Professional Documents
Culture Documents
Magnesium Sulfate
Uploaded by
Karla Karina Dela Cruz0 ratings0% found this document useful (0 votes)
69 views2 pagesOriginal Title
Magnesium sulfate
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
69 views2 pagesMagnesium Sulfate
Uploaded by
Karla Karina Dela CruzCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
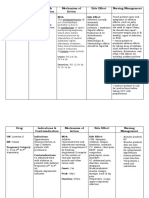
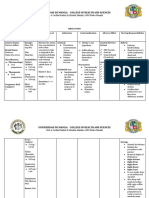
magnesium sulfate
Brand name:
Price:
250 mg/mL, 10 mL Ampule (Highest-Lowest Tender Price: 5.22 - 26.50 Php; Drug Price
Reference: 9. 05 Php)
250 mg/mL, 2 mL Ampule (Highest-Lowest Tender Price: 8.92 - 27.00 Php; Drug Price
Reference: 18.37 Php)
250 mg/mL, 20 mL Vial (Highest-Lowest Tender Price: 8.00 - 65.00 Php; Drug Price
Reference: 17.85 Php)
Therapeutic Class: Electrolyte Replacement
Pharmacologic Class: Minerals
Available Forms:
Injectable: 4%, 8%, 50% in 2-, 10-, 20-, and 50-mL ampules, vials, and prefilled syringes.
Injection Solution: 1% in D5W; 2% in D5W or NSS; 4% in water for injection, D5W, or NSS;
8% in water for injection, D5W, or NSS
Indications and Dosages:
Mild Hypomagnesemia: Adults (1 g I.M. every 6 hours for four doses, depending on
magnesium level.
Symptomatic severe hypomagnesemia, with magnesium level of 0.8 mEq/L or
less: Adults (5 g I.V. in 1 L of D5W or NSS over 3 hours. Base subsequent doses on
magnesium level)
Magnesium supplementation in total parenteral nutrition (TPN): Adults (8 to 24 mEq
I.V. daily added to TPN solution); Infants (2 to 10 mEq/day I.V. added to TPN solution.
Seizures in preeclampsia or eclampsia: Adults (Total initial dose is 10 to 14 g I.V. To
accomplish this, give 4 to 5 g I.V. in 250 mL of solution and simultaneously give up to 10
g I.M. (5 g or 10 mL of the undiluted 50% solution in each buttock). After initial IV dose,
some clinicians administer 1 to 2 g / hour by constant I.V. infusion. Base subsequent
doses on magnesium level; serum magnesium level of 6 mg/ 100 mL is considered
optimal for seizure control. Don’t exceed 40 g in a 24-hour period. Maximum dose in
patients with severe renal insufficiency is 20 g/ 48 hours.
Action: Replaces magnesium and maintain magnesium level; as an anticonvulsant, reduces
muscle contractions by interfering with release of acetylcholine at myoneural junction.
Adverse Reactions:
CNS: toxicity, weak or absent deep tendon reflexes, flaccid paralysis, drowsiness, stupor
CV: slow, weak pulse; arrhythmias; hypotension; circulatory collapse; flushing
GI: diarrhea
Metabolic: hypocalcemia
Respiratory: respiratory paralysis
Skin: diaphoresis
Other: hypothermia
Interactions:
Drug-Drug: Calcium channel blockers: may increase magnesium-related adverse
effects. Monitor therapy.
Cardiac glycosides: May cause serious cardiac conduction changes. Use together with
caution.
CNS depressants: May increase CNS depression. Use together cautiously.
Neuromuscular blockers: May cause increase neuromuscular blockage. Use together
cautiously. Closely monitor clinical response.
Drug-lifestyle: Alcohol use (May decrease magnesium level. Discourage use together.)
Effects on Lab Test Results: May decrease calcium level.
Contraindications and Cautions:
Contraindicated in patients with myocardial damage, heart block, or coma.
Use cautiously in patients with impaired renal function.
