Professional Documents
Culture Documents
Obstructive Shock Pediatric - Journal PDF
Uploaded by
Gerald SweinslionOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obstructive Shock Pediatric - Journal PDF
Uploaded by
Gerald SweinslionCopyright:
Available Formats
Send Orders of Reprints at reprints@benthamscience.
net
The Open Pediatric Medicine Journal, 2013, 7, (Suppl 1: M7) 35-37 35
Open Access
Obstructive Shock
Carrie Morgan 1 and Derek S. Wheeler*,2,3
1
Division of Critical Care Medicine, Blair E. Batson Children’s Hospital, Jackson, MS, USA
2
Division of Critical Care Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
3
Department of Pediatrics, University of Cincinnati, College of Medicine, USA
Abstract: Obstructive shock is a less common, but important cause of shock in critically ill infants and children. It is
caused by mechanical obstruction of blood flow to and/or from the heart and causes can include a tension pneumothorax,
cardiac tamponade, pulmonary embolus, or cardiac defects resulting in left-sided outflow tract obstruction. Each of these
can result in similar physiology with poor perfusion and oxygen delivery to the body, though the diagnosis and treatment
are unique to each process and thus described individually.
Keywords: Obstructive shock, pneumothorax, cardiac tamponade, pulmonary embolus, left-sided obstructive heart lesion.
INTRODUCTION placement of central venous catheters in the chest vessels.
The incidence of secondary pneumothorax in pediatric
Hinshaw and Cox developed a classification of shock
patients is not well described, however, in critically ill
based upon the different hemodynamic profiles of shock
children requiring mechanical ventilation it is reported to be
states in 1972. These categories included hypovolemic
4-15% [2, 3]. Notably, the incidence of secondary pneumothorax
shock, distributive shock, cardiogenic shock, and in mechanically ventilated pediatric patients has declined
extracardiac obstructive shock. The latter was described as
markedly since the introduction of protective lung strategies
involving obstruction to flow in the cardiovascular circuit
[4].
and characterized by impairment of diastolic filling or
excessive afterload [1]. The consequent obstruction of blood Pneumothoraces can be well tolerated in some patients,
flow into or out of the heart causes a decrease in cardiac though signs and symptoms of obstructive shock can develop
output, and hence inadequate oxygen delivery, which is if the pneumothorax is under tension. In this scenario, the air
manifest by the classic signs and symptoms of the shock in the pleural space continues to collect under a one-way or
state. Obstructive shock is rare in pediatrics, though the most ball valve effect, such that air enters during inhalation, but
common causes generally include tension pneumothorax, cannot exit during exhalation. Eventually, enough air
cardiac tamponade, and pulmonary embolism. Also included accumulates such that the intrathoracic pressure of the
in this category physiologically, and more specific to affected hemi-thorax equilibrates with atmospheric pressure,
pediatrics, are congenital heart lesions characterized by left leading to complete lung collapse or atelectasis. Air under
ventricular outflow tract obstruction, including critical aortic tension also causes a shifting of the mediastinum,
stenosis, coarctation of the aorta, interrupted aortic arch, and compression and total collapse of the lung and great vessels,
hypoplastic left heart syndrome. Herein, we will briefly thereby compromising both cardiovascular and respiratory
review the major causes of obstructive shock found in function [5]. Studies in animal models have shown that the
children. early clinical features of a tension pneumothorax include
hypoxemia, tachycardia, and respiratory distress due to
TENSION PNEUMOTHORAX compression and collapse of lung segments. As mechanical
A pneumothorax is defined as the accumulation of air in compromise of venous structures develops, there is a drastic
the pleural space, a cavity that is normally filled with a small and profound reduction in venous return to the heart as well,
amount of pleural fluid. It can be spontaneous (more clinically manifested by symptoms of shock and poor
common in adolescent males) or secondary to underlying perfusion. Thus, overt hypotension may be a late sign.
lung pathology, such as trauma (both penetrating and blunt Complete occlusive mechanical compression is suggested by
trauma), asthma, cystic fibrosis, and pneumonia [2]. Also equalization of the Mean Intrathoracic Pressure (MIP) and
included in this subcategory are iatrogenic causes such as Central Venous Pressure (CVP), which is a very late event
barotrauma during positive pressure ventilation or during and results in cardiovascular collapse [6]. Treatment of a
tension pneumothorax requires emergent needle
decompression, usually performed by placing a sterile needle
*Address correspondence to this author at the Division of Critical Care in the second intercostal space along the midclavicular line.
