Professional Documents
Culture Documents
Hemiartroplastia de Cadera Cementada VS No Cementada en FX, Metanalisis 2017
Uploaded by
Daniel Cancino CallirgosOriginal Title
Copyright
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentHemiartroplastia de Cadera Cementada VS No Cementada en FX, Metanalisis 2017
Uploaded by
Daniel Cancino Callirgos SPECIALTY UPDATE
Cemented versus cementless
hemiarthroplasty for a displaced fracture of
the femoral neck
A SYSTEMATIC REVIEW AND META-ANALYSIS OF CURRENT
GENERATION HIP STEMS
H. D. Veldman, Aims
I. C. Heyligers, Our aim was to prepare a systematic review and meta-analysis to compare the outcomes of
B. Grimm, cemented and cementless hemiarthroplasty of the hip, in elderly patients with a fracture of
T. A. E. J. Boymans the femoral neck, to investigate the mortality, complications, length of stay in hospital,
blood loss, operating time and functional results.
From Zuyderland
Materials and Methods
Medical Center, A systematic review and meta-analysis was conducted following the Preferred Reporting
Heerlen, The Items for Systematic Reviews and Meta-Analyses guidelines on randomised controlled trials
Netherlands (RCTs), studying current generation designs of stem only. The synthesis of results was done
of pooled data, with a fixed effects or random effects model, based on heterogeneity.
Results
A total of five RCTs including 950 patients (950 hips) were included. Cementless stems were
found to be associated with more complications compared with cemented stems (odds
ratio (OR) 1.61, 95% confidence interval (CI) 1.12 to 2.31, p = 0.01), especially implant-related
complications (OR 3.15, 95% CI 1.55 to 6.41, p = 0.002). The operating time was shorter for
cementless stems (weighted mean difference -9.96 mins, 95%CI -12.93 to -6.98, p < 0.001).
The data on functional outcomes could not be pooled. There was no statistically significant
difference for any other outcome between the two methods of fixation.
Conclusion
In hemiarthroplasty of the hip using current generation stems, cemented stems result in
fewer implant-related complications and similar mortality compared with cementless
stems.
H. D. Veldman, BSc, Medical
student
Cite this article: Bone Joint J 2017;99-B:421–31.
I. C. Heyligers, Prof. MD PhD,
Orthopaedic Surgeon Fractures of the hip account for 23.8% of all pain and fewer implant-related complica-
B. Grimm, MEng PhD, fractures in patients over the age of 75 years, tions.12,13,15 However, these reviews mainly
Research Director
T. A. E. J. Boymans, MD, mostly as a consequence of trauma and osteo- included older studies which compared previ-
Orthopaedic Surgeon porosis.1 As the population ages, the incidence ous prostheses such as the Austin Moore and
AHORSE Research Foundation,
Department of Orthopaedic of these fractures will increase.2-4 Cooper et al3 Thompson (Corin Group, Cirencester, United
Surgery and Traumatology projected a worldwide increase in fractures of Kingdom).12-15 These are now outdated and
Zuyderland Medical Center, H.
Dunantstraat 5, NL-6419 PC the hip from 1.66 million in 1990 to 6.26 mil- rarely used16-20 and their inferior clinical
Heerlen, The Netherlands. lion by 2050. A substantial proportion of these outcome16,21-24 may have affected the conclu-
Correspondence should be sent are fractures of the femoral neck, which puts sions of these reviews. In Sweden, for example,
to H. D. Veldman; email:
h.veldman@student.maastricht
the femoral head at risk of osteonecrosis and as a proportion of all hemiarthroplasty
university.nl nonunion due to the tenuous blood supply.5 implants, the use of Austin Moore and Thomp-
©2017 The British Editorial
Hemiarthroplasty of the hip is the routine son stems decreased from 18% in 2005 to
Society of Bone & Joint treatment for displaced fractures of the femo- 0.9% in 2009.18
Surgery
doi:10.1302/0301-620X.99B4.
ral neck.5,6 However, whether cemented or The aim of this systematic review and meta-
BJJ-2016-0758.R1 $2.00 cementless fixation should be used remains analysis of randomised controlled trials
Bone Joint J
controversial.7-11 Many studies, systematic (RCTs) was to investigate whether either con-
2017;99-B:421–31. reviews and meta-analyses have been temporary cemented or cementless hemiar-
Received 8 August 2016;
Accepted after revision 5
published12-15 which suggest that cemented throplasty is more successful in elderly patients
December 2016 hemiarthroplasty results in better function, less with a fracture of the femoral neck, with
VOL. 99-B, No. 4, APRIL 2017 421
422 H. D. VELDMAN, I. C. HEYLIGERS, B. GRIMM, T. A. E. J. BOYMANS
regards to mortality, function, complications, length of stay aseptic loosening and dislocation. Cardiovascular compli-
in hospital, blood loss and operating time. cations included intra-operative cardiac arrest, myocardial
infarction, cerebral infarction, pulmonary embolism, acute
Materials and Methods arrhythmia and severe intra-operative hypotension. Local
The report is structured according to the Preferred Report- complications included superficial or deep wound infec-
ing Items for Systematic Reviews and Meta-Analyses state- tion. General complications included pneumonia, urinary
ment.25 Two reviewers (HDV and TAEJB) independently tract infection, acute renal failure, gastric disease or decub-
conducted a systematic search, in April 2016, of Pubmed itus ulcers.
(1966 to 2016), EMBASE (1974 to 2016), the Web of Sci- The methodological quality of the studies which were
ence (1950 to 2016) and the Cochrane Central Register of included, was assessed according to a modified version of
Controlled Trials (1948 to 2016). The search consisted of the ‘Cochrane Collaboration tool’ by two authors (HDV
terms relating to the condition (‘hip fracture’, ‘hip frac- and TAEJB).26 The risk of selection bias, detection bias,
tures’, ‘fractured hip’, ‘proximal femur fracture’, ‘femoral attrition bias and reporting bias was examined for each
fracture’ or ‘fractured femur’), to treatment (‘hemiarthro- study. The possibility of other bias (e.g. confounding or co-
plasty’ or ‘hemiprosthesis’) and to the method of fixation interventions) was also examined. Each of these aspects
(‘cemented’, ‘cementless’ or ‘uncemented’). The two was rated as ‘low risk', ‘unclear risk’ or ‘high risk' of bias.
authors independently assessed the compliance of each arti- Any disagreements on the rating were solved by discussion
cle with the inclusion criteria. Any disagreements were and consultation with a third author (BG).
solved by discussion. Statistical analysis. The outcomes of interest consisted of
Current generation (modern) stems were defined as hip dichotomous and continuous outcomes. Odds ratios (ORs)
stems developed after 1985. Studies which investigated dis- were calculated for the dichotomous outcomes and a
continued or unavailable stems were excluded, as were weighted mean difference (WMD) was obtained for the
those which considered Austin Moore or Thompson stems. continuous outcomes. The 95% confidence intervals (CI)
Studies were included if at least one of the outcomes of were also acquired for each outcome. Heterogeneity
interest was investigated: mortality, functional perfor- between results was measured by a chi-squared test and
mance, number and type of complications, length of stay, subsequently quantified by I2. Synthesis of results was done
blood loss and/or operating time. These outcomes were by pooling the data and a fixed effects model meta-analysis.
chosen because they reflect clinical outcome and are ame- However, if the I2 indicated moderate or high heterogeneity
nable quantitative outcome measures for meta-analysis. (i.e. I2 ≥ 50%), as defined by Higgins et al,27 data were
Studies were only eligible for inclusion if a strict follow-up pooled according to the random-effects model. The level of
period was defined (although we set no requirements as to statistical significance was set at p < 0.05. All analyses were
the length of follow-up), to ensure comparability between performed in Revman Review Manager (Revman 5.3; The
studies. No further requirements were defined regarding Nordic Cochrane Centre, Cochrane Collaboration, Copen-
the surgical procedure or patient characteristics. hagen, Denmark, 2014). In order to evaluate the possibility
All relevant information was independently extracted of publication bias, Revman Review Manager was used to
from the studies which were selected by two reviewers create a funnel plot.
(HDV and TAEJB). Where there was inconsistency in the
data, the study was discussed and critically appraised. Data Results
of interest were methodological data, patient characteris- The initial search, reasons for exclusion and final selection
tics and outcome measures. Methodological data included of studies are shown in a flow diagram (Fig. 1). One study
the number of centres which were involved in the recruit- was published twice with a different length of follow-
ment of the patients, the method of enrolment, the type of up.28,29 In order to derive the most recent and complete
stem and the principle of data analysis (‘intention-to-treat’ information from their data, only the most recent study was
or ‘per protocol’). The characteristics of the patients included.29 In total, five RCTs were included.29-33 They
included the total number of patients and the number in were published between 2005 and 2014, and included 950
each group (cemented versus cementless), the mean age and patients (950 hips) (Table I). The outcome measures and
gender. Outcome measures were recorded, including their lengths of follow-up differed between the studies (Table II).
