Professional Documents
Culture Documents
Endoscopic Optical Enhancement Technologies in IBD
Uploaded by
Trình BiomedicOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endoscopic Optical Enhancement Technologies in IBD
Uploaded by
Trình BiomedicCopyright:
Available Formats
ENDOSCOPIC OPTICAL ENHANCEMENT
TECHNOLOGIES IN IBD
Gian Eugenio Tontini,1,2 Maurizio Vecchi,2,3 Markus F. Neurath,1
Helmut Neumann1
1. Department of Medicine I, University of Erlangen-Nuremberg, Germany
2. Gastroenterology and Digestive Endoscopy Unit, IRCCS Policlinico San Donato,
San Donato Milanese, Italy
3. Department of Biomedical Science for Health, University of Milan, Italy
Disclosure: No potential conflict of interest.
Received: 14.10.13 Accepted: 20.11.13
Citation: EMJ Gastroenterol. 2013;1:54-61.
ABSTRACT
Optical enhancement technologies are emerging as promising tools to improve diagnosis and
clinical management of patients with inflammatory bowel diseases (IBD). The use of dye-based and
dye-less chromoendoscopy may improve either characterisation of mucosal inflammation or detection
of dysplastic and early neoplastic lesions. Confocal laser endomicroscopy and endocytoscopy both
allow for in vivo and real-time microscopic analysis of the tissue. Moreover, the newly introduced
molecular imaging has now also become feasible for in vivo diagnosis in IBD. This review focuses on the
more recent progresses of advanced endoscopic imaging techniques in the setting of IBD and provides
the reader with an updated overview on accepted clinical evidence and ongoing fields of research.
Keywords: Inflammatory bowel disease, Crohn’s disease, ulcerative colitis, colonoscopy, advanced
endoscopic imaging, dye-based chromoendoscopy, dye-less chromoendoscopy, confocal laser
endomicroscopy, molecular imaging, endocytoscopy, surveillance, colorectal cancer.
INTRODUCTION of chronic inflammation are recognised as the
major risk factors of colitis-associated cancer
Crohn’s disease (CD) and ulcerative colitis (CAC).10-12 Therefore, national and international
(UC), the two major entities of inflammatory guidelines strongly recommend colonoscopic
bowel disease (IBD), are gastrointestinal chronic surveillance protocols starting 8-10 years after
disorders that affect more than 1 million people the onset of symptoms, and every 1 to 2 years
in the United States and several million after that in extensive colitis.5,13-16 This strategy is
worldwide.1,2 The intestinal mucosal layer is the aimed at early detection of non-polypoid and
main target of such disorders and represents the
early dysplastic lesions, which are the most
environment where exogenous and host related
reliable biomarker of concomitant or impending
factors mould the immunological background
malignancy.17,18 In 2005, an international consensus
that bears IBD pathogenesis. Accordingly,
conference agreed that a minimum of 32 biopsies
endoscopic imaging has a pivotal role for both
diagnostic and therapeutic issues in patients should be performed at each surveillance
with IBD. Indeed, the differential diagnosis among colonoscopy by obtaining four-quadrant biopsies
IBD entities and other gastrointestinal disorders every 10 cm separately retrieved, plus targeted
is based on clinical evaluation and the combination sampling of macroscopically suspicious lesions.16
of endoscopic, histological, radiologic, and However, this approach has raised several
biochemical results.3-9 Moreover, patients with concerns as it failed to show concrete
either CD or UC are at an increased risk of cost-effectiveness and to cut down the risk of
malignancies as severity, extent, and standing overlooked neoplastic lesions.11,18-27
54 GASTROENTEROLOGY • December 2013 EMJ EUROPEAN MEDICAL JOURNAL
Consistently, growing efforts have been theoretically avoiding the potential carcinogenic
made to improve the efficacy of advanced effect ascribed to the prolonged use of
endoscopic imaging techniques during endoscopic methylene-blue under white-light scanning.49-52
surveillance protocols.26-33 In addition, emerging A meta-analysis of six randomised controlled
evidence has raised increasing attention to a trials demonstrated a pooled sensitivity,
new clinical topic, namely mucosal healing. This specificity and diagnostic odds ratio of 83.3%
includes the precise staging of disease extent (95%-CI=35.9-99.6%), 91.3% (95%-CI=43.8-100%),
and activity, and the mucosal early response to and 17.5% (95%-CI=1.2-247.1), respectively, for
biological therapy.34,35 In this context, advanced dysplasia detection in long-standing UC by using
endoscopic imaging techniques could refine our DBC compared with white-light endoscopy.53
traditional approach of diagnosis in patients with Accordingly, international guidelines have included
IBD and may become the crucial diagnostic test the use of DBC in highly specialised centres to
for more disease-specific and patient-centred improve IBD surveillance protocols [4,13-16].
