Professional Documents
Culture Documents
CARDIO
Uploaded by
Rayana Ubas0 ratings0% found this document useful (0 votes)
324 views5 pagesCopyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
324 views5 pagesCARDIO
Uploaded by
Rayana UbasCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
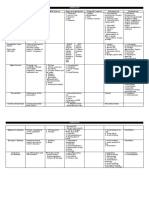
CARDIOVASCULAR DISORDERS
Coronary arteries - Levine’s signs
- Give blood supply to heart - Dyspnea
Branches - N/V
- Right coronary artery - Dizziness
o Right atrium Diagnostic exams
o Right ventricle - Cardiac catheterization
Inferior/posterior o Visualize coronary arteries
- Left coronary artery o Uses contrast media (iodine dye)
o Circumflex artery left atrium lateral o Catheter insertion site: femoral artery
o Left anterior descending artery left o Pre procedure
ventricle anterior Increase OFI
Extend the affected leg to
Coronary artery diseases prevent bleeding
Causes Assess digital pulses
- Atherosclerosis - ECG
- Arteriosclerosis o Check electrical activity of the heart
o Decrease blood flow to the heart Angina
decrease O2 delivery anaerobic Ischemia: T wave
metabolism lactic acid chest pain inversion (reversible)
Types MI
- Angina pectoris Ischemia: T wave
- Myocardial infarction inversion (reversible)
Injury: ST segment
Angina elevation (reversible)
- Chest pain caused by ischemia (reversible) Infarction: pathologic Q
Types wave (irreversible
- Stable angina - Cardiac enzymes
o Predictable o Elevate during injury
o Precipitating factors o Earliest indicator: myoglobin
Exertion o Most reliable: troponin I
Eating heavy meals o Most cardiac specific: CK MB
Exposure to cold Angina: normal
Emotional stress MI: elevated
o Relieved by rest and Nitroglycerine Onset Peak
- Unstable angina/pre infarction CK MB 4-6 hours 18-24 hours
o Unpredictable LDH 24 hours 48-72 hours
o Pain may happen at rest Troponin I 3 hours 7 days
- Variant angina/prinzemetal Myoglobin 1 hour 4-6 hours
o Coronary artery vasospasms Management
o Same each time each day (early AM) MEDICATIONS
- Nitrates
Myocardial infarction o Nitroglycerine
- Chest pain caused by ischemia (reversible) Angina: decreases pain
o Duration is longer increase injury MI: vasodilation
(reversible) death of cells infarction Routes
(irreversible) Sublingual
- Cause: coronary artery thrombosis o Retain saliva
Signs and symptoms o Burning
Angina MI sensation under
Quality Stabbing Same tongue is
Squeezing normal
Location Retrosternal Same o Proper storage
Substernal light sensitive
Radiation Jaw Same Dark
Neck place
Shoulders of
Arm contain
Stomach er
Duration <15 mins > 15 mins o Stock
Relieving factors Rest Morphine replacement
Nitroglycerine sulfate every 6 hours
- Chest pain
CARDIOVASCULAR DISORDERS
o Maximum dose: o Blood vessel:
3 per 5 minutes Saphenous vein (leg)
1st: 5 Internal mammary artery
mins (breast)
2nd: 5 ACUTE ER
mins - Priority: pain relief
3rd: 5 o Angina: Nitroglycerine
mins o MI: Morphine Sulfate
Patch - O2 therapy
o Placed on non - Position: fowlers
hairy part of - Tests
chest - Thrombolytics to dissolve clots
o Hairy chest: MI
shaving, clips Resumption of ADL: after 6 weeks
o Rotate Resumption of sex: after 8 weeks
application site: - Climb 2 flights of stairs
prevent burns - W/O chest pain
Ointment: wear gloves Patient w/o problem should assume activities
Side effects:
Orthostatic hypotension Congestive heart failure
Headache - Failure of the heart to pump blood
- Narcotics/Opioids: MI - Decrease cardiac output backflow of blood
o Morphine decreases pain congestion
- Thrombolytics - No cure
o Dissolve clots Types
o MI - Right side heart failure
o Streptokinase - Left side heart failure
o Tissue plasminogen activator (TPA) Signs and symptoms
Given within 3 hours - Right side heart failure
- Anti coagulants: both o Systemic congestion
o Heparin Fatigue
IV Oliguria
Initial Neck vein distention
Protamine Sulfate Hepatomegaly
o Warfarin Ascites
Oral Bipedal edema
Maintenance Anasarca
Vitamin K Weight gain
o Side effects: bleeding Hypertension
- Anti platelets: both - Left side heart failure
o Prevent platelet aggregation prevent o Pulmonary congestion
clots Fatigue
o Aspirin Oliguria
