Professional Documents
Culture Documents
Ajcpath116 0331
Ajcpath116 0331
Uploaded by
surekhaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ajcpath116 0331
Ajcpath116 0331
Uploaded by
surekhaCopyright:
Available Formats
Anatomic Pathology / FACTORS THAT INFLUENCE THE ASCUS/SIL RATIO
An Analysis of Factors That Influence the ASCUS/SIL Ratio
of Pathologists
Ridas Juskevicius, MD,1* Kelly H. Zou, PhD,3,4 and Edmund S. Cibas, MD2,5
Key Words: Atypical squamous cells of undetermined significance; Squamous intraepithelial lesion; Cytopathologist; Pap smear; Quality
control; Cytology; Credentialing
Abstract The most commonly made abnormal diagnosis on a
In pursuit of physician-specific performance data in Papanicolaou (Pap) test is “atypical squamous cells of unde-
cytology, we have been calculating the ASCUS/SIL termined significance” (ASCUS). The concept that some Pap
(atypical squamous cells of undetermined smears may harbor atypical cells whose significance is uncer-
significance/squamous intraepithelial lesion) ratio of tain was not invented by the Bethesda System (TBS),
cytopathologists (CPs) and providing confidential currently the de facto standard for reporting cervical/vaginal
feedback every 6 months. At the same time, thin-layer diagnoses in the United States. TBS did, however, more
technology was introduced as an alternative to narrowly define the previously vague “atypical” Pap to
conventional smears. Thus we analyzed factors that exclude obviously benign cellular changes, as well as clear-
may influence the ASCUS/SIL ratio, particularly the cut intraepithelial lesions, thus limiting the category to
effect of periodic feedback on outliers (defined by a “borderline” cases of undetermined significance.1
professional benchmark). For 3 years, the mean The authors of TBS recognized the potential for overuse
ASCUS/SIL ratio for all CPs decreased significantly of the ASCUS diagnosis and suggested a benchmark, namely,
from 2.92 to 1.87. There was great variability in the that the ratio of ASCUS diagnoses to outright diagnoses of a
mean ASCUS/SIL ratio among 12 CPs (range, 1.11- squamous intraepithelial lesion (SIL), abbreviated as the
5.89). Of the 6 CPs who worked continuously during ASCUS/SIL ratio, be no greater than 3:1.2 The implication
this time, 2 showed a statistically significant decrease in was that any laboratory and, hence, any cytopathologist with
their ASCUS/SIL ratio, including the CP with the a higher ratio might be expressing uncertainty too frequently.
highest ratio; 1 showed a significant increase. The Some authors have suggested that even this benchmark is too
mean ASCUS/SIL ratio did not correlate well with lenient,3 and others hope to eliminate ASCUS entirely.4
years of CP experience or with individual annual case Clearly, there is no consensus on an ideal ASCUS/SIL ratio.
volume. The ASCUS/SIL ratio of some CPs can In an effort to define common practice, a nationwide labora-
decrease significantly over time. Whether it was due to tory survey found that the median ASCUS/SIL ratio is 2.0
feedback or the introduction of thin-layer preparations and that 80% of laboratories report ratios between 0.64 and
could not be determined. 4.23.5 Because there is some consensus regarding its upper
limits, monitoring the ASCUS/SIL ratio has been proposed
as a quality improvement measure for laboratories,6,7 but so
far there have been no studies of its use in evaluating the
performance of individual cytopathologists (CPs).
In looking for quantitative, physician-specific perfor-
mance data, particularly for the recredentialing process
required by the Joint Commission on Accreditation of
Healthcare Organizations and state medical boards, in 1997
© American Society of Clinical Pathologists Am J Clin Pathol 2001;116:331-335 331
Juskevicius et al / FACTORS THAT INFLUENCE THE ASCUS/SIL RATIO
we began to systematically calculate the ASCUS/SIL ratio term ASCUS/SIL ratio used throughout this article, therefore,
for CPs at the Brigham and Women’s Hospital (BWH), should be understood to include AGUS cases as well.
