................. 10
II. Capillaries ........................................................................................................................................ 10
III. Veins ............................................................................................................................................... 10
Section 3.2: Diseases of the Cardiovascular System ................................................................................... 11
3.2.1. Heart Attack, Angina, and CHD ..................................................................................................... 12
3.2.2. Stroke ............................................................................................................................................ 15
3.2.3. Peripheral Vascular Disease .......................................................................................................... 16
3.2.4. Congestive Heart Failure (CHF) ..................................................................................................... 16
Section 3.3: Burden of Cardiovascular Disease........................................................................................... 18
3.3.1. Socio-Economic Burden ................................................................................................................ 19
Module 3 Post-Test ..................................................................................................................................... 20
Final 3.0 – 2015-September-17 Page 2 of 20
NPHW Training Manual Module 3
Module 3 Pre-test
Instructions: Read the following statements carefully and tick [√] the appropriate column. If you are
unsure of any answer you may tick the “Don’t Know” column. The time allotted to you is 5 minutes.
Don’t
Number Question True False
Know
1 Blood delivers oxygen throughout the body.
2 The heart normally contains 5 chambers.
Blood pressure is created by the lungs putting
3
pressure on blood vessels.
A heart attack is caused by a clot in the blood vessels
4
of the heart.
5 A stroke occurs when the brain is deprived of oxygen.
Congestive heart failure means the heart stops
6
beating.
Cardiovascular disease primarily affects higher income
7
countries and groups.
Final 3.0 – 2015-September-17 Page 3 of 20
NPHW Training Manual Module 3
Section 3.1: Structure and Function of the Cardiovascular System
In this section, you will learn about the structure of different parts of the cardiovascular system (CVS) as
well as their functions. It is important to have a clear idea of the CVS structures and functions discussed
in this section in order to understand the ways cardiovascular diseases can occur, which are discussed in
the next sections. This section will also help you understand the CVS, so if/when a participant or their
treatment supporter has questions, you will be able to discuss the participant’s CV conditions.
The body is made up of a number of systems that control different functions, such as the respiratory
system for breathing, the digestive system that helps us break down the foods we eat, and the nervous
system that allows us to think and react to the environment around us. In the HOPE-4 program, we are
interested in the CVS – the system responsible for supplying blood to all parts of our bodies. It is an
essential system for survival, and in this module we will look at the parts of this system and why we
need to keep it healthy.
Learning objectives – at the end of this section you should be able to:
List the key components of the CVS
List the components and function of blood
Understand the flow of blood and chambers in the heart
Explain the types of blood vessels and flow of blood throughout the body
Describe blood pressure and its importance
This section contains the following subsections:
3.1.1. Introduction to the Cardiovascular System
3.1.2. Blood
3.1.3. Heart
3.1.4. Blood Vessels
3.1.1. Introduction to the Cardiovascular System
All the organs and tissues in the body require oxygen. This requirement is fulfilled by the constant flow
of oxygen-carrying blood. The CVS is responsible for making sure the flow of blood is constant, allowing
every cell in the body to have access to oxygen. Without a properly functioning CVS, our cells would be
unable to function properly. The CVS has a number of parts that control the flow of blood. These
components are:
Blood
Heart
Blood vessels
Final 3.0 – 2015-September-17 Page 4 of 20
NPHW Training Manual Module 3
The main function of the CVS is to pump blood throughout the body. The function of the heart is to act
as the pump, pushing blood into the blood vessels. The blood vessels carry blood to all the different
parts of the body, before it is returned back to the heart to start the cycle again. Blood carries oxygen
from the lungs throughout the body. It is also responsible for transporting waste products such as
carbon dioxide, which are then eliminated by other bodily systems.
Remember:
The major components of the cardiovascular system are:
- Blood
- Heart
- Blood vessels
The main purpose of the cardiovascular system is to pump
nutrient-rich and oxygen-rich blood to all parts of the body.
3.1.2. Blood
Blood is a fluid that delivers necessary substances, including nutrients and oxygen, to all different parts
and cells of the body. Blood also carries waste products away from the cells to other areas where they
can be processed. The average adult has around 5 liters of blood.
Blood is mainly composed of solid blood cells, which are suspended in the liquid plasma. The plasma
consists of approximately 90% water, with the rest being made up of other dissolved substances (e.g.
clotting proteins, sugars, hormones, and minerals). There are four main components of blood (Figure 1):
I. Red blood cells
II. White blood cells
III. Platelets
IV. Plasma
I. Red blood cells (RBCs)
These are the most common cells in the blood. These cells contain a special protein called hemoglobin
that allows them to transport oxygen and carbon dioxide within the blood stream. This function makes
these cells extremely important.
II. White blood cells (WBCs)
These cells are part of the immune system, acting to defend the body from infectious diseases or
intruding cells. They destroy and remove old cells and debris from the blood, while also attacking foreign
disease-causing agents and foreign substances in the body.
Final 3.0 – 2015-September-17 Page 5 of 20
NPHW Training Manual Module 3
III. Platelets
These cells are responsible for the clotting of blood, also referred to as ‘coagulation’. When the skin is
cut, these cells create a mesh-like barrier over the cut. Other blood cells become caught in the mesh and
collect to form a clot, which stops blood from leaving the body and prevents bacteria from entering the
bloodstream. Platelets are very important in tissue healing.
IV. Plasma
Plasma is the liquid component of blood that the cells are suspended in. It accounts for around 50% of
the total volume of blood and contains things like dissolved proteins, glucose, and platelets, as well as
the blood cells themselves.
