Professional Documents
Culture Documents
Bioethics 1.01 Introduction To Bioethics - Dr. Sombilon PDF
Bioethics 1.01 Introduction To Bioethics - Dr. Sombilon PDF
Uploaded by
Jennifer Pisco Lirac0 ratings0% found this document useful (0 votes)
17 views2 pagesOriginal Title
Bioethics 1.01 Introduction to Bioethics - Dr. Sombilon.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
17 views2 pagesBioethics 1.01 Introduction To Bioethics - Dr. Sombilon PDF
Bioethics 1.01 Introduction To Bioethics - Dr. Sombilon PDF
Uploaded by
Jennifer Pisco LiracCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Subject: Bioethics
Topic: 1.01 Intro to Bioethics
Lecturer: Dr. Sombilon
Date: November 10, 2014
I. ETHICS o Medical ethics (more correct term)
A branch of philosophy o Business ethics
Practical science of MORALITY of human acts (Human act not the o Sexual ethics
same as the act of man as it is willful and voluntary.) o Social ethics
Teaches us how to judge accurately the moral GOODNESS or o Environmental policy and ethics
BADNESS of any human action, which is, learned since childhood at
home, school. It is a set of values/ training that you grew up with. IV. MEDICAL ETHICS
A “subset” of bioethics – a clinical or case-based approach
II. BASIC PRINCIPLES IN BIOETHICS Used interchangeably: “bioethics”, “medical ethics” and
A. Beneficence “biomedical ethics”
ONE OUGHT TO DO GOOD Encompasses (but not limited to):
Seek the patient’s well-being (Patient’s well-being is the #1 o Abortion
priority) o Euthanasia
Provide standards of due care and risk/benefit assessment (Be o Confidentiality
competent. You cannot be ethical if you’re not competent because o Truth telling
you can’t provide adequate care. Always tell the risk of the o Fair distribution of resources
procedure/treatment!) o Informed consent
o Research involving human subjects
B. Non-Maleficence o HIV/AIDS issues
o Organ transplantation
DO NO HARM
o Genetic engineering
Latin: “Primum Non Nocere” = First Do No Harm
o Human cloning
Avoid unnecessary expense, consult, procedures and medications
o Stem cell research
Mirror image of Beneficence o Reproductive rights and assisted reproductive techniques
The application of the GENERAL PRINCIPLES of ethics to the moral
C. Informed Consent problems of the medical profession
In any procedure, provide the patient with a COMPLETE, CORE: based on TRUST; ethics of a physician- patient relationship
ADEQUATE DISCLOSURE of his illness and OPTIONS in a language o As a physician, you have to follow certain specific RULES OF
he understands for the patient to be able to make a rational and CONDUCT (you can’t just act whatever you want to do) – it is
free decision mandated and looked-after by Philippine Medical Association
o What the physician PROVIDES for the patient: you should be
D. Autonomy competent, you should care for your patient, you should have
RESPECT FOR PERSONS empathy and compassion
Respect the patient’s rational decision as long as he is aware of the o What the physician’s DUTIES are to the patient and VICE-
consequences VERSA – the patients have to be truthful, and forward in their
The patient has a right to refuse (if he is competent or in his right dealings with you
mind) o Further proofreading of the trans
Especially important in terminally ill patients when they refuse o correction of minor details such as
extraordinary means of treatment chemical synapse is faster than electrical synapse ->
This premise serves as basis why Jehovah’s witnesses do not electrical synapse is faster
accept blood transfusion, and women do abortion fertilized egg goes through respiratory tract ->
reproductive tract
E. Justice Addition of information from the book should there be a
Allocating scarce resources fairly and according to medical needs need
Improvement of explanation should there be a need
MNEMONIC- Principles in Bioethics Ensure that the trans was properly formatted by following
A- Autonomy the Trans Template
B- Beneficence Please note. They are to ensure that it is properly
C- Consent (Informed Consent) formatted. They are not to format it for you.
