Professional Documents
Culture Documents
Aldehyde Dehydrogenase Inhibitor Disulfiram
Uploaded by
Sri SriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aldehyde Dehydrogenase Inhibitor Disulfiram
Uploaded by
Sri SriCopyright:
Available Formats
Aldehyde dehydrogenase inhibitor Disulfiram
It inhibits the enzyme aldehyde dehydrogenase probably after conversion into active metabolites. When alcohol is
ingested after taking disulfiram, the concentration of acetaldehyde in tissues and blood rises and a number of highly
distressing symptoms (aldehyde syndrome) are produced promptly. These are—flushing, burning sensation, throbbing
headache, perspiration, uneasiness, tightness in chest, dizziness, vomiting, visual disturbances, mental confusion, postural
fainting and circulatory collapse. Duration of the syndrome (1–4 hours) depends on the amount of alcohol consumed.
Because of risk of severe reaction, disulfiram is to be used with great caution, only in well-motivated subjects. Disulfiram
aversion therapy is indicated in abstinent subjects who sincerely desire to leave the habit. After making sure that the
subject has not taken alcohol in the past 12 hours, disufiram is given at a dose of 500 mg/day for one week followed by 250
mg daily. Sensitization to alcohol develops after 2–3 hours of first dose, reaches its peak at ~12 hours and lasts for 7–14
days after stopping it, because inhibition of aldehyde dehydrogenase with disulfiram is irreversible: synthesis of fresh
enzyme is required for return of activity. The subject’s resolve not to drink is reinforced by the distressing symptoms that
occur if he drinks a little bit. The subject should be cautioned to avoid alcohol altogether. Disulfiram should not be used in
patients who are physically dependent on alcohol. Side effects of disulfiram (as such) are infrequent, include rashes,
metallic taste, nervousness, malaise and abdominal upset. It inhibits a number of other enzymes as well including alcohol
dehydrogenase, dopamine β hydroxylase and several cytochrome P450 isoenzymes. Thus, it prolongs t½ of many drugs.
ESPERAL, ANTADICT, DEADICT 250 mg tab. (internationally marketed as ANTABUSE)
(Methanol, Wood alcohol) Methyl alcohol is added to industrial rectified spirit to render it unfit for drinking. It is only of
toxicological importance. Mixing of methylated spirit with alcoholic beverages by bootlegers or its inadvertent ingestion
results in methanol poisoning. Methanol is metabolized to formaldehyde and formic acid by alcohol and aldehyde
dehydrogenases respectively (Fig. 28.1), but the rate is 1 /7th that of ethanol. Like ethanol, metabolism of methanol also
follows zero order kinetics and t½ of 20–60 hours has been measured.
Methanol also is a CNS depressant, but less inebriating than ethanol. Toxic
effects of methanol are largely due to formic acid, since its further
metabolism is slow and folate dependent. A blood level of >50 mg/dl
methanol is associated with severe poisoning. Even 15 ml of methanol has
caused blindness and 30 ml has caused death; fatal dose is regarded to be
75–100 ml. Manifestations of methanol poisoning are vomiting, headache,
epigastric pain, uneasiness, drunkenness, disorientation, tachypnoea,
dyspnoea, bradycardia and hypotension. Delirium and seizures may occur
and the patient may suddenly pass into coma. Acidosis is prominent and
entirely due to production of formic acid. The specific toxicity of formic acid
is retinal damage. Blurring of vision, congestion of optic disc followed by
blindness always precede death which is due to respiratory failure.
Treatment 1. Keep the patient in a quiet, dark room; protect the eyes from
light. 2. Gastric lavage with sod. bicarbonate if the patient is brought within
2 hours of ingesting methanol lg . Supportive measures to maintain
ventilation and BP should be instituted. 3. Combat acidosis by i.v. Sod.
