Professional Documents
Culture Documents
Low Level Laser Therapy - A Standard of Supportive Care For Cancer
Uploaded by
Eduardo Garza GarzaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Low Level Laser Therapy - A Standard of Supportive Care For Cancer
Uploaded by
Eduardo Garza GarzaCopyright:
Available Formats
available at www.jstage.jst.go.
jp/browse/islsm REVIEW ARTICLES
Low-level laser therapy: a standard of supportive care
for cancer therapy-induced oral mucositis in head
and neck cancer patients?
E Jadaud 1, RJ Bensadoun 2
1: Institut de Cancérologie de l’Ouest, Paul Papin, Service d’Oncologie Radiothérapie,
49933 Angers Cedex 9, France
2: Service d’Oncologie radiothérapique, CHU de Poitiers, BP 577, 86021 Poitiers Cedex, France
Background and aims: Oral mucositis (OM) is still a common and severe acute side-effect of
many oncologic treatments, especially in patients treated for head and neck cancer. It may affect
quality of life, require supportive care and impact treatment planning and its efficacy. Low-level
laser therapy (LLLT) seems to promote pain relief and reduces OM incidence and its severity. It has
been recommended for these patients as a treatment option but without any consensus in the LLLT
procedure. New recommendations and perspectives for clinical trials will be discussed.
Materials (Subjects) and Methods: Step by step, the efficacy of soft laser in the management of
iatrogenic oral mucositis has been evaluated during the last two decades. Its effectiveness and level
of recommendation got stronger with time. We will report and discuss some major results and the
latest recommendations published on this topic.
Results: The major clinical results have been reported and analysed last year in a first meta-analy-
sis 1). 11 randomized placebo-controlled trials were selected with a total of 415 patients treated
with chemotherapy and/or radiotherapy for head and neck cancer. The relative risk for developing
OM was significantly reduced after LLLT but only for a dose between 1 to 6 Joules per point. Pain,
severity and duration of OM grade ≥ 2 were also reduced without difference with placebo for pos-
sible side-effects. Nine years after the positive results published for patients treated by radiotherapy
alone 2), a new French randomized, multicentric, phase III trial for patients treated with new stan-
dard treatment, using LLLT in accordance to recent recommendations is ongoing. Seven centers are
specifically established for this trial which should include a hundred patients.
Conclusions: The very encouraging results of LLLT in the prevention and treatment of OM in
patients treated by chemotherapy or radiotherapy for advanced head and neck cancer could soon
be proposed as a new standard of care, according to the multinational Association of Supportive
care in Cancer (MASCC) criteria. Modern lasers are less time consuming and extraoral applicators
for a possible use by trained paramedical staff could be helpful to complete clinician practice. A
preventive dose of 2 J/cm2 and a curative dose of 4 J/cm2 if using a red wavelength lasers are now
recommended.
Key words: low-level laser therapy, oral mucositis, radiation therapy, chemotherapy
INTRODUCTION neck cancer (Fig.1). Its prevalence has increased over
the last 5 years due to more aggressive treatment pro-
Oral mucositis (OM) is a frequent acute side effect of tocols and combined modality regimens, reaching 36%
antineoplastic treatment in patients treated by radio- to 100% of patients 3). This painful side effect reduces
therapy and/or chemotherapy especially for head and quality of life and often requires narcotic analgesia,
enteral or parenteral nutrition with additional costs 4).
Addressee for Correspondence: Modifications of treatment planning may be nec-
Eric Jadaud. ICO Paul papin, Service de radiothérapie. essary, leading to 19% of interruptions and possibly
2 rue moll. 49933 Angers Cedex 9. France
eric.jadaud@ico.unicancer.fr; Received Date: October 17th, 2012
00(33)241352700 Accepted Date: December 1st, 2012
©2012 JMLL, Tokyo, Japan Laser Therapy 21.4: 297-303 297
REVIEW ARTICLES available at www.jstage.jst.go.jp/browse/islsm
areas of medicine and dentistry. Trials using soft laser
to prevent and control OM are difficult to compare
because many wavelengths and tools to assess mucosi-
tis were tested, and there was no protocol standardiza-
tion. Nevertheless, the Multinational Association of
Supportive Care in Cancer (MASCC) recommend the
use of soft laser to prevent OM with a level IIB in
patients undergoing high dose chemotherapy with
hematopoietic stem cell transplant (HSCT). Until last
year, scientific evidence of laser therapy in the man-
agement of OM in patients treated with other
chemotherapy and / or radiotherapy was still limited to
a level III 11).
Fig. 1: Oral mucositis grade 3 : MATERIALS AND METHODS
Step by step, the efficacy of soft laser in the manage-
ment of iatrogenic oral mucositis has been reported in
the past literature, spanning over many years of
affect local control and finally survival 5). Treatment of research, a higher level of evidence and some recom-
OM is still essentially palliative and there is no consen- mendations. We will comment on the major results
sus on any agent for prophylactic or therapeutic use, published during the last three decades. We will finally
even for oral care with mouth rinse and cryotherapy. present the ongoing first French multicentric phase III
Several topical and systemic treatments have been test- prospective double-blind randomized trial in the pre-
ed to decrease frequency and severity of OM, but only vention and treatment of oral mucositis in head and
few of them such as oral cryotherapy and palifermin 6), neck cancer patients treated with concurrent chemora-
have shown a significant preventive effect. Some 12 diation.
different interventions have yielded partly positive
results in controlled trials with varying degree of scien-
tific support, but none of them has emerged as a gold
standard 7).