Blood Cells
•WBCs
•RBCs
Plasma Platelets
Blood
Figure 1. The components of blood
Functions of Blood
Blood is a vital fluid in our bodies and performs many important functions.
Some of these functions include:
Supplying oxygen to tissues (carried by RBCs)
Supplying nutrients from food to cells around the body
Removal of waste, including carbon dioxide
Defense against diseases and detection of foreign material (by WBCs)
Clotting and prevention of blood loss (platelets and clotting proteins)
Messenger functions by transporting hormones to various systems, allowing them to interact
(e.g. insulin is created by the digestive system and circulated through the blood, allowing cells to
absorb sugars from food we eat)
Helping regulate and maintain body temperature
Final 3.0 – 2015-September-17 Page 6 of 20
NPHW Training Manual Module 3
Activity: Matching
Match the listed components with their functions.
I. Responsible for blood clotting A. Red blood cells
II. Contain hemoglobin responsible for carrying oxygen B. Plasma
III. Destroy and remove old cells and foreign substances C. White blood cells
IV. Liquid part of blood containing 90% water D. Platelets
3.1.3. Heart
The heart pumps blood in order for it to circulate throughout the body. The heart is a very strong muscle
that is able to contract and relax rhythmically throughout a person’s lifetime. Each day, the heart will
beat an average of 100,000 times, pumping over 7,500 liters of blood. The heart is located in the left
side of the chest, in a cavity between the right and left lungs. It weighs between 200 and 425 grams
(around the weight of a can of pop), and is a little larger than an individual’s clenched fist. Because the
heart is a large, constantly active muscle, it must also have its own constant supply of oxygen, allowing it
to continue pumping.
Chambers and Valves
The human heart has four chambers, each separated by a valve (Figure 2). The four chambers include
the right atrium, right ventricle, left atrium, and left ventricle. When you are looking at the diagram
below, it is important to note that the left and right are reversed. Imagine they are the left and right side
of your body as you would see them. It is the relaxation and contraction of these chambers that allows
the heart to pump blood. The valves that separate the four chambers prevent blood from flowing
backwards, thus only allowing the flow of blood in one direction. Genetic defects or illness-related
damage in the heart chambers or valves disrupt the flow of blood, which may be contributing factors to
the development and severity of cardiovascular diseases.
Aorta
Left Atrium
Right Atrium
Left Ventricle
Right Ventricle
Figure 2. The heart with the four chambers and aorta
Final 3.0 – 2015-September-17 Page 7 of 20
NPHW Training Manual Module 3
Flow of Blood
The heart is made up of large muscles that cause the contraction and relaxation of the heart, and when
these muscles take turns contracting, blood is passed through the valves separating the chambers, from
one chamber into another. The two right chambers (the right atrium and right ventricle) are responsible
for pumping blood to the lungs. When this blood passes by the lungs, it collects oxygen (enters the body
during inhalation), and drops off carbon dioxide (exits the body during exhalation). The freshly
oxygenated blood returns to the left side of the heart (left atrium and left ventricle), from which it is
pumped into the aorta. The aorta splits into the other blood vessels of the body and distributes the
oxygenated blood.
When the oxygen is used by cells, they replace it with carbon dioxide. The blood collects through the
blood vessels and returns to the right side of the heart. From here, the cycle is repeated, with the right
side of the heart pumping the deoxygenated blood to the lungs where it becomes oxygenated.
Beating of the Heart
We know that it is the contraction of the heart that pumps blood throughout the body, but what is it
that causes these contractions to happen? The heartbeat is created by small electrical impulses that
perpetually cause the muscles in the heart to contract. A network of nerve fibers is present between the
muscles in the heart, and these fibers act like electrical wires, coordinating the contraction and
relaxation of the different chambers. By keeping all of these muscles contracting and relaxing in a
coordinated way, the heart creates a wave-like pumping action that efficiently moves blood throughout
the body. The steady pumping action of the heart is often described as its ‘rhythm’.
It is normal for the heart to beat at different rates throughout the day. People may occasionally
experience harmless variations in heart rhythm, referred to as palpitations. To contrast, a consistently
abnormal heart rhythm is referred to as an arrhythmia. The heart may beat too fast, too slow, or with
an irregular pattern. Changes to heart rhythm are caused by irregularities in the transmission of the
electrical impulses that cause the heart muscles to contract. An arryhthmia does not necessarily mean
that the heart is unhealthy, but some types of arrhythmias are of concern. Syncope (fainting) is
associated with some arrhythmias. Arrhythmias must be diagnosed by a physician, often using an
electrocardiogram (ECG) or other heart monitoring device.
The most common arrhythmia is atrial fibrillation, which is characterized by a rapid, irregular heart
beat. Atrial fibrillation is caused by abnormal electrical impulses in the upper chambers of the heart (left
atrium and right atrium). These abnormal electrical impulses cause the upper chambers to contract very
rapidly and irregularly, in comparison to the lower chambers of the heart (left and right ventricles). The
pumping action of the heart is therefore uncoordinated, so the heart does not pump blood as efficiently.
Atrial fibrillation decreases the heart’s pumping efficiency and increases the risk of blood clot formation
in the heart and the arteries. These effects can increase a person’s risk of congestive heart failure, heart
attack, and stroke, which you will discuss in section 3.2.