Medicine, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Definitive treatment requires thoracostomy tube placement
Avenue, Cincinnati, OH 45229-3039, USA; Tel: (513) 636-4259; [3, 5].
Fax: (513) 636-4267; E-mail: Derek.wheeler@cchmc.org
1874-3099/13 2013 Bentham Open
36 The Open Pediatric Medicine Journal, 2013, Volume 7 Morgan and Wheeler
CARDIAC TAMPONADE resuscitation may worsen tamponade physiology, especially
in children who are either normovolemic or hypervolemic
The pericardial sac around the heart is relatively non-
[10]. In the latter scenario, fluid administration will increase
compliant, and the accumulation of even small amounts of
intracardiac pressures further, hence increasing
fluid can be sufficient to produce cardiac tamponade
intrapericardial pressures and worsening tamponade [12].
physiology. While acute pericardial fluid changes are usually
symptomatic, the chronic accumulation of fluid may occur PULMONARY EMBOLISM
with little to no hemodynamic derangements, as the
Pulmonary embolism (PE) is uncommonly diagnosed in
pericardium slowly stretches to accommodate the excess
children, making its true incidence difficult to determine.
volume over time [7]. Pericardial effusions can develop as a
However, the incidence of PE does appear to be on the rise,
result of any type of pericardial inflammation (i.e.,
though this may be due to a heightened index of clinical
pericarditis), causing a range of physiologic perturbations
along the spectrum of minor flu-like symptoms (i.e., suspicion and better recognition by pediatric providers.
Alternatively, it may be due to the fact that more children are
manifestations of the pericarditis itself) to a life-threatening
surviving from previously fatal conditions that place them at
state characterized by cardiac tamponade and obstructive
an increased risk for developing PE, such as congenital heart
shock [7]. Historically, the most common cause of
disease and malignancy. In addition, more children are
pericardial effusions was infectious pericarditis, though a
requiring central venous catheterization for vascular access,
recent review suggests that idiopathic and neoplastic causes
are much more frequent due to the success of childhood a major risk factor for venous thromboembolism (VTE),
which can lead to a PE [13, 14].
vaccinations [8]. Other common causes include
postpericardiotomy syndrome (following cardiac surgery for PE is frequently fatal and difficult to diagnose. In a
congenital heart disease) and trauma, most often causing recent literature review comparing pediatric PE with adult
hemopericardium. Effusions may also develop as a result of PE, pediatric cases were more often diagnosed at autopsy
a central line that erodes through the thin wall of the right and were associated with a higher mortality rate than adults
atrium, a phenomenon that appears primarily limited to [13]. The clinical presentation often is confusing, perhaps
neonates and young infants [9]. compounded by the fact that very few pediatricians have
much experience with this disorder. Results of screening
The pathophysiology of cardiac tamponade is well-
tests, such as oxygen saturation, electrocardiography, and
described. Briefly, increased intrapericardial pressure limits
chest radiography, may be normal. Thus, a high index of
venous return to the heart and causes right ventricular
compression. There is a progressive decline in right clinical suspicion is necessary. Evaluation should be
performed with spiral computed tomography (CT)
ventricular end-diastolic volume as diastolic filling lessens,
venography, which is now widely considered the study of
worsening cardiac output. In severe tamponade, venous
choice due to its >90% sensitivity and specificity in adults.
return during inspiration into the compressed right ventricle
Ventilation/ Perfusion (V/Q) scans are also available but are
bows the interventricular septum into the left ventricle,
more difficult to obtain and to interpret in pediatrics [15].
further diminishing systemic cardiac output. As pericardial
pressure increases and surpasses ventricular end-diastolic As a cause of cardiogenic shock, a massive PE has a
pressure, the ventricular volumes grow smaller and smaller profound impact upon gas exchange and hemodynamics.