number and the time of follow-up, and the number and The methodological quality varied greatly between the
type of complications. The outcome measures ‘mortality’ studies (Figs 2 and 3). In two trials, randomisation was ade-
and ‘functional outcomes’ were recorded according to the quately performed using a random number generator.29,33
time from surgery. The ‘number of complications’, ‘length A further two studies used a blinded block design but did
of stay’, ‘blood loss’ and ‘operating time’ were not bound to not describe how randomisation was performed,30,32 and
a single point in time. Complications were classified as one study randomised patients based on the day of the
implant-related, cardiovascular, local or general, and re- operation,31 which has a high risk of bias. In two studies,
operations for any reason. Implant-related complications allocation was performed by an opaque numbered
included intra- and post-operative periprosthetic fractures, envelope which was opened in the operating theatre,29,33
THE BONE & JOINT JOURNAL
CEMENTED VERSUS CEMENTLESS HEMIARTHROPLASTY FOR A DISPLACED FRACTURE OF THE FEMORAL NECK 423
Initial search (n = 354)
(pubmed (n =103), Embase (n = 50),
Cochrane (n = 50), Web of science (n =151)
Studies not investigating
Titles and abstracts the role of cementing in
screened (n = 354) hemiarthroplasty (n = 214)
Abstracts of potential
Duplicates removed (n = 67)
relevance (n = 140)
67 articles removed
- Non-RCTs (n = 57)
- Conference paper (n = 1)
- Not available (n = 2)
Full text articles - RCTs investigating
assessed for eligibility outdated Austin Moore
(n = 73) and/or Thompson stems
(n = 7)
One study was published
twice (a one-yr follow-up
RCTs suitable for and a five-yr follow-up),
inclusion (n = 6) the one-yr follow-up
was excluded (n = 1)
RCTs included in
quantitive synthesis
(n = 5)
Fig. 1
Flowchart of the selection of studies (RCT, randomised controlled
trial).
whilst three studies did not fully describe the allocation.30-32 described mortality at one month post-operatively were
Of the four RCTs which described functional outcomes, pooled.29,30 There was moderate heterogeneity between the
three were considered to have a low risk of attrition bias studies (I2 = 70%, p = 0.07), and analysis was performed
because of a small loss to follow-up, with equal distribution according to the random effects model. Pooling revealed no
between groups.29,30,33 The one RCT which did not significant difference between the groups in these two stud-
describe loss to follow-up or protocol violations had an ies (OR 1.11, 95% CI 0.17 to 7.10, p = 0.92).
unclear risk of bias.31 Only one study described the use of a All five studies investigated mortality at one year post-
national register to define death in their missing patients.30 operatively.29-33 The mortality at this time ranged from
In the other studies, it was unclear how the distinction was 20.3%30 to 30.0%32 in the cementless group, and from
made between missing patients and deaths.29,31-33 The 18.8%29 to 31.3%33 in the cemented groups. No study
extremely low loss to follow-up in the study by Langslet et found a significant difference in mortality after one year
al29 (2.2%) resulted in a low risk of bias. An unclear between cemented and cementless hemiarthroplasty. After
risk30,32 or high risk31 of ‘other bias’ was allocated mainly pooling of the data no significant difference was found (OR
because of the possibility of confounding and/or co- 0.82, 95% CI 0.61 to 1.09, p = 0.17) (Fig. 4).
interventions in those trials. Mortality at two years post-operatively was described in
Mortality. The studies defined peri-operative and early mor- two studies.29,33 At this time, the mortality was 35.2%29
tality at different times (Table II). Mortality within the first and 40.0%33 in the cementless group and 28.6%29 and
post-operative year ranged from the day of the operation to 43.8%33 in the cemented group. Neither study found a sig-
six months post-operatively. None of the studies reported a nificant difference in mortality, and there was no significant
significant difference in mortality between the two groups difference after pooling the data (OR 0.91, 95% CI 0.60 to
at any of these times. Data from the two studies which 1.38, p = 0.65) (Fig. 4). There was no heterogeneity at one
VOL. 99-B, No. 4, APRIL 2017
424 H. D. VELDMAN, I. C. HEYLIGERS, B. GRIMM, T. A. E. J. BOYMANS
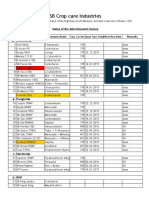
Table I. Details of the included randomised controlled trials (RCTs)
Gender
Age* (yrs)
Patients (n) (female) (%) Implant type ITT/PP
Study Enrolment
design period Total CLH CH Total CLH CH CLH CH CLH CH
Santini et al 200531 RCT, 1 Sept 2000 106 53 53 80.9 (?) 82.1 (7.6) 79.7 (8.6) 79.2 75.5 Bipolar stem Bipolar stem PP
center to Dec 2001 (Zimmer, (Zimmer)
Warsaw,
Indiana)
DeAngelis et al RCT, 1 Mar 2005 130 64 66 82.3 (55 to 100) 82.8 (7.6) 81.8 (9.0) 75.0 78.8 VerSys Beaded VerSys LD/Fx ITT
201230 center to May FullCoat (Zimmer)
2008 (Zimmer)
Taylor et al 201233 RCT, 1 May 2006 160 80 80 85.2 (70 to 99) 85.1 (6.6) 85.3 (7.0) 66.3 71.3 Zweymüller Exeter (Stryker, ITT
center to Nov Alloclassic Kalamazoo,
2008 (Zimmer) Michigan)
Talsnes et al 201332 RCT, 2 2005 to 334 172 162 84.1 (75 to ?) 84.0 (5.1) 84.3 (5.0) 78.5 72.4 Corail (Depuy, Titan (Depuy) PP
centers 2010 Warsaw,
Indiana)
Langslet et al 201429 RCT, 2 Sept 2004 220 108 112 83 (70 to ?) 83.0 (6.3) 83.4 (5.7) 74.0 78.0 Corail (Depuy) Spectron PP
centers to Aug (Smith &
2006 Nephew,
London, United
Kingdom)
*age is displayed as mean (range) for the total population and as mean (standard deviation) for each subgroup; where a value was not included in the
study a ‘?’ has been inserted
CLH, cementless hemiarthroplasty; CH, cemented hemiarthroplasty; ITT, intention-to-treat; PP, per protocol
Table II. Outcome measures and follow-up of the studies
Study outcomes Described complications Follow-up
Santini et al 200531 Complications, hospital length of stay, mortality, Decubitus score, gastric disease, iatrogenic 1 yr
operation time, VELCA functional scores femur fractures, MI, pneumonia, prosthesis
dislocation, pulmonary embolism, urinary
tract infection, wound infection
DeAngelis et al 201230 ADL, blood loss, complications, fatigue/level CVA, ICU stay, major haemorrhage, MI, In hospital, 30 days, 60 days,
of energy, mortality, operation time, physical pneumonia, pulmonary embolism, re- 1 yr
activity operation, wound infection
Taylor et al 201233 Blood loss, complications, hospital length of Cardiovascular complications, dislocation, 6 wks, 6 mths, 1 yr, 2 yrs
stay, mortality, operation time, Oxford Hip fractures, reoperation, respiratory/ urinary
Score, pain, quality of life, use of walking aids tract/ wound infection
Talsnes et al 201332 Blood loss, mortality, operation time None Operation day, 1 yr
Langslet et al 201429 Barthel index, blood loss, complications, Cardiac arrest, dislocation, fracture, MI, 7 days, 30 days, 90 days, 1 yr,
EQ-5D, Harris Hip Score, hospital length of pneumonia, pulmonary embolism, 2 yrs, 5 yrs
stay, mortality, operation time, pain, use of re-operation, thrombosis, wound infection
walking aids
ADL, activities of daily living; ICU, intensive care unit; MI, myocardial infarct; CVA, cerebrovascular accident; EQ-5D, Euroqol-5D; Qol, quality of life;
GI, gastro-intestinal; VELCA, Verona Elderly Care functional score
year follow-up (I2 = 0%, p = 0.45) and a small heterogene- p 0.01) (Fig. 5). There was small heterogeneity (I2 = 10%,
ity at two-year follow-up (I2 = 11%, p= 0.29). p = 0.34).
Additionally, Langslet et al29 studied the rate of mortality Implant-related complications. Implant-related complications
five years post-operatively, when there remained no signifi- were described in three studies.29,31,33 Significantly more
cant difference between the groups (Fig. 4). implant-related complications occurred in the cementless
Complications. Four studies described the number and type group (OR 3.15, 95% CI 1.55 to 6.41, p = 0.002) (Fig. 5).
of complications for each group.29-31,33 Only Taylor et al33 There was small heterogeneity (I2 = 41%, p = 0.18).
found a significant difference between the groups, noting Cardiovascular complications. Four studies described cardi-
fewer complications in the cemented group when compared ovascular complications.29-31,33 There was no significant
with the cementless group (OR 2.54, 95% CI 1.34 to 4.83). difference between the groups in any study, or after pooling
The total number of complications in the four studies of the data (OR 0.54, 95% CI 0.24 to 1.20, p = 0.13)
ranged from 20.3%30 to 55.0%33 in the cementless group (Fig. 5). There was no heterogeneity (I2 = 0%, p = 0.70).
and from 17.9%29 to 32.5%33 in the cemented group. Pool- Local complications. Four studies mentioned local compli-
ing revealed a significantly higher number of complications cations.29-31,33 Pooling did not indicate a significant differ-
in the cementless groups (OR 1.61, 95% CI 1.12 to 2.31, ence between groups (OR 0.71, 95% CI 0.27 to 1.86,
THE BONE & JOINT JOURNAL
CEMENTED VERSUS CEMENTLESS HEMIARTHROPLASTY FOR A DISPLACED FRACTURE OF THE FEMORAL NECK 425
0.36 days, 95% CI -1.13 to 1.85, p = 0.63) (Fig. 6). There
Incomplete outcome data (attrition bias): operation and hospital outcomes
was no heterogeneity (I2 = 0%, p = 0.87).