bicarbonate infusion. This is the most important measure; prevents retinal damage and other symptoms; large quantities
may be needed. 4. Pot. chloride infusion is needed only when hypokalemia occurs due to alkali therapy. 5. Ethanol is
preferentially metabolized by alcohol dehydrogenase over methanol. At a concentration of 100 mg/dl in blood it saturates
alcohol dehydrogenase and retards methanol metabolism. This helps by reducing the rate of generation of formaldehyde
and formic acid. Ethanol (10% in water) is administered through a nasogastric tube; loading dose of 0.7 ml/kg is followed
by 0.15 ml/kg/hour. Because pharmacokinetics of alcohol changes over time and no i.v. formulation is available,
maintenance of a fixed concentration is difficult. Alcohol blood level needs to be repeatedly measured. Moreover, the
enzyme saturating concentration of ethanol itself produces intoxication and can cause hypoglycaemia. Use of ethanol for
this purpose is tricky. Treatment has to be continued for several days because the sojourn of methanol in body is long. 6.
Haemodialysis: clears methanol as well as formate and hastens recovery. 7. Fomepizole (4-methylpyrazole) is a specific
inhibitor of alcohol dehydrogenase and the drug of choice for methanol poisoning by retarding its metabolism. A loading
dose of 15 mg/kg i.v. followed by 10 mg/kg every 12 hours till serum methanol falls below 20 mg/dl, has been found
effective and safe. It has several advantages over ethanol, viz. longer t½ and lack of inebriating action, but is not available
commercially in India. 8. Folate therapy: Calcium leucovorin 50 mg injected 6 hourly has been shown to reduce blood
formate levels by enhancing its oxidation. This is a promising adjuvant approach.
You might also like
- AlcoholsDocument23 pagesAlcoholsdhaineyNo ratings yet
- Pharma Katzung - AlcoholsDocument5 pagesPharma Katzung - AlcoholsJoshua RemonNo ratings yet
- AlcoholDocument20 pagesAlcoholrecklesspeshal2058100% (1)
- Fpgee SummaryDocument23 pagesFpgee Summaryzxcasdqwe123No ratings yet
- Pharmacology of Alcohol Management of Chronic Alcoholism Treatment of Alcoholic Liver DiseasesDocument41 pagesPharmacology of Alcohol Management of Chronic Alcoholism Treatment of Alcoholic Liver DiseasesVarsha Shende Khobragade100% (2)
- Sodium BicarbonateDocument8 pagesSodium BicarbonateRaf AylaniNo ratings yet
- A Little BookDocument75 pagesA Little Bookfati_cenNo ratings yet
- 3 Composites PDFDocument14 pages3 Composites PDFKavya ulliNo ratings yet
- Pharmacology 2 NotesDocument18 pagesPharmacology 2 NotesAnna ConigraveNo ratings yet
- Practical Approach To Electron Beam Dosimetry at Extended SSDDocument10 pagesPractical Approach To Electron Beam Dosimetry at Extended SSDAhmet Kürşat ÖzkanNo ratings yet
- HMPE1 (Catering MGT.)Document17 pagesHMPE1 (Catering MGT.)Rysyl Mae MoquerioNo ratings yet
- ALCOHOL Pharmacology: Samuel Murano. Dept. of PharmacologyDocument23 pagesALCOHOL Pharmacology: Samuel Murano. Dept. of PharmacologyGideon K. MutaiNo ratings yet
- Methanol ToxicityDocument9 pagesMethanol Toxicityalaamed100% (3)
- The AlcoholsDocument22 pagesThe Alcoholsdr.ramyaravichandarNo ratings yet
- Alcohols & Glycols: Prepared By: Rawan ShamsDocument41 pagesAlcohols & Glycols: Prepared By: Rawan ShamsAhmad AltarefeNo ratings yet