Alert: Using magnesium sulphate to stop preterm labor is not an FDA-approved use of
the drug; safety and effectiveness of drug for this indication have not been established.
Overdose S&S: hypotension, facial flushing, feeling of warmth, thirst, nausea, vomiting,
lethargy, dysarthria, drowsiness, diminished deep tendon reflexes, shallow respirations,
apnea, coma, cardiac arrest, respiratory paralysis, disappearance of patellar reflex
Nursing Considerations:
Keep I.V. calcium available to reverse magnesium intoxication.
Test knee-jerk and patellar reflexes before each additional dose. If absent, notify
prescriber and give no more magnesium until reflexes return; otherwise, patient may
develop temporary respiratory failure and need cardiopulmonary resuscitation or I.V.
administration of calcium.
Check magnesium level after repeated doses. Monitor levels hourly in patients with
severe hypomagnesemia. Normal plasma magnesium is 1.5-2.5 mEq/L.
Monitor fluid intake and output. Output should be 100 mL or more during 4-hour period
before dose.
Monitor renal function.
Drug may contain aluminium. Premature neonate are at high risk for aluminium toxicity
due to immature renal function. Aluminum exposure of more than 4 to 5 mcg/kg/day is
associated with CNS and bone toxicity.
Patients with prolonged exposure to magnesium sulphate who have impaired renal
function are at risk for aluminium toxicity.
Look alike-sound alike: Don’t confuse magnesium sulphate with manganese sulphate.
Patient Teaching:
Explain use and administration of drug to patient and family.
Tell patient to report all adverse effects.
You might also like
- Magnesium SulfateDocument2 pagesMagnesium SulfateGwyn Rosales100% (1)
- Carboprost TromethamineDocument2 pagesCarboprost TromethamineDeathDefying DonutNo ratings yet
- BuscopanDocument2 pagesBuscopancen janber cabrillosNo ratings yet
- Methyldopa nursing management for hypertensionDocument4 pagesMethyldopa nursing management for hypertensionRico Mae ValenciaNo ratings yet
- Drug Study OrthoDocument4 pagesDrug Study OrthoJhessa Curie Pitagan100% (1)
- DS (Calcium + Vit. D)Document6 pagesDS (Calcium + Vit. D)Mary April MendezNo ratings yet
- Name of Drug Mechanism of Action Indications and Contraindication Adverse Effect Nursing ConsiderationDocument2 pagesName of Drug Mechanism of Action Indications and Contraindication Adverse Effect Nursing ConsiderationNicole CalpoturaNo ratings yet
- Drug Study ObDocument6 pagesDrug Study Obednaria100% (1)
- Obat ObgynDocument8 pagesObat ObgynMuhammad Naqiuddin JalaluddinNo ratings yet
- Check The Physician's Observe and Follow The 14 Warn The Mother AboutDocument2 pagesCheck The Physician's Observe and Follow The 14 Warn The Mother AboutJust nowNo ratings yet
- Manage uterine contractions and bleeding with MetherginDocument2 pagesManage uterine contractions and bleeding with MetherginOtan Cuison100% (1)
- Timolol MaleateDocument3 pagesTimolol MaleateAP TOROBXNo ratings yet
- Drug Study - Magnesium SulfateDocument6 pagesDrug Study - Magnesium SulfatePrincess Alane MorenoNo ratings yet
