Professional Documents
Culture Documents
Braun Colloquium Poster
Uploaded by
api-414657737Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Braun Colloquium Poster
Uploaded by
api-414657737Copyright:
Available Formats
Subacute Management Following a Basal Ganglia Hemorrhage Using PNF and Lower Extremity
Strengthening in Combination with Best Physical Therapy Practices
Jocelyn Braun
Advisor: Karen E.H. Grossnickle
Doctoral Program in Physical Therapy, Central Michigan University
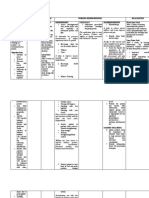
Background & Purpose Timeline for Episode of Care Outcomes
- Strokes affect 795,000 people each year in United States - Met the minimal detectable change of the FIST and the
- Hemorrhagic stroke occurs when there is a bursting of a PASS from the time of reexamination to the last day of
blood vessel in the brain treatment
- Basal ganglia is a common location for hemorrhagic - Improvements in functional mobility
strokes with resulting impairments in movement disorders - Less cuing needed and patient demonstrated better motor
due to the basal ganglia’s role in movement planning
- Disorders are commonly unilateral and will occur on - Improved postural control during transfers and less tactile
contralateral side of body to where damage was sustained and verbal cuing needed
- Physical therapy management commonly includes gait - Completed transfers from bed to and from wheelchair
training, transfer training, bed mobility training without use of assistive device
- Proprioceptive Neuromuscular Facilitation (PNF) and - Gait showed greatest improvements during duration of
lower extremity strengthening exercises have been shown treatment
to be beneficial for patients following a stroke - Able to walk longer distances with only minimum
- Purpose: To determine if PNF and lower extremity assistance for postural control and right step length with
strengthening exercises are beneficial in improving use of platform walker
functional mobility, including transfers and ambulation, - Increased gait speed and quality with no cuing
when used with best physical therapy practices - Able to make turns during ambulation trials
Results - Able to walk short distances with patient taking a right
Case Description step on his own after given tactile and verbal cuing
Test or Measure Initial Examination Reexamination End of Interventions
- 45-year-old male who sustained a basal ganglia
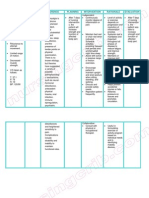
Discussion
hemorrhagic stroke
- Lived independently with no functional limitations prior to Sit to/from Standa Maximum Assist x2 Minimum Assist Minimum Assist - Frequency of lower extremity and PNF exercises may have
stroke
- Referred to subacute rehab due to inability to complete
Therapists played a role in outcomes
transfers or ambulate without assistance - Doing exercises 3 times per week for 30 minutes at each
Supine to/from Sita Maximum Assist x2 Minimum Assist Minimum Assist trial is beneficial in improving mobility
- Stroke had resulted in right-sided hemiparesis, global
aphasia, and dysphagia Therapists - Exercises need to have sufficient frequency, intensity,
- Initial examination and reexamination findings can be and duration
found in the table under “Results” Transfer Bed to/from Maximum Assist x2 Minimum Assist with Stand Pivot Transfer - PNF exercises were only done during 5 sessions
- Outcome Measures: Function in Sitting Test (FIST) and Wheelchair Therapists use of Slideboard with Minimum Assist - Frequency and intensity of gait and transfer training could
Postural Assessment Scale for Stroke (PASS) have also been increased
Ambulation a Unable to Attempt 8 feet in parallel bars 40 feet with TRAMb - Use gait training devices, such as the TRAM, more
frequently
Interventions with use of left arm for with patient able to take - Body weight supported over ground training and body