Boston, MA, and provide confidential feedback every 6 Case volume reports are generated every 6 months. Each
months. The underlying assumption was that this informa- CP receives a confidential memo listing, among other quality
tion, after identifying outliers, would give CPs an opportu- control measures, the ASCUS/SIL ratio and, for comparison,
nity to bring their ASCUS/SIL ratio in alignment with the the ASCUS/SIL ratio for the entire laboratory.
professional benchmark. The purpose of this study was to Beginning in July 1998, a new Pap test, the ThinPrep
review the data obtained, analyze the impact of factors such (Cytyc, Boxborough, MA) was introduced into the labora-
as annual case volume and the years of experience of the CP tory as an alternative to the conventional Pap smear. These
on ASCUS/SIL ratios, and see whether there was improve- cases were assigned a separate specimen type in the
ment in the ratios of the outliers. Cytology System, and the percentage of ThinPrep Paps and
conventional smears was monitored on a monthly basis.
The overall case mix, ie, the number of cases from high-
risk patients, did not change substantially during the years of
Materials and Methods
this study.
Data Acquisition and Retrieval Statistical Methods
Data on the frequency of various cytologic diagnoses The effect of the following factors on the ASCUS/SIL
were obtained from the BWH Cytology System, one of the ratio was assessed: (1) the progress over time, during which
many components that make up the Brigham Integrated CPs were given feedback on their ratios; (2) the increasing
Computer System, a system of networked PCs. The oper- use of the ThinPrep Pap test during that time; (3) the years of
ating system is an implementation of DateTree MUMPS experience of the CP; and (4) the annual case volume of each
(now InterSystems, Cambridge, MA). The Cytology System CP. The statistical analyses were based on data in ❚Table 1❚
was designed and developed at BWH with the collaboration and ❚Table 2❚ . Each of the time periods was a 6-month
of one of us (E.S.C.) using the MUMPS (Massachusetts interval between July 1997 and June 2000.
General Utility Multi-Programming System) programming First, to study the change in the ratios over time, we
language (now called M) (InterSystems). investigated the practice behavior of 6 of 12 CPs who were
The Cytology System captures events occurring from in the study throughout all time periods as well as pooled
the accessioning to the final reporting of the specimen. All data from all 12 CPs. We compared the mean ratios per time
computer entries are audited, and audit information includes period before and after July 1, 1998. A similar analysis was
a time stamp, the identity of the user, and the information repeated using January 1, 1999, as a cutoff, with the consid-
entered or changed. The system tracks each gynecologic Pap eration that it might have taken some time for a CP to react
test by cytotechnologist and cytopathologist, if the case is to the new Pap test and/or to feedback about the ASCUS/SIL
referred for review. The provisional and/or final diagnoses ratio. For each CP and for the pooled data, a 2-sample
are coded as one of 10 possible major diagnostic categories: Student t test was conducted to evaluate whether there was a
(1) unsatisfactory; (2) within normal limits; (3) benign statistically significant difference in the ASCUS/SIL ratio
cellular changes; (4) endometrial cells, cytologically benign, before and after the defined cutoff time. The correlation