clinical strategies.36,37 This review describes the Potential limitations that could hamper the use
concept of advanced endoscopic imaging for of DBC in clinical practice include additional
diagnosis and characterisation of patients with costs for the dye and the spraying catheter,
IBD, focusing on the newly introduced optical operator training, and a non-uniform distribution
enhancement technologies. on the mucosal surface.28,33-37 Furthermore, there
is no dye that provides a detailed evaluation of
CHROMOENDOSCOPY the mucosal vascular pattern (MVP), which is
nowadays emerging as an important parameter
Chromoendoscopy uses different staining for neoplasia detection and assessment of
techniques to enhance the mucosal detail and disease activity. 37
submucosal vascular pattern, thereby improving
Dye-Less Chromoendoscopy
the detection of pathological lesions and
enabling a more precise diagnosis.28,36-38 Currently, Recently, dye-less chromoendoscopy (DLC)
chromoendoscopy is distinguished in dye-based techniques have been implemented into daily
and dye-less imaging techniques. routine practice to overcome the above-mentioned
limitations of DBC. By pushing a button on the
Dye-Based Chromoendoscopy
handle of the endoscope, these integrated
Dye-based chromoendoscopy (DBC) refers endoscopic systems enable a detailed
to topical application of dyes at the time of examination of both the mucosal surface and
endoscopy in an effort to enhance tissue the MVP morphology, thereby providing
characterisation, differentiation, and diagnosis.39 high-contrast imaging in real-time and without
Dye spraying techniques were first described in the use of additional equipment. DLC
the 1970s40 and include absorptive agents encompasses optical chromoendoscopy and
(e.g. Lugol’s solution, methylene blue, toluidine digital chromoendoscopy techniques.37
blue, and cresyl violet), contrast agents (e.g. indigo
Optical chromoendoscopy techniques (Narrow
carmine and acetic acid), and reactive staining
Band Imaging or NBI, Olympus, Tokyo, Japan
agents (e.g. congo red and phenol red).28,41 DBC
and Compound Band Imaging or CBI, Aohua,
may allow for an improved diagnosis of disease
Shanghai, China) are based on optical lenses
severity and extent in subjects with IBD. integrated within the light source of the
Nevertheless, DBC has been implemented in endoscope, which narrow the bandwidth of
clinical practice specially to improve detection spectral transmittance.54 In contrast, digital
of dysplastic lesions in long-standing IBD chromoendoscopy (Fujinon Intelligent Color
colitis.21,42-47 In this context it has been estimated Enhancement or FICE, Fujifilm, Tokyo, Japan and
that methylene blue-aided chromoendoscopy i-scan, Pentax, Tokyo, Japan) rests on a digital
yields a 2.2-fold increased dysplasia detection post-processing of endoscopic images made in
rate, particularly due to the enhanced detection real-time by the video processor.37
of non-polypoid lesions.21,47,48 Similar results
have also been shown for indigo carmine-aided As formerly discussed, detection of colorectal
chromoendoscopy;43,46 moreover, indigo carmine dysplasia in IBD is of paramount importance,
has no oxidative damage on DNA chains, thereby being the most reliable biomarker of CAC.17,18
GASTROENTEROLOGY • December 2013 EMJ EUROPEAN MEDICAL JOURNAL 55
Consistently, several studies have recently identified only a common ‘distorted’ MVP.
addressed the potential of DLC, particularly Histopathology revealed that both acute and
NBI, in improving the accuracy and effectiveness chronic signs of microscopic inflammation were
of current surveillance programs in IBD. In a remarkably correlated with the ‘obscure’ MVP
crossover randomised trial in which patients with (p<0.05), while only few signs of chronic
UC underwent both NBI and high-definition (HD) inflammation correlated with the ‘distorted and
white-light colonoscopy, van den Broek and clear’ MVP.60 Additional research from the same
co-workers55 have found that NBI does not group confirmed that MVP’s analysis with NBI
improve the detection of neoplastic lesions. In offers the concrete possibility to predict signs of
addition, NBI proved the suboptimal accuracy acute microscopic inflammation in patients with
(73%) for differentiating neoplastic from quiescent UC.60-63
non-neoplastic mucosa. 55
A further study by
the same group confirmed that NBI has only a Very recently, our group evaluated the potential
moderate accuracy for the prediction of of i-scan to improve the characterisation of
histology (80%).56 mucosal inflammation in IBD.64 During
pancolonoscopy, patients were examined using
Another prospective, randomised, crossover trial both HD white-light (Group A) and HD plus i-scan
compared NBI to DBC with indigo carmine in (Group B). Agreement between endoscopic
60 clinically inactive IBD patients 8 years after the prediction of disease severity and histological
onset of symptoms.57 NBI detected significantly findings was 54% in group A and 90% in group
less false-positive biopsies, sparing time and B (p=0.066). The endoscopic prediction of
yielding an equivalent true-positive rate. the inflammatory activity’s extent was 49%
However, DBC scored slightly better than NBI in group A and 92% in group B (p=0.001)
identifying more neoplastic lesions and more using histology as reference standard, thereby
neoplastic patients (p=0.2), thereby harbouring suggesting that i-scan has the potential to
some concern about the use of this DLC improve both diagnosis of severity and extent
technique as standard surveillance strategy in of mucosal inflammation in patients with IBD.
IBD.56 Assessing the characterisation of early Therefore, this allows for a more precise diagnosis
colorectal lesions in long-standing UC, Matsumoto of mucosal inflammation compared to HD
et al.58 combined NBI with magnification colonoscopy alone.64 Taken together, even if
colonoscopy in a pilot study based on 46 patients. DBC still represents the best choice to improve
According to the modified classification for dysplasia detection in long-standing IBD, optical
‘magnifying chromoscopic findings’ the surface and digital DLC techniques have the potential
pattern of each lesion was defined as ’honeycomb- to better quantify disease activity and
like’, ‘villous’ or ‘tortuous-like’. Dysplasia was mucosal healing, and currently appear as more
positively correlated with the ‘tortuous’ pattern, practical tools to spread into daily routine
therefore suggesting that NBI and magnified clinical practice.