o Side effects: bleeding Pulmonary edema: fluid and
- Anti arrhythmic: MI blood filled alveoli
o Pathologic Q wave arrhythmia Dyspnea (DOB)
premature ventricular contractions Coughing
o Irreversible Sputum: frothy, pink
o Lidocaine Auscultation: crackles
SURGICAL Orthopnea
- Percutaneous Transluminal Coronary Angioplasty Paroxysmal nocturnal dyspnea
o Insertion of a balloon tipped catheter in Management
the coronary artery to compress plaques - Position: fowlers
o Indication: narrowing (atherosclerosis) - O2 therapy
- Coronary stent - Monitor intake/output
o Insertion of a catheter with a mesh wire - Decrease OFI
in the coronary artery to compress - Diet: decrease Na
plaques - Weigh patient daily
o Indication: narrowing (atherosclerosis) - Medications
- Coronary artery bypass graft (CABG) o Inotropics
o Create a new route for reperfusion Dopamine
o Indication: clots not dissolved by Dobutamine
thrombolytics
CARDIOVASCULAR DISORDERS
Increase force of o Spironolactone
contraction improve o Anti hypertensives
cardiac output ACE inhibitors
increase urination Beta blockers
o Cardiac glycosides (Digitalis) Calcium channel blockers
Digoxin
Inotropic: force Hypertension
Chronotropic: decrease heart BP classification
rate - 2-3 BP checks
Check HR (apical) - 2-3 clinic visits
Do not give if HR is Systole Diastole
below 60 Normal BP <120 and <80
Normal: 0.5-2 Elevated BP 120-129 and <80
Digitalis toxicity Stage 1 130-130 or 80-89
Causes Stage 2 >140 or >90
o Liver disorder Hypertensive crisis >180 or >120
Check Types/causes:
liver - Primary/essential
function o Non modifiable risk factors
test: o Lifestyles
ALT, AST - Secondary
o Kidney disorder o Pregnancy
Check o Diseases
kidney o Medication use
function Risk factors
test:
- Age: old age
BUN,
- Race: African Americans
Creatini
- Hereditary
ne
- Diet: increase sodium and fat
o Hypokalemia
- Obesity
Increas
- Smoking
e
- Increase stimulants
action
o Caffeine
of
o Carbonated
Digoxin
- Stress
Check
- Inactivity/immobility
serum Signs and symptoms
potassiu - Asymptomatic: most common
m - Headache
Over dosage - Visual changes
Signs and symptoms - N/V
o Bradycardia - Facial flushing
o Anorexia Management
o Nausea and - Monitor BP
vomiting - Diet: decrease sodium, decrease fat
o Diarrhea - Lose weight if obese
o Abdominal - Avoid smoking
cramps
- Decrease intake of caffeinated/carbonated
o Visual changes:
drinks
halos
- Stress management techniques
Management
- Regular exercise
o Antidote:
- Medications
Digoxin Immune
o Centrally acting adrenergic blockers
Fab (Digibind)
Block the reuptake of
o Diuretics
Norepinephrine in the central
Excrete excess fluids
venous nervous system PNS
Furosemide
decrease BP
Digoxin
Clonidine (Catapres)
o Potassium
o Beta blockers
sparing diuretics Beta receptors
o Prevent B1 heart
hyperkalemia: B2 lungs
digitalis toxicity
CARDIOVASCULAR DISORDERS
Block the SNS effect to heart Pericarditis
and lungs PNS decrease - Pericardium
heart rate vasodilation o Covering of the heart
decrease BP o Layer
Bronchoconstriction Visceral: inner
Contraindicated: Parietal: outer
COPD/asthma Between
o Calcium channel blockers Pericardial space
Block the entry of calcium to Prevent friction
heart cells decrease muscle - Pericarditis: inflammation of pericarditis
contraction vasodilation Signs and symptoms
decrease BP - Pericardial friction rub
Very Nice Drug o Auscultation: rubbing of hair sound
Verapamil - Chest pain
Nifedipine - Fever
Diltazaem - Elevation of ESR inflammation
o ACE inhibitors Management
Decrease BP angiotensinogen - Pain relief: analgesics
(liver) angiotensin I ACE - Corticosteroids: decreases inflammation
(lungs) angiotensin II - Position: fowlers
stimulates adrenal cortex
aldosterone Na H2O retention Cardiac tamponade
& blood vessels - Increase pericardial fluids (above 20ML)
vasoconstriction elevated BP Signs and symptoms
(RAAS) - Beck’s triad
Group of meds to prevent o Distended neck vein
conversion of angiotensin I and II o Distant heart sounds
No stimulation of adrenal cortex o Decrease BP
and blood vessels decrease Management
Na and H2O retention - Pericardiocentesis
vasodilation decrease BP o Removes excess fluids from excess space
