Professional Documents
Culture Documents
Jama Poston 2020 Gs 200003
Uploaded by
Alex Fernando Páez VallejoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jama Poston 2020 Gs 200003
Uploaded by
Alex Fernando Páez VallejoCopyright:
Available Formats
Clinical Review & Education
JAMA Clinical Guidelines Synopsis
Management of Critically Ill Adults With COVID-19
Jason T. Poston, MD; Bhakti K. Patel, MD; Andrew M. Davis, MD, MPH
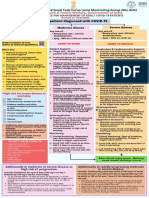
GUIDELINE TITLE Surviving Sepsis Campaign: Guidelines on the 2. For acute hypoxemic respiratory failure despite conventional oxygen
Management of Critically Ill Adults With COVID-19 therapy, use of high-flow nasal cannula (HFNC) is suggested relative to
conventional oxygen therapy and noninvasive positive pressure ventila-
DEVELOPER Surviving Sepsis Campaign (SSC) tion (NIPPV) (weak recommendation, LQE). If HFNC is not available, a trial
of NIPPV is suggested (weak recommendation, very LQE). Close monitor-
ing for worsening of respiratory status and early intubation if worsening
RELEASE DATE March 23, 2020
occurs is recommended (best practice statement).
3. For adults receiving mechanical ventilation who have acute respiratory
TARGET POPULATION Critically ill adults with COVID-19
distress syndrome (ARDS), use of low tidal volume ventilation (4-8
mL/kg of predicted body weight) is recommended and preferred over
SELECTED MAJOR RECOMMENDATIONS
higher tidal volumes (>8 mL/kg) (strong recommendation, moderate
Infection Control and Testing QE). Targeting plateau pressures of <30 cm H2O (strong recommenda-
tion, moderate QE) is recommended. Using a higher positive end-expira-
1. For health care workers performing aerosol-generating procedures (eg, tory pressure (PEEP) strategy over lower PEEP strategy is suggested
endotracheal intubation, nebulized treatments, open suctioning) use of (weak recommendation, LQE).
fitted respirator masks is recommended (N95 respirators, FFP2), instead 4. For adults receiving mechanical ventilation who have moderate to severe
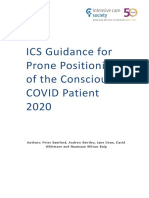
of surgical masks, in addition to other personal protective equipment ARDS, prone ventilation for 12 to 16 hours is suggested over no prone venti-
(PPE) (best practice statement). lation (weak recommendation, LQE). Using as-needed neuromuscular
2. For usual care of nonventilated patients, or for performing non–aerosol- blocking agents (NMBAs) instead of continuous NMBA infusion to facilitate
generating procedures on patients receiving mechanical ventilation, use protective lung ventilation is suggested (weak recommendation, LQE).
of medical masks is recommended, instead of respirator masks, in addi- 5. For adults receiving mechanical ventilation who have severe ARDS and
tion to other PPE (weak recommendation, low-quality evidence [LQE]). hypoxemia despite optimizing ventilation, a trial of inhaled pulmonary
3. Diagnostic lower respiratory tract samples (endotracheal aspirates) are vasodilator is suggested. If no rapid improvement in oxygenation is ob-
preferred over bronchial washings, bronchoalveolar lavage, and upper served, the treatment should be tapered (weak recommendation, very
respiratory tract (nasopharyngeal or oropharyngeal) samples (weak rec- LQE). The use of lung recruitment maneuvers (intended to open other-
ommendation, LQE). wise closed lung segments, such as 40 cm H2O inspiratory hold for 40
Hemodynamic Support seconds) is suggested, over not using recruitment maneuvers (weak
recommendation, LQE), but using staircase (incremental PEEP) recruit-
1. For acute resuscitation of adults with shock, the following are suggested: ment maneuvers is not recommended (strong recommendation, moder-
measuring dynamic parameters to assess fluid responsiveness (weak ate QE). Use of veno-venous circulation for extracorporeal membrane
recommendation, LQE), using a conservative fluid administration strategy oxygenation (ECMO) or referral to an ECMO center is suggested, if avail-
(weakrecommendation,veryLQE),andusingcrystalloidsovercolloids(strong able, for selected patients (weak recommendation, LQE).