- Name of Drug Dosage/Frequency/ Timing/Route Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilitiesDocument2 pagesName of Drug Dosage/Frequency/ Timing/Route Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilitieskyleNo ratings yet
- Drug Action, Contraindications, Adverse Effects and Nursing ConsiderationsDocument14 pagesDrug Action, Contraindications, Adverse Effects and Nursing ConsiderationsArdel LabadaNo ratings yet
- Ampicillin 2Document1 pageAmpicillin 2Kristine YoungNo ratings yet
- CefuroximeDocument11 pagesCefuroximeAlmira Ballesteros CestonaNo ratings yet
- Ferrous Sulfate Supplement GuideDocument1 pageFerrous Sulfate Supplement GuidezjoshuacNo ratings yet
- Nursing Care Plan for Risk of Bleeding During PregnancyDocument4 pagesNursing Care Plan for Risk of Bleeding During PregnancybananakyuNo ratings yet
- MetamucilDocument1 pageMetamucilSheri490No ratings yet
- WVSU Nursing Drug Study on MycrogynonDocument17 pagesWVSU Nursing Drug Study on MycrogynonEdmel Pamplona DuquesaNo ratings yet
- CELINDocument9 pagesCELINaikoestrellaNo ratings yet
- Drug Study: ChlorthalidoneDocument2 pagesDrug Study: ChlorthalidoneLIEZEL GRACE VELAYONo ratings yet
- Mefenamic AcidDocument3 pagesMefenamic AcidVaibhav MehtaNo ratings yet
- Ferrous Sulfate - Drug StudyDocument3 pagesFerrous Sulfate - Drug StudyElla Musk100% (1)
- Tramadol Drug StudyDocument2 pagesTramadol Drug StudyTipey Segismundo0% (1)
- Nursing Care Plan For Interrupted Breastfeeding NCPDocument3 pagesNursing Care Plan For Interrupted Breastfeeding NCPSaira SucgangNo ratings yet
- General Objective: College of NursingDocument3 pagesGeneral Objective: College of NursingRaan Lade KilemNo ratings yet
- Cefotaxime Drug Class, Uses, Side EffectsDocument3 pagesCefotaxime Drug Class, Uses, Side EffectsKristi WrayNo ratings yet
- Drug Study on CelecoxibDocument11 pagesDrug Study on CelecoxibPrincess Brigitte R. PATE�ANo ratings yet
- Methyldopa: An Alpha-2 Adrenergic Agonist for HypertensionDocument4 pagesMethyldopa: An Alpha-2 Adrenergic Agonist for HypertensionJinnijinniNo ratings yet
- Dexamethasone and MgSO4Document2 pagesDexamethasone and MgSO4Nasriah MacadatoNo ratings yet
- Drug StudyDocument4 pagesDrug StudyKristine Young100% (1)
- Drug Study on OxytocinDocument4 pagesDrug Study on OxytocinCarissa Mae Tapec EstradaNo ratings yet
- Vit EDocument2 pagesVit EkingpinNo ratings yet
- Vii. Drug Study Drug Mechanism of ActionDocument7 pagesVii. Drug Study Drug Mechanism of ActionRifa'atul MahmudahNo ratings yet
- Sotalol HydrochlorideDocument2 pagesSotalol HydrochlorideLIEZEL GRACE VELAYONo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationAbigail BascoNo ratings yet
- Drug Study: Name of PatientDocument1 pageDrug Study: Name of PatientKaloy KamaoNo ratings yet
- Drug StudyDocument4 pagesDrug StudyhsiriaNo ratings yet
- Drug StudyDocument8 pagesDrug StudymYiE23No ratings yet
- Oxytocin Generic Name Action and ContraindicationsDocument2 pagesOxytocin Generic Name Action and ContraindicationsJoanne Kaye TaylorNo ratings yet
- Drug Study Ko ToDocument4 pagesDrug Study Ko ToGian Carlo FernandezNo ratings yet
- Nursing Care Plan for PreeclampsiaDocument2 pagesNursing Care Plan for PreeclampsiaTsu Wei Chua0% (1)
- Insulin Mechanism of Action and Nursing ResponsibilitiesDocument7 pagesInsulin Mechanism of Action and Nursing ResponsibilitiesGrape JuiceNo ratings yet