colonoscopy could improve dysplasia detection
during surveillance in UC.58 To the best of our CONFOCAL LASER ENDOMICROSCOPY
knowledge, there are no studies on the use of
digital chromoendoscopy techniques (i.e. i-scan Introduced in 2004, confocal laser
and FICE) for detection and characterisation endomicroscopy (CLE) has rapidly emerged
of intraepithelial neoplasia in IBD. as a promising approach to obtain real-time in
vivo histology in luminal endoscopy as in several
More recently, DLC techniques have shown other clinical fields.65 Briefly, this technique is
promising results for the characterisation of based on tissue illumination with a blue laser
disease extent and activity in patients with light after topical or systemic application of
mild or inactive IBD.37,59 Kudo et al.60 have fluorescence agents. In IBD, various studies have
focused their analysis on MVP comparing HD investigated the potential of CLE for disease
white-light endoscopy and NBI in UC patients by classification and characterisation.21,35,66-76
using histology as the reference standard. NBI
was able to better characterise abnormal vessel In 2007, a study from Kiesslich et al.21 clearly
structures, distinguishing between ‘clear’ and demonstrated that during surveillance of
‘obscure’ MVP where HD white-light endoscopy long-standing UC, the use of DBC-aided CLE
56 GASTROENTEROLOGY • December 2013 EMJ EUROPEAN MEDICAL JOURNAL
could detect 4.75-fold more neoplastic lesions the intestinal lumen identified by CLE is a marker
compared with standard white-light endoscopy. of loss of barrier function, as it implies the
In addition, the authors reported a remarkable inward flow of antigens, toxins and microbes
biopsy sparing and an optimal accuracy (95%) in activating the mucosal immune system.
predicting the presence of neoplastic changes.21 Furthermore, the authors developed a grading
Consistent with this figure, Hurlstone and system (‘Watson grade’) based on three CLE
co-workers76 described a high overall accuracy signs of barrier function impairment such as
(97%) and excellent agreement with histological cell shedding, fluorescein flow into the intestinal
results (κappa=0.91) when using CLE for lumen, and microerosions. The ‘Watson grade’
differentiation of dysplasia-associated lesion was shown to predict the relapse of IBD patients
or mass (DALM) from sporadic adenoma in remission within the subsequent 12 months
(adenoma-like mass; ALM). (Watson grade II/III versus grade I: p<0.001),
harbouring the use of CLE for on demand in vivo
Beyond the characterisation of dysplastic prediction of relapse during ongoing endoscopy.73
changes, confocal imaging could also reveal signs Another pilot study based on both CD and UC
of impaired intestinal barrier function, which is patients with a median follow-up of 14 months
emerging as a crucial step in the pathogenesis has recently confirmed that gap density in
of IBD.68,73,74,77-82 The lining of the intestine endoscopically normal mucosa of the terminal
undergoes a continuous renewal, resulting in ileum is a significant predictor for risk of major
epithelial gaps as a consequence of intestinal events such as hospitalisation or surgery.74
cell shedding.68 A refined process, based on
the redistribution of tight junction round the Moreover, several studies have recently
basolateral surface of the shed cell, preserves established that CLE allows the characterisation of
the barrier function at the gap site.74 When this most microscopic architectural and inflammatory
physiologic process is impaired, the intestinal changes, which are conventionally regarded as
barrier become permeable to the inward flow of histopathological hallmarks for the diagnosis
antigens and microbes from the intestinal lumen of IBD.9,66-72 In a study published in 2012,
into the bowel wall, paving the way to a prompt our group evaluated the feasibility of CLE for
reaction of the immune system.78 Accordingly, it in vivo microscopic diagnosis of disease severity
has been hypothesised that the rate of epithelial in patients with CD.72 Consistent with
cell shedding is increased in patients with IBD.68 histopathological results, CLE showed a sharp
Recently, Liu et al.69 have shown that CLE can distinction between CD and controls based on
be used to quantify in vivo the epithelial gap different rates of the following findings: crypt
density of the terminal ileum during ongoing morphology (number of colonic crypts, crypt
colonoscopy. They confirmed that epithelial gap tortuosity, crypt lumen), microerosions, vascularity,
density is significantly higher in IBD subjects than cellular infiltrate within the lamina propria and
in negative controls. Nonetheless, ulcerative number of goblet cells. In addition, CLE was
pancolitis and severe clinical disease were able to differentiate quiescent from active CD
associated with lower gap densities compared showing a high rate of crypt atrophy in the
with those observed in IBD with limited colitis and former group, as well as control subjects from
with mild-to-moderate clinical disease, thereby quiescent CD, detecting a significant increase
suggesting that gap density does not correlate in crypt and goblet cell number as hallmarks
with disease activity and neither with specific of chronic inflammation.72 Similar results were
IBD entities.69 also shown in another study based on the use of
CLE in patients suffering from UC.71 Both
A further study by Kiesslich and co-workers73 assessment of crypt architecture (irregular
confirmed that CLE can identify cell shedding arrangement, density, dilation, abscess) and
and barrier loss at a microscopic level in real- fluorescein leakage into the crypt lumen with
time. Employing a murine model of cell shedding, CLE showed good correlations with histological
they also demonstrated that an incomplete results (both p<0.001). Moreover, 57% of patients
sealing at the site of cell shedding (‘gap’) can with normal mucosa seen on conventional
result in either outward flow, inward flow or white-light endoscopy (Baron score=0) showed
bidirectional flow. This finding supports the acute inflammation on histology (Geboes index
hypothesis that outward flow of fluorescein into >3), whereas no patients with normal mucosa or
GASTROENTEROLOGY • December 2013 EMJ EUROPEAN MEDICAL JOURNAL 57
with chronic inflammation seen on CLE showed expensive and time-consuming, therefore
acute inflammation on histology. harbouring potential shortcomings that currently
limit its implementation into daily routine
In recent years, CLE has been integrated with clinical practice.