- Alcohol by Dr. SibbalucaDocument4 pagesAlcohol by Dr. SibbalucaRobin TolentinoNo ratings yet
- Medind Nic inDocument8 pagesMedind Nic inSyukron FadillahNo ratings yet
- Alcohol: V Sem KMC IcDocument22 pagesAlcohol: V Sem KMC IcbosepharmaNo ratings yet
- Methanol ToxicityDocument75 pagesMethanol ToxicitySyNo ratings yet
- Why To Study Alcohols in Pharmacology?Document4 pagesWhy To Study Alcohols in Pharmacology?Ronald DarwinNo ratings yet
- Volatile PoisoningDocument21 pagesVolatile Poisoningد.عبدالله الهاديNo ratings yet
- Resentation On Lcohol: Presented by ElissyDocument12 pagesResentation On Lcohol: Presented by ElissyElissy HlawnmualNo ratings yet
- MethanolDocument4 pagesMethanolvinneth vineethNo ratings yet
- Dr. Hisham Zein Elabdin: Alcohols Ethyl Alcohol (Ethanol)Document11 pagesDr. Hisham Zein Elabdin: Alcohols Ethyl Alcohol (Ethanol)Asia AlhkeemNo ratings yet
- Alcohols: Pharmacological ActionDocument5 pagesAlcohols: Pharmacological ActionMuhammad AbbasNo ratings yet
- 3 - Toxicity of AlcoholsDocument22 pages3 - Toxicity of AlcoholsxIRONxWOLFxNo ratings yet
- Alcohol ToxicityDocument81 pagesAlcohol ToxicityKarim RezaNo ratings yet
- Mrcpch-Pharma: Acute Aspirin OverdoseDocument15 pagesMrcpch-Pharma: Acute Aspirin OverdoseRajiv KabadNo ratings yet
- Toksisitas Alkohol Dan Penanganannya PDFDocument9 pagesToksisitas Alkohol Dan Penanganannya PDFvivi novitaliaNo ratings yet
- Ethanol ACUTE and Chronic IntoxicationDocument44 pagesEthanol ACUTE and Chronic IntoxicationMagda MagNo ratings yet
- Volatile PoisonsDocument23 pagesVolatile PoisonshaidaraalkhafajiNo ratings yet
- PHARMACOLOGYDocument69 pagesPHARMACOLOGYKiran ShahNo ratings yet
- Alcohol and DisulfiramDocument13 pagesAlcohol and DisulfiramDivyaNo ratings yet
- Acute Alcohol ToxicityDocument18 pagesAcute Alcohol Toxicityping pongNo ratings yet
- AlcoholDocument5 pagesAlcoholShubham TarapureNo ratings yet
- Cosopt PiDocument11 pagesCosopt PiMaria SpatariNo ratings yet
- Non Essential IonsDocument6 pagesNon Essential Ionsh1iraqNo ratings yet
- Methanol Poisoning OverviewDocument5 pagesMethanol Poisoning OverviewDya AndryanNo ratings yet
- Alcohol Pharmacology Siju Prakash Assistant ProfessorDocument29 pagesAlcohol Pharmacology Siju Prakash Assistant ProfessorFuckyouNo ratings yet
- Uspi LomotilDocument8 pagesUspi LomotilhaiduvnNo ratings yet
- Re-Treatment With Ethambutol After Toxic Optic Neuropathy: Fachria JumahDocument42 pagesRe-Treatment With Ethambutol After Toxic Optic Neuropathy: Fachria JumahfahriajumiahNo ratings yet
- Sign, Sypmtoms and Tretment of PosioningDocument18 pagesSign, Sypmtoms and Tretment of PosioningmaryamNo ratings yet
- STEROGYL 15A and 15H: ErgocalciferolDocument3 pagesSTEROGYL 15A and 15H: ErgocalciferolkcstincasNo ratings yet
- Group 6: Neñeria, Sharla Marsh: Methanol PoisoningDocument3 pagesGroup 6: Neñeria, Sharla Marsh: Methanol PoisoningStephanie Guibone QuiaoNo ratings yet
- ALCHOLDocument15 pagesALCHOLHashim MohammedNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument6 pagesDr. Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- Management of Alcohol IntoxicationDocument8 pagesManagement of Alcohol IntoxicationJyoti Kumari sharmaNo ratings yet
- Ethylene Glycol: DR Keli Med III Lectures 2013Document24 pagesEthylene Glycol: DR Keli Med III Lectures 2013theintrov100% (1)