Intra-operative blood loss. The mean intra-operative blood
loss ranged from 251 ml31 to 390 ml29 in the four studies
which described blood loss.29,30,32,33 There was no signifi-
Incomplete outcome data (attrition bias): functional outcomes
cant difference between the groups in two studies,30,33 the
other two recorded less blood loss in the cementless
group (WMD -90.00 mL, 95% CI -136.99 to -43.01 and
WMD -75.00 mL, 95% CI -119.52 to -30.48).29,32 Data
Incomplete outcome data (attrition bias): mortality
Blinding of outcome assessment (detection bias)
were pooled according to the random effects model because
Random sequence generation (selection bias)
of high heterogeneity (I2 = 82%, p < 0.001). There was no
significant difference in blood loss after pooling of the
Allocation concealment (selection bias)
data (WMD -36.19 ml, 95% CI -89.45 to 17.07, p = 0.18)
Selective reporting (reporting bias)
(Fig. 7).
Operating time. All five studies reported this; two found no
difference between the two groups.30,33 The other three
reported a longer operating time in the cemented
group.29,31,32 The pooled data also found a significantly
shorter duration of surgery in the cementless group (WMD
-9.96 minutes, 95% CI -12.93 to -6.98, p < 0.001) (Fig. 8).
Heterogeneity was low (I2 = 46%, p = 0.12).
Others bias
Functional outcomes. Four studies investigated these.29-31,33
However, the data could not be pooled as it was assessed
in different ways and at different times (Table II). The
individual studies reported comparable functional out-
DeAngelis 201230 ? ? + + + + + ?
comes for the cemented and cementless groups at all
Langslet 201429 + + + + + + + + follow-up times.29-31,33 However, Taylor et al33 reported
better functional results in the cemented group at six
Santini 200531 − ? ? ? ? ? + − weeks post-operatively, with regards to pain when flexing
the hip to 45° and the Oxford Hip Score.34 At six months
Talsnes 201332 ? ? ? + ? + ? post-operatively, the timed up and go (TUG) test35 was
lower in the cemented groups, representing a better out-
Taylor 201233 + + + + + ? + + come.33 Langslet et al,29 however, found a higher Harris
Hip Score36 and therefore a better functional outcome in
Fig. 2
the cementless group at five years post-operatively. There
Assessment of the risk of bias in the studies; ‘+’ low risk of bias, ‘?’ were no significant differences between the cemented and
unclear risk of bias, ‘-’ high risk of bias.29-33
cementless group for all other functional measurements
and follow-up times (Table II).
Risk of bias across studies. Since the outcome measures
‘mortality’ and ‘operating time’ were recorded in all the
p = 0.49) (Fig. 5). There was no heterogeneity (I2 = 0%, studies, funnel plots of these data were obtained. The fun-
p = 0.61). nel plots are asymmetrical. However, because of the limited
General complications. The same four studies described number of included studies, it remains questionable if this is
general complications.29-31,33 There was no significant dif- the result of publication bias.
ference between the groups in any study or after pooling of Current versus previous generation of stems. In order to
the data (OR 1.09, 95% CI 0.62 to 1.91, p = 0.76) (Fig. 5). examine whether the analyses of outcomes in exclusively
There was no heterogeneity (I2 = 0%, p = 0.74). current hip stems leads to different conclusions than analy-
Number of re-operations. This was described in three stud- ses of exclusively previous stems, further analyses were per-
ies.29-31 There was no significant difference between groups formed. The four most recently published systematic
within any study or after pooling of data (OR 1.24, 95% CI reviews and meta-analyses12-15 were searched for studies
0.53 to 2.88, p = 0.62) (Fig. 5). There was no heterogeneity investigating exclusively previous stems such as the
(I2 = 0%, p = 0.62). Thompson and Austin Moore. Seven studies were
Length of hospital stay. This was described by three stud- identified37-43 and checked for the same outcome measures
ies.29,31,33 The mean length ranged from 7.829 to 27.233 as investigated in the analyses of current stems. Unfortu-
days. There was no significant difference between the nately, one study was not accessible43 and one did not
groups in any study or after pooling of the data (WMD describe any of the outcomes of interest.41 The data from
VOL. 99-B, No. 4, APRIL 2017
426 H. D. VELDMAN, I. C. HEYLIGERS, B. GRIMM, T. A. E. J. BOYMANS
Random sequence generation (selection bias)
Allocation concealment (selection bias)
Blinding of outcome assessment (detection bias)
Incomplete outcome data (attrition bias): functional outcomes
Incomplete outcome data (attrition bias): operation and hospital outcomes
Incomplete outcome data (attrition bias): mortality
Selective reporting (reporting bias)
Others bias
0% 25% 50% 75% 100%
Low risk of bias Unclear risk of bias High risk of bias
Fig. 3
Summary of the assessment of the risk of bias.
Cemented Cementless Odds ratio Odds ratio
Study or subgroup Events Total Events Total Weight % M-H, Fixed, 95% CI Yr M-H,Fixed,95% CI
1.1.2 1-year mortality
Santini 2005 13 53 14 53 10.4 0.91 (0.38 to 2.17) 2005
Taylor 2012 25 80 23 80 15.6 1.13 (0.57 to 2.22) 2012
DeAngelis 2012 16 66 13 64 9.9 1.26 (0.55 to 2.88) 2012
Talsnes 2013 39 162 52 172 37.9 0.73 (0.45 to 1.19) 2013
Langslet 2014 21 112 32 108 26.2 0.55 (0.29 to 1.03) 2014
Subtotal (95% CI) 473 477 100 0.82 (0.61 to 1.09)
Total events 114 134
Heterogeneity: chi2 = 3.69, df = 4 (p = 0.45); I2 = 0%
Test for overall effect: Z = 1.38 (p = 0.17)
1.1.3 2-year mortality
Taylor 2012 35 80 32 80 39.4 1.17 (0.62 to 2.19) 2012
Langslet 2014 32 112 38 108 60.6 0.74 (0.42 to 1.30) 2014
Subtotal (95% CI) 192 188 100.0 0.91 (0.60 to 1.38)
Total events 67 70
Heterogeneity: chi2 = 1.13, df = 1 (p = 0.29); I2 = 11%
Test for overall effect: Z = 0.46 (p = 0.65)
1.1.4 5-year mortality
Langslet 2014 63 112 64 108 100.0 0.88 (0.52 to 1.51) 2014
Subtotal (95% CI) 112 108 100.0 0.88 (0.52 to 1.51)
Total events 63 64
Heterogeneity Not applicable
Test for overall effect: Z = 0.45 (p = 0.65)
0.2 0.5 1 2 5
Favours (cemented) Favours (cementless)
Fig. 4
Forest plot of mortality one, two and five years after cemented versus cementless hemiarthroplasty (CI, confidence interval; M-H, Mantel-Haenszel;
df, degrees of freedom).29-33
the remaining five studies37-40,42 were pooled as described Comparison of the results (ORs and WMDs) of previous
for the studies on current generation stems. A total of six stems with those of current stems revealed similar trends.
outcomes could be compared with our analyses of current The significantly higher number of complications in the
hip stems (Table III). cementless group was only found in the current generation
In the comparison of previous generation cemented ver- of stems.
sus cementless stems, only the shorter operating time in the
cementless groups was statistically significant. The mortal- Discussion
ity one year post-operatively, total number of complica- The goal of this systematic review and meta-analysis was to
tions, number of re-operations, length of stay and blood compare the results of current cemented and cementless
loss did not differ between the groups. hemiarthroplasty of the hip.