the use of exogenous fluorescently labelled
probes to specifically highlight neoplastic and
ENDOCYTOSCOPY
inflammatory changes on the basis of their
molecular signature; this novel and promising field Endocytoscopy (EC) is another advanced
in gastroenterology is called ‘molecular imaging’.8 imaging technique implemented for in vivo
In a pilot study, Atreya and co-workers35 used microscopic imaging at a magnification up to
CLE-based molecular imaging with monoclonal 1390-fold.86 Based on the principle of contact
anti-tumour necrosis factor (TNF) antibodies to light microscopy, this technique enables the
evaluate whether the therapeutic responses to visualisation of the very superficial mucosal layer
Adalimumab correlate with the amount of mucosal at a cellular and subcellular level.87 EC has
membrane TNF receptor in patients with CD. recently been evaluated in gastrointestinal
The inflamed mucosa was coated with a newly endoscopy, particularly to detect neoplastic
developed fluorescent anti-TNF antibody (FITC- changes in aberrant crypt foci and to differentiate
Adalimumab) during the colonoscopy prior to neoplastic from non-neoplasic colorectal
anti-TNF therapy. Fluorescein expression on lesions.88-90 Our group has recently published
a cellular level was quantified by CLE analysis the results of a pilot study designed to assess
focused on mucosal membrane-bound TNF+ the feasibility of EC in distinguishing single
(mTNF+) cells. During a follow-up period of inflammatory cells in patients with IBD.91 It has
1 year, patients with a great density of mTNF+ been observed that EC enables a sharp
cells showed significantly higher short-term characterisation of several cellular (cell size,
response rates at week 12 (92%) upon subsequent arrangement and density) and subcellular details
anti-TNF therapy as compared to patients with (size and shape of nuclei and nucleus-to-
low amounts of mTNF+ cells (15%). These data cytoplasm ratio). Consistently, EC could reliably
indicate for the first time that in vivo molecular distinguish different inflammatory cells with the
imaging with fluorescent antibodies is feasible following respective sensitivities and specificities:
and safe, and could predict therapeutic responses neutrophilic (60% and 95%), basophilic (74%
to biological treatment, depicting promising and 94%), eosinophilic granulocytes (75% and 91%),
and immediate potential for translational science and lymphocytes (89% and 93%). Furthermore,
and prompting effects on clinical practice.35 intestinal disease activity assessed by EC was
Multiphoton microscopy (MPM) is emerging as perfectly in agreement with histopathological
one of the most important in vivo imaging results (100%).91 Taken together, these data seem
techniques for basic research. In comparison to nominate EC as a new promising method to
with the single photon excitation performed by characterise and assess the severity of mucosal
CLE, MPM uses nonlinear optics, so that various inflammation in IBD.
molecular components can be discriminated
without the need to apply fluorophores. The result CONCLUSION
is a superior effective resolution in thick tissue
samples and an increased penetration depth, Recent technological advances in optical imaging
with images perfectly suited for the acquisition and luminal endoscopy are greatly improving
in 3D.84 One recent article impressively the quality of gastrointestinal imaging, enabling
demonstrated how MPM allows for a well-defined microscopic and molecular analysis in real-time
3D visualisation of pathologic changes in tissue during ongoing endoscopy. Converging lines of
samples from patients with IBD without requiring evidence suggest many promising applications
exogenous fluorophores.85 of these optical advanced imaging techniques in
several IBD clinical settings. DLC is emerging as a
Taken together, CLE appears as a versatile tool practical method to enhance in real-time mucosal
capable of enriching the power of endoscopy, subtle details, thereby potentially improving the
predicting in vivo both several valuable cues detection and characterisation of dysplastic
of histology and the response rate to anti-TNF lesions, as well as the accuracy in assessing
therapy. However, currently CLE is relatively disease activity and extent. CLE and EC allow
58 GASTROENTEROLOGY • December 2013 EMJ EUROPEAN MEDICAL JOURNAL
for real-time in vivo histology during ongoing quantification of specific biochemical processes,
endoscopy with predictable benefits for diagnosis thereby promoting the examination of functional
and surveillance of IBD subjects. The newly data. However, further clinical studies are still
introduced molecular imaging can even overcome required to assess the cost-effectiveness and
the limits of traditional morphological analysis, the best strategies for the correct use of these
driving the endoscopic imaging towards the optical enhanced techniques in clinical practice.
Acknowledgements
Gian Eugenio Tontini has gained a grant from the Italian Group for the study of IBD (IG-IBD) supporting
his research works at the Department of Medicine I, University of Erlangen-Nuremberg, Germany.
REFERENCES
1. Abraham C, Cho JH. Inflammatory bowel detecting colon cancer and/or dysplasia ulcerative colitis. Gastroenterology.
disease. N Engl J Med. 2009;361(121):2066- in patients with inflammatory bowel 2007;132(3):874-82.
78. disease. Cochrane Database Syst Rev. 22. Robertson DJ et al. Colorectal cancer
2. Cominelli F. Inhibition of leukocyte 2006;2:CD000279. in patients under close colonoscopic
trafficking in inflammatory bowel disease. 12. Ullman TA, Itzkowitz SH. surveillance. Gastroenterology.
N Engl J Med. 2013;369(8):775-6. Intestinal inflammation and cancer. 2005;129(1):34-41.
3. Dignass A et al. Second European Gastroenterology. 2011;140(6):1807-16. 23. Rutter M et al. Endoscopic
evidence-based consensus on the 13. Farraye FA et al. AGA technical review appearance of dysplasia in ulcerative
diagnosis and management of ulcerative on the diagnosis and management of colitis and the role of staining. Endoscopy.
colitis part 1: definitions and diagnosis. J colorectal neoplasia in inflammatory 2004;36(12):1109-14.