and cardiac output worsens [10]. Obstruction to flow through the pulmonary artery results in
increased dead space ventilation where affected lung
Tamponade is a clinical diagnosis and classically,
segments are ventilated but not perfused, observed clinically
patients with critical cardiac tamponade present with Beck’s
triad of symptoms including hypotension, quiet (“muffled”) as a substantial decrease in the end-tidal CO2 (ETCO2) that
no longer reflects arterial PCO2. A widened alveolar-arterial
heart sounds, and raised jugular venous pressure [7, 10, 11].
gradient (A-a) is present as well. The mechanism for
Patients may present with dyspnea, compensatory
hypoxemia likely involves several mechanisms. In some
tachycardia, and poor perfusion. On auscultation, a friction
pediatric patients, an intracardiac right-to-left shunt through
rub and distant heart sounds may be present. Pulsus
a patent foramen ovale may be present and as right atrial
paradoxus, defined as a decline in systolic blood pressure
greater than or equal to 10 mm Hg during inspiration, results pressure increases and eventually exceeds the left atrial
pressure, deoxygenated blood can shunt directly into the
from the inspiratory reduction in pleural pressure that
systemic circulation. In addition, V/Q mismatching is
produces a fall in left ventricular output and arterial systolic
compounded by the accompanying fall in cardiac output that
pressure [5, 7, 12]. An electrocardiogram may show
results from massive PE, leading to mixed venous
electrical alternans due to the heart swinging within the large
desaturation. PE increases the right ventricular (RV)
effusion. Formal evaluation with an urgent echocardiogram
should be performed in those patients with symptoms afterload, resulting in an increase in the RV end-diastolic
volume (EDV). The increase in RVEDV adversely affects
suspicious for cardiac tamponade. However, emergent
left ventricular hemodynamics through ventricular
management should not wait for echocardiography and is
interdependence. Specifically, the interventricular septum
frequently based upon the recognition of tamponade
bows into the left ventricle (LV) and impairs diastolic filling,
physiology in the appropriate clinical context.
resulting in decreased LV preload and subsequently
Pericardiocentesis is the lifesaving procedure of choice diminished cardiac output and hypotension [5, 16, 17]. These
for children with cardiac tamponade and can safely be done physiologic phenomenon are manifested by respiratory
with bedside echocardiographic guidance [11]. Medical distress, hypoxia, and decreased cardiac output with signs of
stabilization with fluid resuscitation and inotropic support is shock.
temporary at best and somewhat controversial as fluid
Obstructive Shock The Open Pediatric Medicine Journal, 2013, Volume 7 37
Treatment of an acute pulmonary embolus in children mechanisms of shock. In: Lerner B, Hinshaw, Barbara GC, Eds.
should begin with initiation of a heparin infusion with or Proceedings of a symposium held in Oklahoma City; 1971 October
1-2, New York: Plenum Press 1972.
without fibrinolytic agents such as tPA, depending on the [2] Yarmus L, Feller-Kopman D. Pneumothorax in the critically ill
child and the extent of the clot. In the resolution period, the patient. Chest 2012; 141: 1098-105.
child will then warrant at least 3-6 months of anticoagulation [3] Johnson NN, Toledo A, Endom EE. Pneumothorax,
with low molecular weight heparin (LMWH) or warfarin [5]. pneumomediastinum, and pulmonary embolism. Pediatr Clin North
Am 2010; 57: 1357-83.
More detailed antithrombotic therapy instruction for [4] Miller MP, Sagy M. Pressure characteristics of mechanical
pediatric and neonatal patients can be found in the clinical ventilation and incidence of pneumothorax before and after the
practice guidelines for anti-thrombotic therapy published in implementation of protective lung strategies in the management of
2008 [18]. pediatric patients with severe ARDS. Chest 2008; 134: 969-73.
[5] Wheeler DS, Wong HR, Shanley TP. Pediatric critical care
LEFT-SIDED CARDIAC OBSTRUCTION medicine : Basic science and clinical evidence. London: Springer
2007.