Final 3.0 – 2015-September-17 Page 8 of 20
NPHW Training Manual Module 3
The Cardiac Cycle
The cardiac cycle is the sequence of events that occurs when the heart beats. There are two phases of
this cycle:
I. Systole (contraction)
II. Diastole (relaxation)
I. Systole
Systole is the phase in which both ventricles contract. When these two chambers contract, the muscles
powerfully push the blood out into the blood vessels moving away from the heart. As noted before, the
right ventricle pushes blood to the lungs, while the left ventricle pushes blood into the aorta, before it is
distributed to the rest of the body. During this phase, the contractions cause an increase in the pressure
within the blood vessels.
II. Diastole
Diastole is the phase in which both ventricles are relaxed. When these two chambers are relaxed, they
are refilled with blood from the each atrium, getting new blood to pump out from the heart and into the
blood vessels when the cycle begins again. During this phase, no new blood is pumped into the blood
vessels, and thus the pressure in the blood vessels is lower than it is during systole.
The cycle of systole and diastole phases continues repeating and is called the cardiac cycle. A normal
human heart beats around 60-70 times per minute when at rest.
Remember:
It is the contraction and relaxation of the heart that pushes blood through the blood vessels.
Systole is when the heart is contracting (higher pressure).
Diastole is when the heart is relaxed (lower pressure).
3.1.4. Blood Vessels
The blood vessels are the part of the CVS that carry blood throughout the different parts of the body.
These vessels carry blood into all of our organs and tissues, supplying the oxygen and nutrients
necessary for our bodies to function properly.
There are 3 major types of blood vessels:
I. Arteries – carry blood (rich in oxygen) away from the heart to the body
II. Capillaries – very small blood vessels that allow for exchange of gases (oxygen and carbon
dioxide), water, nutrients, and waste products to and from the blood
III. Veins – carry blood (poor in oxygen) back to the heart
Final 3.0 – 2015-September-17 Page 9 of 20
NPHW Training Manual Module 3
I. Arteries
Arteries are the blood vessels that carry blood away from the heart. The walls of these vessels are elastic
in nature, which allows them to expand and contract as the heart powerfully pumps blood through
them. The size of these vessels decreases as they move further and further away from the heart, until
they become the smallest vessels – capillaries. The heart has its own set of arteries to supply it with
blood called the coronary arteries. These will be further discussed in section 3.2.
The powerful pumping of the heart exerts pressure on the walls of the arteries as blood flows through
them, causing them to expand. This rhythmic expansion and contraction of the blood vessels can be felt
as the pulse (or heart rate), and it can be measured as blood pressure (BP). We will discuss these further
in Module 4 and Module 5. It is important to remember, however, that the force of the blood on the
blood vessels is what creates BP.
II. Capillaries
As the arteries become smaller and smaller, they eventually turn into capillaries – very thin blood
vessels. These vessels are thin enough to allow the products carried within the blood to be exchanged
with the surrounding tissues. These include nutrients derived from food, oxygen, carbon dioxide, and
waste products. As waste products and carbon dioxide collect in the capillaries, many capillaries come
together and form larger vessels to transport the blood back to the heart – these larger vessels are the
veins.
III. Veins
Veins collect blood from the capillaries and return it to the heart. Since they are farther away from the
heart, the BP in these vessels is much lower compared to arteries. The veins all carry low oxygen (poor in
oxygen) blood back to the heart, where the cycle can repeat itself.
Remember:
There are three major types of blood vessels:
I. Arteries
II. Capillaries
III. Veins
It is important to note that the two most important organs of the body – the heart and the brain – have
networks of blood vessels that ensure they are constantly supplied with blood. A constant supply to
these organs is crucial for our well-being, and problems with circulation to these organs can cause
serious problems, as will be discussed in the next section.
Discussion Questions
What are the main functions of blood, and what might happen if one of these functions were to be
disabled?
Final 3.0 – 2015-September-17 Page 10 of 20
NPHW Training Manual Module 3
During systole is the heart contracting or relaxing? Does the BP increase or decrease during this phase?
How about for diastole?
If a blood vessel becomes blocked, what might happen?
Section 3.2: Diseases of the Cardiovascular System
Now that you have an understanding of the structure and normal function of the CVS, we will look at
some important diseases that occur as a result of issues that affect the CVS. Disturbances to any part of
the CVS, including conditions discussed in the previous section, such as heart chamber or valve defects
and arrhythmias like atrial fibrillation, can contribute to the development and severity of diseases that
ultimately prevent the blood from adequately circulating to all parts of the body.
Cardiovascular Disease (CVD) includes a group of disorders of the heart and blood vessels, including:
Coronary heart disease (CHD) (heart attack, angina, congestive heart failure)
Cerebrovascular disease (stroke)
Peripheral vascular disease (poor blood supply to limbs)
Rheumatic heart disease (heart damage from bacterial infection)
Congenital heart disease (heart defect present at birth)
Deep vein thrombosis and pulmonary embolism (blockages of blood flow due to blood clots)
CHD and cerebrovascular disease (stroke) account for the majority of cases of CVD. CHD includes heart
attacks, angina, and congestive heart failure.
Learning objectives – at the end of this section, you should be able to:
Identify and describe significant CVD
Understand the conditions that lead to these diseases
List the parts of the CVS that are affected by these diseases
This section contains the following subsections:
3.2.1. Heart Attack, Angina, and CHD
3.2.2. Stroke
3.2.3. Peripheral Vascular Disease
3.2.4. Congestive Heart Failure
Final 3.0 – 2015-September-17 Page 11 of 20
NPHW Training Manual Module 3
3.2.1. Heart Attack, Angina, and CHD
The heart requires a constant supply of oxygenated blood. As mentioned previously, the heart has its
own blood supply, which is critical to its function. When the muscle cells in the heart do not receive
adequate oxygen, they die. A blocked artery within the heart is the usual cause of insufficient oxygen for
heart function. How is this caused?