(-pril) Catapril by aspiration
Management o Position: upright position
Monitor cough
Angiotensin 2 receptor
blockers (ARBS) Raynaud’s disease (white – blue – red disease)
o Block - Peripheral arterial arteries
stimulation of - Periodic vasospasms of small arteries of the
angiotensin 2 to hands
adrenal cortex - Cause: cold exposure
and blood - Incidence: female
vessels Signs and symptoms
decrease Na - Color changes of hands
and H2O o White: pallor (early)
retention to o Blue: cyanosis (late)
blood vessels o Red: perfusion
decrease BP - Skin temp: cold
o (-sartan) - Decrease or absence of distal pulses of the
o Diuretics hands
Excretion of excess fluids Management
decrease BP - Avoid exposure to cold
Thiazide - Careful when handling cold items
Low ceiling (least o Thick gloves
potent) - Avoid smoking
Can cause hypokalemia - Medications
Chlorothiazide (Diuril) o Vasodilators
Loop diuretic
Cause hypokalemia Buerger’s disease (thromboangitis obliterans)
Furosemide - Peripheral arterial (major) and venous (minor)
Potassium sparring diuretic disorder
Prevents hypokalemia - Decrease blood flow to legs and feet
Spironolactone - Cause: smoking
(Aldactone)
CARDIOVASCULAR DISORDERS
- Incidence: male
Signs and symptoms
- Intermittent claudication
o Leg pain
o Increase in walking
o Decrease at rest
- Skin temp: cold
- Decrease or absence of distal pulses of legs
- Leg/feet necrosis
Management
- Avoid/stop smoking
- Position of legs: lower
- Medications: Vasodilators
- Amputation
Deep vein thrombosis
- Peripheral venous
- Characterized by leg inflammation and clot
formation
- Causes
o Virchow’s triad
Venous stasis
Hypercoagulation
Vessel wall damage
Signs and symptoms
- Leg inflammation
- Skin temp: warm
- Leg edema
- Homan’s: dorsiflexion of the foot, calf pain
Management
- Ambulation
- ROM leg exercises
- Elevate legs only as prevention
o Contraindicated: clots
- Increase OFI
o Anti embolism stockings
Intermittent
Remove stockings for 30 minutes
every 8 hours
- Avoid
o Smoking
o Prolonged standing
o Cross sitting
o Leg massage
- Medications
o Thrombolytics: dissolve clots
o Anticoagulants: prevent clots
You might also like
- Renal TableDocument1 pageRenal TableRayana UbasNo ratings yet
- Respiratory TableDocument1 pageRespiratory TableRayana UbasNo ratings yet
- Batch KairosDocument2 pagesBatch KairosRayana UbasNo ratings yet
- TELEMEDICINEDocument2 pagesTELEMEDICINERayana UbasNo ratings yet
- Cardio TableDocument2 pagesCardio TableRayana UbasNo ratings yet
- CARDIODocument17 pagesCARDIORayana Ubas100% (1)
- NUTRITIONDocument6 pagesNUTRITIONRayana UbasNo ratings yet
- Campus Club FairDocument2 pagesCampus Club FairRayana UbasNo ratings yet
- Batch HirayaDocument2 pagesBatch HirayaRayana UbasNo ratings yet
- Hema 4Document64 pagesHema 4Rayana UbasNo ratings yet
- Cake FiestaDocument6 pagesCake FiestaRayana UbasNo ratings yet
- CCF BoothDocument3 pagesCCF BoothRayana UbasNo ratings yet
- Dengue FeverDocument5 pagesDengue FeverRayana UbasNo ratings yet
- Parenteral NutritionDocument4 pagesParenteral NutritionRayana UbasNo ratings yet
- Intravenous TherapyDocument6 pagesIntravenous TherapyRayana UbasNo ratings yet
- Hema 5Document33 pagesHema 5Rayana UbasNo ratings yet
- Fluids & ElectrolytesDocument4 pagesFluids & ElectrolytesRayana UbasNo ratings yet
- EARDocument2 pagesEARRayana UbasNo ratings yet
- Hema 1Document48 pagesHema 1Rayana UbasNo ratings yet
- EYEDocument4 pagesEYERayana UbasNo ratings yet
- Hema 3Document35 pagesHema 3Rayana UbasNo ratings yet
- Cake FiestaDocument3 pagesCake FiestaAl DavidNo ratings yet
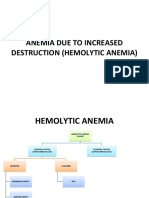
- ANEMIA: Types, Causes, Signs and TreatmentDocument45 pagesANEMIA: Types, Causes, Signs and TreatmentRayana UbasNo ratings yet
- SLCN Days 2019Document5 pagesSLCN Days 2019Rayana UbasNo ratings yet
- Psych FinalDocument19 pagesPsych FinalRayana UbasNo ratings yet
- Chapter 19Document11 pagesChapter 19RAYANA UBASNo ratings yet
- Ivt 4Document2 pagesIvt 4Rayana UbasNo ratings yet
- Ca1 29 YoDocument1 pageCa1 29 YoAl DavidNo ratings yet
- SLCN Days 2019Document5 pagesSLCN Days 2019Rayana UbasNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)