Obstructive shock may also present in specific cardiac [6] Barton ED, Rhee P, Hutton KC, Rosen P. The pathophysiology of
lesions that have ductal-dependent systemic blood flow. tension pneumothorax in ventilated swine. J Emerg Med 1997; 15:
There are several left-sided heart lesions that are dependent 147-53.
[7] Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet 2004;
upon ductal blood flow through a patent ductus arteriosus 363: 717-27.
(PDA) to maintain systemic circulation, these include [8] Kuhn B, Peters J, Marx GR, Breitbart RE. Etiology, management,
coarctation of the aorta, critical aortic valve stenosis, and outcome of pediatric pericardial effusions. Pediatr Cardiol
interrupted aortic arch, and hypoplastic left heart syndrome. 2008; 29: 90-4.
[9] Weil BR, Ladd AP, Yoder K. Pericardial effusion and cardiac
As the PDA closes after birth, systemic blood flow decreases tamponade associated with central venous catheters in children: an
and the pulmonary system receives more and more blood uncommon but serious and treatable condition. J Pediatr Surg 2010;
flow. This results in the development of heart failure with 45: 1687-92.
respiratory distress due to pulmonary edema, impaired [10] Knudson JD. Diseases of the pericardium. Congenit Heart Dis
systemic perfusion with acidosis, and eventually circulatory 2011; 6: 504-13.
[11] Azam S, Hoit BD. Treatment of pericardial disease. Cardiovasc
collapse. These anatomic defects require prompt recognition Ther 2011; 29: 308-14.
in the neonatal period, if not prenatally diagnosed, and the [12] Keane JF, Lock JE, Fyler DC, Nadas AS. Nadas' pediatric
treatment depends on circulatory and respiratory support cardiology. 2nd ed. Philadelphia: Saunders Elsevier 2006.
including mechanical ventilation and inotropic support of the [13] Baird JS, Killinger JS, Kalkbrenner KJ, Bye MR, Schleien CL.
Massive pulmonary embolism in children. J Pediatr 2010; 156:
fluid-overloaded right ventricle, as well as securing ductal 148-51.
patency with prostaglandin E2 infusion. Definitive treatment [14] Victoria T, Mong A, Altes T, et al. Evaluation of pulmonary
is later achieved through surgical palliation, discussions of embolism in a pediatric population with high clinical suspicion.
which are outside of the scope of this article [5, 12, 19]. Pediatr Radiol 2009; 39: 35-41.
[15] McCrory MC, Brady KM, Takemoto C, Tobias JD, Easley RB.
CONFLICT OF INTEREST Thrombotic disease in critically ill children. Pediatr Crit Care Med
2011; 12: 80-9.
The authors confirm that this article content has no [16] Tapson VF. Acute pulmonary embolism. Cardiol Clin 2004; 22:
conflict of interest. 353-65, v.
[17] Patocka C, Nemeth J. Pulmonary embolism in pediatrics. J Emerg
ACKNOWLEDGEMENTS Med 2012, 42: 105-16.
[18] Monagle P, Chalmers E, Chan A, et al. American College of Chest
Declared none. P. Antithrombotic therapy in neonates and children: American
College of Chest Physicians Evidence-Based Clinical Practice
REFERENCES Guidelines 8th Ed. Chest 2008; 133(6 Suppl): 887S-968S.
[19] Barron DJ, Kilby MD, Davies B, Wright JG, Jones TJ, Brawn WJ.
[1] Cox BG, Hinshaw LB, United States Navy Project THEMIS.
Hypoplastic left heart syndrome. Lancet 2009; 374: 551-64.
University of Oklahoma. Health Sciences Center. The Fundamental
Received: December 17, 2012 Revised: December 21, 2012 Accepted: January 2, 2013
© Morgan and Wheeler; Licensee Bentham Open.