First, we must understand atherosclerosis (blockages in the arteries due to plaque build-up). Previously,
arteries were described as elastic vessels that expand and contract with each beat of the heart. As a
person ages, these arteries lose their elasticity and can get harder and thicker. This thickening and
hardening is due to the deposition of plaque on the internal lining of the arteries. Plaque typically
contains cholesterol (fatty substance), waste products from cells, and calcium. As this plaque deposits
itself on the normally smooth lining of the arteries, it reduces the amount of space through which blood
can flow (Figure 3). Plaques can rupture or crack, which can cause the sudden formation of a blood clot.
Figure 3. The effects of
Plaque
atherosclerosis on blood vessels
narrows
artery;
Obstacle to
Normal blood flow
Blood
Flow
Normal Artery Atherosclerosis Artery
Pressure is exerted onto the walls of blood vessels as blood flow through them, so blood vessel walls
must be strong to contain the blood. The hardening of blood vessels from plaque build-up can weaken
the walls of blood vessels. Narrowing of the arteries due to atherosclerosis, and high blood pressure, put
additional pressure on blood vessels, particularly where they branch. A weakened blood vessel can
develop an outward bulge, referred to as an aneurysm. Rupture of an aneurysm can lead to internal
bleeding and may be life-threatening if undetected.
Since the heart is essentially a large muscle that is constantly contracting and relaxing, it requires its
own blood supply to provide it with sufficient oxygen. This blood is supplied through a specific group of
arteries known as the coronary arteries. When atherosclerosis occurs within the coronary arteries, it can
lead to decreased blood supply to those areas of the heart that are affected. Without sufficient blood
flow in the coronary arteries, the heart becomes fatigued from a lack of nutrients and oxygen. The
restriction of blood flow to vessels in the heart is called coronary heart disease (CHD) (Figure 4).
Final 3.0 – 2015-September-17 Page 12 of 20
NPHW Training Manual Module 3
Figure 4. The effects of
atherosclerosis on arteries in
the heart cause CHD
Angina (chest pain) is a result of
partial blockages of coronary
arteries due to CHD.
To treat CHD, a hospital procedure is generally required and can be either surgical or non-surgical. The
non-surgical intervention is called angioplasty, which is a medical term to describe the procedure in
which narrow coronary arteries are widened using a tiny balloon that is inflated to widen the artery. A
stent is often put in place after the artery is widened. It is essentially a tube that is placed in the
narrowed coronary artery that allows blood to flow through more easily (Figure 5).
Balloon
Figure 5. The Stent
angioplasty
procedure
A small balloon
opens up the
narrowed artery
and a stent is
placed to re-
establish proper
blood flow.
The surgical procedure to treat CHD is called coronary bypass surgery, wherein a narrowed coronary
artery is surgically removed and the narrowed section bypassed (Figure 6). An analogy of the bypass
surgery would be like building a new road around a congested highway to avoid the traffic – a new
coronary artery is placed around the old one so the blood can flow past it more freely.
Final 3.0 – 2015-September-17 Page 13 of 20
NPHW Training Manual Module 3
Figure 6. Bypass surgery
A bypass graft (a replacement artery) is
placed to avoid blood flow through a
narrowed or blocked coronary artery.
Angina (chest pain) is a condition caused by decreased blood flow to areas of the heart, due to CHD
(Figure 4). As previously discussed, CHD is caused by atherosclerosis, which narrows or blocks coronary
arteries. Heart valve problems can also restrict blood flow in the coronary arteries and cause angina.
Pain is caused by a buildup of lactic acid – a waste product from heart muscles that are not getting
enough oxygen. Lactic acid buildup is the same thing that causes pain in your arms or legs when
exercising for a long period of time. Angina is usually treated by using drugs that that either increase the
oxygen available to the heart, or reduce its demand for oxygen, allowing the reduced blood flow to
provide enough oxygenated blood. Angina can be brought on by strenuous activity or exertion. The pain
often goes away after less than 10 minutes rest, or when medication (e.g. nitroglycerin) is taken.
Angioplasty and coronary artery bypass surgery can improve blood flow in people with angina.
Worsening CHD can result in the development of a clot. Clots are formed by platelets in the blood
binding together. The clot may form in an artery and completely block blood flow through that artery. A
complete blockage of a coronary artery from a clot prevents heart cells from receiving an adequate
amount of oxygen, causing the heart cells to function improperly and even die. When a complete
blockage occurs suddenly and causes heart muscle cells to die, it is known as a heart attack. The severity
of a heart attack depends on the size of the artery that is blocked by the clot (and therefore the
corresponding reduction in oxygen-rich blood that reaches heart muscle cells). A heart attack causes
chest pain that can extend into the shoulders, arms and jaw. It must be treated in the hospital using
drugs to control pain, and to reduce or remove the clot. Bypass surgery may also be used to bypass the
clot, similar to CHD and angina treatment. The risk of clot formation inside the chambers of the heart is
increased if a person has atherosclerosis, due to restricted blood flow. Similarly, conditions that impair
blood flow, such as heart valve defects or atrial fibrillation, further increase the risk of clot formation.