- Chlorpheniramine Maleate: (klor-fen-AIR-uh-meen MAL-ee-ate)Document4 pagesChlorpheniramine Maleate: (klor-fen-AIR-uh-meen MAL-ee-ate)Nurginayah RusliNo ratings yet
- Drug Study BISACODYLDocument1 pageDrug Study BISACODYLAnna Sofia ReyesNo ratings yet
- Simethicone Relieves Gas and BloatingDocument1 pageSimethicone Relieves Gas and BloatingDivine Dela PenaNo ratings yet
- MisoprostolDocument3 pagesMisoprostolMichael Aditya LesmanaNo ratings yet
- Name of Drug Classification of Drug Mechanism of Action Indication Contraindications Side Effects Nursing ResponsibilitiesDocument4 pagesName of Drug Classification of Drug Mechanism of Action Indication Contraindications Side Effects Nursing ResponsibilitiesNemo Del RosarioNo ratings yet
- Drug Study On METHERGINEDocument4 pagesDrug Study On METHERGINEshadow gonzalezNo ratings yet
- AtroventDocument2 pagesAtroventKatie McPeekNo ratings yet
- Drug SDocument2 pagesDrug SJane CasiquinNo ratings yet
- Metronidazole 500mg/tab 1 Tab 3xadayDocument4 pagesMetronidazole 500mg/tab 1 Tab 3xadayCrisyl LipawenNo ratings yet
- Essential care universally available at affordable cost defined as primary health careDocument11 pagesEssential care universally available at affordable cost defined as primary health careAngelina Janiya NicoleNo ratings yet
- DRUG-STUDY - BALLON, Karlo CDocument6 pagesDRUG-STUDY - BALLON, Karlo CMelinda Cariño BallonNo ratings yet
- Pilocarpine (Drug Monograph)Document1 pagePilocarpine (Drug Monograph)Muhammad ArsalanNo ratings yet
- LidocaineDocument2 pagesLidocaineAhprelle Quiring Rodiel100% (1)
- DRUG STUDY Magnesium SulfateDocument4 pagesDRUG STUDY Magnesium SulfateTempoNo ratings yet
- Magnesium Sulfa-WPS OfficeDocument21 pagesMagnesium Sulfa-WPS OfficeNeha SinghNo ratings yet
- SPACERSDocument1 pageSPACERSKarla Karina Dela CruzNo ratings yet
- Drug StudyDocument4 pagesDrug StudyKarla Karina Dela Cruz100% (1)
- PathophysiologyDocument2 pagesPathophysiologyKarla Karina Dela CruzNo ratings yet
- Breastfeeding vs. Bottlefeeding On Weight GainDocument2 pagesBreastfeeding vs. Bottlefeeding On Weight GainKarla Karina Dela CruzNo ratings yet
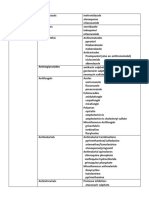
- CEPHALOSPORINSDocument2 pagesCEPHALOSPORINSKarla Karina Dela CruzNo ratings yet
- Classification of DrugsDocument20 pagesClassification of DrugsKarla Karina Dela CruzNo ratings yet
- Relationship of Digoxin and Potassium LevelsDocument1 pageRelationship of Digoxin and Potassium LevelsKarla Karina Dela CruzNo ratings yet
- Classification of DrugsDocument20 pagesClassification of DrugsKarla Karina Dela CruzNo ratings yet
- BIOCHEMISTRYDocument7 pagesBIOCHEMISTRYKarla Karina Dela CruzNo ratings yet
- BIOCHEMISTRYDocument7 pagesBIOCHEMISTRYKarla Karina Dela CruzNo ratings yet
- Skeletal Muscle Relaxant (Lecture Notes QIUP 2017)Document9 pagesSkeletal Muscle Relaxant (Lecture Notes QIUP 2017)Monissha ThiaguNo ratings yet
- Physiology of Respiration: Gas Exchange, Lung Volumes & Pulmonary VentilationDocument20 pagesPhysiology of Respiration: Gas Exchange, Lung Volumes & Pulmonary VentilationMustafa SaßerNo ratings yet
