Professional Documents
Culture Documents
Evidence Statement Anal Incontinence Flowchart PDF
Uploaded by
silkofosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Evidence Statement Anal Incontinence Flowchart PDF
Uploaded by
silkofosCopyright:
Available Formats
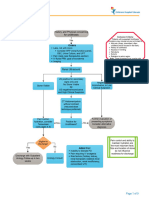
KNGF Evidence Statement Royal Dutch Society for Physical Therapy
Anal incontinence
Methodical approach Red flags*
• (recent) trauma
• pre-existing (unexplained) fever
Direct Access to Physical Therapy • recent unexplained weight loss (> 5 kg/month)
recommendation: contact family • prolonged use of corticosteroids
physician/specialist (with patient’s permission) • constant pain that does not decrease at rest or after changing position
• history of cancer
• general malaise
• nocturnal pain
Referral • extensive neurological signs and symptoms
• inability to urinate/defecate
• blood and mucus in stools
• pain during defecation
• acute loss of stools
• abnormal color of stools not related to food consumed
• brief anemia episode
* Attention to red flags is required throughout the diagnostic and therapeutic process for physical
therapy.
(Supplementary) history • reason for contact and patient’s presenting problem
• nature (underlying cause/condition) and severity of anal incontinence (in ICF terms) and
modifiability (impeding factors, general and local)
• proctological, gynecological, obstetrical, urological and sexological history in relation to the
musculoskeletal system
• comorbidity
• coping strategies
• psychosocial problems
• defecation and micturition patterns
• nutrient and fluid intake
• status of components of continence system (muscle function, reservoir function, consistency of
stools, awareness and acknowledgment of health problem; interactions between these)
• patient’s pattern of expectations
Physical examination General inspection
• inspecting breathing, spinal column, pelvis, hips, gait analysis
Local inspection of vagina/anus/perineum
• inspecting pelvic floor at rest (introitus, perineum, vagina, anus)
• inspecting pelvic floor during contraction (contraction strength, performance, co-contractions and
breathing)
• inspecting pelvic floor during coughing
• inspecting pelvic floor during straining
Supplementary functional examination
• palpation at rest, anorectal
• palpation during contraction, anorectal
• palpation during straining, Valsalva, coughing (involuntary) rectal
• rectal balloon and electromyography
Measurement instruments
• Wexner score
• Global Perceived Effect
• defecation diary
Physical therapy analysis/diagnosis identification of impairments (nature, severity), limitations and participation restrictions
(consequences of anal incontinence)
V-25/2013 The full-text Evidence Statement is available from www.fysionet-evidencebased.nl © KNGF
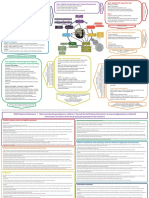
KNGF Evidence Statement Royal Dutch Society for Physical Therapy
Anal incontinence
Identification of problem category:
I, II, III en IV
Treatment plan for patients with anal incontinence
I-II
anal incontinence with pelvic floor dysfunction III IV
anal incontinence anal incontinence (I/II/III) + general
I II without pelvic floor factors impeding recovery or adjustment
with awareness of loss of stools (urgency): without awareness of loss of stools dysfunction processes
external anal sphincter + m. puborectalis/levator ani (passive): internal anal sphincter
neurological problema neurological problemb
yes (local/central) yes (local/central)
no no
anorectal sensation normal anorectal sensation abnormal
3rd/4th degree tear peripheral dysfunction
traumas spinal cord S2-S4
IA IB IC ID IIA IIB III IVA IVB