- Alcoholics QuizDocument54 pagesAlcoholics QuizChitra K LakshmanNo ratings yet
- Alcohol Toxicity and Withdrawal SyndromeDocument65 pagesAlcohol Toxicity and Withdrawal SyndromeAlex beharuNo ratings yet
- Methyl AlcoholDocument29 pagesMethyl AlcoholRuchira NishshankaNo ratings yet
- Drugs Used For GlaucomaDocument40 pagesDrugs Used For GlaucomaAgust SalimNo ratings yet
- SEM (CC3) ToxicologyDocument5 pagesSEM (CC3) ToxicologyBea EvangelistaNo ratings yet
- Drugs Acting On Potassium Channel: Submitted By: Md. Ashikur Rahman ID: 171-021-032Document12 pagesDrugs Acting On Potassium Channel: Submitted By: Md. Ashikur Rahman ID: 171-021-032broken reedNo ratings yet
- FDCDocument10 pagesFDCAnkit PandeyNo ratings yet
- Internal Medicine STUDY GUIDEDocument276 pagesInternal Medicine STUDY GUIDEanabananan100% (1)
- Acetaminophen: Acetaminophen: Anacin-3, Liquiprin, Panadol, Paracetamol, Tempra, TylenolDocument18 pagesAcetaminophen: Acetaminophen: Anacin-3, Liquiprin, Panadol, Paracetamol, Tempra, TylenolAyu DewiNo ratings yet
- Toxicology ICU PDFDocument49 pagesToxicology ICU PDFAhmed Shihab AhmedNo ratings yet
- 8 Drug StudyDocument19 pages8 Drug StudyLoyloy D ManNo ratings yet
- Organochlorines: by Touseef SiddiquieDocument14 pagesOrganochlorines: by Touseef Siddiquiejagadish yadgirNo ratings yet
- Acute Poisoning Guidelines.Document7 pagesAcute Poisoning Guidelines.Manoj KumarNo ratings yet
- Acute Poisoning of Therapeutic Agents: by Alemayehu TomaDocument42 pagesAcute Poisoning of Therapeutic Agents: by Alemayehu TomaYohannis AsefaNo ratings yet
- Adr & Di PDFDocument30 pagesAdr & Di PDFSri SriNo ratings yet
- Mpharm - pc1 - Syall BY JNTUK - 1Document10 pagesMpharm - pc1 - Syall BY JNTUK - 1Sri SriNo ratings yet
- HandbookofExperimentalPharmacology MergedDocument16 pagesHandbookofExperimentalPharmacology MergedSri SriNo ratings yet
- R22M Pharm PharmacologySyllabusDocument53 pagesR22M Pharm PharmacologySyllabusSri SriNo ratings yet
- Herbal Drug Technology Typed - 1Document7 pagesHerbal Drug Technology Typed - 1Sri SriNo ratings yet
- Anti Asthmatic DrugsDocument1 pageAnti Asthmatic DrugsSri SriNo ratings yet
- Survey On Dispensing of OTC Drugs at Retail Drug Stores (Pharmacies) in West GodavariDocument3 pagesSurvey On Dispensing of OTC Drugs at Retail Drug Stores (Pharmacies) in West GodavariSri SriNo ratings yet
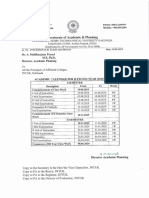
- Students Navasakam ListDocument13 pagesStudents Navasakam ListSri SriNo ratings yet
- JNTUK B.Tech 2 1 2 2 Sem Academic Calendar For A.Y 2019 20Document1 pageJNTUK B.Tech 2 1 2 2 Sem Academic Calendar For A.Y 2019 20Sri SriNo ratings yet
- Iv - Semister: Pharmaceutical Organic Chemistry - Iii (Theory)Document9 pagesIv - Semister: Pharmaceutical Organic Chemistry - Iii (Theory)Sri SriNo ratings yet
- A Compara Ve Evalua On of Quality and Price of Rani Dine, Me Ormin HCL Branded and Generic MedicinesDocument4 pagesA Compara Ve Evalua On of Quality and Price of Rani Dine, Me Ormin HCL Branded and Generic MedicinesSri SriNo ratings yet
- A Compara Ve Evalua On of Quality and Price of Rani Dine, Me Ormin HCL Branded and Generic MedicinesDocument4 pagesA Compara Ve Evalua On of Quality and Price of Rani Dine, Me Ormin HCL Branded and Generic MedicinesSri SriNo ratings yet