recommendation; moderate QE). Balanced crystalloids are preferred over
unbalanced crystalloids (weak recommendation, moderate QE). Therapy
2. For adults with shock, the following are suggested: using norepinephrine 1. In adults receiving mechanical ventilation who do not have ARDS, rou-
as the first-line vasoactive (weak recommendation, LQE), use of either tine use of systematic corticosteroids is suggested against (weak recom-
vasopressin or epinephrine as the first line if norepinephrine is not avail- mendation, LQE). In those with ARDS, use of corticosteroids is sug-
able (weak recommendation, LQE). Dopamine is not recommended if gested (weak recommendation, LQE).
norepinephrine is not available (strong recommendation, high QE). Add- 2. In COVID-19 patients receiving mechanical ventilation who have respira-
ing vasopressin as a second-line agent is suggested if the target (60-65 tory failure, use of empiric antimicrobial/antibacterial agents is sug-
mm Hg) mean arterial pressure cannot be achieved by norepinephrine gested (no evidence rating); assess for deescalation.
alone (weak recommendation, moderate QE). 3. In critically ill adults with fever, use of pharmacologic agents for tempera-
Ventilatory Support ture control is suggested over nonpharmacologic agents or no treatment.
Routine use of standard IV immunoglobulins is not suggested. Convales-
1. Starting supplemental oxygen is recommended if the SpO2 is less than cent plasma is not suggested. There is insufficient evidence to issue a rec-
90% (strong recommendation, moderate QE). SpO2 should be main- ommendation on use of any of the following: antiviral agents, recombi-
tained no higher than 96% (strong recommendation, moderate QE). nant interferons, chloroquine/hydroxychloroquine, or tocilizumab.
Summary of the Clinical Problem Characteristics of the Guideline Source
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is The Surviving Sepsis Campaign (SSC) has previously published a se-
the cause of COVID-19, a pandemic that has affected more than ries of guidelines for sepsis and septic shock. Based on this experi-
400 000 individuals and caused nearly 20 000 deaths as of late ence, experts were recruited to write guidelines on the manage-
March 2020. Approximately 5% to 10% of patients require inten- ment of COVID-19 in critically ill adults. These guidelines were
sive care unit (ICU) admission and mechanical ventilation.1 authored by 36 experts from 12 countries (Table).2 Recommendations
jama.com (Reprinted) JAMA Published online March 26, 2020 E1
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/07/2020
Clinical Review & Education JAMA Clinical Guidelines Synopsis
mortality (odds ratio, 2.76 [95% CI, 2.06-3.69]), although the
Table. Guideline Rating
association among patients with coronaviruses was unclear (odds
Standard Rating ratio, 0.83 [95% CI, 0.32-2.17]).
Establishing transparency Good The guideline recommendations for management of respira-
Management of COI in the guideline development group Good tory failure highlight the competing goals unique to the COVID-19
Guideline development group composition Good pandemic. A recommendation for the use of HFNC oxygen
Clinical practice guideline–systematic review intersection Good therapy is based on findings from a clinical trial that showed a
Establishing evidence foundations and rating strength for each Good benefit relative to standard oxygen and NIPPV in progression to
of the guideline recommendations intubation. 8 The panel also recommended a trial of NIPPV if
Articulation of recommendations Good HFNC is unavailable or ineffective. Following these recommenda-
External review Fair tions may prevent intubation and the need for ventilator support,
Updating Good a scarce resource when there are large numbers of COVID-19
Implementation issues Fair cases. However, HFNC and NIPPV may also aerosolize respiratory
droplets, which will increase the need for negative-pressure
rooms and N95 or FFP2 masks, which are also a scarce
were developed based on limited direct evidence with COVID-19 resource.