• without voluntary • without • with voluntary • plus negative anorectal sensation anorectal sensation • reduced rectal without with comorbidities
control of pelvic involuntary control of pelvic effects on pelvic normal abnormal capacity comorbidity • increased
floorc control of pelvic floorc floor muscle • 3rd/4th degree • peripheral • intestinal • diet sensitivity
Disorder floor function from tear dysfunction system function • medication for (chronic fatigue,
respiratory • traumas • spinal cord S2-S4 problemse constipation chronic stress,
problems, • overflow diarrhea • pelvic organ • fecal consistency (incl. difficulty
musculoskeletal • paradoxical prolapse (POP)d • soiling antimuscarinic concentrating)
problems and/or straining • loss of drugs M3/ • neurological,
toileting posture, discrimination M4), diarrhea, urological,
regime and/or between flatus sensitivity, gynecological,
behavior and feces cognition, muscle endocrinological,
relaxants psychological
and cognitive
problems
• connective tissue
diseases
• chronic
obstructive
pulmonary
disease (COPD)
• morbid obesity
• eating disorders
• panic/anxiety/
psychosis
• functional
problems relating
to toileting
improving components of continence :
1. muscle function: basic activity, timing, coordination, relaxation, duration, reflex activity (fast-twitch/slow-twitch)
2. reservoir function (perception of filling sensation): first sensation, first feeling of urgency, maximum tolerable volume, appropriate reaction of pelvic floor to rectal filling (= being continent)
Goal
3. fecal consistency: from loose to soft shapeds
4. recognition of health problem, acknowledgement of health problem, expression (uttering, setting in motion) and letting go*
5. interaction between the above continence components
Strategy optimizing one continence component → optimizing the complex mechanism of continence components → making ADL tasks become automatic
Therapy providing education and advice
IA IB IC ID IIA IIB III IVA IVB
• verbal instruction • training to reduce • PFMT • exercises • PFMT • PFMT • PFMT • addressing • addressing
• ES for PFMT (m. anorectal angle to address impeding factors impeding factors
puborectalis / • training pelvic • BFf unfavorable • BFf • BFf Note: complete where possible where possible
external anal floor during trunk factors recovery unlikely • informing patient • informing patient
sphincter) stabilization about what about what
• ES separate • PFMT exercise therapy exercise therapy
• BF can and cannot can and cannot
• BFf achieve achieve
when in doubt • PFMT • PFMT
about pelvic floor
contraction capacity • BFf • BFf
• voluntary control
present PFMT
• voluntary control
absent refer to
family doctor/
medical specialist
Evaluation evaluating the outcome: Wexner score, Global Perceived Effect, defecation diary
Follow-up checkup at predefined moment(s) → brief reminder therapy (if necessary)
ES = electrostimulation; PFMT = pelvic floor muscle training; BF = biofeedback (electromyogram, pressure and rectal balloon).
a. without neurological problem (motor); local neurological problem (motor): n. pudendus lesion (S2-S4), iatrogenic; central neurological problem: coordination problem.
b. without neurological problem: 3rd/4th degree tear, traumas, overflow diarrhea, paradoxical straining; local or central neurological problem (sensory): n. pudendus lesion (S2-S4), iatrogenic.
c. voluntary control, i.e. ‘awareness’.
d. pelvic organ prolapse (POP).
e. overflow diarrhea, irritable bowel syndrome, Morbus Crohn, colitis ulcerosa.
f. biofeedback (EMG/pressure/rectal balloon training): if insufficient progress and to speed up results.