THE BONE & JOINT JOURNAL
CEMENTED VERSUS CEMENTLESS HEMIARTHROPLASTY FOR A DISPLACED FRACTURE OF THE FEMORAL NECK 427
Cementless Cemented Odds ratio Odds ratio
Study or subgroup Events Total Events Total Weight % M-H, Fixed, 95% CI Yr M-H,Fixed,95% CI
5.1.5 Total number of complicatlons
Santini 2005 22 53 16 53 20.3 1.64 (0.74 to 3.66) 2005
DeAngelis 2012 13 64 12 66 20.4 1.15 (0.48 to 2.75) 2012
Taylor 2012 44 80 26 80 25.4 2.54 (1.34 to 4.83) 2012
Langslet 2014 22 108 20 112 33.9 1.18 (0.60 to 2.31) 2014
Subtotal (95% CI) 305 311 100.0 1.61 (1.12 to 2.31)
Total events 101 74
Heterogeneity: chi2 = 3.34, df = 3 (p = 0.34); I2 = 10%
Test for overall effect: Z = 2.58 (p = 0.01)
5.1.6 Number of implant related complications
Santini 2005 2 53 1 53 10.2 2.04 (0.18 to 23.19) 2005
Taylor 2012 18 80 3 80 24.6 7.45 (2.10 to 26.46) 2012
Langslet 2014 11 108 7 112 65.3 1.70 (0.63 to 4.56) 2014
Subtotal (95% CI) 241 245 100.0 3.15 (1.55 to 6.41)
Total events 31 11
Heterogeneity: chi2 = 3.39, df = 2 (p = 0.18); I2 = 41%
Test for overall effect: Z = 3.16 (p = 0.002)
5.1.7 Number of cardiovascular complications
Santini 2005 2 53 4 53 22.5 0.48 (0.08 to 2.74) 2005
DeAngelis 2012 1 64 2 66 11.3 0.51 (0.04 to 5.74) 2012
Taylor 2012 6 80 7 80 37.8 0.85 (0.27 to 2.64) 2012
Langslet 2014 1 108 5 112 28.4 0.20 (0.02 to 1.74) 2014
Subtotal (95% CI) 305 311 100.0 0.54 (0.24 to 1.20)
Total events
Heterogeneity: chi2 = 1.42, df = 3 (p = 0.70); I2 = 0%
Test for overall effect: Z = 1.51 (p = 0.13)
5.1.8 Number of local complications
Santini 2005 0 53 1 53 14.7 0.33 (0.01, to 8.21) 2005
DeAngelis 2012 1 64 1 66 9.6 1.03 (0.06 to 16.85) 2012
Taylor 2012 5 80 4 80 37.1 1.27 (0.33 to 4.90) 2012
Langslet 2014 1 108 4 112 38.5 0.25 (0.03 to 2.29) 2014
Subtotal (95% CI) 305 311 100.0 0.71 (0.27 to 1.86)
Total events
Heterogeneity: chi2 = 1.83, df = 3 (p = 0.61); I2 = 0%
Test for overall effect: Z = 0.69 (p = 0.49)
5.1.9 Number of general complications
Santini 2005 17 53 15 53 43.1 1.20 (0.52 to 2.75) 2005
DeAngelis 2012 1 64 3 66 12.3 0.33 (0.03 to 3.29) 2012
Taylor 2012 11 80 10 80 36.5 1.12 (0.45 to 2.80) 2012
Langslet 2014 3 108 2 112 8.1 1.57 (0.26 to 9.59) 2014
Subtotal (95% CI) 305 311 100.0 1.09 (0.62 to 1.91)
Total events 32 30
Heterogeneity: chi2 = 1.24, df = 3 (p = 0.74); I2 = 0%
Test for overall effect: Z = 0.31 (p = 0.76)
5.1.10 Number of reoperations
Taylor 2012 4 80 2 80 19.5 2.05 (0.37 to 11.54) 2012
DeAngelis 2012 0 64 1 66 15.1 0.34 (0.01 to 8.46) 2012
Langslet 2014 8 108 7 112 65.4 1.20 (0.42 to 3.43) 2014
Subtotal (95% CI) 252 258 100.0 1.24 (0.53 to 2.88)
Total events 12 10
Heterogeneity: chi2 = 0.96, df = 3 (p = 0.62); I2 = 0%
Test for overall effect: Z = 0.49 (p = 0.62)
0.02 0.1 1 10 50
Favours (cementless) Favours (cemented)
Fig. 5
Forest plot of complications after cemented versus cementless hemiarthroplasty (CI, confidence interval; M-H, Mantel-Haenszel; df, degrees of
freedom).29-33
Many previously performed studies included stems of a Thompson stems; six of eight studies in the review by Luo
previous generation, or those which are now unavailable or et al,13 four of seven in the review by Li et al,12 seven of 12
have been discontinued. This problem is extensively in the review by Ning et al14and five of seven in the review
described in the literature.12,15,19,29,31,33,44-46 However, this by Parker et al.15
is the first systematic review which only includes RCTs The systematic review of Luo et al13 found no significant
involving current generation stems. Previous systematic difference in the mortality or the number of complications
reviews are largely based on data from Austin Moore and and re-operations but found that patients with a cemented
VOL. 99-B, No. 4, APRIL 2017
428 H. D. VELDMAN, I. C. HEYLIGERS, B. GRIMM, T. A. E. J. BOYMANS
Cementless Cemented Mean difference Mean difference
Study or subgroup Mean SD Total Mean SD Total Weight % IV, Fixed, 95% CI Year IV, Fixed, 95% CI
Santini 2005 17.46 6.29 53 17.23 9.1 53 25.0 0.23 (-2.75 to 3.21) 2005
Taylor 2012 26.5 14.26 80 27.2 14.6 80 11.1 -0.70 (-5.17 to 3.77) 2012
Langslet 2014 8.4 9.02 108 7.8 4.11 112 63.9 0.60 (-1.26 to 2.46) 2014
Total (95% CI) 241 245 100.0 0.36 (-1.13 to 1.85)
Heterogeneity: chi2 = 0.29, df = 2 (p = 0.87); I2 = 0%
Test for overall effect: Z = 0.48 (p = 0.63) -4 -2 0 2 4
Favours (cementless) Favours (cemented)
Fig. 6
Forest plot of the length of stay after cemented versus cementless hemiarthroplasty (SD, standard deviation; CI, confidence interval; IV, inverse-
variance method; df, degrees of freedom).29,31,33
Cementless Cemented Mean difference Mean difference
Study or subgroup Mean SD Total Mean SD Total Weight % IV, Random, 95% CI Year IV, Random, 95% CI
DeAngelis 2012 279 177 64 257 30.8 66 25.2 22.00 (-22 to 66.00) 2012
Taylor 2012 251 156.8 80 254 130.8 80 25.1 -3.00 (-47.74 to,41.74) 2012
Talsnes 2013 260 163 172 335 242 162 25.1 -75.00 (-119.52 to -30.48) 2013
Langslet 2014 300 171.9 108 390 183.7 112 24.6 -90.00 (-136.99 to -43.01) 2014
Total (95% CI) 424 420 100.0 -36.19 (-89.45 to 17.07)
2 2 2
Heterogeneity: Tau = 2424.75; chi = 16.77, df = 3 (p = 0.0008); I = 82%
Test for overall effect: Z = 1.33 (p = 0.18) -200 -100 0 100 200
Favours (cementless) Favours (cemented)
Fig. 7
Forest plot of the blood loss after cementedversus cementless hemiarthroplasty (SD, standard deviation; CI, confidence interval; IV, inverse-variance
method; df, degrees of freedom).29,30,32,33
Cementless Cemented Mean difference Mean difference
Study or subgroup Mean SD Total Mean SD TotalWeight % IV, Fixed, 95% CI Year IV, Fixed, 95% CI
Santini 2005 56.98 55 53 75 22.43 53 3.5 18.02 (-34.01 to -2.03)2005
Taylor 2012 74.7 18.8 80 79.3 17.2 80 28.4 -4.60 (-10.18 to 0.98) 2012
DeAngelis 2012 103.6 32 64 108.2 30.8 66 7.6 -4.60 (-15.40 to 6.20) 2012
Talsnes 2013 71 22 172 84 30 162 27.5-13.00 (-18.67 to -7.23) 2013
Langslet 2014 70.2 19.3 108 82.6 19.8 112 33.1 -12.40 (-17.57 to -7.23) 2014
Total (95% CI) 477 473 100.0 -9.96 (-12.93 to-6.98)
Heterogeneity: chi2= 7.42, df = 4 (p = 0.12); I2 = 46% -20 -10 0 10 20
Test for overall effect: Z = 6.56 (p < 0.00001) Favours (cementless) Favours (cemented)
Fig. 8
Forest plot of the blood loss after cementedversus cementless hemiarthroplasty (SD, standard deviation; CI, confidence interval; IV, inverse-variance
method; df, degrees of freedom).29-33
stem had better functional results and less pain.13 Li et al12 stems, emphasising the relevance of the current review of
included two more recent RCTs30,33 but did not include the modern stems.
three studies by Faraj and Branfoot,37 Harper47 and Santini Synthesis of results. The rates of mortality at one month
et al.31 However, they also concluded that cemented stems and one, two and five years post-operatively were equal in
achieve better function of the hip, less pain and fewer both groups, indicating that the use of cement has no detri-
implant-related complications compared with cementless mental effect on the short- and mid-term mortality.
stems.12 The risk of mortality, re-operation or cardiovascu- We found that cementless stems were associated with a
lar, cerebrovascular, local or general complications, were higher total number of complications when compared with
identical in both groups. The most recent systematic review cemented stems. There were also more implant-related
was conducted by Ning et al14 in 2014. Based on two stud- complications, such as periprosthetic fractures, aseptic
ies, they concluded that there was no significant difference loosening and dislocation. This is in agreement with previ-
between cementless and cemented stems. The most recent ously published observational studies involving current
Cochrane review, from 2010, was conducted by Parker et generation stems.8,46,48 Also, a recently published RCT49
al.15 They concluded that there was reasonable evidence comparing cemented and cementless fixation in patients
that there was less pain and more mobility when a who were treated with a hemiarthroplasty or total hip
cemented stem was used. They also stated that these differ- arthroplasty (THA) after a displaced fracture of the femoral
ences may not exist with cementless hydroxyapatite-coated neck, found a higher number of periprosthetic fractures in
THE BONE & JOINT JOURNAL
CEMENTED VERSUS CEMENTLESS HEMIARTHROPLASTY FOR A DISPLACED FRACTURE OF THE FEMORAL NECK 429
Table III. Results of analyses on cemented versus cementless hemiarthroplasty in exclusively current generation stems and in exclusively previous
generation stems
Current generation stems (present
report) Analysed (n) Previous generation stems Analysed (n)
Patients Patients
OR/WMD Favours 95% CI Studies CLH:CH OR/WMD Favours 95% CI Studies CLH:CH
Mortality 1-yr 0.82 CH 0.61 to 1.09 5 134:114 0.93 CH 0.67 to 1.30 5 390:347
post-operatively
Total number of 1.61* CH 1.12 to 2.31 4 305:311 1.14† CH 0.41 to 3.15 2 226:227
complications
Total number of 1.24 CH 0.53 to 2.88 3 252:258 1.64 CH 0.77 to 3.51 2 278:223
re-operations
Length of hospital 0.36 CH -1.13 to 1.85 3 241:245 1.95 CH -0.16 to 4.07 3 292:304
stay (days)
Intra-operative -36.19† CLH -8.45 to 17.07 4 424:420 -49.00 CLH -120.10 to 22.10 1 26:27
blood loss (ml)
Duration of surgery -9.96* CLH -12.93 to -6.98 5 477:473 -6.97* CLH -9.49 to -4.45 2 226:227
(mins)
*OR or WMD considered statistically significant (p < 0.05)
†Data pooled according the random effects model due to moderate heterogeneity (I2 ≥ 50%)
OR, odds ratio (for dichotomous outcomes); WMD, weighted mean difference (for continuous outcomes); CI, confidence interval; CLH, cementless
hemiarthroplasty; CH, cemented hemiarthroplasty
patients with a cementless stem. The number of re- which is low considering the high incidence of fracture of
operations for any reason did not differ between the the femoral neck. This led to asymmetrical funnel plots
groups. The incidence of local and general complications which are barely useable in the assessment of publication
was also equal in the two groups. Interestingly, the number bias in the studies.