This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-
nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
You might also like
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtFrom EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtRating: 5 out of 5 stars5/5 (1)
- 14 Test Bank Cardiovascular Physiology MCQ Test Bank With AnswersDocument45 pages14 Test Bank Cardiovascular Physiology MCQ Test Bank With Answersmugtaba100% (4)
- MTY 1211 Chapter 1 Overview Clinical Lab HematologyDocument68 pagesMTY 1211 Chapter 1 Overview Clinical Lab Hematologychris andrieNo ratings yet
- Urinary SystemDocument5 pagesUrinary SystemJushelle Anne Tigoy Pilare100% (1)
- ATLS Practice Test 2 Answers & ExplanationsDocument8 pagesATLS Practice Test 2 Answers & ExplanationsCarl Sars50% (2)
- Robbins - 12 The HeartDocument5 pagesRobbins - 12 The HeartCM NajitoNo ratings yet
- Science Quest 8 AC 3E c04 PDFDocument94 pagesScience Quest 8 AC 3E c04 PDFmaxx100% (1)
- Cardiac TamponadeDocument18 pagesCardiac Tamponadeyelsinosmin romeroalvaradoNo ratings yet
- Recovery in TrainingDocument7 pagesRecovery in TrainingAnonymous 92hWDcNo ratings yet
- Newborn Resuscitation (Newborn CPR) BSN 12C: Madeline N. Gerzon, RN, MM Clinical Instructor Davao Doctors CollegeDocument59 pagesNewborn Resuscitation (Newborn CPR) BSN 12C: Madeline N. Gerzon, RN, MM Clinical Instructor Davao Doctors CollegemgerzonNo ratings yet
- NCM 112 Midterm ExamDocument16 pagesNCM 112 Midterm ExamYman Gio BumanglagNo ratings yet
- Mechanical VentilationDocument16 pagesMechanical VentilationBhawna JoshiNo ratings yet
- NCP CopdDocument6 pagesNCP Copdjoelette100% (1)
- Persistent Pulmonary Hypertension of The NewbornDocument4 pagesPersistent Pulmonary Hypertension of The NewbornMarwa Adly100% (1)
- BLS CPR GuideDocument27 pagesBLS CPR GuideMoh PurnomoNo ratings yet
- Acute Respiratory Distress Syndrome - Background, Pathophysiology, EtiologyDocument5 pagesAcute Respiratory Distress Syndrome - Background, Pathophysiology, EtiologyARHNo ratings yet
- 2013 CLSIFDA Table UpdateDocument5 pages2013 CLSIFDA Table UpdateGerald SweinslionNo ratings yet
- Paediatric Respiratory Reviews: F. Healy, B.D. Hanna, R. ZinmanDocument6 pagesPaediatric Respiratory Reviews: F. Healy, B.D. Hanna, R. ZinmanfadmayulianiNo ratings yet
- Tension Pneumothorax - StatPearls - NCBI BookshelfDocument9 pagesTension Pneumothorax - StatPearls - NCBI Bookshelfshinta damayantiNo ratings yet
- Go To:: Respiratory ImpairmentDocument18 pagesGo To:: Respiratory ImpairmentNanik LestariNo ratings yet
- TBL Enfermedades de La Pleura - Lectura 2Document13 pagesTBL Enfermedades de La Pleura - Lectura 2Jose LunaNo ratings yet
- handa2018Document18 pageshanda2018rocio enriquezNo ratings yet
- 28 Infective EndocarditisDocument10 pages28 Infective EndocarditisVictor PazNo ratings yet
- Stenosis Pulmonal.Document21 pagesStenosis Pulmonal.syelNo ratings yet
- Obstructive Shock, From Diagnosis To TreatmentDocument10 pagesObstructive Shock, From Diagnosis To TreatmentJonathan PuenteNo ratings yet
- Acute Pulmonary Edema - NEJMDocument4 pagesAcute Pulmonary Edema - NEJMSuzika Dewi0% (1)
- Neurogenic Pulmonary Edema - StatPearls - NCBI BookshelfDocument1 pageNeurogenic Pulmonary Edema - StatPearls - NCBI Bookshelfkud4l14rNo ratings yet