D- Do no harm (Non-maleficence) Ensure that a hard copy is left in Alva so it may be
E- Equality (Justice) photocopied by those who prefer to have a hard copy
TUSKEGEE EXPERIMENT (1930s)
III. BIOETHICS o Done by the US Government
“Life ethics” – philosophical and broad o 400 Black American farmers with Syphilis were signed up to
observe the course of the disease
More encompassing than medical ethics, includes additional issues
o 1949 – discovery of a cure Penicillin
not necessarily a part of medical ethics
o Treatment was deliberately withheld from the subjects in order
Trans Group: Page 1 of 2
Edited By:
to observe the progress of the disease and its complications Bioethics (1995-2001)
until death o Bioethics Institutes
o Patients were told they s imply had “bad blood” and lived with Consists of physicians (not just one), layman, lawyer, and
the disease until their death, some in the 1970s theologians to help resolve medico-moral problems, NOT
o US Gov’t reparations and recognition of these men did little to just doctors!
regain the trust of the public in human experimentation o Ethics Review Board (ERB)
o Only in the last term of President Clinton (recent) was a No paper can be started without going through the ERB
FORMAL APOLOGY to the families of the Tuskegee victims o The Future of Bioethics
given Brain mapping and highly precise image technology –
neuroethical issues to determine personality traits and
MODERN DAY BIOETHICS CASE CANDIDATES dis ease and behavior predisposition: assessing a
o 1962 – Shana Alexander on Seattle Artificial Kidney Program person’s memories for legal or forensic purposes
First dialysis machine
“God’s Squad” – decides who gets to live or die since
organ transplant was very limited
o 1967 – Dr. Christian Barnard on first successful heart transplant
o 1973 – Roe vs. Wade: US Supreme Court decision on abortion
Declared the principle of autonomy
Basis for legalization of abortion
o 1974 – Exposure of Tuskegee Syphilis study
The National Commission for the Protection of Human
o Subjects in Biomedical and Behavioral Research
o 1976 – Quinlan Case: US Supreme Court decision on end of life
Case of Karen Quinlan who was then in her 20s (First
Case of PVS)
She took drugs, went to a party and consumed alcohol.
She was in a coma for years and was hooked on artificial
respirator
She was in PVS (Persistent Vegetative State)
Decision was in favor of parent’s plea to remove life
support
o 1978 – Drs. Patrick Steptoe and Robert Edwards
First test tube baby (In Vitro Fertilization or IVF) and
embryo trans plant baby Louise Brown
o 1980s-Present – HIV/AIDS
Ethical issues: Discrimination and absence of beneficence
for the African population who were first tested and
studied for the diseases
o 1991 – The Patient Self-determination Act
Emphasis on need for advanced directives, living will and
ethics committees
Example is the case of Nancy Cruzan who was in PVS
o 1983 – Case of Nancy Cruzan (right-to-die, 2nd case of PVS)
You may access her story at:
http://www.che.org/members/ethics/docs/2146/The%2
0case%20of%20Nancy%20Cruzan%20AC%20Module%20
12.pdf
o 1996 – Dolly the first cloned sheep and Stem Cell Technology
o 2002 – Legalization of Euthanasia in Netherlands
Emergence of Right to Die advocates and movement
Oregon Death with Dignity Act
o 2007 – Terri Schiavo
End of life case involving termination of feeding (Third
Case of PVS)
BIOETHICS AS A FIELD MORE DEFINED
o Bioethics Institutes
1969 Hastings Center
1971 – Kennedy Institute for Ethics (Georgetown Univ.)
o Tom Beauchamp and James Childress (1977) - The Principles of
Biomedical Ethics (bible of bioethics)
o National Bioethics Advisory Committee, President’s Council on
Page 2 of 2
You might also like
- Reflection About Patients With DementiaDocument2 pagesReflection About Patients With Dementiaalexander abasNo ratings yet
- Ethical Issues With Informed Consent (Escobedo, 2007) PDFDocument8 pagesEthical Issues With Informed Consent (Escobedo, 2007) PDFMuhammad YusarNo ratings yet