Remember:
Atherosclerosis is the thickening and hardening of the arteries due to buildup of plaque
Thickening and partial blockage of coronary arteries is called CHD
CHD can lead to angina
A sudden total blockage due to a blood clot in the coronary arteries can cause a heart attack
Final 3.0 – 2015-September-17 Page 14 of 20
NPHW Training Manual Module 3
3.2.2. Stroke
Like the heart, the cells of the brain are extremely sensitive and require a constant flow of oxygenated
blood in order to function properly. These cells cannot survive without oxygen for more than a few
minutes. A lack of oxygenated blood flow to any part of the brain can result in a stroke (Figure 7).
Atherosclerosis can occur in the arteries leading to the brain, just as in any other arteries.
Atherosclerosis can therefore cause stroke from partial or complete blockage of arteries leading to the
brain, just as partial or complete blockage of coronary arteries respectively leads to CHD and angina, or
heart attack. Consequently, stroke is most commonly (80%) due to a blockage in an artery supplying
blood to a part of the brain (Figure 8). As previously mentioned, arrhythmias and heart defects can also
increase the risk of blood clot formation because they disrupt normal blood flow.
Figure 7. Cause of stroke
The most common cause of
stroke is a clot or blockage of
blood vessels to the brain, which
deprives it of oxygen.
Less commonly (20%), stroke can be caused by the rupturing of a blood vessel in the brain, which causes
internal bleeding and results in inadequate blood flow to a part of the brain. Aneurysm rupture is
associated with this cause of stroke, as aneurysms form where blood vessels walls are weakened and
therefore more likely to rupture.
Symptoms of stroke depend on which part of the brain is affected by the lack of blood flow. Most
commonly, weakness occurs on one side of the body, with complete lack of movement and sensation in
a leg or arm. There can be speech problems and a weakness of muscles in the face. Numbing and
tingling sensations are common. Some strokes affect balance, vision, swallowing, breathing, and can
lead to loss of consciousness.
Final 3.0 – 2015-September-17 Page 15 of 20
NPHW Training Manual Module 3
Figure 8. Blood flow problems may that lead to stroke
Remember:
A stroke is the result of oxygen depletion in the brain and can occur due to:
o A clot forming in arteries of the brain (80% of cases)
o The rupturing of a blood vessel in the brain (bleeding; 20% of cases)
3.2.3. Peripheral Vascular Disease
In addition to narrowing arteries of the heart and brain, atherosclerosis can also cause a narrowing of
the arteries in the legs or arms, which limits their blood supply and leads to peripheral vascular disease.
After exercise, or even mild exertion such as walking, a poor blood supply to the arteries in the limbs can
result in pain referred to as claudication. Like angina of the heart, the pain in the limbs is caused by
lactic acid accumulation in the muscles because of poor blood flow (insufficient oxygen supply).
Claudication is relieved by rest. In severe cases of peripheral vascular disease, pain is present at rest and
skin ulcers may develop. Like CHD, angioplasty or arterial bypass surgery treatments are available.
3.2.4. Congestive Heart Failure (CHF)
Heart failure is a condition in which the heart muscles have become very stiff and/or weak. When this
occurs, the heart is unable to pump blood with as much force, and therefore the blood travels through
the body at a slower rate. Due to this impeded blood flow, the pumping of sufficient oxygen and
nutrients is reduced. In order to compensate for this drop, the chambers of the heart can stretch and/or
thicken. While this helps to re-establish sufficient blood flow in the short-term, over time the muscles
can further weaken and become increasingly unable to pump blood efficiently. Heart defects including
valve problems, and arrhythmias such as atrial fibrillation, can also contribute to heart failure because
they decrease the heart’s pumping efficiency and affect blood flow.
Final 3.0 – 2015-September-17 Page 16 of 20
NPHW Training Manual Module 3
The pumping action of the heart extends throughout the entire body and is responsible for pumping
fluids from the extremities (like the arms and legs) back up to the heart so circulation can continue. In
those with CHF, this pumping action is reduced. Lower blood flow results in the body retaining more
fluids. This occurs primarily in the legs, feet, abdomen, and the lungs or other organs. This causes
congestion in the body, which is why it is called congestive heart failure.
CHF can be caused by a number of contributing factors. As in angina, a buildup of plaque on the arteries
supplying blood to the heart can contribute to stiffening and/or weakening of the heart muscles. Also, as
discussed, a heart attack in which the arteries in the heart are blocked causes muscle cells to die from a
lack of oxygen. If a number of muscles cells have died, the ability of the heart to pump blood is reduced,
and can result in CHF. Other impairments to the heart can also contribute to CHF, including genetic
defects, infection or illness-related damage, as well as damage from lifestyle factors like drug use and
excessive alcohol consumption.
Symptoms of CHF include weight gain due to swelling in the ankles and legs (from fluid retention),
fatigue, shortness of breath, trouble lying flat, and weakness due to decreased blood flow. An irregular
heartbeat can also be caused by CHF, as the heart beats faster in an attempt to increase blood flow. A
large number of medications exist to treat CHF, and severe cases can require surgery. One notable
medication is called lasix (or furosemide), which is used to reduce congestion and swelling in the legs.
Remember:
CHF is due to stiffened and/or weakened heart muscles
CHF can cause shortness of breath and swelling of the ankles and legs
Discussion Questions
What conditions can blocked blood vessels lead to?
Why do people with congestive heart failure get swollen legs?
How do arrhythmias and genetic heart defects increase risk of CVD?