of cardiovascular complications did not differ between the We acknowledge that our strict inclusion criteria is at the
groups in contradistinction to the widely held view that expense of statistical power, which is not necessarily high in
there is an association between cement and cardiovascular meta-analyses.54,55 Nevertheless, pooling of the data
complications known as the ‘bone cement implantation revealed statistically significant evidence regarding compli-
syndrome’.50 This was also described by Li et al.12 cations that were not identified in three RCTs.29-31 In addi-
The length of stay in hospital was equal in both groups, tion, a significant difference was revealed regarding the
suggesting that both groups start mobilisation within the operating time, which was not found by half of the studies
same time period. The blood loss was comparable between describing this parameter.30,33 This suggests that the meta-
the groups. The mean operating time was nine minutes analysis achieved sufficient power to detect significant dif-
shorter for cementless stems, which was statistically signif- ferences.
icant (p < 0.001). This will be partly due to the time for the Post hoc power analyses were conducted, which revealed
polymerisation of the cement. The shorter operating time in that the achieved power differed among the analyses (range
this group may have some economic and organisational 5.3% to 100.0%), with three of the 12 analyses achieving a
benefits, but should not be overrated. The longer anaes- statistical power of ≥ 80%. The analyses that were ade-
thetic time in the cemented group results in higher costs.51 quately powered were for the operating time, blood loss
There are some studies on revision hip surgery52 and total and implant related complications (100%, 92.2% and
knee arthroplasty53 that have investigated the correlation 90.9%, respectively). The achieved power in the analysis of
between operating time and the rate of complications; how- the total number of complications was 72.8%. The sub-
ever, no such data are available for hemiarthroplasty. analyses within the total number of complications regard-
The data about the functional outcomes could not be ing cardiovascular, local, general complications and the
pooled as different functional scores and follow-up times number of re-operations were underpowered (32%,
were recorded in the studies. The effect of using cement 10.3%, 5.3% and 7.1%, respectively). The statistical
with a hemiarthroplasty on the functional results thus power of the analyses of mortality after one, two and five
remains unclear. years was also low (28.9%, 12.4% and 6.6%, respectively).
The most likely explanation for an increased rate of com- Finally, the length of stay in hospital achieved a statistical
plications when using contemporary cementless stems power of only 6.5%. In conclusion, not all analyses in the
could be the improvement due to improved cement, the current study were adequately powered. This, however, is
design of the stem and/or the surgical techniques for a not uncommon in meta-analyses in general.54,55 Turner et
cemented procedure. al54 studied the role of underpowered studies in Cochrane
Limitations. This meta-analysis has limitations. First, there reviews (n = 1991), including 14 886 meta-analyses. They
were only five RCTs, describing 950 patients (950 hips), concluded that the proportion of Cochrane meta-analyses
VOL. 99-B, No. 4, APRIL 2017
430 H. D. VELDMAN, I. C. HEYLIGERS, B. GRIMM, T. A. E. J. BOYMANS
with a power of ≥ 80%, to detect a relative reduction of risk times more common. The number of re-operations and car-
of 30% which had been published was 22%; 12% were diovascular, local and general complications did not differ
powered between 50% and 80%, and 66% were under- between the groups. The use of cement was not associated
powered. Therefore, the risk of any meta-analysis being with a detrimental effect on mortality five years post-oper-
underpowered should be kept in mind when interpreting atively. There were no differences in the length of stay in
results.54 hospital and the blood loss. The operating time was signif-
It should be noticed that the ORs and WMDs are accom- icantly shorter in the cementless group. Due to differences
panied with relatively wide 95% CIs. Thus, equal, higher or in follow-up times and measurement tools in the studies, no
lower risks are established, but the exact size of detected conclusions can be made about the functional outcomes
differences remains difficult to determine. Additionally, the after treatment with a hemiarthroplasty based on this meta-
individual studies carry a substantial risk of bias in their analysis.
methodology. It is not known how and to what extent these In conclusion, although cemented hemiarthroplasty
risks of bias influence our findings. seems to be a safer option than cementless hemiarthro-
Some outcome specific limitations have to be acknowl- plasty, there remains a need for a methodologically sound,
edged. Due to differences in follow-up times between stud- large multicentre RCT comparing modern cemented and
ies, not all data about every follow-up time could be cementless hemiarthroplasty stems in the the medium- and
pooled. Mortality was therefore only analysed at one long-term, not only focusing on mortality and complica-
month and one, two and five years post-operatively; the tions but also on patient reported outcome measures.
five-year mortality being only described in one study.29 The
difference in follow-up times and the different functional Take home message:
outcomes made it impossible to pool these data. Therefore, - This is the first meta-analysis comparing cemented and
cementless hemiarthroplasty based on RCTs, investigating
the overall effect of cementing the hemiarthroplasty on the
exclusively current generation hip stems.
functional outcome remains unclear. In order to provide - In hemiarthroplasty of the hip, current generation cemented stems seem
more insight into the functional outcomes after cemented to be a safer option resulting in fewer implant-related complications and
versus cementless hemiarthroplasty, future RCTs should similar mortality compared with current generation cementless stems.
record validated functional outcomes at standardised times - Although the duration of surgery in cementless hemiarthroplasty is
shorter, the use of cemented fixation in hemiarthroplasty after a femoral
post-operatively.
neck fracture is thus recommended in current practice.
Finally, the total number of complications was based on
the complications which were reported in the studies. Pos- Author contributions:
H. D. Veldman: Study idea, Study design, Data collection, Data analysis, Writing
sible differences in the definition of a complication in the the paper.
studies may affect our results. Differences in the length of B. Grimm: Study design, Data analysis, Writing the paper.
I. C. Heyligers: Study design, Writing the paper.
follow-up might influence the number of complications T. A. E. J. Boymans: Study idea, Study design, Data collection, Data analysis,
reported in each study. The rates of complications which Writing the paper.
typically occur in the mid- or long-term, such as aseptic No benefits in any form have been received or will be received from a commer-
cial party related directly or indirectly to the subject of this article.
loosening, may therefore differ between studies. Also, other
This article was primary edited by E. Moulder and first proof edited by J. Scott.
factors might influence the occurrence of specific
complications. For example, in THA it is described that
design and location of fixation of the cementless stem in the References
patients’ specific proximal femur morphology influences 1. Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden
of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res
the osteointegration. In case of failing to achieve osteointe- 2007;22:465–475.
gration, it might be necessary to perform revision sur- 2. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the chal-
gery.56,57 The type of cementless stem used therefore, might lenges ahead. Lancet 2009;374:1196–1208.
play a role in the number of implant-related complications 3. Cooper C, Campion G, Melton LJ III. Hip fractures in the elderly: a world-wide pro-
jection. Osteoporos In 1992;2:285–289.
or re-operations. Furthermore, the features of the cement 4. Thorngren KG, Hommel A, Norrman PO, Thorngren J, Wingstrand H. Epidemi-
used for fixating the implant may affect the outcome. For ology of femoral neck fractures. Injury 2002;33(Suppl 3):C1–C7.
example, a recent study by Sprowson et al58 showed a sig- 5. Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD. Surgical man-
agement of hip fractures: an evidence-based review of the literature. I: femoral neck
nificantly lower rate of surgical site infection after fixating fractures. J Am Acad Orthop Surg 2008;16:596–607.
the implant with dual-antibiotic impregnated cement, when 6. Wang F, Zhang H, Zhang Z, Ma C, Feng X. Comparison of bipolar hemiarthroplasty
compared with standard low dose single antiobiotic loaded and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly:
a meta-analysis. BMC Musculoskelet Disord 2015;16:229.
bone cement. 7. Yurdakul E, Karaaslan F, Korkmaz M, Duygulu F, Baktır A. Is cemented bipolar
Our study is the first meta-analysis comparing cemented hemiarthroplasty a safe treatment for femoral neck fracture in elderly patients? Clin
and cementless hemiarthroplasty based on RCTs investigat- Interv Aging 2015;10:1063–1067.
8. Grammatopoulos G, Wilson HA, Kendrick BJ, et al. Hemiarthroplasty using
ing exclusively current generation stems. Our analysis sug- cemented or uncemented stems of proven design: a comparative study. Bone Joint J
gests that cementless stems have a 61% higher number of 2015;97-B:94–99.
complications, in particular implant-related complications 9. Middleton RG, Uzoigwe CE, Young PS, et al. Peri-operative mortality after hemi-
arthroplasty for fracture of the hip: does cement make a difference? Bone Joint J
such as periprosthetic fractures, which are almost three- 2014;96-B:1185–1191.
THE BONE & JOINT JOURNAL
CEMENTED VERSUS CEMENTLESS HEMIARTHROPLASTY FOR A DISPLACED FRACTURE OF THE FEMORAL NECK 431
10. Ng ZD, Krishna L. Cemented versus cementless hemiarthroplasty for femoral neck 34. Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of
fractures in the elderly. J Orthop Surg (Hong Kong) 2014;22:186–189. patients about total hip replacement. J Bone Joint Surg [Br] 1996;78-B:185–190.