- Trauma - Dr. TayagDocument2 pagesTrauma - Dr. TayagJyl Yan SelasorNo ratings yet
- CLASSIFICATION OF MALOCCLUSION DR AnamikaDocument110 pagesCLASSIFICATION OF MALOCCLUSION DR Anamikadeepankar sarkarNo ratings yet
- Larynx MCQSDocument114 pagesLarynx MCQSsidsudp100% (2)
- Physiological-Changes-in-Aging - RESPIRATORY-SYSTEM (Autosaved)Document70 pagesPhysiological-Changes-in-Aging - RESPIRATORY-SYSTEM (Autosaved)Patric Aaron de VillaNo ratings yet
- NCM 108 Week 1 Topic 2 Part 2: International Code of Ethics For NursesDocument4 pagesNCM 108 Week 1 Topic 2 Part 2: International Code of Ethics For NursesMarielle ChuaNo ratings yet
- Student Activity Sheet Nur 104 Health Care Ethics Bs Nursing / Third Year Session # 2 MaterialsDocument5 pagesStudent Activity Sheet Nur 104 Health Care Ethics Bs Nursing / Third Year Session # 2 MaterialsMary Jane RodecaNo ratings yet
- FINAL PAPER Xtian EthicsDocument55 pagesFINAL PAPER Xtian EthicsMary Neil GalvisoNo ratings yet
- GordonDocument4 pagesGordonShekinah Fuellas CantorNo ratings yet
- Mod 1 Theories and Principles of Healthcare EthicsDocument58 pagesMod 1 Theories and Principles of Healthcare EthicsKelly Arceo100% (1)
- Health PromotionDocument5 pagesHealth PromotionLei SantillanNo ratings yet
- BIOETHICS 2011 TransparencyDocument12 pagesBIOETHICS 2011 TransparencyLean RossNo ratings yet
- Lesson 1 Principles and TheoriesDocument11 pagesLesson 1 Principles and TheoriesCelline Isabelle ReyesNo ratings yet
- Health Care Ethics PrinciplesDocument2 pagesHealth Care Ethics PrinciplesNicco AcaylarNo ratings yet
- A Case Report of Obsessive-Compulsive DisorderDocument6 pagesA Case Report of Obsessive-Compulsive DisorderfonsoalNo ratings yet
- Ethical Theories: Prepared By: Regine Emerald B Dela Cruz RNDocument20 pagesEthical Theories: Prepared By: Regine Emerald B Dela Cruz RNRegine Dela CruzNo ratings yet
- Ethical Principles of NursingDocument2 pagesEthical Principles of NursingClarissa HeatonNo ratings yet
- Care of The Elderly: Presented By: Roselily CoquillaDocument33 pagesCare of The Elderly: Presented By: Roselily CoquillaOng KarlNo ratings yet
- Stages of Infection 2Document7 pagesStages of Infection 2Karren Taquiqui PleteNo ratings yet
- NCMB 314 - M2-Cu10Document10 pagesNCMB 314 - M2-Cu10Giselle EstoquiaNo ratings yet
- SchizophreniaDocument36 pagesSchizophreniasanyakotwani08No ratings yet
- Caring and The Professional Practice of NursingDocument4 pagesCaring and The Professional Practice of NursingGalihPioNo ratings yet
- Virtue EthicsDocument21 pagesVirtue EthicsNikko SterlingNo ratings yet
- Health Care EthicsDocument4 pagesHealth Care EthicsJaimie Banaag100% (1)
- Bioethics Midterm 1Document82 pagesBioethics Midterm 1Pasay Trisha Faye Y.No ratings yet
- Nursing Philosophy: Watson's Theory of Human Caring: Maria Celina Casis, RN, MSNDocument45 pagesNursing Philosophy: Watson's Theory of Human Caring: Maria Celina Casis, RN, MSNChristian Fel MoralitaNo ratings yet
- Bioethics: Walbert F. Delos Santos, RN - MNDocument43 pagesBioethics: Walbert F. Delos Santos, RN - MNmaidymae lopezNo ratings yet
- Bioethics Mediation: A Guide to Shaping Shared Solutions, Revised and Expanded EditionFrom EverandBioethics Mediation: A Guide to Shaping Shared Solutions, Revised and Expanded EditionNo ratings yet
- Biliran Province State University: ISO 9001:2015 CERTIFIED School of Nursing and Health SciencesDocument10 pagesBiliran Province State University: ISO 9001:2015 CERTIFIED School of Nursing and Health SciencesMaia Saivi OmegaNo ratings yet
- Health Care Ethics 2024Document13 pagesHealth Care Ethics 2024celestineNo ratings yet
- Behavior and Mental StatusDocument41 pagesBehavior and Mental StatusGokul Poudel100% (1)
- Ethics in Research FMCHDocument44 pagesEthics in Research FMCHPatricia Hariramani100% (1)
- Medsurg Reviewer1Document27 pagesMedsurg Reviewer1Angelie BigayNo ratings yet