- Pulmonary Edema - StatPearls - NCBI BookshelfDocument7 pagesPulmonary Edema - StatPearls - NCBI BookshelfriyanasirNo ratings yet
- Pneumothorax, Tension and TraumaticDocument29 pagesPneumothorax, Tension and TraumaticicaNo ratings yet
- Neonatal Pericardial Effusion: Case Report and Review of The LiteratureDocument9 pagesNeonatal Pericardial Effusion: Case Report and Review of The LiteratureMarsya Yulinesia LoppiesNo ratings yet
- Emergency Department Guide to Diagnosing and Treating Pleural DiseaseDocument25 pagesEmergency Department Guide to Diagnosing and Treating Pleural DiseaseEdgardo Vargas AlvarezNo ratings yet
- Pleural Effusion in Adults—Etiology, Diagnosis, and Treatment (24.05.2019)Document10 pagesPleural Effusion in Adults—Etiology, Diagnosis, and Treatment (24.05.2019)lordiroh1No ratings yet
- PneumothotaxDocument32 pagesPneumothotaxAvishay ZoarNo ratings yet
- Cor Pulmonale An Overview 2003Document12 pagesCor Pulmonale An Overview 2003Ade Cahyo IslamiNo ratings yet
- Diagnosis and Management of Traumatic PneumothoraxDocument8 pagesDiagnosis and Management of Traumatic PneumothoraxsimcassNo ratings yet
- Acute Pulmonary EmbolismDocument13 pagesAcute Pulmonary EmbolismIrina SumeicoNo ratings yet
- (Cardiology Clinics) Ori Ben-Yehuda, Michael H. Crawford - Pulmonary Vascular Disease-Saunders (2004)Document145 pages(Cardiology Clinics) Ori Ben-Yehuda, Michael H. Crawford - Pulmonary Vascular Disease-Saunders (2004)LucasPeresBetNo ratings yet
- Pulmonary Embolism (PE) - Pulmonary Disorders - MSD Manual Professional EditionDocument25 pagesPulmonary Embolism (PE) - Pulmonary Disorders - MSD Manual Professional Editionpeterpavel112No ratings yet
- Neurogenic Pulmonary EdemaDocument7 pagesNeurogenic Pulmonary EdemajuanNo ratings yet
- Young Man With Cardiac Arrest Secondary To Undiagnosed Mediastinal MassDocument4 pagesYoung Man With Cardiac Arrest Secondary To Undiagnosed Mediastinal MassPxPPxH ChanNo ratings yet
- Dyspnoea: Pathophysiology and A Clinical Approach: ArticleDocument5 pagesDyspnoea: Pathophysiology and A Clinical Approach: ArticleadninhanafiNo ratings yet
- Chest 2002 TEP Excelente PDFDocument31 pagesChest 2002 TEP Excelente PDFEdwin AlvarezNo ratings yet
- Tetzlaff 2003Document9 pagesTetzlaff 2003Lên DươngNo ratings yet
- IJMR - Volume 3 - Issue 1 - Pages 365-370Document6 pagesIJMR - Volume 3 - Issue 1 - Pages 365-370AzaliRiccoNo ratings yet
- Management of Primary Spontaneous PneumothoraxDocument6 pagesManagement of Primary Spontaneous PneumothoraxPendragon ArthurNo ratings yet
- Congestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications For Respiratory CareDocument10 pagesCongestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications For Respiratory CareMirachel AugustNo ratings yet
- Non-Cardiogenic Pulmonary EdemaDocument7 pagesNon-Cardiogenic Pulmonary EdemadarmariantoNo ratings yet
- ABIGAIL 2010_Diffuse Alveolar HemorrhageDocument10 pagesABIGAIL 2010_Diffuse Alveolar HemorrhageRafael JustinoNo ratings yet
- CASE REPORT ON LANDAU KLEFFNER SYNDROMEDocument49 pagesCASE REPORT ON LANDAU KLEFFNER SYNDROMEMageswari SelvarajooNo ratings yet
- Sclerodactyly, and Telangiectasis) Syndrome Accompany-: Cor PulmonaleDocument2 pagesSclerodactyly, and Telangiectasis) Syndrome Accompany-: Cor PulmonaledivinaNo ratings yet