11. Bell KR, Clement ND, Jenkins PJ, Keating JF. A comparison of the use of unce- 35. Podsiadlo D, Richardson S. The timed ‘‘Up & Go’’: a test of basic functional mobil-
mented hydroxyapatite-coated bipolar and cemented femoral stems in the treatment ity for frail elderly persons. J Am Geriatr Soc 1991;39:142–148.
of femoral neck fractures: a case-control study. Bone Joint J 2014;96-B:299–305. 36. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures:
12. Li T, Zhuang Q, Weng X, Zhou L, Bian Y. Cemented versus uncemented hemiar- treatment by mold arthroplasty. An end-result study using a new method of result
throplasty for femoral neck fractures in elderly patients: a meta-analysis. PLoS One evaluation. J Bone Joint Surg [Am] 1969;51-A:737–755.
2013;8:68903. 37. Faraj AA, Branfoot T. Cemented versus uncemented Thompson’s prostheses: a
13. Luo X, He S, Li Z, Huang D. Systematic review of cemented versus uncemented functional outcome study. Injury 1999;30:671–675.
hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop 38. Emery RJ, Broughton NS, Desai K, Bulstrode CJ, Thomas TL. Bipolar hemiar-
Trauma Surg 2012;132:455–463. throplasty for subcapital fracture of the femoral neck. A prospective randomised trial
14. Ning GZ, Li YL, Wu Q, et al. Cemented versus uncemented hemiarthroplasty for dis- of cemented Thompson and uncemented Moore stems. J Bone Joint Surg [Br]
placed femoral neck fractures: an updated meta-analysis. Eur J Orthop Surg Trauma- 1991;73-B:322–324.
tol 2014;24:7–14. 39. Parker MI, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty
15. Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone for intracapsular hip fractures: A randomised controlled trial in 400 patients. J Bone
cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev Joint Surg [Br] 2010;92-B:116–122.
2010;6:CD001706. 40. Sadr B, Arden GP. A comparison of the stability of proplast-coated and cemented
16. Rogmark C, Leonardsson O, Garellick G, Kärrholm J. Monoblock hemiarthro- Thompson prostheses in the treatment of subcapital femoral fractures. Injury
plasties for femoral neck fractures--a part of orthopaedic history? Analysis of national 1977;8:234–237.
registration of hemiarthroplasties 2005-2009. Injury 2012;43:946–949. 41. Sonne-Holm S, Walter S, Jensen JS. Moore hemi-arthroplasty with and without
17. Gjertsen JE, Fenstad AM, Leonardsson O, et al. Hemiarthroplasties after hip bone cement in femoral neck fractures. A clinical controlled trial. Acta Orthop Scand
fractures in Norway and Sweden: a collaboration between the Norwegian and Swed- 1982;53:953–956.
ish national registries. Hip 2014;24:223–230. 42. Harper WMGP, Greg PJ. The treatment of intracapsular proximal femoral frac-
18. Leonardsson O, Garellick G, Kärrholm J, Akesson K, Rogmark C. Changes in tures: A randomized prospective trial. J Bone Joint Surg [Am] 1992;74-A(Suppl
implant choice and surgical technique for hemiarthroplasty. 21,346 procedures from III):282.
the Swedish Hip Arthroplasty Register 2005-2009. Acta Orthop 2012;83:7–13. 43. Cumming D, Parker M. Randomised trial of cemented versus uncemented hemiar-
19. Rogmark C, Fenstad AM, Leonardsson O, et al. Posterior approach and unce- throplasty for displaced intracapsular fractures. J Bone Joint Surg [Br] 2012;B(SUPP
mented stems increases the risk of reoperation after hemiarthroplasties in elderly hip III):63.
fracture patients. Acta Orthop 2014;85:18–25. 44. Chana R, Mansouri R, Jack C, et al. The suitability of an uncemented hydroxyapa-
20. No authors listed. Australian Orthopaedic Association National Joint Replacement tite coated (HAC) hip hemiarthroplasty stem for intra-capsular femoral neck fractures
Registry. Annual Report. Adelaide: AOA; 2015. https://aoanjrr.sahmri.com/annual- in osteoporotic elderly patients: the Metaphyseal-Diaphyseal Index, a solution to pre-
reports-2016 (date last accessed 24 January 2017). venting intra-operative periprosthetic fracture. J Orthop Surg Res 2011;6:59.
21. Jalovaara P, Virkkunen H. Quality of life after primary hemiarthroplasty for femoral 45. Jameson SS, Jensen CD, Elson DW, et al. Cemented versus cementless hemiar-
neck fracture. 6-year follow-up of 185 patients. Acta Orthop Scand 1991;62:208–217. throplasty for intracapsular neck of femur fracture--a comparison of 60,848 matched
22. Fang C, Liu RP, Lau TW, et al. Is It Time to Phase Out the Austin Moore Hemiarthro- patients using national data. Injury 2013;44:730–734.
plasty? A Propensity Score Matched Case Control Comparison versus Cemented 46. Morris K, Davies H, Wronka K. Implant-related complications following hip hemi-
Hemiarthroplasty. Biomed Res Int 2016;2016:7627216. arthroplasty: a comparison of modern cemented and uncemented prostheses. Eur J
23. Lin CC, Huang SC, Ou YK, et al. Survival of patients aged over 80 years after Aus- Orthop Surg 2015;25:1161–1164.
tin-Moore hemiarthroplasty and bipolar hemiarthroplasty for femoral neck fractures. 47. Harper WMGP. The treatment of intracapsular proximal femoral fractures: a rand-
Asian J Surg 2012;35:62–66. omized prospective trial. J Bone Joint Surg [Br] 1992;74-B:282.
24. Sadoghi P, Thaler M, Janda W, et al. Comparative pooled survival and revision 48. Yli-Kyyny T, Ojanperä J, Venesmaa P, et al. Perioperative complications after
rate of Austin-Moore hip arthroplasty in published literature and arthroplasty register cemented or uncemented hemiarthroplasty in hip fracture patients. Scand J Surg
data. J Arthroplasty 2013;28:1349–1353. 2013;102:124–128.
25. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic 49. Inngul C, Blomfeldt R, Ponzer S, Enocson A. Cemented versus uncemented
reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006– arthroplasty in patients with a displaced fracture of the femoral neck: a randomised
1012. controlled trial. Bone Joint J 2015;97-B:1475–1480.
26. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Inter- 50. Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation
ventions Version 510 [updated March 2011]. http://www.cochrane-handbook.org. syndrome. Br J Anaesth 2009;102:12–22.
(date last accessed 24 January 2017). 51. Tripuraneni KR, Carothers JT, Junick DW, Archibeck MJ. Cost comparison of
27. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in cementless versus cemented hemiarthroplasty for displaced femoral neck fractures.
meta-analyses. BMJ 2003;327:557–560. Orthopedics 2012;35:1461–1464.
28. Figved W, Opland V, Frihagen F, et al. Cemented versus uncemented hemiarthro- 52. Kessler S, Kinkel S, Käfer W, Puhl W, Schochat T. Influence of operation dura-
plasty for displaced femoral neck fractures. Clin Orthop Relat Res 2009;467:2426– tion on perioperative morbidity in revision total hip arthroplasty. Acta Orthop Belg
2435. 2003;69:328–333.
29. Langslet E, Frihagen F, Opland V, et al. Cemented versus uncemented hemiarthro- 53. Peersman G, Laskin R, Davis J, Peterson MG, Richart T. Prolonged operative
plasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin time correlates with increased infection rate after total knee arthroplasty. HSS J
Orthop Relat Res 2014;472:1291–1299. 2006;2:70–72.
30. Deangelis JP, Ademi A, Staff I, Lewis CG. Cemented versus uncemented hemiar- 54. Turner RM, Bird SM, Higgins JP. The impact of study size on meta-analyses:
throplasty for displaced femoral neck fractures: a prospective randomized trial with examination of underpowered studies in Cochrane reviews. PLoS One 2013;8:59202.
early follow-up. J Orthop Trauma 2012;26:135–140. 55. Hedges LV, Pigott TD. The power of statistical tests in meta-analysis. Psychol
31. Santini S, Rebeccato A, Bolgan I. Turi G. Hip fractures in elderly patients treated Methods 2001;6:203–217.
with bipolar hemiarthroplasty: comparison between cemented and cementless 56. Cooper HJ, Jacob AP, Rodriguez JA. Distal fixation of proximally coated tapered
implants. J Orthopaed Traumatol 2005;6:80–87. stems may predispose to a failure of osteointegration. J Arthroplasty 2011;26(6
32. Talsnes O, Hjelmstedt F, Pripp AH, Reikerås O, Dahl OE. No difference in mor- Suppl):78–83.
tality between cemented and uncemented hemiprosthesis for elderly patients with 57. Su EP, Barrack RL. Cementless femoral fixation: not all stems are created equally.
cervical hip fracture. A prospective randomized study on 334 patients over 75 years. Bone Joint J 2013;95-B(11 Suppl A):53–56.
Arch Orthop Trauma Surg 2013;133:805–809.
58. Sprowson AP, Jensen C, Chambers S, et al. The use of high-dose dual-impreg-
33. Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: nated antibiotic-laden cement with hemiarthroplasty for the treatment of a fracture of
a randomized clinical trial. J Bone Joint Surg [Am] 2012;94-A:577–583. the hip: the fractured hip infection trial. Bone Joint J 2016;98-B:1534–1541.