support and minimum right step on his own weight supported treadmill training has been found to
⁻ Gait training using parallel bars, platform walker, hemi- assistance for trunk with cuing, 70 feet with improve gait outcomes
walker, and TRAM. Cuing and assistance for trunk support - Attitude and motivation may have played a role in
and for right swing phase. Increased distances and control and moderate to platform walker and outcomes as this was a common limitation in the amount of
decreased amount of support given. Added turns. maximum assistance for minimum assistance for practice that was able to be done
⁻ Transfer and bed mobility training with and without - Depression and anxiety are common diagnoses after
assistive device, caregiver education to nursing staff
right step right step and minimum stroke and have been associated with less desirable
⁻ PNF: rhythmic initiation and alternating isotonics for the assist for trunk control outcomes
right lower extremity in and out of flexion and extension, - Patient showed signs and symptoms of these diagnoses
Function in Sitting Test 29/56 45/56 54/56 - Encouragement, imagery, and targets were useful strategies
moderate resistance given, pelvic anterior elevation and
posterior depression that were used during gait training
⁻ Lower extremity strengthening: mini squats, step-ups with - Appropriate discharge locations for patients following acute
the right leg onto varying surfaces, hip abduction and
Postural Assessment 8/36 23/36 27/36 care stay
adduction with manual resistance Scale for Stroke - Patient was appropriate for subacute rehabilitation
⁻ Neuromuscular Re-education: single leg stance on right aFIM
- Factors to consider for discharge from acute care:
leg, reaching in midline and outside base of support in = Functional Independence Measure: Levels of Assistance: dependent= patient performs <25% of effort, maximum assistance= patient performs patient’s abilities and tolerance for therapy, patient’s
25-50% of effort, moderate assistance= patient performs 50-75% of effort, minimal assistance= patient performs 75% or more of effort, supervision or wants and needs, support patient has available
varying directions, static standing with no support, weight
standby assistance= cueing required or setting up items for use, independent= patient performs 100% of effort safely and without cueing
shifting b TRAM, Community Products, LLC, Rifton, NY
POSTER TEMPLATE BY:
www.PosterPresentations.com
You might also like
- Brain Breakthrough: The Art of Neurological Rehabilitation: Easy and Innovative Techniques, #1From EverandBrain Breakthrough: The Art of Neurological Rehabilitation: Easy and Innovative Techniques, #1No ratings yet
- Regis Overy AAOMPT Poster 2008Document1 pageRegis Overy AAOMPT Poster 2008smokey73100% (2)
- Effect of Trunk Muscles Stabilization Exercises and General Exercises On Disability in Recurrent Non Specific Low Back AcheDocument9 pagesEffect of Trunk Muscles Stabilization Exercises and General Exercises On Disability in Recurrent Non Specific Low Back AcheDr. Krishna N. SharmaNo ratings yet
- NCP ImmobilityDocument1 pageNCP ImmobilityBcoi QuilacioNo ratings yet
- Rabanal, Lovely Jane A. Bsn-Ii Benner MCN Final Exam Case 2Document3 pagesRabanal, Lovely Jane A. Bsn-Ii Benner MCN Final Exam Case 2mark OrpillaNo ratings yet
- Arya 2017Document19 pagesArya 2017Sherly NazviNo ratings yet
- Cirugia Multinivel en PciDocument14 pagesCirugia Multinivel en Pcianateresalopez271No ratings yet
- Management of Patellofemoral Pain Targeting Hip, Pelvis, and Trunk Muscle Function: 2 Case ReportsDocument14 pagesManagement of Patellofemoral Pain Targeting Hip, Pelvis, and Trunk Muscle Function: 2 Case ReportsItai IzhakNo ratings yet
- PT Guidelines Ankle Fracture With ORIF FinalDocument3 pagesPT Guidelines Ankle Fracture With ORIF FinalShinta ParamithaNo ratings yet