- Medical and Surgical Practice TestDocument9 pagesMedical and Surgical Practice TestJainah Rose GubacNo ratings yet
- M1 - Nusing Care ManagementDocument40 pagesM1 - Nusing Care ManagementKristine KimNo ratings yet
- NCMB314 Prelim ReadingsDocument77 pagesNCMB314 Prelim ReadingsNine SoleilNo ratings yet
- Lesson 6 Bioethics and Its Application in VariousDocument19 pagesLesson 6 Bioethics and Its Application in VariousJoycee BoNo ratings yet
- Ethical and Moral Issues in Healthcare by Reason ChivakaDocument15 pagesEthical and Moral Issues in Healthcare by Reason Chivakareach2250% (2)
- Ethical Concepts in NursingDocument18 pagesEthical Concepts in Nursingjenn1722No ratings yet
- Ethical Issues in Pediatric AnesDocument16 pagesEthical Issues in Pediatric AnesrejNo ratings yet
- St. Anthony'S College - Nursing Department: Theoretical Foundations in NursingDocument86 pagesSt. Anthony'S College - Nursing Department: Theoretical Foundations in NursingCandido Kenneth JohnNo ratings yet
- NCM108 Module 2 MidtermDocument18 pagesNCM108 Module 2 MidtermblaireNo ratings yet
- ObjectivityDocument13 pagesObjectivityDeepu JoseNo ratings yet
- Jean Watson's TheoryDocument11 pagesJean Watson's TheoryBishwajitMazumder100% (1)
- Ethical Issues at The End of LifeDocument7 pagesEthical Issues at The End of LifeCarina FranciscoNo ratings yet
- Elimination Disorder: Presented by Saba AhmedDocument49 pagesElimination Disorder: Presented by Saba AhmedRana Ahmad Gulraiz100% (1)
- She Believed That in The Nurturing Environment, The Body Could Repair ItselfDocument7 pagesShe Believed That in The Nurturing Environment, The Body Could Repair ItselfMegan N. ReyesNo ratings yet
- NCM 103Document48 pagesNCM 103Cheenapot BerberNo ratings yet
- The Role of Ethical Principles in Health Care and The Implications For Ethical CodesDocument6 pagesThe Role of Ethical Principles in Health Care and The Implications For Ethical CodesNewfaceNo ratings yet
- Non Communicable DiseaseDocument13 pagesNon Communicable DiseaseClancy Anne Garcia Naval100% (1)
- Physical Examination & Health Assessment CH 1-10 Flashcards - QuizletDocument8 pagesPhysical Examination & Health Assessment CH 1-10 Flashcards - QuizletskrameerNo ratings yet
- Nursing Philosophy ReflectionDocument7 pagesNursing Philosophy Reflectionapi-480790431No ratings yet
- Module 5 Ethics in GeriatricPsychiatric and Mental Health NursingDocument7 pagesModule 5 Ethics in GeriatricPsychiatric and Mental Health NursingMaia Saivi OmegaNo ratings yet
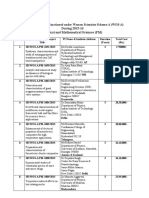
- Family Health AssessmentDocument23 pagesFamily Health AssessmentPatrick Poculan100% (1)
- Incontinence Case StudyDocument26 pagesIncontinence Case StudyRose AnnNo ratings yet
- Care PlanDocument26 pagesCare PlanChevelle Valenciano-GaanNo ratings yet
- Activity 2 Answer The Following Questions: 10 Points EachDocument4 pagesActivity 2 Answer The Following Questions: 10 Points EachArmySapphireNo ratings yet
- NCMA113 SL RUBRICS Administering Blood TransfusionDocument2 pagesNCMA113 SL RUBRICS Administering Blood TransfusionJoy Ann BasisNo ratings yet
- Medical Ethics - Bioethical PrinciplesDocument2 pagesMedical Ethics - Bioethical PrinciplesApril AramNo ratings yet
- Urinary Tract InfectionsDocument4 pagesUrinary Tract InfectionsRalph Patrick SamaniegoNo ratings yet
- Angel BioethicsDocument13 pagesAngel BioethicsJen PanganibanNo ratings yet
- Barriers To Teaching and Obstacles To Learning: Click To Edit Master Subtitle StyleDocument7 pagesBarriers To Teaching and Obstacles To Learning: Click To Edit Master Subtitle StyleAngel RescoNo ratings yet
- RSC Application Form 04 10 18 (V 7)Document2 pagesRSC Application Form 04 10 18 (V 7)Jyl Yan SelasorNo ratings yet
- A Case History of Dedifferentiated LiposarcomaDocument27 pagesA Case History of Dedifferentiated LiposarcomaJyl Yan SelasorNo ratings yet
- Fairy TailDocument59 pagesFairy TailJyl Yan SelasorNo ratings yet