*Dutch acronym HEEL: Herkennen van gezondheidsprobleem, Erkennen van gezondheidsprobleem, Expressie (uiten, in beweging brengen) en Loslaten (eigen maken)
V-25/2013 The full-text Evidence Statement is available from www.fysionet-evidencebased.nl © KNGF
You might also like
- A Simple Guide To Nocturia, (Excessive Night Urination) Diagnosis, Treatment And Related ConditionsFrom EverandA Simple Guide To Nocturia, (Excessive Night Urination) Diagnosis, Treatment And Related ConditionsNo ratings yet
- KNGF Evidence Statement: Anal IncontinenceDocument2 pagesKNGF Evidence Statement: Anal IncontinencesilkofosNo ratings yet
- 3 Urinary Incontinence in WomenDocument4 pages3 Urinary Incontinence in WomenDanilo Pereira Dos SantosNo ratings yet
- Abdominal PainDocument3 pagesAbdominal PainNoor AlblushiNo ratings yet
- 04pelvic Floor Physiotherapy For The Management of Incontinence by Kealy France (1 Jun 2016)Document44 pages04pelvic Floor Physiotherapy For The Management of Incontinence by Kealy France (1 Jun 2016)RajiNo ratings yet
- Home Care RN Skills ChecklistDocument2 pagesHome Care RN Skills ChecklistGloryJaneNo ratings yet
- Evaluation of The Incontinent Woman: Yeditepe University, Medical Faculty Dept of Ob&GynDocument47 pagesEvaluation of The Incontinent Woman: Yeditepe University, Medical Faculty Dept of Ob&GynAdnan WalidNo ratings yet
- Week 11: Nursing Care of Patients With Intestinal and Rectal Disorders Abnormalities of Fecal EliminationDocument9 pagesWeek 11: Nursing Care of Patients With Intestinal and Rectal Disorders Abnormalities of Fecal Eliminationeliza luisNo ratings yet
- Rheumatology: - Red Flag DiagnosisDocument3 pagesRheumatology: - Red Flag DiagnosisEmilee Joice Rochelle MalutoNo ratings yet
- 1 Urinary Incontinence in ChildrenDocument5 pages1 Urinary Incontinence in Childrenguido murrieta rojasNo ratings yet
- GI Disorders Lecture on Constipation in Geriatric PatientsDocument11 pagesGI Disorders Lecture on Constipation in Geriatric PatientsYunus AmmarieNo ratings yet
- Managing LUTS BPH For Patients at Risk of Progression - DR RickyDocument37 pagesManaging LUTS BPH For Patients at Risk of Progression - DR RickyafifberlianNo ratings yet
- Urology Referral Recommendations SummaryDocument12 pagesUrology Referral Recommendations Summarymichelle octavianiNo ratings yet
- Làm Gì Khi SDMA TăngDocument1 pageLàm Gì Khi SDMA TăngNguyễn Tấn TàiNo ratings yet
- Inkontinensia Urin: Dr. Adhi Permana, SPPDDocument35 pagesInkontinensia Urin: Dr. Adhi Permana, SPPDTiara KhairinaNo ratings yet
- HISTORY-TAKING-AND-PHYSICAL-EXAMINATION PediatricsDocument50 pagesHISTORY-TAKING-AND-PHYSICAL-EXAMINATION PediatricsShiela GutierrezNo ratings yet
- L19 - Pelvic Pain & EndometriosisDocument8 pagesL19 - Pelvic Pain & EndometriosisBrandonRyanF.MosidinNo ratings yet
- H.A.M. Akil Fardah Akil: "GI Disorders" Lecture in GERIATRI System, FKUHDocument14 pagesH.A.M. Akil Fardah Akil: "GI Disorders" Lecture in GERIATRI System, FKUHCutDianafitriaNo ratings yet
- Creog Urogyn ReviewDocument97 pagesCreog Urogyn ReviewAlexandriah AlasNo ratings yet
- Treating Overactive Bladder NaturallyDocument53 pagesTreating Overactive Bladder NaturallyTô Hoàng DũngNo ratings yet
- I. Introduction To Pelvic Organ Prolapse: Normal Support of Pelvic OrgansDocument14 pagesI. Introduction To Pelvic Organ Prolapse: Normal Support of Pelvic OrgansColeen TrinidadNo ratings yet