Final 3.0 – 2015-September-17 Page 17 of 20
NPHW Training Manual Module 3
Section 3.3: Burden of Cardiovascular Disease
Of all annual deaths around the globe, CVDs are the number one cause, attributable to over 17 million
deaths per year (Figure 9). This number is expected to approach 25 million deaths per year by 2030. CVD
affects half of the world’s population at some point in their lifetime. In low- and middle-income
countries, CVD generally affects people earlier in life, and is becoming increasingly more common at
younger ages.
Figure 9. Causes of deaths globally
(WHO Burden of Disease 2011)
In addition to deaths, CVD contributes to significant global disability, with around 30 million people
surviving a stroke or heart attack every year. CVDs have no geographic, gender, or socio-economic
boundaries. CVDs spread between both rich and poor, resulting in disease in all parts of society. In fact,
more than 80% of CVD occurs in low- and middle-income countries – it is not just a problem for wealthy
countries. As a result, there are a number of socio-economic, socio-cultural, and psychological
implications.
Final 3.0 – 2015-September-17 Page 18 of 20
NPHW Training Manual Module 3
3.3.1. Socio-Economic Burden
CVD is a burden on social and economic interests. CVDs generally occur in a productive age group, and
they often cause premature death and disability. This prevents a part of the work force from being able
to produce the same level of quality and quantity of work as would otherwise be possible. CVDs also
generally require hospital visits, doctor check-ups, and medications, which along with being absent from
work, can cause financial strain.
As discussed in Module 1, diseases have many consequences for the individuals with the disease, their
families, and their communities. There are a number of direct costs that can be attributed to CVDs.
These costs include things like drug costs, hospital fees, doctors and laboratory fees, etc... There are also
a large number of indirect costs, which are a little harder to see but are just as important. These include
things like loss of salary, personal or financial costs to family members that help take care of sick
relatives, and costs of missing work. Furthermore, indirect costs can include socio-cultural costs. These
can be points such as persons not wanting to socialize as much because they cannot consume alcohol,
or feeling excluded from family meals if they have to watch their diet specifically. Cumulatively, these
direct and indirect economic and cultural costs can lead to negative psychological effects, which may
have further socio-economic and socio-cultural implications.
Discussion Question
What are some non-medical problems that may arise in the life of a participant that has CVD?
Final 3.0 – 2015-September-17 Page 19 of 20
NPHW Training Manual Module 3
Module 3 Post-Test
Instructions: Read the following statements carefully and tick [√] the appropriate column. If you are
unsure of any answer you may tick the “Don’t Know” column. The time allotted to you is 5 minutes.
Don’t
Number Question True False
Know
The blood has four main components: platelets, red blood
1
cells, white blood cells, and plasma.
Systole is when the heart is relaxed and diastole is when
2
the heart is contracting.
Blood pressure increases during the systolic phase and
3
decreases during the diastolic phase.
4 A person who has angina will never have a heart attack.
5 Angina is only treated through surgery.
Stroke can have two different causes – bleeding in the
6
brain and a blockage of blood flow to the brain.
Shortness of breath, and swelling of the ankles and legs,
7
are common symptoms of CHF.
In middle and low income countries, CVD most often
8
affects people later in life.
CHD, angina and peripheral vascular disease are caused by
9
atherosclerosis.
Atrial fibrillation and heart valve irregularities decrease the
10 likelihood of CVD because they increase the pumping
efficiency of the heart.
Final 3.0 – 2015-September-17 Page 20 of 20
You might also like
- Integrative Anatomy and Pathophysiology in TCM CardiologyFrom EverandIntegrative Anatomy and Pathophysiology in TCM CardiologyNo ratings yet
- Human Anatomy and Physiology-XBHA2103-Final Exam Answer Paper-16122022Document10 pagesHuman Anatomy and Physiology-XBHA2103-Final Exam Answer Paper-16122022AnandNo ratings yet
- Section Unit Lesson Title Student Learning ObjectivesDocument15 pagesSection Unit Lesson Title Student Learning ObjectivesSoham MultaniNo ratings yet
- Neuro Critical CareDocument101 pagesNeuro Critical Caregliftan67% (3)
- Module 4-6Document7 pagesModule 4-6Eljen Dave CayambaNo ratings yet
- Lesson Plan No 2Document7 pagesLesson Plan No 2hafeez ahmedNo ratings yet
- Transport in Animals - Components of BloodDocument30 pagesTransport in Animals - Components of BloodrekhaNo ratings yet