Low-Level laser therapy (LLLT) is a non invasive
simple and atraumatic therapeutic management corre-
sponding to a local application of a high density
monochromatic narrow-band light source (Fig. 2). The
output power range from 5 to 200 mW with
helium/neon (632.8 nm) or diode laser with various
wavelengths (630-680, 700-830 and 900 nm). With ade-
quate energy and fluence, three main effects have
been clinically observed and reported: an analgesic
effect 8), an anti-inflammatory effect and a wound heal-
ing property 9). Various biological effects explaining
the last property has been described: an activation of
energy production in mitochondria, an increased colla-
gen production, a fibroblast cell proliferation, a detoxi-
fication of free radicals produced by the oncologic
treatments, an inhibition of NK-Kappa B and also an
angiogenesis 10). These mechanisms do not seem to be
wavelength specific in the red and infrared spectrum
but dose-dependent. No known toxicity has been
reported by in vivo studies.
Laser therapy has been investigated in various Fig. 2: Intraoral treatment with LLLT
298 E Jadaud & RJ Bensadoun
available at www.jstage.jst.go.jp/browse/islsm REVIEW ARTICLES
RESULTS transplantation 21-23). In 2004, the expert panels of the
Multinational Association of Supportive Care in Cancer
The efficiency of Laser on reducing OM has been (MASCC) and the International Society for Oral
reported thirty years ago in France, in a retrospective Oncology (ISOO) considered LLLT, after reviewing lit-
study conducted by Ciais 12). Patients were treated with erature published from 1966 to May 2002, as a possible
chemotherapy including Fluorouracil. Frequency and option in the management of OM for these patients,
severity of OM were significantly reduced by laser ther- with a level II of evidence and a grade B of recom-
apy and incidence of oral complications decreased mendation 5) . Two years later, after selecting and
from 43% to 6%. With laser therapy, the compliance for reviewing results from 2 new clinical studies, soft laser
cancer treatment was improved and all the patients was still a promising but not conclusive tool because
received their chemotherapy as originally scheduled. In of heterogeneity in laser parameters (wavelength,
1999, Bensadoun et al published the first randomized power, doses) and tools used to assess mucositis 6). In
double blind trial for patients treated by radiotherapy 2007, it became in updated data a “recommended”
for head and neck cancer. 30 patients were included, method for the prevention of OM during bone marrow
treated by radiotherapy alone and randomized transplantation or hematopoietic stem cell transplant
between a 60 mW He-Ne 632.8 nm laser and a placebo 11). By contrast, there was no specific chapter for OM
light treatment. Again, there was a significant reduction in the World Association for Laser Therapy (WALT)
of both grade 3 mucositis (7.6% versus 35.2%) and guidelines with a lack of consensus for the use of LLLT
pain (1.9% versus 23.8%), with a reduction of pain and its useful technical parameters. In 2010, a UK
relief in patients treated with active laser therapy 2). analysis using electronic searches from 1950 and
The efficacy of LLLT has been later evaluated in vari- selecting randomized controlled trials for patients
ous randomized trials over the world, for patients treat- receiving chemotherapy or radiotherapy or both, also
ed by radiotherapy alone 14-16) or by concurrent showed a significant reduction in severe mucositis
chemoradiation 17-20). when compared with a sham procedure with a RR of
During the last 2 decades, the benefit on inci- 5.28. Nevertheless, the authors concluded with a non-
dence, time and duration of OM has been confirmed in enthusiastic, weak and unreliable evidence of low level
most of randomized controlled studies published espe- laser efficacy on mucositis and suggested that further
cially for patients submitted to a high dose chemother- well designed, placebo-controlled trials were needed
apy prior to hematopoietic stem cell or bone marrow to improve this level of evidence 24).
Day 33
Day 35
(end of RT)
8 day after
the end of RT
Fig. 3: Healed oral mucositis after LLLT treatment
Low-level laser in the management of oral induced mucositis 299
REVIEW ARTICLES available at www.jstage.jst.go.jp/browse/islsm
A next step to achieve this goal has been made moderate to strong evidence in favour of laser when
last year with the publication a systematic review of lit- applied with optimal dose (1-6 J per point), both in
erature. It was the first meta-analysis on this topic 1). prevention, reduction of severity and duration of OM
The objectives were to analyse the prophylactic and than on pain.
therapeutic effect of LLLT on OM, and to identify the
effect of different technical parameters like power, DISCUSSION
dose, wavelength, time of treatment, and finally to
point out some devices and a possible procedure. 11 Can we point out a gold standard for laser therapy in
randomized placebo-control trials published between Oral mucositis? On the basis of randomized trials
1997 and 2009 for a total of 415 patients were selected results and this meta-analysis, recommendations for
according to the exclusion / inclusion procedure cho- LLLT parameters in prophylactic and therapeutic use
sen. Methodological quality was high with a mean have been recently proposed by Bensadoun and Nair
score of 4.10 on a 5-point Jadad scale. 25), remaining that not less than 2J/cm2 for prophylac-
When LLLT started before OM ulcers occurred, tic and 4J/cm2 for therapeutic intents should be used
there was a significant preventive effect of LLLT with a with a red wavelength. In practice, treatment point per
relative risk at 2.03 less (95% confidence interval: 1.11- point with at least 1cm 2 during 20 sec or 40 sec
3.69) for OM occurrence and p = 0.02. One trial using depending on the aim, should be applied. Also, laser
a very low dose of 0.18J/cm2 and short time of treat- therapy should be used daily during RT and other days
ment was source of significant heterogeneity. But, after until ulcer resolution with a minimum of three times a
sub-grouping trials with doses above or over 1J/cm2, week (table 1).