Crohns Colitis. 2012;6(10):965-90. bowel disease. Gastroenterology. 24. Ransohoff DF et al. Ulcerative
4. Annese V et al. European evidence 2010;138(2):746-74. colitis and colonic cancer. Problems
based consensus for endoscopy in 14. Cairns SR et al. Guidelines for colorectal in assessing diagnostic usefulness of
inflammatory bowel disease. J Crohns cancer screening and surveillance in mucosal dysplasia. Dis Colon Rectum.
Colitis. 2013;7(12):982-1018. moderate and high risk groups. Gut. 1985;28(6):383-8.
5. Van Assche G et al. Second European 2010;59:666-89. 25. Eaden JA et al. How gastroenterologists
evidence-based consensus on the 15. Rex DK et al. American College screen for colonic cancer in ulcerative
diagnosis and management of ulcerative of Gastroenterology guidelines for colitis: an analysis of performance.
colitis part 3: special situations. J Crohns colorectal cancer screening 2009. Am J Gastrointest Endosc. 2000;51(2):123-28.
Colitis. 2013;7(1):1-33. Gastroenterol. 2009;104(3):739-50. 26. Vienne A et al. Low prevalence of
6. Mowat C et al. Guidelines for the 16. Itzkowitz SH, Present DH. Consensus colonoscopic surveillance of inflammatory
management of inflammatory bowel conference: Colorectal cancer screening bowel disease patients with longstanding
disease in adults. Gut. 2011;60(5):571-607. and surveillance in inflammatory extensive colitis: a clinical practice survey
7. Lichtenstein GR et al. Practice bowel disease. Inflamm Bowel Dis. nested in the CESAME cohort. Aliment
Parameters Committee of American 2005;11(3):314-21. Pharmacol Ther. 2011;34(2):188-95.
College of Gastroenterology. 17. Goldmann H. Significance and 27. Ullman TA et al. Biopsy specimen
Management of Crohn’s disease in adults. detection of dysplasia in chronic colitis. numbers in the routine practice of
Am J Gastroenterol. 2009;104(2):465-83. Cancer. 1996;78(11):2261–3. surveillance colonoscopy in ulcerative
8. Kornbluth A, Sachar DB, Practice 18. Rubin CE et al. DNA aneuploidy colitis (UC).Gastroenterology.
Parameters Committee of the American in colonic biopsies predicts future 2004;126:471.
College of Gastroenterology. Ulcerative development of dysplasia in ulcerative 28. Kiesslich R, Neurath MF.
colitis practice guidelines in adults: colitis. Gastroenterology. 1992;103(5):1611- Chromoendoscopy in inflammatory
American College Of Gastroenterology, 20. bowel disease. Gastroenterol Clin North
Practice Parameters Committee. Am 19. Rutter MD et al. Thirty-year analysis Am. 2012;41(2):291-302.
J Gastroenterol. 2010;105(3):501- of a colonoscopic surveillance program 29. Bernstein CN. The color of the
23. Erratum in Am J Gastroenterol. for neoplasia in ulcerative colitis. most effective tool to use in dysplasia
2010;105(3):500. Gastroenterology. 2006;130(4):1030-8. surveillance in inflammatory bowel
9. Magro F et al. European consensus on 20. Leung K et al. Ongoing colorectal disease. Gastrointest Endosc.
the histopathology of inflammatory bowel cancer risk despite surveillance 2011;74(4):849-51.
disease. J Crohns Colitis. 2013;7(10):827- colonoscopy: The Polyp Prevention Trial 30. Efthymiou M et al. Cancer surveillance
51. Continued Follow-up Study. Gastrointest strategies in ulcerative colitis: the need
10. Eaden JA et al. The risk of colorectal Endosc. 2010;71(1):111–7. for modernization. Inflamm Bowel Dis.
cancer in ulcerative colitis: a meta- 21. Kiesslich R et al. Chromoscopy-guided 2011;17(8):1800-13.
analysis. Gut. 2001;48:526-35. endomicroscopy increases the diagnostic 31. Bessissow T, Bisschops R. Advanced
11. Collins PD et al. Strategies for yield of intraepithelial neoplasia in endoscopic imaging for dysplasia
GASTROENTEROLOGY • December 2013 EMJ EUROPEAN MEDICAL JOURNAL 59
surveillance in ulcerative colitis. Expert targeted biopsies are superior to standard Gastrointest Endosc. 2007;66(5):957-65.
Rev Gastroenterol Hepatol. 2013;7(1):57- colonoscopic surveillance for detecting 59.Tontini GE et al. Advanced endoscopic
67. dysplasia in inflammatory bowel disease imaging techniques in Crohn’s disease.
32. Ullman TA. Chromoendoscopy should patients: a prospective endoscopic trial. J Crohns Colitis 2013;doi:10.1016/j.
be the standard method and more widely Am J Gastroenterol. 2008;103(9):2342-9. crohns.2013.09.004. [Epub ahead of
used for cancer surveillance colonoscopy 46. Rutter MD et al. Pancolonic indigo print].
in ulcerative colitis. Inflamm Bowel Dis. carmine dye spraying for the detection 60. Kudo T et al. Mucosal vascular pattern
2007;13(10):1273-4. of dysplasia in ulcerative colitis. Gut. in ulcerative colitis: observations using
33. Kiesslich R, Neurath MF. 2004;53(2):256-60. narrow band imaging colonoscopy
Chromoendoscopy: an evolving standard 47. Kiesslich R et al. Methylene blue aided with special reference to histologic
in surveillance for ulcerative colitis. chromoendoscopy for the detection of inflammation. Int J Colorectal Dis.