- Self Learning Packet in Science 9: Learning Plan Prayer/QuoteDocument9 pagesSelf Learning Packet in Science 9: Learning Plan Prayer/QuoteCamille Sison-AlmirolNo ratings yet
- Heart Muscle Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHeart Muscle Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Biology C - Lesson 1 - Circulatory SystemDocument47 pagesBiology C - Lesson 1 - Circulatory SystemMary Jewel0% (1)
- Manual Cardiovascular SystemDocument5 pagesManual Cardiovascular SystemVynz Morales CosepNo ratings yet
- Chapter QuestionsDocument8 pagesChapter QuestionsAric DelinaNo ratings yet
- Practice Worksheets - Cardiac PhysiologyDocument5 pagesPractice Worksheets - Cardiac PhysiologyrickNo ratings yet
- Overview of Cardiovascular System: An Introduction To Chapters 9 - 24 and Chapter 36 Guyton and Hall, 12 EditionDocument10 pagesOverview of Cardiovascular System: An Introduction To Chapters 9 - 24 and Chapter 36 Guyton and Hall, 12 EditionbahahahahNo ratings yet
- Chi Nei Tsang IIIDocument0 pagesChi Nei Tsang IIIDevlinPyx100% (1)
- Respiratory System: VocabularyDocument4 pagesRespiratory System: VocabularyFely NatadNo ratings yet
- Reymart Baguio A. Iii Bsed-Science Module 4 - Fluids and Transport Module Assessment Critical Thinking QuestionsDocument13 pagesReymart Baguio A. Iii Bsed-Science Module 4 - Fluids and Transport Module Assessment Critical Thinking QuestionsReymart Anga Baguio IINo ratings yet
- Heart, Functions, Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHeart, Functions, Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- MF3219Document32 pagesMF3219okundigiecynthiaNo ratings yet
- Praktikum Faal-Blok14-3BDocument18 pagesPraktikum Faal-Blok14-3BKelompok 5A Semester 4No ratings yet
- DAN BLS CPR Student HandbookDocument109 pagesDAN BLS CPR Student HandbookNicole Sue BucatNo ratings yet
- CPT Exam Prep WorkbookDocument63 pagesCPT Exam Prep WorkbookAmethyst Carey100% (1)
- Medical Terminology: Learn to Pronounce, Understand and Memorize Over 2000 Medical TermsFrom EverandMedical Terminology: Learn to Pronounce, Understand and Memorize Over 2000 Medical TermsRating: 5 out of 5 stars5/5 (1)
- Cileni Cortes Camacho AntologiaDocument62 pagesCileni Cortes Camacho AntologiaCileni CortesNo ratings yet
- Measuring Pulse OximeterDocument94 pagesMeasuring Pulse OximeterMuhammed HammadNo ratings yet
- Health Fitness Test ReviewDocument5 pagesHealth Fitness Test ReviewJoshNo ratings yet
- b1 RevisionDocument68 pagesb1 Revisionapi-320022467No ratings yet
- 4.3 Blood VesselsDocument22 pages4.3 Blood VesselsKarlapudi RonakNo ratings yet
- 2023 - Handout - Cardiovascular System - STUDENT'SDocument17 pages2023 - Handout - Cardiovascular System - STUDENT'SmilifacultadfcmNo ratings yet
- 1545Document20 pages1545micjenNo ratings yet
- Latest Cva 1...Document57 pagesLatest Cva 1...eric macabiogNo ratings yet
- Sci9 Q1 W1b Humancirculatorysystem Boslay v2Document23 pagesSci9 Q1 W1b Humancirculatorysystem Boslay v2donaldkarryNo ratings yet
- Lesson 1 - Module 1 - Circulatory SystemDocument27 pagesLesson 1 - Module 1 - Circulatory SystemPapiNo ratings yet
- Module Cardiovascular SystemDocument14 pagesModule Cardiovascular SystemVynz Morales CosepNo ratings yet
- Batimentos Cardiacos e ArritimiaDocument18 pagesBatimentos Cardiacos e ArritimiaDomingos NetoNo ratings yet
- Arrhythmia BrochureDocument19 pagesArrhythmia BrochureSohail LatifNo ratings yet
- 1 Mjh1 / Bio 103/ Assignment/ Spring 20Document6 pages1 Mjh1 / Bio 103/ Assignment/ Spring 20Fahim ZamanNo ratings yet
- DAN BLS CPR FA Student HandbookDocument120 pagesDAN BLS CPR FA Student HandbookYtamar Visbal PerezNo ratings yet
- Cardiovascular System LP AskepDocument25 pagesCardiovascular System LP AskepGusti RiniNo ratings yet
- Human A&P Module 4Document51 pagesHuman A&P Module 4Allan IgbuhayNo ratings yet
- Electronics Digital StethoscopeDocument4 pagesElectronics Digital StethoscopeoyunpurevoyunaaNo ratings yet
- US Army Medical Course MD0853-200 - Hematology IDocument216 pagesUS Army Medical Course MD0853-200 - Hematology IGeorgesNo ratings yet
- Module 3-CDocument8 pagesModule 3-Cfiids.castroNo ratings yet
- Diver First Aid CPRDocument108 pagesDiver First Aid CPREthanBrandtNo ratings yet
- Cardiorespiratory QuestionsDocument12 pagesCardiorespiratory QuestionsKim Oliveri ReedNo ratings yet
- Essential Clinically Applied Anatomy of the Peripheral Nervous System in the Head and NeckFrom EverandEssential Clinically Applied Anatomy of the Peripheral Nervous System in the Head and NeckNo ratings yet
- Grade 9 Science: Self Learning Module (SLM)Document11 pagesGrade 9 Science: Self Learning Module (SLM)MariedelSindayenDelfinadoNo ratings yet
- Hematology in Traditional Chinese Medicine CardiologyFrom EverandHematology in Traditional Chinese Medicine CardiologyNo ratings yet
- Objectives: Circulatory SystemDocument3 pagesObjectives: Circulatory SystemJennifer Padolina-ManluctaoNo ratings yet