- PericarditisDocument11 pagesPericarditisrbarcellonaNo ratings yet
- Hall 2013Document6 pagesHall 2013Julio Orallo MartínezNo ratings yet
- Clinical Presentation and Diagnosis of PneumothoraxDocument49 pagesClinical Presentation and Diagnosis of PneumothoraxisahNo ratings yet
- HemodinmiaDocument8 pagesHemodinmiaPepin SalasNo ratings yet
- SaludDocument16 pagesSaluddianamera84No ratings yet
- Iadt 11 I 1 P 10Document2 pagesIadt 11 I 1 P 10anmolmani20003190No ratings yet
- 31990-PB3-7415-R3Document7 pages31990-PB3-7415-R3Rolando Miranda PeñaNo ratings yet
- PericarditisDocument11 pagesPericarditisjosefamdNo ratings yet
- Saddle Embolism in The Pulmonary Artery BifurcationDocument3 pagesSaddle Embolism in The Pulmonary Artery BifurcationAtiquzzaman RinkuNo ratings yet
- Bronchiolitis Obliterans PDFDocument7 pagesBronchiolitis Obliterans PDFSatnam KaurNo ratings yet
- Vascular Air Embolism: Symposium: Embolism in The Intensive Care UnitDocument5 pagesVascular Air Embolism: Symposium: Embolism in The Intensive Care UnitAdsoni IndoNo ratings yet
- Pulmonary Edema II: Noncardiogenic Pulmonary EdemaDocument31 pagesPulmonary Edema II: Noncardiogenic Pulmonary EdemaGita Helvia SariNo ratings yet
- Bullae, PneumothraxDocument20 pagesBullae, PneumothraxJim Albert PerlasNo ratings yet
- Pneumothorax Review: Causes, Diagnosis and ManagementDocument5 pagesPneumothorax Review: Causes, Diagnosis and ManagementAby SuryaNo ratings yet
- Modern Management of Cardiogenic Pulmonary Edema: Amal Mattu, MD, Joseph P. Martinez, MD, Brian S. Kelly, MDDocument21 pagesModern Management of Cardiogenic Pulmonary Edema: Amal Mattu, MD, Joseph P. Martinez, MD, Brian S. Kelly, MDJoni MokodoNo ratings yet
- Overview of Acute Pulmonary Embolism in AdultsDocument33 pagesOverview of Acute Pulmonary Embolism in AdultsEyla Breceda Garc�aNo ratings yet
- Pi Is 0140673696980010Document4 pagesPi Is 0140673696980010JoeNo ratings yet
- 403 Full PDFDocument10 pages403 Full PDFKuroto YoshikiNo ratings yet
- Principles of Diagnosis and Management of Traumatic PneumothoraxDocument14 pagesPrinciples of Diagnosis and Management of Traumatic PneumothoraxEkaNo ratings yet
- Causes, Effects and Treatment of Submersion InjuriesDocument9 pagesCauses, Effects and Treatment of Submersion InjuriesJ-two PallayaNo ratings yet
- Edema Pulmonar AgudaDocument4 pagesEdema Pulmonar AgudaAna Belén Artero CastañoNo ratings yet
- Superior Mediastinal Syndrome: Emergency Management: Symposium On Pgimer Management Protocols On Oncological EmergenciesDocument5 pagesSuperior Mediastinal Syndrome: Emergency Management: Symposium On Pgimer Management Protocols On Oncological EmergenciesakshayajainaNo ratings yet
- Pathophysiology: Pulmonary Embolus Hypoalbuminemia CirrhosisDocument42 pagesPathophysiology: Pulmonary Embolus Hypoalbuminemia CirrhosisLala Aya-ayNo ratings yet
- Management of Medical Records: Facts and Figures For SurgeonsDocument4 pagesManagement of Medical Records: Facts and Figures For SurgeonsGerald SweinslionNo ratings yet
- ptj4004277 PDFDocument7 pagesptj4004277 PDFChristian AriNo ratings yet
- Mayoclinproc 86 2 013 PDFDocument12 pagesMayoclinproc 86 2 013 PDFMagdy Ali ELsherbenyNo ratings yet
- Pediatric ShockDocument19 pagesPediatric ShockdarlingcarvajalduqueNo ratings yet