in a postmenopausal woman; (5) ASCUS; (6) atypical glan- between the pooled ratio and the percentage of conversion to
dular cells of undetermined significance (AGUS); (7) low- the ThinPrep was assessed using the Pearson correlation
grade SIL; (8) SIL, difficult to grade; (9) high-grade SIL; coefficient and the Spearman rho.8
and (10) carcinoma. Cases requiring CP review are not To evaluate the effect of experience, we created a single
routinely reviewed by a supervisory cytotechnologist, but ASCUS/SIL ratio for each of the 12 participating CPs ❚Table
rather are passed directly to the CP by the cytotechnologist. 3❚. It was defined as the CP-specific ratio between the sum
For any specified time frame, a case volume report can of all ASCUS values and the sum of all SIL values for all 6
be generated that summarizes the number (with percentage) time periods. We used the Pearson correlation coefficient and
of cases diagnosed in each of the categories by individual CP the Spearman rho8 to assess the correlation between the
and by the laboratory as a whole. This report also calculates ASCUS/SIL ratio and the CP’s experience practicing
an ASCUS/SIL ratio, obtained by dividing the sum of cytology as of July 1998. Owing to the high variability
ASCUS and AGUS cases by the sum of low-grade SIL; SIL, exhibited in both variables, we dichotomized the ratio at a
difficult to grade; high-grade SIL; and carcinoma cases. cutoff point of 2.5, classifying it into a low (less than or
Although this ratio includes AGUS cases, these were much equal to 2.5) or a high (greater than 2.5) group. The under-
less common than ASCUS cases (AGUS/ASCUS <3%). The lying mean years of experience then were compared for
332 Am J Clin Pathol 2001;116:331-335 © American Society of Clinical Pathologists
Anatomic Pathology / ORIGINAL ARTICLE
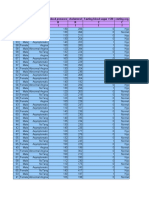
❚Table 1❚
ASCUS/SIL Ratios for 12 Cytopathologists for Six Separate Periods*
Time Period
Cytopathologist 1 2 3 4 5 6
1 0 0 0 0 2.39 (239/100) 2.50 (200/80)
2 2.39 (440/184) 2.51 (430/171) 2.31 (335/145) 1.63 (385/236) 1.39 (262/189) 1.32 (226/171)
3 0 0 0 0 1.14 (50/44) 1.45 (84/58)
4 6.99 (496/71) 6.97 (551/79) 6.39 (556/87) 4.74(526/111) 4.76 (238/50) 5.26 (200/38)
5 2.78 (242/87) 2.81 (315/112) 2.13 (215/101) 1.85 (226/122) 3.46 (225/65) 2.02 (341/169)
6 3.18 (156/49) 0.67 (6/9) 2.51(248/99) 3.20 (227/71) 3.14 (226/72) 4.10 (82/20)
7 1.47 (88/60) 2.40 (36/15) 1.33 (24/18) 2.92 (76/26) 1.91 (122/64) 2.44 (144/59)
8 1.45 (133/92) 1.23 (97/79) 1.04 (120/115) 1.31 (101/77) 1.24 (72/58) 0.72 (100/139)
9 0.00 (3/0) 3.07 (83/27) 5.19 (140/27) 3.99 (339/85) 0 0
10 0 0 0 0 1.66 (214/129) 1.80 (187/104)
11 3.34 (207/62) 2.90 (261/90) 4.05 (166/41) 0 0 0
12 0 0 3.00 (81/27) 0 0 0
Laboratory total 2.92 (1,765/605) 3.06 (1,779/582) 2.86 (1,885/660) 2.58 (1,880/728) 2.14 (1,648/771) 1.87 (1,564/838)
ASCUS, atypical squamous cells of undetermined significance; SIL, squamous intraepithelial lesion.
* Each time period was a 6-month interval (see text for details).
❚Table 2❚
Years of Experience, Number of Papanicolaou Tests Reviewed by 12 Cytopathologists, and Percentage Conversion to ThinPrep
Pap for Six Periods*
Time Period
Cytopathologist Experience (y) 1 2 3 4 5 6
1 0 0 0 0 0 659 502
2 11 1,050 1,159 889 1,144 778 708
3 0 0 0 0 0 156 251
4 15 799 908 947 835 427 315
5 4 574 974 685 741 580 1077
6 3 290 25 459 364 350 139
7 1 248 117 54 205 315 353
8 21 517 462 548 430 284 496
9 5 3 173 212 568 0 0
10 0 0 0 0 0 923 593
11 3 444 651 378 0 0 0
12 0 0 0 136 0 0 0
ThinPrep/All Pap Tests (%) 0 0 27 54 78 84
* Each period was a 6-month interval (see text for details).
