Professional Documents
Culture Documents
cp1 Week 7 Tutorial 1
Uploaded by
api-4680937140 ratings0% found this document useful (0 votes)
33 views4 pagesOriginal Title
cp1 week 7 tutorial 1
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
33 views4 pagescp1 Week 7 Tutorial 1
Uploaded by
api-468093714Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
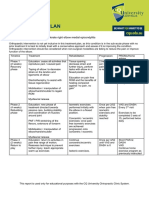
CP1 Tutorial Week 7
Summary of this term:
Techniques/Systems Core Principles/Values When do we use them?
Paul Hodges N/A Neuromotor control of movement Spinal control – lower back and
and stability changes with pain. pelvic pain
The effect of pain on motor control
and possible mechanisms.
Karel Lewit MRT: Manipulation treatment does not Reduction of skin
(Zac) 1. Proprioceptive Neuromuscular change the shape or position of a tenderness
Facilitation a) Hold–relax b) structure, but it could change the Reduction of connective
Contract–relax c) Rhythmic function of the MSK system. tissue pain
stabilization Frequently used muscles Release myofascial pressure
2. Muscle energy procedures will have a roundness of Shifting and stretching
3. Post-isometric relaxation shape and or convexity fascia
4. Post-facilitation stretch between origin and Relaxation of hypertonic or
insertion overactive muscle
Less used or atrophied
muscles will have a
hollowness or concavity of a
shape
Observation of muscle form
by looking at the
topography of the body,
notice asymmetries and
decreased development
areas
Observing muscles can tell
you a lot about how a
person moves and where
pain might be or develop.
Vladimir Janda Movement Patterns: Movement patterns rather Functional assessment of
JIMBO Hip Extension than individual muscles and movements
Hip Adduction looked globally rather than Upper cross syndrome
Hip Abduction locally for the causes of Lower cross syndrome
Trunk Curl-up muscle dysfunction Inner cross syndrome
Cervical flexion Layer syndrome
Push-up Looks into Phasic and tonic
Shoulder abduction Muscles
Pavel Koler N/A Prague school – N/A
neurodevelopmental aspects of
motor control.
The importance of the diaphragm in
the stability of the spine.
Stuart MacGill Dynamic Neuromuscular Injury – failure of tissue when load Lower back pain
Stabilization exceeds tolerance/strength of tissue
McGill ‘big 3’ - curl up; Stability through stiffness – motor
bird/dog; side bridge control increases stability
Robin McKenzie 1. flexion in standing Mechanical pain may Identify causes of low back pain,
2. repeated flexion in develop from postural disc pathology in postural
standing stressed, joint derangement syndromes, pathology from
3. extension in standing or by dysfunction muscles, ligaments, disc, apophyseal
4. repeated extension in McKenzie believes that joints and fascia due to adaptive
standing almost all low back pain is shortening of muscles in
5. side gliding in standing aggravated and dysfunction syndrome and internal
6. repeated side gliding in perpetuated, if not caused, derangement of the disc, alteration
standing by poor sitting postures in in the position of the fluid in the
7. flexion in lying both sedentary and manual nucleus and the surrounding
8. repeated flexion in lying workers annulus, disturbing the resting
9. extension in lying Physicians should exclude position of the above and below
10. repeated extension in serious and unsuitable vertebrae in derangement
lying pathologies from being syndrome.
treated by mechanical
therapy. McKenzie feels the Movements are chosen to decrease
therapist should confine mechanical deformation by
themselves to diagnosing reducing the derangement.
MSK mechanical lesions –
this is where chiros differ The movements will gradually
from therapists stretch and lengthen contracted soft
Spinal pain of mechanical tissues, eventually reducing
origin can be classified into mechanical deformation
1. Postural syndrome
2. Dysfunction syndrome
3. Derangement syndrome
Movement of the vertebral
column, the nucleus can
alter its shape and with
sustained positions or
repeated movements will
eventually alter its position.
Gray Cook FMS The whole is greater than the sum Non acute
SFMA of its parts.
“Movement patterns are purposeful
combinations of mobile and stable
segments working in coordinated
harmony to produce efficient and
effective movement sequences”
Screening helps us identify what we
want to change, improve or
rehabilitate.