heterogeneity disappeared and Risk Ratio for prevent- These recommendations have been mostly
ing OM increased to 2.72 with a narrow confidence applied in a Brazilian phase III double-blind placebo-
interval (95% CI: 19.8-3.74). LLLT reduced significantly controlled trial presented during the ASCO annual
in five studies the duration of OM grade 2 or worse meeting in 2011 17). The purpose was to examine the
with 4.38 days less than with placebo (p =0.0004, 95% effectiveness of laser therapy on Oral Mucositis and
CI: 3.35-5.40). Mucositis severity was analysed on a outcomes like pain, dysphagia, quality of life, in 94
Standardized Mean Difference (SMD) because of het- head and neck cancer patients submitted to concurrent
erogeneity in index scales used. The combined SMD chemoradiation. The majority of patients were treated
effect size was 1.33 (95% CI: 0.68-1.98) which corre- for an oropharyngeal tumor, with a conventional radia-
spond to a very good effect (Fig. 3). What was the tion and a concurrent cisplatin every 3 weeks. Main
effect of Wavelengh? A subgroup analysis revealed no endpoints were OM incidence and severity, pain inten-
heterogeneity between trials for the red (630-670 nm) sity and RT interruptions. A crossover was used for
and the infrared (780-830 nm) subgroups respectively patients in placebo-arm presented a grade 3 mucositis
(p>0.21) and there were no significant wavelength dif- and/or a giant ulcer. In this particular case, LLLT densi-
ferences in relative risks of OM between red at 2.72 ty energy was double from 4J/cm2 to 8J/cm2. Laser was
and infrared at 3.48. But a further analysis of wave- used daily during the chemoradiation with a punctual
length-specific doses revealed that a dose of 2J/cm2 or form and 10 seconds per point, which is shorter than
less with infrared light was ineffective in reducing time of treatment recommended by Bensadoun.
mucositis severity (SMD = 0.38; 95% CI: 0.19-0.96), Nevertheless, the incidence of grade ¾ OM was 6.4 %
whereas, a dose of 6J/ cm2 for both red and infrared in the LLLT arm versus 48% in the placebo arm which
wavelengths was highly effective, increasing SMD is highly significant (HR = 0.13 and p< 0.001). The inci-
effect at 2.17 (95% CI 1.48-2.86). dence of ulcer was also lower with active laser with
Analysis of pain intensity was performed in 4 tri- 17% versus 51% (p<0.001). Beside this benefits, pain
als using different scales. The combined analysis was less severe in patients treated with active laser
revealed a significant effect in favour of LLLT with an (p=0.012), with less used narcotic analgesic (HR = 0.33,
SMD at 1.22(95% CI 0.19-2.25) but also with hetero- p<0.001), feeding tube insertion or gastrostomy (HR =
geneity caused by one trial. 0.037, p= 0.005). No patients in this study had RT or
All trials reported possible side effects but none CT interruption due to OM but almost half patients of
of them found a difference between active laser treat- the placebo group used the cross over.
ment and placebo. Most of papers also reported that Finally, many points of quality of life, like physi-
laser was very well tolerated by patients. cal and emotional functioning (p=0.037), pain
In conclusion, this first meta-analysis showed a (p=0.043), swallowing (p=0.001) and fatigue (p=0.011),
300 E Jadaud & RJ Bensadoun
available at www.jstage.jst.go.jp/browse/islsm REVIEW ARTICLES
were significantly improved by laser therapy. In con- opiod analgesic use.
clusion, the authors suggested that LLLT should be a According to last Bensadoun’s recommendations,
new standard of care in this setting. a national multicentric phase III trial, double-blind with
Recently, the largest sample study on this topic placebo controlled, started in France in 2009. This
has been submitted to publication 20). It was a triple study is coordinated by the west oncologic institute
blinded randomized trial for 221 patients treated with a Paul Papin (ICO Paul papin) and funded by a national
conventional radiotherapy (66 Gy, 33 fractions, 5 frac- public grant (PHRC 2008). The objective is to evaluate
tions/week) and cisplatin every three weeks. Power the effectiveness of a 100 mW and 660 nm diode laser
density and dosage were both low (24 mW and 3 on OM in advanced head and neck patients treated
J/point with a 1 cm2 spot size). LLLT was used every with concurrent chemoradiotherapy, with or without
day prior to radiation. The incidence of severe mucosi- surgery. RT is delivered with a conformational or IMRT
tis (grade > 2) was significantly reduced with laser technique. Chemotherapy is a 5FU-CDDP protocol, or
(23.4% vs 70%). Pain and dysphagia were also signifi- CDDP alone or Cetuximab, according to the exclusive
cantly improved by LLLT with a significant reduction in or post-operative statement and to the co-morbidities
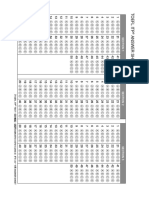
Table 1: recommendations for low-level laser therapy (intraoral applicators only) in prophylaxis and curative
treatment of oral mucositis : from Bensadoun RJ, Nair RG in Curr Opin Oncol, 24(4): 363-70
Low-level laser in the management of oral induced mucositis 301
REVIEW ARTICLES available at www.jstage.jst.go.jp/browse/islsm
of the patient. ing targeted therapy like cetuximab.