- Pediatric Surg TransDocument4 pagesPediatric Surg TransSven OrdanzaNo ratings yet
- Hernia: and Other Digestive Congenital DiseaseDocument14 pagesHernia: and Other Digestive Congenital DiseaseLingga GumelarNo ratings yet
- Low Back PainDocument34 pagesLow Back PainFAMED RESIDENTS CESMEDNo ratings yet
- Inkontinensia Urin Causes, Diagnosis and TreatmentDocument35 pagesInkontinensia Urin Causes, Diagnosis and Treatmenttutor tujuhNo ratings yet
- finalsURINARY ELIMINATION DIAGNOSTICSDocument11 pagesfinalsURINARY ELIMINATION DIAGNOSTICSFrances LiqueNo ratings yet
- Assessment of The Genitourinary System: GeneralDocument2 pagesAssessment of The Genitourinary System: GeneralMaharani UtamiNo ratings yet
- Male Pelvic Pain Jen ShifferdDocument13 pagesMale Pelvic Pain Jen ShifferdCorey EasleyNo ratings yet
- Emergenze Addome RXDocument9 pagesEmergenze Addome RXBrovazzo PieroNo ratings yet
- 1stprize CR Auditpostercomp C Reid 2015Document1 page1stprize CR Auditpostercomp C Reid 2015webber_denzNo ratings yet
- 3-ASKEP GI defect-HIRSCHSPRUNG & MAR-2021-mhsDocument58 pages3-ASKEP GI defect-HIRSCHSPRUNG & MAR-2021-mhsSasNo ratings yet
- HARLE FinalsDocument15 pagesHARLE Finalsangelapadilla0893No ratings yet
- Incontinence AlviDocument54 pagesIncontinence AlviIskandar MusgamyNo ratings yet
- Acute AUBDocument9 pagesAcute AUBJessa MaeNo ratings yet
- Pelvic Floor PresentationDocument9 pagesPelvic Floor PresentationrohiniNo ratings yet
- Sherazi 2019. The Genitourinary SystemDocument26 pagesSherazi 2019. The Genitourinary SystemZadig MuñozNo ratings yet
- UrolithiasisDocument9 pagesUrolithiasisJessa MaeNo ratings yet
- Dysphagia 2001 11 SlidesDocument46 pagesDysphagia 2001 11 SlidescafemedNo ratings yet
- Cleft Lip & Palate: Nursing Management in Children With Congenital DiseaseDocument75 pagesCleft Lip & Palate: Nursing Management in Children With Congenital DiseaseSherly Mectildis BakerNo ratings yet
- Document (3) - 1Document5 pagesDocument (3) - 1Diljot AulakhNo ratings yet
- Assignment 3Document5 pagesAssignment 3Samantha PargadNo ratings yet
- Gs Toronto Nots PdaDocument34 pagesGs Toronto Nots PdaAhmed AttiaNo ratings yet
- Common Health Problems That Develop During InfancyDocument28 pagesCommon Health Problems That Develop During Infancylaurie.charlynjaneNo ratings yet
- Fecal IncontinenceDocument25 pagesFecal IncontinenceBinita ShresthaNo ratings yet
- Nursing Health History: Princess Jamela Camu Celline Isabelle ReyesDocument12 pagesNursing Health History: Princess Jamela Camu Celline Isabelle ReyesCelline Isabelle ReyesNo ratings yet
- Group 1Document9 pagesGroup 1VIVIEN CONSIGNANo ratings yet
- Early Diagnosis & Prompt Treatment of Acute Abdominal PainDocument69 pagesEarly Diagnosis & Prompt Treatment of Acute Abdominal PainRani Silmi ZulafaNo ratings yet
- Cleft Lip & Palate: Nursing Management in Children With Congenital DiseaseDocument84 pagesCleft Lip & Palate: Nursing Management in Children With Congenital DiseaseAnonymous KXYykpaZPNo ratings yet
- 4-ASKEP GI DefectDocument84 pages4-ASKEP GI DefectAnonymous KXYykpaZPNo ratings yet
- Intermittant Claudication FlowchartDocument2 pagesIntermittant Claudication FlowchartsilkofosNo ratings yet
- Acute Pyelonephritis: Diagnostic Test ResultsDocument2 pagesAcute Pyelonephritis: Diagnostic Test ResultschoobiNo ratings yet