Screening may be predictive of
injury
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Saes TABLEDocument13 pagesSaes TABLERiyaz BasheerNo ratings yet
- EPB2.4 + V3f20 Installation - Start-Up ProcDocument30 pagesEPB2.4 + V3f20 Installation - Start-Up ProcBeltran Héctor75% (4)
- EHS Audit - Review PaperDocument5 pagesEHS Audit - Review PaperYousef OlabiNo ratings yet
- Fms Score SheetDocument2 pagesFms Score Sheetapi-468093714No ratings yet
- wk8 - Group1 RehabDocument3 pageswk8 - Group1 Rehabapi-468093714No ratings yet
- Week 8 Category 2Document4 pagesWeek 8 Category 2api-468093714No ratings yet
- Week 6 Category 1Document4 pagesWeek 6 Category 1api-468093714No ratings yet
- Zac Williams Category 1 Week 8Document3 pagesZac Williams Category 1 Week 8api-468093714No ratings yet
- Week 7 Category 3Document3 pagesWeek 7 Category 3api-468093714No ratings yet
- Rehab - Week 7 - Group 1 1Document9 pagesRehab - Week 7 - Group 1 1api-468093714No ratings yet
- Williams Zac - Nutrition ReflectionDocument5 pagesWilliams Zac - Nutrition Reflectionapi-468093714No ratings yet
- Category 3 Week 8Document1 pageCategory 3 Week 8api-468093714No ratings yet
- Week 6 - Group 1 RehabDocument6 pagesWeek 6 - Group 1 Rehabapi-468093714No ratings yet
- Category 2 Week 6Document6 pagesCategory 2 Week 6api-468093714No ratings yet
- Week 7 Category 2Document5 pagesWeek 7 Category 2api-468093714No ratings yet
- Category 1 - Week 5 - Zac WilliamsDocument4 pagesCategory 1 - Week 5 - Zac Williamsapi-468093714No ratings yet
- Week 6 - Group 1 RehabDocument6 pagesWeek 6 - Group 1 Rehabapi-468093714No ratings yet
- Zac Williams Category 3 - Week 6Document6 pagesZac Williams Category 3 - Week 6api-468093714No ratings yet
- Week 6 Category 1Document4 pagesWeek 6 Category 1api-468093714No ratings yet
- Week 5 Case Catagory 3Document5 pagesWeek 5 Case Catagory 3api-468093714No ratings yet
- Zac Williams Simple MSK Management PlanDocument1 pageZac Williams Simple MSK Management Planapi-468093714No ratings yet
- Zac Williams Patient ReferralDocument1 pageZac Williams Patient Referralapi-468093714No ratings yet
- MR JD Case Summary - Zac WilliamsDocument5 pagesMR JD Case Summary - Zac Williamsapi-468093714No ratings yet
- Week 4 Group 1 - Nursemaids ElbowDocument3 pagesWeek 4 Group 1 - Nursemaids Elbowapi-468093714No ratings yet
- Week 5 Category 2 QuestionsDocument4 pagesWeek 5 Category 2 Questionsapi-468093714No ratings yet
- Zac Williams Serious MSK Management PlanDocument1 pageZac Williams Serious MSK Management Planapi-468093714No ratings yet
- Zac Williams ReportDocument1 pageZac Williams Reportapi-468093714No ratings yet
- cp1 Rehab Ica Sign SheetDocument7 pagescp1 Rehab Ica Sign Sheetapi-468093714No ratings yet
- cp1 Week 6 Tutorial 2Document4 pagescp1 Week 6 Tutorial 2api-468093714No ratings yet
- cp1 Week 8 TutorialDocument3 pagescp1 Week 8 Tutorialapi-468093714No ratings yet
- cp120 Competency ListDocument1 pagecp120 Competency Listapi-468093714No ratings yet
- Group 1 Tutorial IcaDocument7 pagesGroup 1 Tutorial Icaapi-468093714No ratings yet
- M7Ge-Iiib-1: Renante Tillo JosolDocument3 pagesM7Ge-Iiib-1: Renante Tillo JosolRenante T. JosolNo ratings yet