VOL. 99-B, No. 4, APRIL 2017
You might also like
- Acetabular Fractures in Older Patients: Assessment and ManagementFrom EverandAcetabular Fractures in Older Patients: Assessment and ManagementTheodore T. MansonNo ratings yet
- 2017 - Article - 459 FracturiDocument5 pages2017 - Article - 459 FracturiTinkovan IonNo ratings yet
- HIP ORTHOPEDICS October 2008Document4 pagesHIP ORTHOPEDICS October 2008kennice_nereaNo ratings yet
- Bsms 6Document6 pagesBsms 6Filip starcevicNo ratings yet
- Dislocation of Hip Hemiarthroplasty Following Posterolateral Surgical Approach: A Nested Case - Control StudyDocument6 pagesDislocation of Hip Hemiarthroplasty Following Posterolateral Surgical Approach: A Nested Case - Control StudydrusmanjamilhcmdNo ratings yet
- Medicina 59 01545 v2Document6 pagesMedicina 59 01545 v2materthaiNo ratings yet
- Nej Mo A 1906190Document10 pagesNej Mo A 1906190RobNo ratings yet
- Bot 0000000000002494Document9 pagesBot 0000000000002494Lukman Al NomaniNo ratings yet
- The Journal of Foot & Ankle SurgeryDocument8 pagesThe Journal of Foot & Ankle SurgerySergioNo ratings yet
- Elmoumni2012 Long-Term Functional Outcome Following Intramedullary Nailing ofDocument5 pagesElmoumni2012 Long-Term Functional Outcome Following Intramedullary Nailing ofJian Wei LowNo ratings yet
- ContohDocument9 pagesContohVino DoangNo ratings yet
- Jama Kuramatsu 2019 Oi 190098Document12 pagesJama Kuramatsu 2019 Oi 190098HeliHiNo ratings yet
- Comparison of Femur Intertrochanteric Fracture Fixation With Hemiarthroplasty and Proximal Femoral Nail SystemsDocument6 pagesComparison of Femur Intertrochanteric Fracture Fixation With Hemiarthroplasty and Proximal Femoral Nail SystemsBREEZE EVERARDINE SUXE TELLONo ratings yet
- Patient Outcomes Following Tricompartmental Total Knee Replacement: A Meta-AnalysisDocument3 pagesPatient Outcomes Following Tricompartmental Total Knee Replacement: A Meta-AnalysisSahithya MNo ratings yet
- Absorbable Metal Stents: Below THE KneeDocument2 pagesAbsorbable Metal Stents: Below THE KneeChavdarNo ratings yet
- Review Article: Bone Graft in Posterior Spine Fusion For Adolescent Idiopathic Scoliosis: A Meta-AnalysisDocument6 pagesReview Article: Bone Graft in Posterior Spine Fusion For Adolescent Idiopathic Scoliosis: A Meta-AnalysisDonny HendrawanNo ratings yet
- Fijcmr 650 May 31 2Document3 pagesFijcmr 650 May 31 2khusnulNo ratings yet
- 2017 Article 528Document12 pages2017 Article 528Marios GhobrialNo ratings yet
- Analysis of Risk Factors Affecting Mortality in Elderly Patients Operated On For Hip FracturesDocument6 pagesAnalysis of Risk Factors Affecting Mortality in Elderly Patients Operated On For Hip FracturesloliNo ratings yet
- The Impact of Long-Term Follow-Up On Total Hip Arthroplasty: A Systematic ReviewDocument7 pagesThe Impact of Long-Term Follow-Up On Total Hip Arthroplasty: A Systematic ReviewIJAR JOURNALNo ratings yet
- THA Polyethylene SurvivalDocument5 pagesTHA Polyethylene SurvivalCleff FlowersNo ratings yet
- 10 1111@cid 12881Document9 pages10 1111@cid 12881everaldocruzNo ratings yet
- Swart 2016Document7 pagesSwart 2016TommysNo ratings yet
- Articulo Deslizamiento Cabeza Del FemurDocument16 pagesArticulo Deslizamiento Cabeza Del FemurJose MielesNo ratings yet
- Choi 2021Document12 pagesChoi 2021paul_androideNo ratings yet
- Prospective Evaluation of Short and Mid-Term Outcomes of Total Hip Arthroplasty Using The Accolade™ StemDocument7 pagesProspective Evaluation of Short and Mid-Term Outcomes of Total Hip Arthroplasty Using The Accolade™ StemDenis AlexandruNo ratings yet
- Patient-Related Risk Factors Associated With Less Favourable Outcomes Following Hip ArthrosDocument10 pagesPatient-Related Risk Factors Associated With Less Favourable Outcomes Following Hip ArthrosAhmad PradhanaNo ratings yet
- Primary Hemiarthroplasty For Intertrochanteric Femur Fractures in Elderly Patients: Our Experience in BIRDEM General HospitalDocument6 pagesPrimary Hemiarthroplasty For Intertrochanteric Femur Fractures in Elderly Patients: Our Experience in BIRDEM General HospitalJonaed HakimNo ratings yet
- Halo-Pelvic Traction in The Treatment of Severe SCDocument9 pagesHalo-Pelvic Traction in The Treatment of Severe SCmmmhmcopdortho2020No ratings yet
- Forgotten Joint Score PDFDocument8 pagesForgotten Joint Score PDFdeepakNo ratings yet
- Conservative Treatment, Plate Fixation, or Prosthesis For Proximal Humeral Fracture. A Prospective Randomized StudyDocument3 pagesConservative Treatment, Plate Fixation, or Prosthesis For Proximal Humeral Fracture. A Prospective Randomized StudyAndi Urviana AsrahNo ratings yet
- Bmri2017 6136205Document11 pagesBmri2017 6136205Petru CarajaNo ratings yet
- Meniscus Root Repair Vs Meniscectomy orDocument8 pagesMeniscus Root Repair Vs Meniscectomy orJulio Cesar Guillen MoralesNo ratings yet
- Asensio, JA, (2020) - Tratamiento Quirúrgico de Las Lesiones de La Arteria Braquial y Predictores de Resultado.Document12 pagesAsensio, JA, (2020) - Tratamiento Quirúrgico de Las Lesiones de La Arteria Braquial y Predictores de Resultado.Edgar Geovanny Cardenas FigueroaNo ratings yet
- Articulo 8Document7 pagesArticulo 8Marcela RodriguezNo ratings yet
- How To Clear Polytrauma Patients For Fracture FixationDocument26 pagesHow To Clear Polytrauma Patients For Fracture FixationTiago FeitosaNo ratings yet
- Do Corticosteroids Reduce The Risk of Fat Embolism Syndrome in Patients With Long-Bone Fractures? A Meta-AnalysisDocument8 pagesDo Corticosteroids Reduce The Risk of Fat Embolism Syndrome in Patients With Long-Bone Fractures? A Meta-AnalysisJorge MontesinosNo ratings yet
- Supracondylar Paper 3Document8 pagesSupracondylar Paper 3Alex ThomasNo ratings yet
- Endovascular Stentgraft Placement in Aortic Dissection A MetaanalysisDocument10 pagesEndovascular Stentgraft Placement in Aortic Dissection A MetaanalysisCiubuc AndrianNo ratings yet
- Artigo LIVE Fukuda (Menisco Hohmann2018)Document10 pagesArtigo LIVE Fukuda (Menisco Hohmann2018)gabynieto.031090No ratings yet
- Long-Term Treatment Effectiveness of Molding HelmeDocument7 pagesLong-Term Treatment Effectiveness of Molding HelmeDianaNo ratings yet
- De Goede 2017Document8 pagesDe Goede 2017jorgeluisgt7No ratings yet
- What's New in Spine Surgery: Specialty UpdateDocument11 pagesWhat's New in Spine Surgery: Specialty UpdatePoliceNo ratings yet
- Ankle Distraction Arthroplasty A Survivorship RevDocument9 pagesAnkle Distraction Arthroplasty A Survivorship RevmirandaroydsNo ratings yet
- 2012 Implant-Supported Single Crowns PredictablyDocument2 pages2012 Implant-Supported Single Crowns PredictablysivakumarNo ratings yet
- 2021 - Arthroplasty Today - Total Joint Arthroplasty in AchondroplasiaDocument6 pages2021 - Arthroplasty Today - Total Joint Arthroplasty in AchondroplasiaDrSheenam BansalNo ratings yet
- Dudda Et Al. - 2011 - Authors' ReplyDocument2 pagesDudda Et Al. - 2011 - Authors' ReplyYuki SATAKENo ratings yet
- Motiei Langroudi2019Document5 pagesMotiei Langroudi2019LailNo ratings yet
- 1 s2.0 S1010518220301803 MainDocument11 pages1 s2.0 S1010518220301803 MainCaio GonçalvesNo ratings yet
- 1807 5932 Clin 71 02 110 PDFDocument4 pages1807 5932 Clin 71 02 110 PDFkinecamposNo ratings yet
- Surgical Versus Non-Surgical Treatment of Mandibular Condylar Fractures: A Meta-AnalysisDocument22 pagesSurgical Versus Non-Surgical Treatment of Mandibular Condylar Fractures: A Meta-AnalysisHNo ratings yet
- Venous Thromboembolism in Patients Discharged From The Emergency Department With Ankle FracturesDocument13 pagesVenous Thromboembolism in Patients Discharged From The Emergency Department With Ankle FracturesSebastiano Della CasaNo ratings yet
- The Oswestry Risk IndexDocument7 pagesThe Oswestry Risk IndexRamon LagoNo ratings yet
- Early Surveillance of Ceramic-On-metal Total Hip ArthroplastyDocument6 pagesEarly Surveillance of Ceramic-On-metal Total Hip ArthroplastydamonenNo ratings yet
- Conservative Treatment, Plate Fixation, or Prosthesis For Proximal Humeral Fracture. A Prospective Randomized StudyDocument7 pagesConservative Treatment, Plate Fixation, or Prosthesis For Proximal Humeral Fracture. A Prospective Randomized Studymahesh_rampalliNo ratings yet
- FIRST2020Document10 pagesFIRST2020Jeisson Daniel Barrera AlvarezNo ratings yet