- Geria NCP, Dela CruzDocument7 pagesGeria NCP, Dela CruzStephany Dela CruzNo ratings yet
- Effect of Core Stabilization Training On Endurance of Trunk Extensor and Functional Capacity in Subjects With Mechanical Low Back PainDocument8 pagesEffect of Core Stabilization Training On Endurance of Trunk Extensor and Functional Capacity in Subjects With Mechanical Low Back PainDr. Krishna N. SharmaNo ratings yet
- Effects of Adding A Neurodynamic Mobilization To.5Document9 pagesEffects of Adding A Neurodynamic Mobilization To.5Ana SoaresNo ratings yet
- The Proprioceptive Lumbar Spine and The Role of Manual Therapy NLDocument41 pagesThe Proprioceptive Lumbar Spine and The Role of Manual Therapy NLVizaNo ratings yet
- FGFKSJHGFKHSFGKJHSDGLDocument11 pagesFGFKSJHGFKHSFGKJHSDGLyannajsdhfjskdhfjkshjfhNo ratings yet
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDocument2 pagesNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDeanne Carla DalilisNo ratings yet
- Damiano 2013 Muscle Plasticity and Ankle ControlDocument8 pagesDamiano 2013 Muscle Plasticity and Ankle ControlAmr Mohamed GalalNo ratings yet
- Aplicación de Ejercicios Basados en Pilates en El Tratamiento Del Dolor Lumbar CrónicoDocument5 pagesAplicación de Ejercicios Basados en Pilates en El Tratamiento Del Dolor Lumbar CrónicoJuan Ma TumiriNo ratings yet
- The Efficacy of Kinesiotaping On Locomotor Abilities in Cerebral Palsy: A Case StudyDocument6 pagesThe Efficacy of Kinesiotaping On Locomotor Abilities in Cerebral Palsy: A Case StudyDr. Krishna N. SharmaNo ratings yet
- Cognitive Functional Therapy For TheDocument13 pagesCognitive Functional Therapy For TheEma DanciuNo ratings yet
- Application of Pilates-Based Exercises in The Treatment of Chronic Non-Specific Low Back Pain: State of The ArtDocument5 pagesApplication of Pilates-Based Exercises in The Treatment of Chronic Non-Specific Low Back Pain: State of The ArtDiana Magnavita MouraNo ratings yet
- Case IcuDocument5 pagesCase IcuTrisha SuazoNo ratings yet
- Effects of PNF Method For Hemiplegic Patients With Brachial Predominance After Stroke: Controlled and Blinded Clinical TrialDocument6 pagesEffects of PNF Method For Hemiplegic Patients With Brachial Predominance After Stroke: Controlled and Blinded Clinical TrialAperito InternationalNo ratings yet
- Content ServerDocument4 pagesContent ServerErika AntalNo ratings yet
- Spinal Injury Nursing Care PlanDocument2 pagesSpinal Injury Nursing Care PlanPatricia OrtegaNo ratings yet
- Regis Garvey AAOMPT Poster 2008Document1 pageRegis Garvey AAOMPT Poster 2008smokey73No ratings yet
- Rehabilitation of Patellar TendinopathyDocument6 pagesRehabilitation of Patellar TendinopathyAlberto Saura RodríguezNo ratings yet
- Compre Notes!!!!!!!!!!!Document12 pagesCompre Notes!!!!!!!!!!!Cyenel DeiparineNo ratings yet
- Wilk Macrina Reinold 2006 Nonoperative Rehab For Traumatic and Atraumatic GH Instability PDFDocument16 pagesWilk Macrina Reinold 2006 Nonoperative Rehab For Traumatic and Atraumatic GH Instability PDFSusan KNo ratings yet
- Assessment Diagnosis Planning Interventions Rationale Evaluation Subjective: IndependentDocument3 pagesAssessment Diagnosis Planning Interventions Rationale Evaluation Subjective: IndependentAce Khiel PeraltaNo ratings yet
- Techniques Utilized in Rehabilitation: MobilizationDocument3 pagesTechniques Utilized in Rehabilitation: MobilizationAditya RanjanNo ratings yet
- DIAGNOSIS: Chronic Pain Related To Disease Process As Manifested by Presence of Mass On The LegDocument5 pagesDIAGNOSIS: Chronic Pain Related To Disease Process As Manifested by Presence of Mass On The LeggrizolaNo ratings yet
- Nursing Care Plan Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationRenie SerranoNo ratings yet
- Subjective Data: Short Term Goal: Independent: 1. Monitor Patient's Vital Signs. 2. Determine Diagnosis That Short Term GoalDocument3 pagesSubjective Data: Short Term Goal: Independent: 1. Monitor Patient's Vital Signs. 2. Determine Diagnosis That Short Term GoalGeralyn KaeNo ratings yet