- Instability of Slender Concrete Deep BeamDocument12 pagesInstability of Slender Concrete Deep BeamFrederick TanNo ratings yet
- ECON 211: Principles of Macroeconomics-901: Smhussain@vcu - EduDocument6 pagesECON 211: Principles of Macroeconomics-901: Smhussain@vcu - EdusshinnNo ratings yet
- Deaths in New York City Are More Than Double The Usual TotalDocument3 pagesDeaths in New York City Are More Than Double The Usual TotalRamón RuizNo ratings yet
- 12 - Chepter 5Document11 pages12 - Chepter 5KhaireddineNo ratings yet
- Dassault Systems Academic CalenderDocument5 pagesDassault Systems Academic CalenderSarath KumarNo ratings yet
- HSC School Ranking 2012Document4 pagesHSC School Ranking 2012jHexst0% (1)
- Table of Contents and Company Profile of JPCOM CARES STAC5Document4 pagesTable of Contents and Company Profile of JPCOM CARES STAC5Ch Ma100% (1)
- Q1 WK 2 To 3 Las Fabm2 Kate DionisioDocument8 pagesQ1 WK 2 To 3 Las Fabm2 Kate DionisioFunji BuhatNo ratings yet
- Alup Allegro 37 AC IE3 400V 4-13bar 50Hz Metric Technical Data ENDocument2 pagesAlup Allegro 37 AC IE3 400V 4-13bar 50Hz Metric Technical Data ENBosznay ZoltánNo ratings yet
- Wooden Buildings: exposed to tiếp xúc với dramatic renewal sự làm mới đáng kểDocument6 pagesWooden Buildings: exposed to tiếp xúc với dramatic renewal sự làm mới đáng kểNguyễn Phạm Thảo NguyênNo ratings yet
- Major06 QP DLP NEET2019 (Pmtcorner - In) PDFDocument40 pagesMajor06 QP DLP NEET2019 (Pmtcorner - In) PDFMegha HazarikaNo ratings yet
- Henry's Bench: Keyes Ky-040 Arduino Rotary Encoder User ManualDocument4 pagesHenry's Bench: Keyes Ky-040 Arduino Rotary Encoder User ManualIsrael ZavalaNo ratings yet
- IIRDocument2 pagesIIRJagan FaithNo ratings yet
- Music and Yoga Are Complementary To Each OtherDocument9 pagesMusic and Yoga Are Complementary To Each OthersatishNo ratings yet
- Research ProposalDocument2 pagesResearch Proposalsmh9662No ratings yet
- Inertia Physics: Defi Ni Ti OnDocument2 pagesInertia Physics: Defi Ni Ti OnSentoash NaiduNo ratings yet
- Zero Voltage Switching Active Clamp Buck-BoostDocument10 pagesZero Voltage Switching Active Clamp Buck-Boostranjitheee1292No ratings yet
- 02 Geotechnical Investigation (General)Document35 pages02 Geotechnical Investigation (General)Miftahul JannaNo ratings yet
- Group 6G Revised Research Manuscript 1Document57 pagesGroup 6G Revised Research Manuscript 1Mc Rollyn VallespinNo ratings yet
- Wireless Cellular and LTE 4g Broadband PDFDocument26 pagesWireless Cellular and LTE 4g Broadband PDFAE videosNo ratings yet
- Factors Affecting Pakistani English Language LearnersDocument19 pagesFactors Affecting Pakistani English Language LearnersSaima Bint e KarimNo ratings yet
- Cebex 305: Constructive SolutionsDocument4 pagesCebex 305: Constructive SolutionsBalasubramanian AnanthNo ratings yet
- UNIT 5 Standard Costing - Variance AnalysisDocument50 pagesUNIT 5 Standard Costing - Variance AnalysisMohsin SheikhNo ratings yet
- Reflective EssayDocument4 pagesReflective Essayapi-385380366No ratings yet
- معالجات ستاذ يزنDocument11 pagesمعالجات ستاذ يزنammerNo ratings yet
- Transfer Request 2022 - CBOA CHENNAIDocument5 pagesTransfer Request 2022 - CBOA CHENNAIVignesh NarayananNo ratings yet