Main endpoint is grade 3-4 OM incidence and
secondary endpoints are the impact on nutrition, quali- CONCLUSIONS
ty of life, treatment interruptions, DFS, OS and laser
toxicity. In summary, low level laser therapy represents more
Laser is used daily when mucositis becomes than a promising agent to prevent or treat cancer–ther-
greater than grade 1 and is interrupted when OM apy induced OM. With diode and new technologies,
becomes less severe than grade 2. This schedule has laser is now less time-consuming and extraoral applica-
been chosen to be less time-consuming as possible to tors with specific wavelength could be helpful to treat
respect medical limited availability, and because severe other sites of mucositis and skin toxicities. Also it may
and not moderate mucositis is in our opinion the main be used by trained paramedical staff like nurses who
target. can complete clinician contribution. We can now use
Among almost 15 French centers using soft laser, published recommendations for soft laser parameters.
7 are now opened for this study and 44 patients have This is important for different clinician communities
been enrolled over a hundred patients planned. This that are concerned with oral mucositis and for the
study could be a new key stone to evaluate the effica- homogeneity of laser procedure in future trials.
cy of laser therapy on oral induced mucositis but new According to the MASCC criteria, and the results
studies are needed to evaluate new laser technologies of the meta-analysis, LLLT could be soon proposed
than can treat with different wavelengths not even with a level I of evidence, as a possible new standard
pharyngeal mucositis which is actually not treated but of care in respect to the last recommendations pub-
also cutaneous toxicities, especially in patients receiv- lished if intraoral application is performed.
REFERENCES
1: Bjordal JM, Bensadoun RJ, Tunèr J, Frigo L, 6: Worthington HV, Clarkson JE, Eden OB (2007):
Gjerde K, Lopes-Martins RA (2011): A systematic Interventions for preventing oral mucositis for
review with meta-analysis of the effect of low-level patients with cancer receiving treatment. Cochrane
laser therapy (LLLT) in cancer therapy-induced oral Database Syst Rev,17(4): CD000978
mucositis. Support Care Cancer, 19(8):1069-77 7: Treister N, Sonis S (2007): Mucositis: biology and
2: Bensadoun RJ, Franquin JC, Ciais G, et al (1999). management. Curr opin Otolaryngol Head Neck
Low-energy He/Ne laser in the prevention of Surg, 15(2):123-9
radio-induced mucositis. A multicenter phase III 8: Jang H, Lee H (2012). Meta-analysis of pain relief
randomized study in patients with head and neck effects by laser irradiation on joint areas:
cancer. Support Care Cancer, 7(4): 244-252 Photomed Laser Surg, 30(8):405-17
3: Caillot E, Denis F (2012): Mucites radio-induites 9: De Paula Eduardo C, de Freitas PM, Esteves-
buccopharyngées: actualités sur la prise en charge. Oliveira M, Aranha AC, Ramalho KM, Simoes A et
Cancer/radiotherapie, 16 : 358-363 al (2010): Laser phototherapy in the treatment of
4: Elting LS, Keefe DM, Sonis ST, Garden AS, periodontal disease. A review. Lasers med Sci,
Spijjkervet FK, Barasch A et al (2008): Patient- 25(6):781-92
reported measurements of oral mucositis in head 10: Corazza AV, Jorge J, Kurachi C, Bagnato VS
and neck cancer patients treated with radiotherapy (2007): Photobiomodulation on the angiogenesis of
with or without chemotherapy: demonstration of skin wounds in rats using different light sources.
increased frequency, severity, resistance to pallia- Photomed Laser Surg, 25(2):102-6
tion, and impact on quality of life. Cancer, 15; 11: Keefe DM, Shubert MM, Elting LS, Sonis ST,
113(10): 2704-13 Epstein JB, Raber-Durlacher JE et al (2007):
5: Rubenstein EB, Peterson DE, SchubertM, Keefe D, Updated clinical practice guidelines for the preven-
McGuire D, Epstein J et al (2004): Mucositis Study tion and treatment of mucositis. Cancer,
section of the Multinational Association for 1;109(5):820-31
Supportive Care in Cancer; International Society for 12: Ciais G, Namer M, Schneider M, Demard F,
Oral Oncology. Cancer, 1;100(9 suppl): 2026-46 Pourreau-Schneider N, Martin PM et al (1992):
302 E Jadaud & RJ Bensadoun
available at www.jstage.jst.go.jp/browse/islsm REVIEW ARTICLES
Laser therapy in the prevention and treatment of level infrared laser therapy for chemo-or radiother-
mucositis caused by anticancer chemotherapy. Bull apy-induced oral mucositis: a randomized, place-
Cancer, 79(2): 183-91 bo-controlled study. J Oral Laser Appl, 7:175-81
13: Migliorati CA, Oberle-Edwards L, Schubert M 20: Gautam AP, Fernandes DJ, Vidyasager MS, Maiya
(2006): The role of alternative and natural agents, AG, Vadhiraja BJ (2012): Low level laser therapy
cryotherapy, and/or laser for management of ali- for concurrent chemoradiotherapy induced oral
mentary mucositis. Support care cancer, 14(6): 533- mucositis in head and neck cancer patients. A
40 triple blinded randomized controlled trial.