- Shock Pediatric in Review Yager Noviski - JournalDocument11 pagesShock Pediatric in Review Yager Noviski - JournalGerald SweinslionNo ratings yet
- Early Recognition and Management of Septic Shock in Children - JournalDocument4 pagesEarly Recognition and Management of Septic Shock in Children - JournalGerald SweinslionNo ratings yet
- Shock Pediatric in Review Yager Noviski - JournalDocument11 pagesShock Pediatric in Review Yager Noviski - JournalGerald SweinslionNo ratings yet
- Pediatric ShockDocument19 pagesPediatric ShockdarlingcarvajalduqueNo ratings yet
- The Hazard of Sharp Force Injuries Factors Influencing OutcomeDocument7 pagesThe Hazard of Sharp Force Injuries Factors Influencing OutcomeGerald SweinslionNo ratings yet
- Sepsis en PediatriaDocument8 pagesSepsis en PediatriaJorge Eduardo Espinoza RiosNo ratings yet
- Early Recognition and Management of Septic Shock in Children - JournalDocument4 pagesEarly Recognition and Management of Septic Shock in Children - JournalGerald SweinslionNo ratings yet
- Septic ShockDocument26 pagesSeptic ShockIma SoniaNo ratings yet
- Alma Saudi 2016Document28 pagesAlma Saudi 2016Gerald SweinslionNo ratings yet
- IgG IgM Pengertian Dari NigeriaDocument9 pagesIgG IgM Pengertian Dari NigeriaGerald SweinslionNo ratings yet
- Quiz #3 - ELS Human Body SystemsDocument3 pagesQuiz #3 - ELS Human Body SystemsVannie MonderoNo ratings yet
- Pharm NotesDocument113 pagesPharm NotesBibek SutradharNo ratings yet
- 2 CTN MSDocument7 pages2 CTN MSAngelie PantajoNo ratings yet
- Oral Surgery Oral Medicine Oral PathologyDocument7 pagesOral Surgery Oral Medicine Oral PathologyDiego LemurNo ratings yet
- Fernalia, Devi Listiana, Harti Monica STIKES Tri Mandiri Sakti, BengkuluDocument10 pagesFernalia, Devi Listiana, Harti Monica STIKES Tri Mandiri Sakti, BengkuluSyafi udinNo ratings yet
- Arianna Mabunga Bsn-3BDocument7 pagesArianna Mabunga Bsn-3BArianna Jasmine MabungaNo ratings yet
- ManitolDocument20 pagesManitolkr PadmanabhanNo ratings yet
- n512 Care Plan 1 3 2Document13 pagesn512 Care Plan 1 3 2api-316574434No ratings yet
- Anaerobic RespirationDocument4 pagesAnaerobic RespirationJackDaviesNo ratings yet
- Nursing Care of ThoracentesisDocument15 pagesNursing Care of ThoracentesisNora AlnaimNo ratings yet
- 2016 - Submaximal Exercise Intensity Modulates Acute Post-Exercise Heart Rate VariabilityDocument10 pages2016 - Submaximal Exercise Intensity Modulates Acute Post-Exercise Heart Rate VariabilityVeronica JanethNo ratings yet
- Cardiac DefibrillatorsDocument8 pagesCardiac Defibrillatorsصفا طلال نايفNo ratings yet
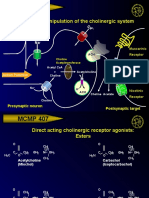
- MCMP 407: Pharmacologic Manipulation of The Cholinergic SystemDocument13 pagesMCMP 407: Pharmacologic Manipulation of The Cholinergic System16_dev5038No ratings yet
- Pathophysiology of Atrial Septal DefectDocument2 pagesPathophysiology of Atrial Septal Defectbobtaguba50% (2)
- Overview - HUMAN BLOOD CIRCULATION AND PATHWAYSDocument2 pagesOverview - HUMAN BLOOD CIRCULATION AND PATHWAYSDj22 JakeNo ratings yet
- Journal Bedah Thorax 2Document15 pagesJournal Bedah Thorax 2Novia LarasatiNo ratings yet
- Hematology: Mohamad H Qari, MD, FRCPADocument49 pagesHematology: Mohamad H Qari, MD, FRCPASantoz ArieNo ratings yet
- Animaltissues 180604115637Document40 pagesAnimaltissues 180604115637proud.student2023No ratings yet