- Nursing Health History: Princess Jamela Camu Celline Isabelle ReyesDocument11 pagesNursing Health History: Princess Jamela Camu Celline Isabelle ReyesCelline Isabelle ReyesNo ratings yet
- Practical approach to non-neoplastic endometrial biopsyDocument141 pagesPractical approach to non-neoplastic endometrial biopsySanders PaezNo ratings yet
- Hirschsprung's Disease Diagnosis and TreatmentDocument9 pagesHirschsprung's Disease Diagnosis and TreatmentHaizel BieberNo ratings yet
- Akut Abdomen 2022 (Dr. Kisman Harahap, SP.B)Document100 pagesAkut Abdomen 2022 (Dr. Kisman Harahap, SP.B)Laila Purnama sariNo ratings yet
- Dr. R. M. Saraoogi's Guide to Overactive BladderDocument53 pagesDr. R. M. Saraoogi's Guide to Overactive BladderPalakh KheriaNo ratings yet
- Pedrajeta-Abdominal AssessmentDocument6 pagesPedrajeta-Abdominal AssessmentAndrei PedrajetaNo ratings yet
- Abruptio Placenta. Final OutputDocument15 pagesAbruptio Placenta. Final OutputCharles Loriaga Cruz IINo ratings yet
- Altered Urinary Elimination - ADPCN Resource UnitDocument5 pagesAltered Urinary Elimination - ADPCN Resource UnitChillette FarraronsNo ratings yet
- Bedwetting in Children PptDocument41 pagesBedwetting in Children PptAnkit ManglaNo ratings yet
- Input5 Stud CDP Postop Edema 2013 PDFDocument12 pagesInput5 Stud CDP Postop Edema 2013 PDFsilkofosNo ratings yet
- Input4 Insufficiency 2012-03-05 PDFDocument14 pagesInput4 Insufficiency 2012-03-05 PDFsilkofosNo ratings yet
- Chronic Leg Edema Exercises Brochure - EN (LR) PDFDocument2 pagesChronic Leg Edema Exercises Brochure - EN (LR) PDFsilkofosNo ratings yet
- NL Handout 2013-03-05 PDFDocument21 pagesNL Handout 2013-03-05 PDFsilkofosNo ratings yet
- Weight Lifting and Lymphedema: Clearing Up MisconceptionsDocument4 pagesWeight Lifting and Lymphedema: Clearing Up MisconceptionssilkofosNo ratings yet
- Complementary and Alternative Medicine For Cancer Pain 2013Document9 pagesComplementary and Alternative Medicine For Cancer Pain 2013silkofosNo ratings yet
- An Overview of Systematic Reviews of Clinical Evidence For Cupping Therapy 2014Document8 pagesAn Overview of Systematic Reviews of Clinical Evidence For Cupping Therapy 2014silkofosNo ratings yet
- Clinical Research Evidence of Cupping Therapy Iin China - A Systematic Literature ReviewDocument10 pagesClinical Research Evidence of Cupping Therapy Iin China - A Systematic Literature ReviewMiki ShimizuNo ratings yet
- Input3 Stud Bandages 2012-03-05pptx PDFDocument12 pagesInput3 Stud Bandages 2012-03-05pptx PDFsilkofosNo ratings yet
- Mode of Action of Cupping Local Metabolism and Pain Thresholds in Neck Pain Patients and Healthy Subjects 2014Document11 pagesMode of Action of Cupping Local Metabolism and Pain Thresholds in Neck Pain Patients and Healthy Subjects 2014silkofosNo ratings yet
- StrokeDocument4 pagesStrokeayuditaNo ratings yet
- Is Cupping An Effective Treatment - An Overview of Systematic ReviewsDocument4 pagesIs Cupping An Effective Treatment - An Overview of Systematic ReviewsMiki ShimizuNo ratings yet
- Clinical Practice Guidelines For Physical Therapy in Patients With Intermittent ClaudicationDocument51 pagesClinical Practice Guidelines For Physical Therapy in Patients With Intermittent ClaudicationsilkofosNo ratings yet