14: Maiya AG, Sagar MS, Fernandes DJ (2006): Effect Radiother Oncol Aug 9 (Epub ahead of print)
of low helium-neon(He-Ne) laser therapy in the 21: Cowen D, Tardieu C, Schubert M et al (1997): Low
prevention and treatment of radiation induced energy helium-neon laser in the prevention of oral
mucositis in head and neck cancer patients. Indian mucositis in patients undergoing bone marrow
J Res, 124: 399-402 transplant : results of a double blind randomized
15: Arora H, Pai KM, Maiya A, Vidyasagar MS, Rajeev trial. Int J Radiat Oncol Biol Phys, 38: 697-703
A (2008): Efficacy of He-Ne laser in the prevention 22: Antunes HS, de Azevedo AM, da Silva Bouzas LF
and treatment of radiotherapy-induced oral et al (2007): Low-power laser in the prevention of
mucositis in oral cancer patients. Oral Surg Oral induced oral mucositis in bone marrow transplan-
Med Oral Pathol Oral Radiol Endod, 105(2):180-6 tation patients: a randomized trial. Blood, 109:
16: Kuhn A, Heinzmann G, da Silva CA et al (2008): 2250-5
Low-level infrared laser therapy to prevent radio- 23: Schubert MM, Eduardo FP, Guthrie KA et al
therapy-induced oral mucositis: a randomized (2007): A phase III randomized double blind place-
placebo-controlled study. J Oral laser Appl, 8:219- bo-controlled clinical trial to determine the efficacy
24 of low level laser therapy for the prevention of
17: Antunes HS, Herchenhorm D, Araujo CM, Cabral oral mucositis in patients undergoing hematopoiet-
R, Ferreira EM, Small A et al (2011): Phase III trial ic cell transplantation. Support care Cancer, 15:
of low-level laser therapy to prevent induced oral 1145-54
mucitis in head and neck cancer patients submitted 24: Clarkson JE, Worthington HV, Furness S, McCabe
to concurrent chemoradiation. J Clin Oncol 29 M, Khalid T, Meyer S (2010): Interventions for
suppl abstr LBA5524 treating oral mucositis for patients with receiving
18: Lima AG, Villar RC, de Castro GJ, Antequera R, Gil treatment. Cochrane Database Syst rev, Aug 4(8):
E, Rosalmeida MC et al (2011): Oral mucositis pre- CD001973
vention by low-level laser therapy in head and 25: Bensadoun RJ, Nair RG (2012): Low-level laser
neck cancer patients undergoing concurrent therapy in the prevention and treatment of cancer
chemoradiotherapy: a phase III randomized study. therapy-induced mucositis: 2012 state of the art
Int J Radiat Oncol Biol Phys, 82: 270-5 based on literature review and meta-analysis. Curr
19: Kuhn A, Vacaro G, Almeida D et al (2007): Low- Opin Oncol, 24(4): 363-70
[Acknowledgement]
The authors would like to thank:
Brigitte Lemarquand, scientific information officer, ICO Paul Papin
Dr Virginie Berger PhD, team manager and clinical research ICO Paul Papin
There are no conflicts of interest.
Low-level laser in the management of oral induced mucositis 303
You might also like
- Clinical Applications of Nuclear Medicine Targeted TherapyFrom EverandClinical Applications of Nuclear Medicine Targeted TherapyEmilio BombardieriNo ratings yet
- 1 s2.0 S1368837519304348 MainDocument8 pages1 s2.0 S1368837519304348 Mainanaperezred11No ratings yet
- Genot-Klastersky2020 Article RetrospectiveEvaluationOfTheSaDocument8 pagesGenot-Klastersky2020 Article RetrospectiveEvaluationOfTheSaLarisssaa FerreiraNo ratings yet
- 1 s2.0 S0196070923000819 MainDocument6 pages1 s2.0 S0196070923000819 MainRALF KEVIN PIANONo ratings yet
- Photodynamic Therapy: APRIL 2006Document9 pagesPhotodynamic Therapy: APRIL 2006Joanna Michelle FERNANDEZNo ratings yet
- Mucosal NekrosisDocument2 pagesMucosal NekrosisYeni PuspitasariNo ratings yet
- Update On Radiotherapy in Gynaecological Malignancies: ReviewDocument8 pagesUpdate On Radiotherapy in Gynaecological Malignancies: ReviewDesrha TangdiseruNo ratings yet
- Bmri2018 3982540Document10 pagesBmri2018 3982540paola lievanoNo ratings yet
- 1-s2.0-S1040842821001232-mainDocument9 pages1-s2.0-S1040842821001232-mainoanaNo ratings yet
- Dermatology Research and Therapy: Radiotherapy For Mycosis Fungoides: Review of The LiteratureDocument5 pagesDermatology Research and Therapy: Radiotherapy For Mycosis Fungoides: Review of The LiteratureLevaszkaNo ratings yet
- MASCC RadiodermiteDocument17 pagesMASCC RadiodermiteDora FerreiraNo ratings yet
- Lasers in PerioDocument14 pagesLasers in Periodhwanit31No ratings yet
- Laser Phototherapy As A Treatment For Radiotherapy-Induced Oral MucositisDocument4 pagesLaser Phototherapy As A Treatment For Radiotherapy-Induced Oral Mucositis5h4d0w89No ratings yet
- International Journal of Scientific Research: Dental ScienceDocument3 pagesInternational Journal of Scientific Research: Dental ScienceCyrish MelchorNo ratings yet