- Pediatric Medication Dosing GuildelinesDocument2 pagesPediatric Medication Dosing GuildelinesMuhammad ZeeshanNo ratings yet
- School Administration and Supervision MAED 605Document24 pagesSchool Administration and Supervision MAED 605Jaynie Ann TapdasanNo ratings yet
- Trophic Levels - 10% RuleDocument5 pagesTrophic Levels - 10% RulerebbiegNo ratings yet
- Taurian Curriculum Framework Grade 12 BIODocument8 pagesTaurian Curriculum Framework Grade 12 BIOpummyg100% (1)
- Moody's Financial Metrics 2007Document35 pagesMoody's Financial Metrics 2007Adrian IlieNo ratings yet
- Osteoarthritis DissertationDocument8 pagesOsteoarthritis DissertationPaperHelpJackson100% (1)
- International Trade Law: AssignmentDocument2 pagesInternational Trade Law: AssignmentQuỳnh PhạmmNo ratings yet
- What Is Aerobic Exercise?Document27 pagesWhat Is Aerobic Exercise?Zedy GullesNo ratings yet
- Notes About BurnsDocument11 pagesNotes About BurnsMichelle Ann GacudNo ratings yet
- Pengaruh Skarifikasi Dan Hormon Giberelin (Ga) Terhadap Daya Kecambah Dan Pertumbuhan Bibit Palem Putri (Veitchia Merillii)Document8 pagesPengaruh Skarifikasi Dan Hormon Giberelin (Ga) Terhadap Daya Kecambah Dan Pertumbuhan Bibit Palem Putri (Veitchia Merillii)Adi IndraNo ratings yet
- Fishing Broken Wire: WCP Slickline Europe Learning Centre SchlumbergerDocument23 pagesFishing Broken Wire: WCP Slickline Europe Learning Centre SchlumbergerAli AliNo ratings yet
- Jan Precious Mille BDocument1 pageJan Precious Mille BJebjeb C. BrañaNo ratings yet
- Elephantgrass Bookchapter PDFDocument22 pagesElephantgrass Bookchapter PDFMuhammad rifayNo ratings yet
- H1.001858 Strongpack Nigeria-Electrical Loads List For Layout Utilities-Rev-02Document1 pageH1.001858 Strongpack Nigeria-Electrical Loads List For Layout Utilities-Rev-02yseffoNo ratings yet
- 50-Article Text-116-1-10-20191113Document6 pages50-Article Text-116-1-10-20191113Annisa FauziahNo ratings yet
- OSCE Pediatric Dentistry Lecture-AnswersDocument40 pagesOSCE Pediatric Dentistry Lecture-AnswersR MNo ratings yet
- Marine Turtle Survey Along The Sindh CoastDocument106 pagesMarine Turtle Survey Along The Sindh CoastSyed Najam Khurshid100% (1)
- 6L45, 6L50, 6L80, 6L90: Time Tested - Industry TrustedDocument1 page6L45, 6L50, 6L80, 6L90: Time Tested - Industry TrustedCelso BidinotiNo ratings yet
- LabExercise2 PoriferaDocument13 pagesLabExercise2 PoriferaMarvin I. Delos SantosNo ratings yet
- Extubation After Difficult IntubationDocument3 pagesExtubation After Difficult Intubationramanrajesh83No ratings yet
- Steel Scrap Recycling Policy 06.11.2019 PDFDocument31 pagesSteel Scrap Recycling Policy 06.11.2019 PDFAnshul SableNo ratings yet
- The D - Block ElementsDocument30 pagesThe D - Block ElementsNandya AristaNo ratings yet
- Performantele MTADocument5 pagesPerformantele MTAana aNo ratings yet
- Narrative Report On Conduct of Classes-October 2021Document1 pageNarrative Report On Conduct of Classes-October 2021Jansen Roy D. JaraboNo ratings yet
- Indian MaDocument1 pageIndian MaAnass LyamaniNo ratings yet
- Notice: Environmental Statements Availability, Etc.: Syngenta Crop Protection, Inc., Et Al.Document8 pagesNotice: Environmental Statements Availability, Etc.: Syngenta Crop Protection, Inc., Et Al.Justia.comNo ratings yet