- Neuromusk. Bol.Document7 pagesNeuromusk. Bol.Irfan SkejicNo ratings yet
- AAN Neurology Board Prep Course: Sample MaterialsDocument5 pagesAAN Neurology Board Prep Course: Sample MaterialsKhaled GharaibehNo ratings yet
- BIO 361 Neural Integration LabDocument5 pagesBIO 361 Neural Integration LabnwandspNo ratings yet
- Disorders of the Diaphragm: Causes, Diagnosis and TreatmentDocument16 pagesDisorders of the Diaphragm: Causes, Diagnosis and TreatmentFajar YuniftiadiNo ratings yet
- Laporan Kasus: Myasthenia GravisDocument41 pagesLaporan Kasus: Myasthenia GravisTias DiahNo ratings yet
- CASE STUDY - THE TIRED SWIMMER (DT) - LouisDocument8 pagesCASE STUDY - THE TIRED SWIMMER (DT) - LouisSMAXICLouis Bintang AlexisNo ratings yet
- Human Physiology From Cells To Systems Sherwood 9th Edition Test BankDocument25 pagesHuman Physiology From Cells To Systems Sherwood 9th Edition Test Bankkeithzunigakzpcfjgbaw100% (27)
- Pex 02 01Document8 pagesPex 02 01Guia Fernandez100% (1)
- Physiology Semifinals NotesDocument20 pagesPhysiology Semifinals NotesIsabille MusongNo ratings yet
- Cholinergic ReceptorsDocument67 pagesCholinergic ReceptorsShynne RPhNo ratings yet
- What Is Neuromuscular Junction?Document3 pagesWhat Is Neuromuscular Junction?CallMeSashaNo ratings yet
- 100 Hints For The Oral BoardsDocument96 pages100 Hints For The Oral BoardsSteve Gibson100% (3)
- Myasthenia Gravis With Respiratory Failure in The Intensive Care UnitDocument4 pagesMyasthenia Gravis With Respiratory Failure in The Intensive Care UnitDr. FarhanNo ratings yet
- Pharmacology MCQs & Past Papers 4 MBBS, DPT, Pharm D (Password Protected)Document247 pagesPharmacology MCQs & Past Papers 4 MBBS, DPT, Pharm D (Password Protected)muhammad awais100% (1)
- Congenital Myasthenic Syndromes: Hometown HighlightsDocument3 pagesCongenital Myasthenic Syndromes: Hometown HighlightsApuse WakumNo ratings yet
- From Neuron To Brain Fifth Edition PDFDocument765 pagesFrom Neuron To Brain Fifth Edition PDFDavid Perdomo96% (25)
- Group 6Document37 pagesGroup 6LohithNo ratings yet
- From Neuron To Brain 5editionDocument13 pagesFrom Neuron To Brain 5editionJuan Carrillo Cruz19% (16)
- (Pharm) 1s-2 Ans DrugsDocument16 pages(Pharm) 1s-2 Ans DrugsKim Ramos67% (3)
- Neonatal HypotoniaDocument8 pagesNeonatal Hypotoniazulfiqar aliNo ratings yet
- Muscarinic Jones Concert: Skeletal Muscle Contraction Analogy WorksheetDocument5 pagesMuscarinic Jones Concert: Skeletal Muscle Contraction Analogy WorksheetCharles VollmersNo ratings yet
- Biology 9701 On23 P41Document19 pagesBiology 9701 On23 P412190ibrahimazeemNo ratings yet
- Muscular SystemDocument23 pagesMuscular SystemHarol CaballeroNo ratings yet
- Pathophysiology (Myasthenia Gravis) ..Document20 pagesPathophysiology (Myasthenia Gravis) ..Suku ydvNo ratings yet
- How to carry out Train of Four monitoringDocument10 pagesHow to carry out Train of Four monitoringAimee Ann Pauco MacaraegNo ratings yet
- Mammalian Neuromuscular PhysiologyDocument18 pagesMammalian Neuromuscular PhysiologymenschNo ratings yet
- Advanced Physio Final Exam PracticeDocument111 pagesAdvanced Physio Final Exam PracticefoufouNo ratings yet
- ChannelopathiesDocument18 pagesChannelopathiesJackyDanielsNo ratings yet