Inflamm Bowel Dis. 2004;10(5):695-6. intraepithelial neoplasia and colon cancer 2009;24(5):495-501.
34. Neurath MF, Travis SP. Mucosal in ulcerative colitis. Gastroenterology. 61. Matsumoto T et al. Magnifying NBI
healing in inflammatory bowel diseases: 2003;124(4):880-8. colonoscopic findings in ulcerative colitis.
a systematic review. Gut. 2012;61(11):1619- 48. East JE et al. Magnification pan- Stomach Intestine. 2007;42:877-81.
35. chromoendoscopy remains the mainstay 62. Matsumoto T et al. Autofluorescence
35. Atreya R et al. In vivo molecular imaging for colitis dysplasia detection and imaging colonoscopy in ulcerative colitis:
using fluorescent anti-TNF antibodies and differentiation. Gastroenterology. comparison with conventional and
confocal laser endomicroscopy predicts 2007;133(1):366-7. narrow-band imaging colonoscopy. Dig
response to anti-TNF therapy in Crohn’s 49. Olliver JR et al. Chromoendoscopy Endosc. 2007;19:139-44.
disease patients. Nature Medicine 2013. with methylene blue and associated DNA 63. Esaki M et al. Endoscopic findings
[In press]. damage in Barrett’s oesophagus. Lancet. under narrow band imaging colonoscopy
36. Neumann H et al. New endoscopic 2003; 362(9381):373-4. in ulcerative colitis. Dig Endosc. 2011;1:140-
approaches in IBD. World J Gastroenterol. 50. Hardie LJ et al. Chromoendoscopy 2.
2011;17(1):63-8. with methylene blue and the risk 64. Neumann H et al. Virtual
37. Tontini GE et al. Review of DNA damage. Gastroenterology. chromoendoscopy for prediction of
article: newer optical and digital 2004;126(2):623; author reply 623-4. severity and disease extent in patients
chromoendoscopy techniques vs. dye- 51. Davies J et al. Methylene blue with inflammatory bowel disease: a
based chromoendoscopy for diagnosis but not indigo carmine causes DNA randomized controlled study. Inflamm
and surveillance in inflammatory bowel damage to colonocytes in vitro and in Bowel Dis. 2013;19(9):1935-42.
disease. Aliment Pharmacol Ther. 2013; vivo at concentrations used in clinical 65. Neumann H et al. Confocal laser
38(10):1198-208. chromoendoscopy. Gut. 2007;56(1):155-6. endomicroscopy: technical advances and
38. Neumann H et al. Advanced 52. Dinis-Ribeiro M, Moreira-Dias L. There clinical applications. Gastroenterology.
endoscopic imaging for diagnosis of is no clinical evidence of consequences 2010;139(2):388-92.
Crohn’s disease. Gastroenterol Res Pract. after methylene blue chromoendoscopy. 66. Watanabe O et al. Confocal
2012;2012:301541. Gastrointest Endosc. 2008;67(7):1209. endomicroscopy in patients with
39. Wong Kee Song LM et al. 53. Wu L et al. The diagnostic accuracy ulcerative colitis. J Gastroenterol Hepatol.
ASGE Technology Committee. of chromoendoscopy for dysplasia in 2008;2:S286-90.
Chromoendoscopy. Gastrointest Endosc. ulcerative colitis: meta-analysis of six 67. Krauss E et al. Characterization of
2007;66(4):639-49. randomized controlled trials. Colorectal lymphoid follicles with red ring signs
40. Tada M et al. On the dye spraying Dis. 2012;14(4):416-20. as first manifestation of early Crohn’s
method in colonofibreoscopy. Endoscopy. 54. Kuznetsov K et al. Narrow−band disease by conventional histopathology
1977;8(2):70-4. imaging: potential and limitations. and confocal laser endomicroscopy. Int J
41. Canto MI. Staining in gastrointestinal Endoscopy. 2006;38(1):76-81. Clin Exp Pathol. 2012;5(5):411-21.
endoscopy: the basics. Endoscopy. 55. van den Broek FJ et al. Narrow-band 68. Liu JJ et al. Mind the gaps: confocal
1999;31(6):479-86. imaging versus high-definition endoscopy endomicroscopy showed increased
42. Subramanian V et al. Meta-analysis: for the diagnosis of neoplasia in ulcerative density of small bowel epithelial gaps
the diagnostic yield of chromoendoscopy colitis. Endoscopy. 2011;43(2):108-15. in inflammatory bowel disease. J Clin
for detecting dysplasia in patients with Gastroenterol. 2011;45(3):240-5.
56. van den Broek FJ et al. Endoscopic
colonic inflammatory bowel disease. tri-modal imaging for surveillance in 69. Liu JJ et al. Increased epithelial
Aliment Pharmacol Ther. 2011;33(3):304- ulcerative colitis: randomised comparison gaps in the small intestines of patients
12. of high-resolution endoscopy and with inflammatory bowel disease:
43. Hurlstone DP et al. Indigo autofluorescence imaging for neoplasia density matters. Gastrointest Endosc.
carmine-assisted high-magnification detection; and evaluation of narrow-band 2011;73(6):1174-80.
chromoscopic colonoscopy for the imaging for classification of lesions. Gut. 70. Trovato C et al. Confocal laser
detection and characterisation of 2008;57(8):1083-9. endomicroscopy for the detection of
intraepithelial neoplasia in ulcerative 57. Pellisé M et al. Narrow-band imaging mucosal changes in ileal pouch after
colitis: a prospective evaluation. as an alternative to chromoendoscopy restorative proctocolectomy. Dig Liver
Endoscopy. 2005;37(12):1186-92. for the detection of dysplasia in long- Dis. 2009;41(8):578-85.