- Carpal Tunnel Syndrome Part I Effectiveness of Nonsurgical 2014 PDFDocument24 pagesCarpal Tunnel Syndrome Part I Effectiveness of Nonsurgical 2014 PDFsilkofosNo ratings yet
- Acupoint Stimulation For Fibromyalgia 2013Document15 pagesAcupoint Stimulation For Fibromyalgia 2013silkofosNo ratings yet
- Research Article Effects of Wet-Cupping On Blood Pressure in Hypertensive Patients: A Randomized Controlled TrialDocument9 pagesResearch Article Effects of Wet-Cupping On Blood Pressure in Hypertensive Patients: A Randomized Controlled TrialDewi Negeri AtikaNo ratings yet
- Journal Pone 0031793 PDFDocument14 pagesJournal Pone 0031793 PDFDaniel raja SotardodoNo ratings yet
- Dutch Motor Handwriting PROBLEM in CHILDREN Physiotherapy FlowchartDocument2 pagesDutch Motor Handwriting PROBLEM in CHILDREN Physiotherapy FlowchartyohanNo ratings yet
- Hartrevalidatie PRL Eng KNGFDocument52 pagesHartrevalidatie PRL Eng KNGFsilkofosNo ratings yet
- Intermittant Claudication FlowchartDocument2 pagesIntermittant Claudication FlowchartsilkofosNo ratings yet
- Carpal Tunnel Syndrome Part I Effectiveness of Nonsurgical 2014 PDFDocument24 pagesCarpal Tunnel Syndrome Part I Effectiveness of Nonsurgical 2014 PDFsilkofosNo ratings yet
- Clinical Practice Guidelines For Physical Therapy in Patients With Intermittent ClaudicationDocument51 pagesClinical Practice Guidelines For Physical Therapy in Patients With Intermittent ClaudicationsilkofosNo ratings yet
- Low Back Pain Practice Guidelines 2013Document12 pagesLow Back Pain Practice Guidelines 2013silkofosNo ratings yet
- Hartrevalidatie PRL Eng KNGFDocument52 pagesHartrevalidatie PRL Eng KNGFsilkofosNo ratings yet
- KNGF Evidence Statement: Anal IncontinenceDocument22 pagesKNGF Evidence Statement: Anal IncontinencesilkofosNo ratings yet
- Dutch Motor Handwriting PROBLEM in CHILDREN Physiotherapy SummaryDocument7 pagesDutch Motor Handwriting PROBLEM in CHILDREN Physiotherapy SummaryyohanNo ratings yet
- Dutch Motor Handwriting PROBLEM in CHILDREN Physiotherapy FlowchartDocument2 pagesDutch Motor Handwriting PROBLEM in CHILDREN Physiotherapy FlowchartyohanNo ratings yet
- Intermittant Claudication FlowchartDocument2 pagesIntermittant Claudication FlowchartsilkofosNo ratings yet
- Discectomy Rehab CohraneDocument105 pagesDiscectomy Rehab CohranesilkofosNo ratings yet
- 300 Npte Questions and Answers PtmasudpdfDocument921 pages300 Npte Questions and Answers PtmasudpdfSindhu MunnyNo ratings yet
- Prometric Mcqs For General Practitioner GP Doctor Mcqs Exam QuestionsDocument28 pagesPrometric Mcqs For General Practitioner GP Doctor Mcqs Exam QuestionsDr. Saqib RazaNo ratings yet
- PNLE III For Care of Clients With Physiologic and Psychosocial AlterationsDocument10 pagesPNLE III For Care of Clients With Physiologic and Psychosocial AlterationsANGELINE PALATINO100% (1)
- Early Embryology: Somite Stage and Limb Bud DevelopmentDocument21 pagesEarly Embryology: Somite Stage and Limb Bud DevelopmentDavidroy IRITSNo ratings yet
- Infection Control and Child AbuseDocument8 pagesInfection Control and Child AbuseÀi ZìjǐNo ratings yet
- Microbiology: A Systems Approach, 2 Ed.: Chapter 19: Infectious Diseases Affecting The Nervous SystemDocument69 pagesMicrobiology: A Systems Approach, 2 Ed.: Chapter 19: Infectious Diseases Affecting The Nervous SystemKim ManlangitNo ratings yet