- Arterial Blood Gases: Clinical Diagnosis LectureDocument3 pagesArterial Blood Gases: Clinical Diagnosis LectureJyl Yan SelasorNo ratings yet
- Far Eastern University - Nicanor Reyes Medical FoundationDocument2 pagesFar Eastern University - Nicanor Reyes Medical FoundationJyl Yan SelasorNo ratings yet
- Psychiatry Reporting - Classification in PsychiatryDocument13 pagesPsychiatry Reporting - Classification in PsychiatryJyl Yan SelasorNo ratings yet
- Travel HistoryDocument1 pageTravel HistoryJyl Yan SelasorNo ratings yet
- Far Eastern University - Nicanor Reyes Medical FoundationDocument2 pagesFar Eastern University - Nicanor Reyes Medical FoundationJyl Yan SelasorNo ratings yet
- Surgery Shock SamplexDocument2 pagesSurgery Shock SamplexJyl Yan SelasorNo ratings yet
- NMAT ChemistryDocument7 pagesNMAT ChemistryJyl Yan SelasorNo ratings yet
- PEDIATRICS GND NotesDocument7 pagesPEDIATRICS GND NotesJyl Yan SelasorNo ratings yet
- NMAT BiologyDocument6 pagesNMAT BiologyJyl Yan SelasorNo ratings yet
- Afrezza Review For FDADocument12 pagesAfrezza Review For FDACREWNo ratings yet
- Drug StudyDocument8 pagesDrug StudyJason AvellanoNo ratings yet
- Community Diagnosis Barangay Mabato: Presented ToDocument73 pagesCommunity Diagnosis Barangay Mabato: Presented ToRose AnnNo ratings yet
- Department of Nursing, Georgetown University School of Nursing & Health Studies, Washington, D.CDocument1 pageDepartment of Nursing, Georgetown University School of Nursing & Health Studies, Washington, D.CBrittany WorrallNo ratings yet
- Cancer Cure Booklet - Drkelleyenzymes PDFDocument21 pagesCancer Cure Booklet - Drkelleyenzymes PDFSengNo ratings yet
- Sex Ed PresentationDocument20 pagesSex Ed Presentationapi-399914198No ratings yet
- Trolley Emergency 2020Document5 pagesTrolley Emergency 2020erma wanda mundariNo ratings yet
- What's in A Definition? Holistic Nursing,, and IntegrativeDocument13 pagesWhat's in A Definition? Holistic Nursing,, and IntegrativeAna MahayaniNo ratings yet
- Daftar PustakaDocument7 pagesDaftar PustakaNitya Manggala JayaNo ratings yet
- Kathleen Noftle Criminal ComplaintDocument14 pagesKathleen Noftle Criminal ComplaintJoe Dwinell0% (1)
- Hospital Tengku Ampuan RahimahDocument14 pagesHospital Tengku Ampuan Rahimahmyvi317No ratings yet
- Dissociation Theory Pierre JanetDocument11 pagesDissociation Theory Pierre Janetvasilisc100% (1)
- Asphyxia in Forensic AspectDocument32 pagesAsphyxia in Forensic Aspectderi100% (1)
- Sleep Disorder Evaluation TemplateDocument2 pagesSleep Disorder Evaluation Templatee-MedTools100% (12)
- Mine Rescue Questions and Answers PDFDocument19 pagesMine Rescue Questions and Answers PDFInayat ullah BalochNo ratings yet
- Barr Bodies The Lyon Hypothesis and Dosage CompensationDocument4 pagesBarr Bodies The Lyon Hypothesis and Dosage CompensationDanny GazaliNo ratings yet
- Armand BarbaultDocument5 pagesArmand BarbaulttravellerfellowNo ratings yet
- LabanLEGALIZE MEDICAL MARIJUANADocument13 pagesLabanLEGALIZE MEDICAL MARIJUANAArnold SumadilaNo ratings yet
- Jurnal Daun KelorDocument7 pagesJurnal Daun Kelormargie ayuNo ratings yet
- Plague Doctor (Fan Wfrp2)Document1 pagePlague Doctor (Fan Wfrp2)PsyckoSama100% (2)
- Job Application LetterDocument12 pagesJob Application LetterIcha Aisah100% (3)
- Trans CulturalDocument97 pagesTrans CulturalkewlangotNo ratings yet
- Complete Project PDFDocument67 pagesComplete Project PDFRaghu Nadh100% (1)
- 2017 Updated Guideline On The Management of Common Bile Duct Stones CBDSDocument19 pages2017 Updated Guideline On The Management of Common Bile Duct Stones CBDSFieska AzizahNo ratings yet
- 1.1 Background of The StudyDocument7 pages1.1 Background of The StudyMarichu CayabyabNo ratings yet
- What Is A Biosensor, Types of Biosensors and ApplicationsDocument12 pagesWhat Is A Biosensor, Types of Biosensors and ApplicationsPramillaNo ratings yet
- HTN CV ComorbiditiesDocument19 pagesHTN CV Comorbiditieslakshminivas PingaliNo ratings yet
- WosaDocument18 pagesWosaAnusheelaNo ratings yet