- Laser treatment reduces periodontal pathogens more than SRPDocument10 pagesLaser treatment reduces periodontal pathogens more than SRPeliasNo ratings yet
- Lacrima Ca CTRTDocument7 pagesLacrima Ca CTRTDrDeepak MittalNo ratings yet
- Photobiomodulation Therapy in The Treatment of Oral Mucositis, Dysphagia, Oral Dryness, Taste Alteration, and Burning Mouth Sensation Due To Cancer Therapy: A Case SeriesDocument11 pagesPhotobiomodulation Therapy in The Treatment of Oral Mucositis, Dysphagia, Oral Dryness, Taste Alteration, and Burning Mouth Sensation Due To Cancer Therapy: A Case SeriesRomian ValenciaNo ratings yet
- Moretto 2014Document8 pagesMoretto 2014Silvie WidyaNo ratings yet
- Use of Therapeutic Laser For Prevention and Treatment of Oral MucositisDocument6 pagesUse of Therapeutic Laser For Prevention and Treatment of Oral Mucositishendra ardiantoNo ratings yet
- Phtobiomodulation Laser ProtocolsDocument22 pagesPhtobiomodulation Laser ProtocolsIana RusuNo ratings yet
- Treatment Results For Patients With Squamous-Cell Carcinoma of The Anus, A Single Institution Retrospective AnalysisDocument10 pagesTreatment Results For Patients With Squamous-Cell Carcinoma of The Anus, A Single Institution Retrospective AnalysisJENIFER KARINA PUTZ LORENZINo ratings yet
- Low Level Laser Therapy in Oral Mucositis PDFDocument7 pagesLow Level Laser Therapy in Oral Mucositis PDFEduardo Garza GarzaNo ratings yet
- File 712 20230127155855Document9 pagesFile 712 20230127155855Nakarit SangsirinawinNo ratings yet
- Rru 093Document10 pagesRru 093maria fernanda torrichelliNo ratings yet
- Principles of chemotherapy and radiotherapy for gynaecological cancersDocument7 pagesPrinciples of chemotherapy and radiotherapy for gynaecological cancersNora100% (3)
- ToxicityDocument18 pagesToxicityAbraham OsunaNo ratings yet
- Ji-Hye Park2019Document9 pagesJi-Hye Park2019Naiadja Santana CerqueiraNo ratings yet
- Journal Pre-Proof: Acta Pharmaceutica Sinica BDocument62 pagesJournal Pre-Proof: Acta Pharmaceutica Sinica BJUAN DIEGO TRUJILLO ROJASNo ratings yet
- Role For Radiation Therapy in MelanomaDocument13 pagesRole For Radiation Therapy in MelanomaHendry HuangNo ratings yet
- Topic Treatment Acne Scars1Document3 pagesTopic Treatment Acne Scars1Stanca NicolaeNo ratings yet
- Hypofractionation in The Real World Rodin 2021Document8 pagesHypofractionation in The Real World Rodin 2021Gloribel BolívarNo ratings yet
- Local Management of NeutropenicDocument3 pagesLocal Management of NeutropenicCláudia Carrara CotomácioNo ratings yet
- Chemotherapy For Head and Neck CancerDocument8 pagesChemotherapy For Head and Neck CancerJames ParkerNo ratings yet
- Cancers 13 04912Document12 pagesCancers 13 04912mirzaNo ratings yet
- Role of Radiation Oncology in Modern Multidisciplinary Cancer Treatment - PMCDocument20 pagesRole of Radiation Oncology in Modern Multidisciplinary Cancer Treatment - PMCRalf Kevin Piano,RMTNo ratings yet
- 1 s2.0 S0959804922002787 MainDocument17 pages1 s2.0 S0959804922002787 MainFNo ratings yet
- Oral Cancer Prevention Potter LodiDocument8 pagesOral Cancer Prevention Potter LodiMoni Abraham KuriakoseNo ratings yet
- Photo-Biomodulation in EndodonticsDocument7 pagesPhoto-Biomodulation in EndodonticsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Censabella 2016Document9 pagesCensabella 2016Naiadja Santana CerqueiraNo ratings yet
- 68 213 2 PBDocument3 pages68 213 2 PBAly OsmanNo ratings yet
- Systemic Therapy in The Curative Treatment of Head and Neck Squamous Cell Cancer: A Systematic ReviewDocument11 pagesSystemic Therapy in The Curative Treatment of Head and Neck Squamous Cell Cancer: A Systematic ReviewLorena Sánchez PérezNo ratings yet
- Treatment of Xanthelasma Palpebrarum by Fractional Carbon Dioxide LaserDocument1 pageTreatment of Xanthelasma Palpebrarum by Fractional Carbon Dioxide LaserАркадий ЖивицаNo ratings yet
- Thoracic Re Irradiation With 3D Conformal or More Advanced - 2021 - Critical ReDocument11 pagesThoracic Re Irradiation With 3D Conformal or More Advanced - 2021 - Critical Renurain fasihahNo ratings yet
- Pi Is 0936655522005015Document8 pagesPi Is 0936655522005015Raul Matute MartinNo ratings yet
- Low-level light therapy effective for diabetic foot ulcersDocument9 pagesLow-level light therapy effective for diabetic foot ulcersErviana Anggi PuteriNo ratings yet
- 2021 MO Laser CCEODocument8 pages2021 MO Laser CCEOAndressa A.No ratings yet
- Jensen Et Al-2014-Journal of Oral Pathology & Medicine PDFDocument10 pagesJensen Et Al-2014-Journal of Oral Pathology & Medicine PDFMega MalyndaNo ratings yet