❚Table 3❚ these 2 ratio groups using a 2-sample Student t test. The
Years of Experience, Average Case Volume, and Average analysis was repeated with a ratio cutoff point of 3.0.
ASCUS/SIL Ratio per Time Period
Finally, to evaluate the effect of annual case volume, we
Cytopathologist Experience (y) Case ASCUS/ performed an overall analysis by computing for each CP the
Volume SIL Ratio* average case volume per time period, defined as the ratio
1 0 580 2.44 between total case volume and the corresponding number of
2 11 955 1.90 participating time periods. The overall analysis was similar to
3 0 204 1.31
4 15 705 5.89 that described for assessing the effect of years of experience.
5 4 772 2.38 All statistical analyses were conducted using software
6 3 271 2.95
7 1 215 2.02
S-Plus (S-Plus 5 for Unix Guide to Statistics, Data Analysis
8 21 456 1.11 Products Division, Mathsoft, Seattle, WA, 1998).
9 5 239 4.06
10 0 758 1.72
11 3 491 3.28
12 0 136 3.00 Results
ASCUS, atypical squamous cells of undetermined significance; SIL, squamous Twelve CPs reviewed Pap smears during this period,
intraepithelial lesion. and 6 of them did so during the entire 3-year period from
* Average ASCUS/SIL ratio for each of the 12 cytopathologists was calculated from
the raw number of ASCUS and SIL cases in Table 1. July 1997 through June 2000. The mean ASCUS/SIL ratio
© American Society of Clinical Pathologists Am J Clin Pathol 2001;116:331-335 333
Juskevicius et al / FACTORS THAT INFLUENCE THE ASCUS/SIL RATIO
for the laboratory (all CPs combined) decreased from 2.92 to When the experience data were dichotomized based on
1.87. This decrease was statistically significant when mean a ratio of 2.5, 7 CPs had a ratio less than 2.5, and 5 CPs had
ASCUS/SIL ratios were compared before and after January one greater than 2.5. In the low ratio group, the years of
1999 (P = .01). With July 1998 as a cutoff, the decrease was experience ranged from 0 to 21 (mean, 5.3; SD, 7.99). In the
not significant (P = .07). When the analysis was restricted to high ratio group, the years of experience ranged from 0 to 15
the 6 CPs who worked continuously during all time periods, (mean, 5.2; SD, 5.76). The t test did not reveal a statistically
the mean ASCUS/SIL ratio decreased from 2.81 to 1.83. significant difference in experience between these 2 groups.
This decrease was statistically significant with January 1999 In the overall analysis, the average case volume per time
as a time cutoff (P = .01) and borderline significant with a period ranged from 136 to 955 (mean, 481.8; SD, 272). This
time cutoff of July 1998. showed an essentially 0 correlation coefficient measure with
When data were analyzed by individual CP, 4 showed a the ASCUS/SIL ratio. In the low ratio group, the average
decrease in their ASCUS/SIL ratios, and 2 of these were volume ranged from 204 to 955 (mean, 562.9; SD, 288). In
statistically significant. With a time cutoff of July 1998, the the high ratio group, the average volume ranged from 136 to
mean ASCUS/SIL ratio for CP2 decreased from 2.45 to 1.66 705 (mean, 368.4; SD, 271). The underlying means of the
(P = .04), and that for CP4 decreased from 6.98 to 5.29 (P = average volumes in these groups were not statistically
.02). The remaining 2 CPs showed an increase that was not different based on the t test.