- Jain 2013Document15 pagesJain 2013Mohan DesaiNo ratings yet
- 190 Disc Repositioning Does It Really WorkDocument23 pages190 Disc Repositioning Does It Really WorkAngélica Valenzuela AndrighiNo ratings yet
- Treatment of Femoral Neck Fractures in Elderly Patients Over 60 Years of Age - Which Is The Ideal Modality of Primary Joint Replacement?Document8 pagesTreatment of Femoral Neck Fractures in Elderly Patients Over 60 Years of Age - Which Is The Ideal Modality of Primary Joint Replacement?FakhriMuhamadRizaldiNo ratings yet
- Below-The-Knee Arterial Injury - The Type of Vessel May Be More Important Than The Number of Vessels InjuredDocument6 pagesBelow-The-Knee Arterial Injury - The Type of Vessel May Be More Important Than The Number of Vessels InjuredelhierofanteNo ratings yet
- Vascular - Anatomy - and - Microcirculation of Femoral HeadDocument7 pagesVascular - Anatomy - and - Microcirculation of Femoral HeadDaniel Cancino CallirgosNo ratings yet
- Lesiones Sindesmales 2Document11 pagesLesiones Sindesmales 2Daniel Cancino CallirgosNo ratings yet
- Aflojamiento Aseptico de Placa Base de Componente Glenoideo en Artroplastia Reversa de Hombro, Metanalisis 2019Document17 pagesAflojamiento Aseptico de Placa Base de Componente Glenoideo en Artroplastia Reversa de Hombro, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Lesiones SindesmalesDocument9 pagesLesiones SindesmalesDaniel Cancino CallirgosNo ratings yet
- Placa Bloqueada Volar de Radio Distal, Abordaje Mipo VS Habitual, Metanalisis 2019Document12 pagesPlaca Bloqueada Volar de Radio Distal, Abordaje Mipo VS Habitual, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- PGI OrthopedicsDocument105 pagesPGI OrthopedicsDaniel Cancino CallirgosNo ratings yet
- Reconstrucción de Lca Temprana o Tardía, Metanalissi 2019Document13 pagesReconstrucción de Lca Temprana o Tardía, Metanalissi 2019Daniel Cancino CallirgosNo ratings yet
- Resultados de La Liberación Lateral Aislada en Inestabilidad Patelofemoral, Metanalisis 2019Document8 pagesResultados de La Liberación Lateral Aislada en Inestabilidad Patelofemoral, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Seguridad y Efectividad de Aspirina y Enoxaparina Tromboprofilaxis Post Artroplastía, Metanalisis 2019Document7 pagesSeguridad y Efectividad de Aspirina y Enoxaparina Tromboprofilaxis Post Artroplastía, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Capsulotomia y Riesgo de Nav en Desplazamiento de Epifisis de Cabeza Femoral Inestable, Metanalisis 2019Document6 pagesCapsulotomia y Riesgo de Nav en Desplazamiento de Epifisis de Cabeza Femoral Inestable, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Tecnica de Cuerda VS Placa Gancho para Luxación Acromioclavicular, Metanalisis 2019Document11 pagesTecnica de Cuerda VS Placa Gancho para Luxación Acromioclavicular, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Resultados de Artroplastía en Pacientes Con Vih, Metanalisis 2019Document7 pagesResultados de Artroplastía en Pacientes Con Vih, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Tasas de Infección y Aumento de La Temperatura Ambiental, Metanalisis 2019Document7 pagesTasas de Infección y Aumento de La Temperatura Ambiental, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Ketorolaco Post Artroscopía de Rodilla, Metanalisis 2020Document7 pagesKetorolaco Post Artroscopía de Rodilla, Metanalisis 2020Daniel Cancino CallirgosNo ratings yet
- Anatomia 1 - Bnx6Document32 pagesAnatomia 1 - Bnx6Daniel Cancino CallirgosNo ratings yet
- Aspirina para Troboprofilaxis Despues de Artroplastia de Cadera y Rodilla, Metanalisis 2019Document8 pagesAspirina para Troboprofilaxis Despues de Artroplastia de Cadera y Rodilla, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Efecto de La Atb Profilaxis Local en FX Abiertas, Metanalisis 2018Document10 pagesEfecto de La Atb Profilaxis Local en FX Abiertas, Metanalisis 2018Daniel Cancino CallirgosNo ratings yet
- Imagenes para Lesiones de Manguito Rotador Metanalisis 2020Document26 pagesImagenes para Lesiones de Manguito Rotador Metanalisis 2020Daniel Cancino CallirgosNo ratings yet
- Sepsis and Septic ShockDocument18 pagesSepsis and Septic ShockMayra Alejandra Prada SerranoNo ratings yet
- PRP para Epicondilitis Lateral, Metaanalisis 2020Document11 pagesPRP para Epicondilitis Lateral, Metaanalisis 2020Daniel Cancino CallirgosNo ratings yet
- Diagnosis and Treatment of Acute Achilles Tendon.7Document8 pagesDiagnosis and Treatment of Acute Achilles Tendon.7Daniel Cancino CallirgosNo ratings yet
- Babeno VI InglesDocument10 pagesBabeno VI InglesDaniel Cancino CallirgosNo ratings yet
- Obesidad y Cancer EndometrialDocument7 pagesObesidad y Cancer EndometrialDaniel Cancino CallirgosNo ratings yet
- Trombocitopenia en El NeonatoDocument14 pagesTrombocitopenia en El NeonatoKah DrumondNo ratings yet
- Advances in The Pathogenesis and Treatment of Systemic Juvenile Idiopathic Arthritis 2014Document8 pagesAdvances in The Pathogenesis and Treatment of Systemic Juvenile Idiopathic Arthritis 2014Daniel Cancino CallirgosNo ratings yet
- Ep Docx Sca SMSC - V2Document45 pagesEp Docx Sca SMSC - V290007No ratings yet
- Credit CardDocument6 pagesCredit CardJ Boy LipayonNo ratings yet
- Nuttall Gear CatalogDocument275 pagesNuttall Gear Catalogjose huertasNo ratings yet
- DR Afwan Fajri - Trauma - Juli 2023Document82 pagesDR Afwan Fajri - Trauma - Juli 2023afwan fajriNo ratings yet
- Teambinder Product BrochureDocument7 pagesTeambinder Product BrochurePrinceNo ratings yet
- Project On Mahindra BoleroDocument35 pagesProject On Mahindra BoleroViPul75% (8)
- Programming MillDocument81 pagesProgramming MillEddy ZalieNo ratings yet
- WeldingDocument23 pagesWeldingMathan EverNo ratings yet
- Coefficient of Restitution - Center of MassDocument3 pagesCoefficient of Restitution - Center of MassMannyCesNo ratings yet
- OMM 618 Final PaperDocument14 pagesOMM 618 Final PaperTerri Mumma100% (1)
- 2012 Conference NewsfgfghsfghsfghDocument3 pages2012 Conference NewsfgfghsfghsfghabdNo ratings yet
- Editor Attach 1327138073 1832Document59 pagesEditor Attach 1327138073 1832Monther Al DebesNo ratings yet
- Early Christian ArchitectureDocument38 pagesEarly Christian ArchitectureInspirations & ArchitectureNo ratings yet
- 6 - European Cluster Partnership For Excellence - European Cluster Collaboration PlatformDocument5 pages6 - European Cluster Partnership For Excellence - European Cluster Collaboration PlatformDaniela DurducNo ratings yet
- Portfolio Final AssignmentDocument2 pagesPortfolio Final Assignmentkaz7878No ratings yet
- Ziarek - The Force of ArtDocument233 pagesZiarek - The Force of ArtVero MenaNo ratings yet
- ProjectDocument22 pagesProjectSayan MondalNo ratings yet
- Adsorption ExperimentDocument5 pagesAdsorption ExperimentNauman KhalidNo ratings yet
- Products ListDocument11 pagesProducts ListPorag AhmedNo ratings yet
- Internship Report PDFDocument71 pagesInternship Report PDFNafiz FahimNo ratings yet
- 8D & 7QC ToolsDocument117 pages8D & 7QC ToolsAshok Kumar100% (1)
- 353 Version 7thDocument1 page353 Version 7thDuc NguyenNo ratings yet
- The Chassis OC 500 LE: Technical InformationDocument12 pagesThe Chassis OC 500 LE: Technical InformationAbdelhak Ezzahrioui100% (1)
- DLL in Health 7 3rd QuarterDocument2 pagesDLL in Health 7 3rd QuarterJuna Lyn Hermida ArellonNo ratings yet
- IGCSE 0408 Unseen Poem QuestionsDocument5 pagesIGCSE 0408 Unseen Poem QuestionsMenon HariNo ratings yet
- Full Download Ebook PDF Introductory Econometrics A Modern Approach 7th Edition by Jeffrey PDFDocument42 pagesFull Download Ebook PDF Introductory Econometrics A Modern Approach 7th Edition by Jeffrey PDFtimothy.mees27497% (39)
- Voice Over Script For Pilot TestingDocument2 pagesVoice Over Script For Pilot TestingRichelle Anne Tecson ApitanNo ratings yet
- Ibragimova Lesson 4Document3 pagesIbragimova Lesson 4Dilnaz IbragimovaNo ratings yet
- Under Suitable Conditions, Butane, C: © OCR 2022. You May Photocopy ThisDocument13 pagesUnder Suitable Conditions, Butane, C: © OCR 2022. You May Photocopy ThisMahmud RahmanNo ratings yet
- BBAG MPR and STR LISTSDocument25 pagesBBAG MPR and STR LISTShimanshu ranjanNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (6)