- Lasers: High Power Laser and Photobiomodulation in Oral Surgery: Case ReportDocument5 pagesLasers: High Power Laser and Photobiomodulation in Oral Surgery: Case ReportLeyla Huamán FrancoNo ratings yet
- 5 ArtigosDocument4 pages5 ArtigosAmanda AiresNo ratings yet
- Ead and Eck Ancer: RADPLAT: An Alternative To Surgery?Document12 pagesEad and Eck Ancer: RADPLAT: An Alternative To Surgery?Manikanta Sai KumarNo ratings yet
- Neuro-Oncology: The Cost-Effectiveness of Tumor-Treating Fields Therapy in Patients With Newly Diagnosed GlioblastomaDocument8 pagesNeuro-Oncology: The Cost-Effectiveness of Tumor-Treating Fields Therapy in Patients With Newly Diagnosed GlioblastomaLuis LiraNo ratings yet
- Dentistry at Best RationaleDocument2 pagesDentistry at Best RationaleObamaNo ratings yet
- 4451 FullDocument4 pages4451 FullSukhvinder Singh RanaNo ratings yet
- Comparison Between Antimicrobial Photodynamic Therapy and Low-Level Laser Therapy On Non-Surgical Periodontal Treatment A Clinical StudyDocument6 pagesComparison Between Antimicrobial Photodynamic Therapy and Low-Level Laser Therapy On Non-Surgical Periodontal Treatment A Clinical StudyFelipe AraujoNo ratings yet
- 904nm 0.6W - 12663 - 2013 - Article - 544Document7 pages904nm 0.6W - 12663 - 2013 - Article - 544Gino DammiuncrodinoNo ratings yet
- Out PDFDocument18 pagesOut PDFRaraNo ratings yet
- CANCER ch14 Radiation TherapyDocument16 pagesCANCER ch14 Radiation TherapysherlyNo ratings yet
- Pi Is 1879850016300947Document7 pagesPi Is 1879850016300947Daniela GordeaNo ratings yet
- J Radonc 2012 08 013Document8 pagesJ Radonc 2012 08 013AnharNo ratings yet
- Adjuvant Therapies For MRONJ - Systematic ReviewDocument40 pagesAdjuvant Therapies For MRONJ - Systematic ReviewVanessa DíazNo ratings yet
- Engaging HIV Positive Clients in CareDocument9 pagesEngaging HIV Positive Clients in CareEduardo Garza GarzaNo ratings yet
- The Matrix Model in Outpatiens Substances AbuseDocument9 pagesThe Matrix Model in Outpatiens Substances AbuseEduardo Garza GarzaNo ratings yet
- Blood-Based Circulating microRNAs As Potential Biomarkers For Predicting The Prognosis of Head and Neck Cancer-A Systematic ReviewDocument9 pagesBlood-Based Circulating microRNAs As Potential Biomarkers For Predicting The Prognosis of Head and Neck Cancer-A Systematic ReviewEduardo Garza GarzaNo ratings yet
- Investigations of Radicular Dentin Permeability and Ultrastructural Changes After Irradiation With ErCrYSGG Laser and Dual Wavelength 2780 and 940 NM LaserDocument7 pagesInvestigations of Radicular Dentin Permeability and Ultrastructural Changes After Irradiation With ErCrYSGG Laser and Dual Wavelength 2780 and 940 NM LaserEduardo Garza GarzaNo ratings yet
- Investigations of Radicular Dentin Permeability and Ultrastructural Changes After Irradiation With ErCrYSGG Laser and Dual Wavelength 2780 and 940 NM LaserDocument7 pagesInvestigations of Radicular Dentin Permeability and Ultrastructural Changes After Irradiation With ErCrYSGG Laser and Dual Wavelength 2780 and 940 NM LaserEduardo Garza GarzaNo ratings yet
- The Matrix Model in Outpatiens Substances AbuseDocument9 pagesThe Matrix Model in Outpatiens Substances AbuseEduardo Garza GarzaNo ratings yet
- Low Level Laser Therapy in Oral Mucositis PDFDocument7 pagesLow Level Laser Therapy in Oral Mucositis PDFEduardo Garza GarzaNo ratings yet
- Low Level Laser Therapy - A Standard of Supportive Care For CancerDocument7 pagesLow Level Laser Therapy - A Standard of Supportive Care For CancerEduardo Garza GarzaNo ratings yet
- Applications of Gold Nanoparticles in ELISA, PCR, and immuno-PCR AssaysDocument17 pagesApplications of Gold Nanoparticles in ELISA, PCR, and immuno-PCR AssaysEduardo Garza GarzaNo ratings yet
- The Efficacy of Radachlorin-Mediated Photodynamic TherapyDocument26 pagesThe Efficacy of Radachlorin-Mediated Photodynamic TherapyEduardo Garza GarzaNo ratings yet
- Laser Therapy and Photosensitive MedicationDocument4 pagesLaser Therapy and Photosensitive MedicationEduardo Garza GarzaNo ratings yet
- Ultrasonography-Guided Arthrocentesis Versus ConventionalDocument10 pagesUltrasonography-Guided Arthrocentesis Versus ConventionalEduardo Garza GarzaNo ratings yet
- Antitumor Immunity Induced by Laser Immunotherapy and Its Adoptive TransferDocument4 pagesAntitumor Immunity Induced by Laser Immunotherapy and Its Adoptive TransferEduardo Garza GarzaNo ratings yet
- Laser Interstitial Thermal Therapy After RadiosurgeryDocument28 pagesLaser Interstitial Thermal Therapy After RadiosurgeryEduardo Garza GarzaNo ratings yet