statistically significant. When the cutoff for comparing ratios
was set at January 1999, the decrease in ratios for CP2 and
CP4 was still significant (both P < .005), but the increase in
Discussion
the ratio for CP6 became significant (P = .05). ❚Figure 1❚ We found that during the 3 years that feedback was
illustrates the change in the ASCUS/SIL ratio for CPs 2 and provided to CPs on their ASCUS/SIL ratio, the ratio
4 and for the laboratory as a whole. ❚Figure 2❚ shows the decreased significantly when data were pooled from the 6
change in the ASCUS/SIL ratio of the 6 CPs who worked CPs who worked continuously during this time. Because this
continuously during this period. period of feedback overlapped with the conversion from
The ThinPrep method was introduced in July 1998, and smears to ThinPrep Paps in our laboratory, it is possible that
the percentage of Pap smears prepared in this fashion rose the decrease in ratio can be attributed in part to the new Pap
steadily; by the end of the study period, it was 84% ❚Figure technology. Nevertheless, we think it likely that a significant
3❚. The decrease in the ASCUS/SIL ratio was highly corre- component of this decrease is due to behavior modification
lated with the increase in the percentage of the ThinPrep based on feedback given twice a year.
Paps (Pearson correlation, –0.96; Spearman rho, –0.99). The ASCUS/SIL ratio was not correlated with either the
The years of experience of the CPs ranged from 0 to 21 years of experience of the CP or with the annual Pap case-
(mean, 5.2; SD, 6.9), and the ASCUS/SIL ratios ranged from load. In other words, experienced CPs did not necessarily
1.11 to 5.89 (mean, 2.67; SD, 1.40). The correlation coeffi- have a lower or higher ASCUS/SIL ratio than less experi-
cients were low (Pearson, 0.38; Spearman 0.33). enced CPs. Similarly, CPs with a higher annual service
7.5 7.5
7.0 7.0
6.5 6.5
6.0 6.0
5.5
ASCUS/SIL Ratio
5.5
ASCUS/SIL Ratio
5.0
CP4 CP4
5.0
4.5 4.5
4.0 4.0 CP6
3.5 3.5
3.0 3.0
2.5 2.5 CP7
2.0 Pooled 2.0 CP5
1.5 1.5
1.0
CP2 CP2
1.0
0.5 0.5 CP8
0.0 0.0
1 2 3 4 5 6 1 2 3 4 5 6
Time Period Time Period
❚Figure 1❚ Plot of mean ASCUS/SIL (atypical squamous cells ❚Figure 2❚ Plot of mean ASCUS/SIL (atypical squamous cells
of undetermined significance/squamous intraepithelial lesion) of undetermined significance/squamous intraepithelial lesion)
ratios for 12 cytopathologists (pooled data) and 2 ratios for 6 individual cytopathologists (CPs) who worked
cytopathologists (CP2 and CP4) who showed a statistically continuously during the study period. Each period is 6
significant decrease over time. Each period is 6 months. months.
334 Am J Clin Pathol 2001;116:331-335 © American Society of Clinical Pathologists
Anatomic Pathology / ORIGINAL ARTICLE
argues that responses to feedback vary among individuals.
90 3.5
84.3
Some may benefit from feedback alone; others may require
80
2.92
3.06
3.0
active measures, such as a period of “double scoping,” if they
77.8
ASCUS/SIL Ratio
2.86 are to lower their ratios to the recommended level.
70
2.58
2.5
From the 1Department of Pathology, Pitt County Memorial
ASCUS/SIL Ratio
60 2.34
% TP Conversion
53.8 Hospital and Brody School of Medicine, East Carolina University,
2.0
50 1.87 Greenville, NC; and the Departments of 2Pathology and
3Radiology, Brigham and Women’s Hospital, and 4Health Care
40
1.5 Policy and 5Pathology, Harvard Medical School, Boston, MA.
30
27.3
Address reprint requests to Dr Cibas: Dept of Pathology,
1.0 Brigham and Women’s Hospital, 75 Francis St, Boston, MA
20 % Conversion
02115.
0.5 * Dr Juskevicius was a visiting resident to the Department of
10
Pathology, Brigham and Women’s Hospital, when the study was
0 0.0
performed.
1 2 3 4 5 6 Acknowledgment: We thank Neal Blustein for expert
Time Period assistance in the preparation of this manuscript.