- Elementary Science 5E+ Lesson Plan CycleDocument3 pagesElementary Science 5E+ Lesson Plan CyclemuneebrahatNo ratings yet
- HUMAN BODY - Human BodyDocument20 pagesHUMAN BODY - Human BodyBaiq Aluh NurfatimahNo ratings yet
- Lesson Exemplar-Circulatory SystemDocument10 pagesLesson Exemplar-Circulatory SystemRica Manansala IbeNo ratings yet
- Anatomy and Physiology of The HeartDocument22 pagesAnatomy and Physiology of The HeartCarimaGhalie100% (2)
- Smooth Muscle Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSmooth Muscle Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Eucharia Chizoba Klenam Kwoke NnalueDocument5 pagesEucharia Chizoba Klenam Kwoke Nnaluekwoke chizobaNo ratings yet
- Body Systems Lecture NotesDocument10 pagesBody Systems Lecture Notesapi-377297552No ratings yet
- Résumés, Applications, and Cover Letters: 125 YEARSDocument13 pagesRésumés, Applications, and Cover Letters: 125 YEARSkoya patNo ratings yet
- Application Letter PDFDocument1 pageApplication Letter PDFkoya patNo ratings yet
- Résumés, Applications, and Cover Letters: 125 YEARSDocument13 pagesRésumés, Applications, and Cover Letters: 125 YEARSkoya patNo ratings yet
- Psa Bullying PDFDocument12 pagesPsa Bullying PDFkoya patNo ratings yet
- Public Service Announcement About BullyingDocument12 pagesPublic Service Announcement About Bullyingkoya patNo ratings yet
- 2nd Term MCQ TrainingDocument53 pages2nd Term MCQ TrainingMedical ImaginationNo ratings yet
- Circulatory TestDocument7 pagesCirculatory TestgarnetNo ratings yet
- New Med UpdatesDocument88 pagesNew Med UpdatesMangesh ParadkarNo ratings yet
- Liver LecDocument107 pagesLiver LecNMD LIFESAVERNo ratings yet
- Kanski'S: Clinical OphthalmologyDocument504 pagesKanski'S: Clinical OphthalmologyMohin hossain100% (1)
- OSTIALLESIONS Final PDFDocument25 pagesOSTIALLESIONS Final PDFwasimNo ratings yet
- Drug Study: Classification: ANTI-INFECTIVES-QuinolonesDocument36 pagesDrug Study: Classification: ANTI-INFECTIVES-QuinolonesRasheila Palti RNNo ratings yet
- Clinical Surgical 1Document2 pagesClinical Surgical 1Ohana NanaNo ratings yet
- Types of Auto ImmuneDocument3 pagesTypes of Auto ImmuneEdgar PunoNo ratings yet
- Nej Mo A 2208391Document11 pagesNej Mo A 2208391Melchor Alcántara BarreraNo ratings yet
- Listening Scripts: Unit 1Document7 pagesListening Scripts: Unit 1Kami MagNo ratings yet
- All Medical Syndromes 2022Document141 pagesAll Medical Syndromes 2022Fercho MedNo ratings yet
- Hepatorenal Syndrome: Pathophysiology, Diagnosis, and ManagementDocument21 pagesHepatorenal Syndrome: Pathophysiology, Diagnosis, and Managementkonas patklinNo ratings yet
- European Journal of Internal MedicineDocument4 pagesEuropean Journal of Internal Medicinesamer battatNo ratings yet
- Neoreviews 201533Document11 pagesNeoreviews 201533Dmitri KaramazovNo ratings yet
- 2016 Acc Aha HFS Focused Up Date On New Pharmacolical Therapy For Heart FailureDocument13 pages2016 Acc Aha HFS Focused Up Date On New Pharmacolical Therapy For Heart Failuredrjorgetorres4777No ratings yet
- 22q11.2 GPC 2023Document24 pages22q11.2 GPC 2023Antoine NinoNo ratings yet
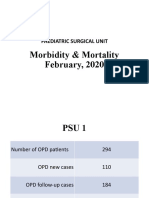
- Morbidity & Mortality (February, 2020)Document14 pagesMorbidity & Mortality (February, 2020)Wai GyiNo ratings yet
- Clinical Manifestations and Diagnosis of Vitamin B12 and Folate Deficiency - UpToDateDocument63 pagesClinical Manifestations and Diagnosis of Vitamin B12 and Folate Deficiency - UpToDateHuỳnh Thị Khả DuyNo ratings yet
- Adult Body Mass Index Bmi ChartDocument2 pagesAdult Body Mass Index Bmi ChartMyo Kyaw KyawNo ratings yet
- Anatomy and Cardiovascular AssessmentDocument52 pagesAnatomy and Cardiovascular AssessmentNaomi Anne AsuntoNo ratings yet
- Anaphy Act 1Document2 pagesAnaphy Act 1TheaNo ratings yet
- Cc1 Lec MidtermsDocument38 pagesCc1 Lec MidtermsOliver Dela CruzNo ratings yet
- 7 Urinary Disorders - 2012 - Small Animal Clinical Diagnosis by Laboratory Methods Fifth EditionDocument30 pages7 Urinary Disorders - 2012 - Small Animal Clinical Diagnosis by Laboratory Methods Fifth EditionNarvarte Hospital Veterinario de EspecialidadesNo ratings yet
- MI Prop - 2Document32 pagesMI Prop - 2M.TennekoonNo ratings yet
- Lithium: Mimicry, Mania, and Muscle Relaxants: Simon Flood MRCP FRCA Andrew Bodenham FRCADocument4 pagesLithium: Mimicry, Mania, and Muscle Relaxants: Simon Flood MRCP FRCA Andrew Bodenham FRCARizwan AhmedNo ratings yet
- Aula 1 - Tracheobronchial BranchingDocument16 pagesAula 1 - Tracheobronchial BranchingThiago StoianovNo ratings yet
- Current Opinion Neurology ED 2019 Zwergal PDFDocument10 pagesCurrent Opinion Neurology ED 2019 Zwergal PDFveronikiNo ratings yet
- ALS Manual 2010.version 1Document84 pagesALS Manual 2010.version 1Elena How100% (1)
- History Taking SurgeryDocument8 pagesHistory Taking SurgeryKingston HoNo ratings yet