- 28 - Rosita Febrianti Jurnal Review (Bahasa Inggris)Document20 pages28 - Rosita Febrianti Jurnal Review (Bahasa Inggris)Restu YasalamNo ratings yet
- Test Sample For ICFDocument6 pagesTest Sample For ICFNeptali CardinalNo ratings yet
- Plab-1 1700 MCQs Solved With Explanation (Shared by Ussama Maqbool)Document729 pagesPlab-1 1700 MCQs Solved With Explanation (Shared by Ussama Maqbool)Omar Abo el nagaNo ratings yet
- Medical English Vocabulary GuideDocument9 pagesMedical English Vocabulary GuideErika Yulia QaNo ratings yet
- Cerebellum and Brain Stem: DR Asim Shrestha SRCC Ped Neuro Fellow MumbaiDocument71 pagesCerebellum and Brain Stem: DR Asim Shrestha SRCC Ped Neuro Fellow MumbaiAsim ShresthaNo ratings yet
- Arduino Guided Smart Rodent Trap (Trapuino)Document9 pagesArduino Guided Smart Rodent Trap (Trapuino)Eunice Nicole Masecampo LautingcoNo ratings yet
- Intro To First Aid and Basic Life SupportDocument31 pagesIntro To First Aid and Basic Life SupportLance BaraquielNo ratings yet
- Phrasal Verbs About Pandemics and Epidemics Conversation Topics Dialogs Debating Argumentation 123928Document14 pagesPhrasal Verbs About Pandemics and Epidemics Conversation Topics Dialogs Debating Argumentation 123928Maier OlimpiuNo ratings yet
- The Endocrine System: Did You KnowDocument40 pagesThe Endocrine System: Did You Knowmir-medicinaNo ratings yet
- Nclex Review Uworld (6515)Document137 pagesNclex Review Uworld (6515)whereswaldo007yahooc88% (8)
- U.S. Preventive Services Task Force (USPSTF) Recommendations - Stats - Medbullets Step 2 - 3Document5 pagesU.S. Preventive Services Task Force (USPSTF) Recommendations - Stats - Medbullets Step 2 - 3mtataNo ratings yet
- (Non Trauma) 24-09-2023 - TN - Kalil - DOC Ec CVA ICHDocument11 pages(Non Trauma) 24-09-2023 - TN - Kalil - DOC Ec CVA ICHRasyidu MashuriNo ratings yet
- 6 Saal Khushhaal Pariwar: A NEW Innovative MEDICLAIMDocument9 pages6 Saal Khushhaal Pariwar: A NEW Innovative MEDICLAIMPalash JhabakNo ratings yet
- Cosmetic and Reconstructive Surgery PolicyDocument13 pagesCosmetic and Reconstructive Surgery PolicyBrian AndrewNo ratings yet
- MD PW 1,2 Eyelids and AnatomyDocument84 pagesMD PW 1,2 Eyelids and Anatomytaliya. shvetzNo ratings yet
- Genetic Testing and Treatment: Lewis Chapter 20Document16 pagesGenetic Testing and Treatment: Lewis Chapter 20Shane G.No ratings yet
- SelvanDocument144 pagesSelvanVenkatesan Vidhya100% (3)
- Fourniers Gangrene of The External Genitalia: Plastic Reconstruction by Thin Skin GraftDocument7 pagesFourniers Gangrene of The External Genitalia: Plastic Reconstruction by Thin Skin GraftIJAR JOURNALNo ratings yet
- This Study Resource Was Shared Via: Hypo HyperDocument1 pageThis Study Resource Was Shared Via: Hypo HyperRobin Abraham-BalisiNo ratings yet
- Nursing Care in MR.X With Urinary Retention: Mega Meilisa Manara 2014901072Document6 pagesNursing Care in MR.X With Urinary Retention: Mega Meilisa Manara 2014901072Hafin WardanaNo ratings yet
- HEALTH 8: Communicable DiseaseDocument31 pagesHEALTH 8: Communicable DiseaseElissah S PabilonaNo ratings yet
- Assignment of Pathology 401: Submitted byDocument5 pagesAssignment of Pathology 401: Submitted byaymen gulzarNo ratings yet
- Lesson Plans k6Document13 pagesLesson Plans k6Regine Delfin AclaracionNo ratings yet
- Constipation Paliatif CareDocument17 pagesConstipation Paliatif Careshu mitunNo ratings yet