- Vestibular Rehab Article 1Document6 pagesVestibular Rehab Article 1kavitha ganesanNo ratings yet
- O Fortalecimento Combinado Do Abdutor Do Quadril e Do Rotador Externo e o Alongamento Do Rotador Interno Do Quadril Melhoram A Dor e A Função em Pacientes Com Síndrome Da Dor Femoropatelar Um EnsaiDocument6 pagesO Fortalecimento Combinado Do Abdutor Do Quadril e Do Rotador Externo e o Alongamento Do Rotador Interno Do Quadril Melhoram A Dor e A Função em Pacientes Com Síndrome Da Dor Femoropatelar Um EnsaiLeticia ZaniniiNo ratings yet
- Priming BilateralDocument11 pagesPriming BilateralGita CahyaniNo ratings yet
- Prioritization of Problems Rank Problem Identified: San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument5 pagesPrioritization of Problems Rank Problem Identified: San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesTom CuencaNo ratings yet
- Anatomia 20iv 20toraceDocument59 pagesAnatomia 20iv 20toraceSufletoiiNo ratings yet
- Galea 2018Document11 pagesGalea 2018annisayaNo ratings yet
- Nursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale Evaluationmyer pasandalanNo ratings yet
- Jurnal KMBDocument8 pagesJurnal KMBRay HannaNo ratings yet
- Hindlimb Stretching Alters Locomotor Function After Spinal Cord Injury in The Adult RatDocument10 pagesHindlimb Stretching Alters Locomotor Function After Spinal Cord Injury in The Adult RatRafliNo ratings yet
- Mencari Bukti-Bukti Dari Hasil Penelitian (Artikel/jurnal) - Nama: Maghfira Cahyani Gumayy NIM: P27226018222 Prodi: D4 Alih Jenjang FisioterapiDocument16 pagesMencari Bukti-Bukti Dari Hasil Penelitian (Artikel/jurnal) - Nama: Maghfira Cahyani Gumayy NIM: P27226018222 Prodi: D4 Alih Jenjang Fisioterapifira gumayNo ratings yet
- NCP Orif Right Femur Post OpDocument2 pagesNCP Orif Right Femur Post OpCen Janber CabrillosNo ratings yet
- The Effect of Long Versus Short Pectoralis Minor Resting Length On Scapular Kinematics in Healthy IndividualsDocument12 pagesThe Effect of Long Versus Short Pectoralis Minor Resting Length On Scapular Kinematics in Healthy IndividualsAmit DhawanNo ratings yet
- Bobath Approach NotesDocument5 pagesBobath Approach NotesJuling Perales100% (3)
- NCP Severe HypocalcemiaDocument4 pagesNCP Severe HypocalcemiaMark Zedrix MediarioNo ratings yet
- 1 s2.0 S1013702513000444 MainDocument7 pages1 s2.0 S1013702513000444 MainChevelle VelleNo ratings yet
- Nursing Care Plan For Hip Fracture Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationDocument1 pageNursing Care Plan For Hip Fracture Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationJaylord Verazon100% (1)
- Sahin2011 (RCT)Document6 pagesSahin2011 (RCT)Diana YulianiNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale Desired Outcomes Subjective: "Napakasakit NG Mga Kasukasuhan Ko" As Verbalized by The PatientDocument5 pagesAssessment Diagnosis Planning Implementation Rationale Desired Outcomes Subjective: "Napakasakit NG Mga Kasukasuhan Ko" As Verbalized by The PatientAngelou Mortos100% (1)
- Cerebral Palsy: Causes and Treatment Alternatives, Based On The Evidence Provided by Gait Analysis - Rupcich M, Bravo RDocument2 pagesCerebral Palsy: Causes and Treatment Alternatives, Based On The Evidence Provided by Gait Analysis - Rupcich M, Bravo RRicardo BravoNo ratings yet
- Proprioceptive Neuromuscular Facilitation: Vicky S. WardlawDocument44 pagesProprioceptive Neuromuscular Facilitation: Vicky S. WardlawPraneetha Nouduri100% (1)
- Spinal Bifida Ncp-Impaired Physical MobilityDocument3 pagesSpinal Bifida Ncp-Impaired Physical MobilityNicole cuencos50% (2)
- OA NCPDocument5 pagesOA NCPsnow.parconNo ratings yet
- Nursing Care Plan FibromyalgiaDocument2 pagesNursing Care Plan Fibromyalgiaderic90% (10)