❚Figure 3❚ Plot of pooled mean ASCUS/SIL (atypical
squamous cells of undetermined significance/squamous
intraepithelial lesion) ratios for 12 cytopathologists and
percentage conversion of Papanicolaou smears to the
References
ThinPrep (TP) method. Although there is a significant 1. National Cancer Institute Workshop. The 1988 Bethesda
System for reporting cervical/vaginal cytological diagnoses.
correlation, this does not prove a causal relationship. The JAMA. 1989;262:931-934.
decrease in the ASCUS/SIL ratio may be the result of 2. Kurman RJ, Solomon D. The Bethesda System for Reporting
feedback provided to the cytopathologists after each time Cervical/Vaginal Cytologic Diagnoses. New York, NY: Springer-
period. Timing of confidential feedback memos is indicated Verlag; 1994:34.
by arrows. 3. Tabbara SO, Faser C, Frost AR, et al. Toward establishing a
target value for the ASCUS:SIL ratio [abstract]. Acta Cytol.
1995;39:989.
commitment to gynecologic cytology had neither a higher 4. Stoler MH. Does every little cell count? don’t “ASCUS”
[editorial]. Cancer. 1999;87:45-47.
nor a lower ratio than those with a lower commitment. We
5. Davey DD, Woodhouse S, Styer P, et al. Atypical epithelial
did not attempt to correlate case load with the ASCUS/SIL cells and specimen adequacy: current laboratory practices of
ratio on a daily basis. It is possible that an especially heavy participants in the College of American Pathologists
workday may increase or decrease the ASCUS/SIL ratio. But Interlaboratory Comparison Program in Cervicovaginal
Cytology. Arch Pathol Lab Med. 2000;124:203-211.
over time, the mean daily caseload was similar for all CPs
6. Mody DR, Davey DD, et al. Quality assurance and risk
and did not change significantly during this 3-year period reduction guidelines. Acta Cytol. 2000;44:496-507.
(data not shown). 7. Mulligan NJ, Morenas AD, Soto-Wright V, et al. Percentages
We are encouraged that 2 CPs showed a statistically of cervical cytologic diagnoses as a quality assurance method.
significant decrease in their ASCUS/SIL ratios during the Acta Cytol. 1998;42:928-932.
period of feedback, particularly the greatest outlier, whose 8. Kendall M, Gibbons JD. Rank Correlation Methods. 5th ed.
New York, NY: Oxford University Press; 1990:8-27.
ratio came closer to the national benchmark. Other CPs
showed a decrease in their ratios and, although this did not
reach statistical significance, it is possible that with a longer
study period, these decreases also would be significant. On
the basis of these results, we believe that confidential feed-
back on individual ASCUS/SIL ratios is a useful quality
improvement tool, and we continue to use it as described
herein. In addition, we have incorporated it into our
cytopathology fellowship program by providing it to fellows
after a period of supervised sign-out responsibility.