44. Hurlstone DP et al. Further validation standing inflammatory bowel disease: a 71. Li CQ et al. Classification of
of high-magnification chromoscopic prospective, randomized, crossover study. inflammation activity in ulcerative colitis
colonoscopy for the detection of Gastrointest Endosc. 2011;74(4):840-8. by confocal laser endomicroscopy. Am J
intraepithelial neoplasia and colon cancer 58. Matsumoto T et al. Magnifying Gastroenterol. 2010;105(6):1391-6.
in ulcerative colitis. Gastroenterology. colonoscopy with narrow band imaging 72. Neumann H et al. Assessment of
2004;126(1):376-8. system for the diagnosis of dysplasia Crohn’s disease activity by confocal laser
45. Marion JF et al. Chromoendoscopy- in ulcerative colitis: a pilot study. endomicroscopy. Inflamm Bowel Dis.
60 GASTROENTEROLOGY • December 2013 EMJ EUROPEAN MEDICAL JOURNAL
2012;18(12):2261-9. inflammatory bowel diseases. Inflamm 86. Neumann H et al. Review article: in
73. Kiesslich R et al. Local barrier Bowel Dis. 2011;17(1):362-81. vivo imaging by endocytoscopy. Aliment
dysfunction identified by confocal 79. Meddings J. The significance Pharmacol Ther. 2011;33(11):1183-93.
laser endomicroscopy predicts relapse of the gut barrier in disease. Gut. 87. Neumann H, Kiesslich R.
in inflammatory bowel disease. Gut. 2008;57(4):438e40. Endomicroscopy and endocytoscopy
2012;61(8):1146-53. 80. Wyatt J et al. Intestinal permeability in IBD. Gastrointest Endosc Clin N Am.
74. Turcotte JF et al. Increased epithelial and the prediction of relapse in Crohn’s 2013;23(3):695-705.
gaps in the small intestine are predictive disease. Lancet. 1993;341:1437e9.
88. Pohl H et al. Endocytoscopy for the
of hospitalization and surgery in patients 81. Marchiando AM et al. The epithelial
with inflammatory bowel disease. Clin detection of microstructural features
barrier is maintained by in vivo tight
Transl Gastroenterol. 2012;3:e19. in adult patients with celiac sprue: a
junction expansion during pathologic
prospective, blinded endocytoscopy-
75. van den Broek FJ et al. Pilot intestinal epithelial shedding.
Gastroenterology. 2011;140(4):1208e18. conventional histology correlation study.
study of probe-based confocal laser
endomicroscopy during colonoscopic Gastrointest Endosc. 2009;70(5):933-41.
82. Su L et al. Targeted epithelial tight
surveillance of patients with longstanding junction dysfunction causes immune 89. Cipolletta L et al. Endocytoscopy can
ulcerative colitis. Endoscopy. activation and contributes to development identify dysplasia in aberrant crypt foci
2011;43(2):116-22. of experimental colitis. Gastroenterology. of the colorectum: a prospective in vivo
76. Hurlstone DP et al. Confocal 2009;136(2):551-63. study. Endoscopy. 2009;41(2):129-32.
endomicroscopy in ulcerative colitis: 83. Atreya R, Goetz M. Molecular 90. Neumann H et al. Image of the month.
differentiating dysplasia-associated imaging in gastroenterology. Nat Rev Endocytoscopy-based detection of focal
lesional mass and adenoma-like mass. Clin Gastroenterol Hepatol. 2013;doi: 10.1038/ high-grade intraepithelial neoplasia
Gastroenterol Hepatol. 2007;5(10):1235- nrgastro.2013.125. [Epub ahead of print]. in colonic polyps. Clin Gastroenterol
41. 84. Zipfel WR et al. Nonlinear Hepatol. 2011;9(2):e13.
77. Su L et al. TNFR2 activates MLCK- magic: multiphoton microscopy in
dependent tight junction dysregulation to 91. Neumann H et al. Endocytoscopy
the biosciences. Nat Biotechnol.
cause apoptosis-mediated barrier loss and 2003;21(11):1369-77. allows accurate in vivo differentiation of
experimental colitis. Gastroenterology. mucosal inflammatory cells in IBD: a pilot
85. Schürmann S et al. Label-free
2013;145(2):407-15. study. Inflamm Bowel Dis. 2013;19(2):356-
imaging of inflammatory bowel
78. Salim SY, Söderholm JD. Importance disease using multiphoton microscopy. 62.
of disrupted intestinal barrier in Gastroenterology. 2013;145(3):514-6.