- The PNF (Proprioceptive Neuromuscular Facilitation) Stretching Technique - A Brief ReviewDocument6 pagesThe PNF (Proprioceptive Neuromuscular Facilitation) Stretching Technique - A Brief ReviewDiane Troncoso Alegria0% (1)
- Piis0003999398902878 PDFDocument7 pagesPiis0003999398902878 PDFErsya MuslihNo ratings yet
- CECS ProtocolDocument6 pagesCECS ProtocolTsz Kwan CheungNo ratings yet
- McCain GDocument5 pagesMcCain GDavid94No ratings yet
- Resume Updated 2020Document2 pagesResume Updated 2020api-414657737No ratings yet
- Brauncasereport Draft 6Document46 pagesBrauncasereport Draft 6api-414657737No ratings yet
- Patient Care Written Practical Portion Case 1Document7 pagesPatient Care Written Practical Portion Case 1api-414657737No ratings yet
- Academy of Geriatric Physical Therapy Knee Replacement BrochureDocument2 pagesAcademy of Geriatric Physical Therapy Knee Replacement Brochureapi-414657737No ratings yet
- Pi 0614 Hiblack f890b en WebDocument2 pagesPi 0614 Hiblack f890b en Web王偉仲No ratings yet
- Popular CultureDocument6 pagesPopular CultureAmritaNo ratings yet
- CFD - Basement Car ParkDocument43 pagesCFD - Basement Car ParkTanveer HasanNo ratings yet
- 1.1 - Selectividad Acti9Document34 pages1.1 - Selectividad Acti9Bladimir MichelNo ratings yet
- CADS Revit Scia Engineer Link Best PracticesDocument32 pagesCADS Revit Scia Engineer Link Best PracticestrevorNo ratings yet
- Modular Air Handling Unit (FMA)Document3 pagesModular Air Handling Unit (FMA)Salamet TeguhNo ratings yet
- EXP1POSTLABDocument13 pagesEXP1POSTLABGiane MagimotNo ratings yet
- Ac 521 007Document10 pagesAc 521 007JacquesNo ratings yet
- 520L0586 MMF044Document48 pages520L0586 MMF044vendas servicosNo ratings yet
- TA308 616configurationDocument1 pageTA308 616configurationJesus AvilaNo ratings yet
- Komatsu Technical BrochurDocument7 pagesKomatsu Technical BrochurBenjamin MossoNo ratings yet
- Augocom Micro 768 Battery Tester User ManualDocument29 pagesAugocom Micro 768 Battery Tester User ManualJorge PontonNo ratings yet
- Into The Unknown 21 Doc PDFDocument9 pagesInto The Unknown 21 Doc PDFFernando AlbuquerqueNo ratings yet
- Chapter 3 FinalizedDocument11 pagesChapter 3 Finalizedpeter vanderNo ratings yet
- Sermo 13 de Tempore (2 Feb in Praes)Document1 pageSermo 13 de Tempore (2 Feb in Praes)GeorgesEdouardNo ratings yet
- Mid-Year Examination, 2023 Science Year 7 1 HourDocument23 pagesMid-Year Examination, 2023 Science Year 7 1 HourAl-Hafiz Bin SajahanNo ratings yet
- Wjec Biology SpectificaionDocument93 pagesWjec Biology SpectificaionLucy EvrettNo ratings yet
- Vibrations - NptelDocument3 pagesVibrations - NptelMSK65No ratings yet
- Avionic ArchitectureDocument127 pagesAvionic ArchitectureRohithsai PasupuletiNo ratings yet
- Age ProblemDocument31 pagesAge ProblemKenny CantilaNo ratings yet
- Fantasy AGE - Spell SheetDocument2 pagesFantasy AGE - Spell SheetpacalypseNo ratings yet
- Texas Instruments FootprintsDocument7 pagesTexas Instruments FootprintsSteve SmithNo ratings yet
- Leta-Leta CaveDocument5 pagesLeta-Leta CaveToniNo ratings yet
- Streamline SWR (S) - Rev - 00-04-2019 PDFDocument2 pagesStreamline SWR (S) - Rev - 00-04-2019 PDFarjun 11No ratings yet
- Solomon On Sex - Avoiding Marital Disaster: February 12, 2012Document14 pagesSolomon On Sex - Avoiding Marital Disaster: February 12, 2012baimareanNo ratings yet
- JCHT35K9 EngDocument5 pagesJCHT35K9 EngRodica PuscauNo ratings yet
- NCERT Solutions For Class 12 Maths Chapter 10 Vector AlgebraDocument51 pagesNCERT Solutions For Class 12 Maths Chapter 10 Vector AlgebraKavin .J.S (KingK)No ratings yet
- XC24M MG DatasheetDocument3 pagesXC24M MG DatasheetAbdulJawad Ibrahim ElmezoghiNo ratings yet
- Draft STATCOM Maintenance Schedule (FINAL)Document36 pagesDraft STATCOM Maintenance Schedule (FINAL)Sukanta Parida100% (2)
- Mathematics For Engineers and Scientists 3 PDFDocument89 pagesMathematics For Engineers and Scientists 3 PDFShailin SequeiraNo ratings yet