Not all CPs responded with a decrease in the ratio
during those 3 years, however, and it is noteworthy that the
ASCUS/SIL ratio of 1 CP increased significantly. This
© American Society of Clinical Pathologists Am J Clin Pathol 2001;116:331-335 335
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5808)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (843)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- TokoJAV.comDocument166 pagesTokoJAV.comKsatrio Pinayung Rizqi50% (2)
- A Immediate Implant With Provisionaliztion Journal of Clinical PeriodontologyDocument12 pagesA Immediate Implant With Provisionaliztion Journal of Clinical PeriodontologyAhmed BadrNo ratings yet
- Prioritization - FNCPDocument10 pagesPrioritization - FNCPJeffer Dancel67% (3)
- Two Handed Process Chart & Ergonomics in Textile and ApparelDocument32 pagesTwo Handed Process Chart & Ergonomics in Textile and ApparelVaanazhaganNo ratings yet
- Lenmed Health BrochureDocument7 pagesLenmed Health Brochuremaputohospital100% (13)
- DO PBL Paper Case 16 HIV OSCEDocument4 pagesDO PBL Paper Case 16 HIV OSCESmelly RaccoonNo ratings yet
- What Is The Best Indicator To Determine Anatomic PDocument12 pagesWhat Is The Best Indicator To Determine Anatomic PjhidalgomdNo ratings yet
- Age Sex Chest Pain Type Blood Pressure Cholesterol Fasting Blood Sugar 120 Resting Ecg R C C R R C C I I I I I I IDocument14 pagesAge Sex Chest Pain Type Blood Pressure Cholesterol Fasting Blood Sugar 120 Resting Ecg R C C R R C C I I I I I I Isantu4_1111No ratings yet
- REGULATIONS AND CURRICULUM1.0 - CompressedDocument50 pagesREGULATIONS AND CURRICULUM1.0 - CompressedneethuNo ratings yet
- BGHMC Investment Needs For 2023 Non-Functional Specialty CentersDocument19 pagesBGHMC Investment Needs For 2023 Non-Functional Specialty CenterslykangelirNo ratings yet
- Newborn NotesDocument3 pagesNewborn NotesSharlotte EbayNo ratings yet
- Dufour 2006 - Biocultural Approaches in Human Biology PDFDocument9 pagesDufour 2006 - Biocultural Approaches in Human Biology PDFFlor DarkoNo ratings yet
- Leadership & Management Ethical - LegalDocument51 pagesLeadership & Management Ethical - Legalamasoud96 amasoud96No ratings yet
- Health Dissertation TopicsDocument6 pagesHealth Dissertation TopicsUK100% (1)
- F561M - 0818 Grapadora de PedalDocument56 pagesF561M - 0818 Grapadora de PedalSST- EshkolNo ratings yet
- Media and Information Literacy The Influence of Media and Information To Communication Learning Activity Sheet No. 1Document41 pagesMedia and Information Literacy The Influence of Media and Information To Communication Learning Activity Sheet No. 1amaya dxeuNo ratings yet
- Example of Group Forum (SCRIPT)Document7 pagesExample of Group Forum (SCRIPT)Michael Arushe50% (2)
- Healthy Heart-3Document1 pageHealthy Heart-3api-309564044No ratings yet
- GHS Format-sds-Gp CleanDocument8 pagesGHS Format-sds-Gp CleanAlan TanNo ratings yet
- Try Scribd FREE For 30 Days To Access Over 125 Million Titles Without Ads or Interruptions!Document1 pageTry Scribd FREE For 30 Days To Access Over 125 Million Titles Without Ads or Interruptions!eyaNo ratings yet
- 107 RLE Group 5 1F Newborn Delivery Final OutputDocument79 pages107 RLE Group 5 1F Newborn Delivery Final OutputJr CaniaNo ratings yet
- Impact of Occupational Stress On Quality WorkDocument9 pagesImpact of Occupational Stress On Quality WorkJasmin NayakNo ratings yet
- Beta Alanine Supplementation PresentationDocument11 pagesBeta Alanine Supplementation Presentationapi-576308167No ratings yet
- Rescue Solutions Brochure 88489Document16 pagesRescue Solutions Brochure 88489ursulaNo ratings yet
- Specimen Collection Manual For Laboratory Serivces LRHDocument100 pagesSpecimen Collection Manual For Laboratory Serivces LRHPasan MaheshaNo ratings yet
- 1577un 2026-01Document79 pages1577un 2026-01ngovantienNo ratings yet
- GRADES 1 To 12 Daily Lesson Log Monday Tuesday Wednesday Thursday FridayDocument13 pagesGRADES 1 To 12 Daily Lesson Log Monday Tuesday Wednesday Thursday FridayJessie Atillo TindoyNo ratings yet
- SACS Back To School 2020Document37 pagesSACS Back To School 2020Saige DriverNo ratings yet
- Medico-Legal Aspect of DeathDocument29 pagesMedico-Legal Aspect of DeathDm Cinco100% (1)
- Stages of LaborDocument3 pagesStages of Laborkatzuhmee leeNo ratings yet