GASTROENTEROLOGY • December 2013 EMJ EUROPEAN MEDICAL JOURNAL 61
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- A List of Prioritized Nursing DiagnosisDocument3 pagesA List of Prioritized Nursing DiagnosisRica DiazNo ratings yet
- AccuRay D5 - 6 Service&Installation Manual - E-5 - ' - 20190515-1 - º ¡Document209 pagesAccuRay D5 - 6 Service&Installation Manual - E-5 - ' - 20190515-1 - º ¡Trình BiomedicNo ratings yet
- Most ImportantDocument3 pagesMost ImportantVenkata Ramana Murthy Vasupilli100% (1)
- Handbook of Diabetes Technology 2019 PDFDocument125 pagesHandbook of Diabetes Technology 2019 PDFPradeep100% (1)
- Natural History of DiseaseDocument31 pagesNatural History of Diseasegabo dasNo ratings yet
- Nursing Practice I: Foundation of Nursing Practice Situation: Nursing IsDocument84 pagesNursing Practice I: Foundation of Nursing Practice Situation: Nursing Isiyoda_05100% (5)
- Affidavit: For Palarong Pambansa OnlyDocument12 pagesAffidavit: For Palarong Pambansa Onlyanno domini67% (3)
- Cac Ham ExcelDocument206 pagesCac Ham ExcelTrình BiomedicNo ratings yet
- CL-50 Plus Product Brochure-TADocument2 pagesCL-50 Plus Product Brochure-TATrình BiomedicNo ratings yet
- Công Cụ Quản Lí Rủi Ro Cho Bệnh ViệnDocument63 pagesCông Cụ Quản Lí Rủi Ro Cho Bệnh ViệnTrình BiomedicNo ratings yet
- Product Data - Accuray D6Document6 pagesProduct Data - Accuray D6Trình BiomedicNo ratings yet
- DR CatalogueDocument2 pagesDR CatalogueTrình BiomedicNo ratings yet
- HTI CL-500 Urine Analyzer: Quality Products and Service For Healthcare ProfessionalsDocument2 pagesHTI CL-500 Urine Analyzer: Quality Products and Service For Healthcare ProfessionalsTrình BiomedicNo ratings yet
- Micra MC1VR01 SpecDocument3 pagesMicra MC1VR01 SpecTrình BiomedicNo ratings yet
- CL-50 Plus Product Brochure-TADocument2 pagesCL-50 Plus Product Brochure-TATrình BiomedicNo ratings yet
- Euroanaesthesia 2015 Abstract BookDocument481 pagesEuroanaesthesia 2015 Abstract BookTrình BiomedicNo ratings yet
- Elisee 350 Product Brochure EngDocument4 pagesElisee 350 Product Brochure EngWidad Mardin Mas JayaNo ratings yet
- Nephro Gudie For HODocument22 pagesNephro Gudie For HOSarmad AsifNo ratings yet
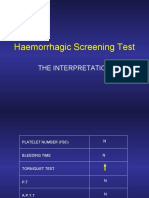
- Haemorrhagic Screening Test: The InterpretationDocument40 pagesHaemorrhagic Screening Test: The InterpretationAngel 冯晓君No ratings yet
- MoclodemideDocument1 pageMoclodemideArnzz AgbulosNo ratings yet
- Bala Murugan E - , MSC Nursing AIIMSDocument33 pagesBala Murugan E - , MSC Nursing AIIMSBalaMuruganNo ratings yet
- Labeling of The Normal Newborn at Risk, High Risk, Sick Client - GARBOSA, RMDocument4 pagesLabeling of The Normal Newborn at Risk, High Risk, Sick Client - GARBOSA, RMRej Garbosa100% (1)
- Model Answer: Important Instructions To ExaminersDocument31 pagesModel Answer: Important Instructions To Examinersmannuu00No ratings yet
- Pain Management, The Veterinary Technicians PerspectyveDocument14 pagesPain Management, The Veterinary Technicians PerspectyveClínica Veterinaria TODOVETNo ratings yet
- Logbook GIDocument15 pagesLogbook GIAna BorodinaNo ratings yet
- HazradDocument16 pagesHazradPhan AnNo ratings yet
- TOG Evolution in Screening For Down SyndromeDocument7 pagesTOG Evolution in Screening For Down SyndromeMarNo ratings yet
- Leo PlusDocument2 pagesLeo PluskbrinaldiNo ratings yet
- IvpDocument18 pagesIvpFranz SalazarNo ratings yet
- Infectious Agent Reservoir Portal of Exit Mode of Transmission Portal of Entry Susceptible HostDocument8 pagesInfectious Agent Reservoir Portal of Exit Mode of Transmission Portal of Entry Susceptible HostAldren BeliberNo ratings yet
- Burn Injury Differential DiagnosisDocument1 pageBurn Injury Differential DiagnosisAjay PhilipNo ratings yet
- Cassava Manioc HydroxiCoumarin - Scopoletin Suppresses Activation of Dendritic Cells and Pathogenesis of Experimental Autoimmune Encephalomyelitis by Inhibiting NF-κB SignalingDocument14 pagesCassava Manioc HydroxiCoumarin - Scopoletin Suppresses Activation of Dendritic Cells and Pathogenesis of Experimental Autoimmune Encephalomyelitis by Inhibiting NF-κB SignalingMiguel AngelNo ratings yet
- Neurocritical Care in The General Intensive Care UnitDocument17 pagesNeurocritical Care in The General Intensive Care UnitdanielNo ratings yet
- Polycystic Ovary Syndrome: Under Supervision ofDocument7 pagesPolycystic Ovary Syndrome: Under Supervision ofHend HamedNo ratings yet
- International HIV & AIDS Charity Donate Fundraising About AVERT AIDS Projects Help & Advice Contact Us Facebook NewsletterDocument22 pagesInternational HIV & AIDS Charity Donate Fundraising About AVERT AIDS Projects Help & Advice Contact Us Facebook NewsletterbasmashaddadNo ratings yet
- Diagnosis and Management of Late-Life Unipolar Depression - UpToDateDocument60 pagesDiagnosis and Management of Late-Life Unipolar Depression - UpToDatearthur argantaraNo ratings yet
- NURS FPX 6212 Assessment 2 Executive SummaryDocument4 pagesNURS FPX 6212 Assessment 2 Executive SummaryCarolyn HarkerNo ratings yet
- EndocrinoDocument15 pagesEndocrinoMichelle ElizaldeNo ratings yet
- CV-Alfred - AgaDocument6 pagesCV-Alfred - AgaAgostin CukajNo ratings yet
- Ce Lenk 2013Document4 pagesCe Lenk 2013RajabSaputraNo ratings yet