- Combination of Photodynamic Therapy + Immunotherapy + ChemotherapyDocument5 pagesCombination of Photodynamic Therapy + Immunotherapy + ChemotherapyEduardo Garza GarzaNo ratings yet
- Low Level Laser Therapy in Oral MucositisDocument7 pagesLow Level Laser Therapy in Oral MucositisEduardo Garza GarzaNo ratings yet
- Hoja de Respuestas PDFDocument1 pageHoja de Respuestas PDFEduardo Garza GarzaNo ratings yet
- Antitumor Immunity Induced by Laser Immunotherapy and Its Adoptive TransferDocument4 pagesAntitumor Immunity Induced by Laser Immunotherapy and Its Adoptive TransferEduardo Garza GarzaNo ratings yet
- Application of Laser in Oral SurgeryDocument11 pagesApplication of Laser in Oral SurgeryEduardo Garza GarzaNo ratings yet
- Laser Interstitial Thermal Therapy After RadiosurgeryDocument28 pagesLaser Interstitial Thermal Therapy After RadiosurgeryEduardo Garza GarzaNo ratings yet
- Laser Therapy and Photosensitive MedicationDocument4 pagesLaser Therapy and Photosensitive MedicationEduardo Garza GarzaNo ratings yet
- Exploratory Factor Analysis PDFDocument14 pagesExploratory Factor Analysis PDFhadiyudhaNo ratings yet
- Application of Laser in Oral SurgeryDocument11 pagesApplication of Laser in Oral SurgeryEduardo Garza GarzaNo ratings yet
- Bacterial Invasion of Epithelial Cells and Spreading in Periodontal TissueDocument16 pagesBacterial Invasion of Epithelial Cells and Spreading in Periodontal TissueEduardo Garza GarzaNo ratings yet
- Day 4Document3 pagesDay 4Elizer Tabil TabugaderNo ratings yet
- SPECPRODocument92 pagesSPECPROapril75No ratings yet
- International UFO Reporter v30Document120 pagesInternational UFO Reporter v30DirkTheDaring11100% (2)
- Introduction To The Principles of Laboratory MedicineDocument19 pagesIntroduction To The Principles of Laboratory Medicinedanielle kaye arangoteNo ratings yet
- Basic English Reviewer 1Document3 pagesBasic English Reviewer 1Odnarf LeahcimNo ratings yet
- Amul SpssDocument41 pagesAmul Spssshikhahota2012No ratings yet
- Fallacy of CompositionDocument3 pagesFallacy of CompositionKen ManeboNo ratings yet
- Understanding the Lexical Field TheoryDocument2 pagesUnderstanding the Lexical Field Theoryfarah zaheer100% (1)
- Workforce Plan 20xx-20xxDocument22 pagesWorkforce Plan 20xx-20xxRani EndarweniNo ratings yet
- Group 1 Math 100L Hqt2 HWDocument5 pagesGroup 1 Math 100L Hqt2 HWAmelie HernandezNo ratings yet
- Constitutional Validity of Citizenship Amendment Act 2019Document3 pagesConstitutional Validity of Citizenship Amendment Act 2019Pratibha DixitNo ratings yet
- One Foot in The Grave - Copy For PlayersDocument76 pagesOne Foot in The Grave - Copy For Playerssveni meierNo ratings yet
- On MCH and Maternal Health in BangladeshDocument46 pagesOn MCH and Maternal Health in BangladeshTanni ChowdhuryNo ratings yet
- 0607 s14 Ms 43Document6 pages0607 s14 Ms 43wizard guyNo ratings yet
- Iowa Board of Regents Settlement Agreement 3Document108 pagesIowa Board of Regents Settlement Agreement 3kcrgdotcomNo ratings yet
- Literature Review 1Document10 pagesLiterature Review 1FahimAnwar100% (1)
- Engineering Prob & Stat Lecture Notes 6Document12 pagesEngineering Prob & Stat Lecture Notes 6EICQ/00154/2020 SAMUEL MWANGI RUKWARONo ratings yet
- DSC MatDocument41 pagesDSC MatRamuCivilNo ratings yet
- Scientific Theological Aspects of GeocentricityDocument222 pagesScientific Theological Aspects of GeocentricityAdi Dumitru100% (1)
- Flying Creatures ZoologyDocument29 pagesFlying Creatures ZoologyJamie Parker SnufferNo ratings yet
- A Literature Survey On The Accuracy of Software Effort Estimation ModelsDocument6 pagesA Literature Survey On The Accuracy of Software Effort Estimation Modelsutkarsh sharmaNo ratings yet
- MUET Reading Task - Print OutDocument5 pagesMUET Reading Task - Print Out萱儿林No ratings yet
- Bibliography Against Sex Differences in The BrainDocument5 pagesBibliography Against Sex Differences in The Brainalanmoore2000No ratings yet
- DECA RolePlayDocument6 pagesDECA RolePlayAftab MohammedNo ratings yet
- ElectrodynamicsDocument4 pagesElectrodynamicsHarold Favian Diaz LeonisNo ratings yet
- Concept of Professional Ethics and BioethicsDocument21 pagesConcept of Professional Ethics and BioethicsTina TalmadgeNo ratings yet
- 2021 BTCI FASTING PREPARATION (Part 1) - 2Document2 pages2021 BTCI FASTING PREPARATION (Part 1) - 2Andrew HunterNo ratings yet
- ĐỀ 15Document7 pagesĐỀ 15DistressNo ratings yet
- Position and Powers of Karta in Hindu LawDocument11 pagesPosition and Powers of Karta in Hindu LawAniket SachanNo ratings yet
- MGT301 - Assignment - GROUP ADocument31 pagesMGT301 - Assignment - GROUP ARahim HossainNo ratings yet