cases and indirect evidence derived from previous pandemics
such as Middle East respiratory syndrome (MERS), severe
acute respiratory syndrome (SARS), and other coronavirus infec-
Discussion
The COVID-19 pandemic has brought unprecedented challenges
tions. Overall, the panel issued 54 statements: 4 best practice
regarding the ability to generate timely evidence, even as the
statements, 9 strong recommendations, and 35 weak recommen-
disease overwhelms health care systems and stresses the
dations. (No recommendations were made for the remaining
clinical workforce. This SSC guideline2 will be frequently updated
6 topics.)
online as global evidence accrues, but it reflects the central ten-
ants of best practices for ARDS: low tidal volume strategy, PEEP
Evidence Base titration, avoidance of hyperoxia, and a conservative fluid
The GRADE method was used, with the actionable guideline ques- strategy.
tions placed in population, intervention, comparator, outcomes
(PICO) format. The first discusses PPE to protect health care work-
Areas in Need of Future Study or Ongoing Research
ers and prevent nosocomial spread of virus. A recent clinical trial of
Many of these recommendations are extrapolated from studies
2862 health care personnel at 137 outpatient sites compared the use
and experience in critically ill patients without COVID-19. How-
of N95 respirators vs medical masks and found no significant dif-
ever, this pandemic has necessitated flexibility and ingenuity to
ference in the incidence of laboratory-confirmed influenza (8.2% vs
address its unique challenges, and it will require continued rapid
7.2% health care personnel seasons; difference, 1.0% [95% CI, −0.5%
and judicious synthesis of heterogeneous and rapidly evolving
to 2.5%]; P = .18) (adjusted odds ratio, 1.18 [95% CI, 0.95-1.45]).3 The
data and clinical experience shared by clinicians.
CDC recently discussed strategies for optimizing the supply of face
For instance, concern for aerosolization with HFNC and
masks.
NIPPV and a critical shortage of mechanical ventilators have led
Critically ill patients with COVID-19 often develop septic (dis-
to consideration of helmet NIPPV as an alternative in centers with
tributive) shock. Fluid resuscitation guided by dynamic assess-
this resource. Additionally, a small single-center clinical trial
ment of fluid responsiveness is recommended based on a reduc-
(n = 83 patients) has suggested decreased intubation and mortal-
tion in mortality (risk ratio, 0.59 [95% CI, 0.42-0.83]; P = .002)
ity with use of helmet NIPPV compared with face mask.9 Unfortu-
in a meta-analysis of 1652 patients in 13 trials.4 These dynamic
nately, these investigations used a ventilator to deliver helmet
measures facilitate a more judicious, rather than liberal, fluid
NIPPV. If the intent is to spare patients from invasive mechanical
strategy both during and after initial resuscitation.5
ventilation while limiting exposure to health care workers, helmet
NIPPV using a ventilator may be an option. Alternatively, if
Benefits and Harms mechanical ventilators are in short supply, it is possible to deliver
The panel issued a suggestion against the routine use of system- helmet NIPPV using a flow generator (ⱖ60 L/min) to deliver
atic corticosteroids for respiratory failure without ARDS in COVID- oxygen and an expiratory pressure valve to maintain PEEP.
19, but issued a suggestion for use in patients with ARDS. One ret- The guideline panel noted the option of helmet NIPPV but
rospective, non–peer-reviewed report of 46 patients6 suggested was not able to make a recommendation, noting uncertainty
treatment with methylprednisolone, 1 to 2 mg/kg/d for 5 to 7 about its safety and efficacy in COVID-19. Such issues underscore
days, was associated with a reduction in duration of fever and the the importance of considering the range of local resources
need for supplemental oxygen. The panel also drew on indirect and context in implementing care plans for patients with
evidence of corticosteroid use in community-acquired pneumo- COVID-19.
nia, ARDS, and other viral infections, using a Cochrane review7 on Finally, there is a pressing need to address resource allocation,
the use of steroids in viral pneumonia, updated to include 15 innovative staffing, and alternative delivery models in providing ethi-
cohort studies on influenza and 10 on coronaviruses. This analysis cal care for critically ill patients when there are insufficient ICU beds
found an association between corticosteroid use and increased during a pandemic.10
E2 JAMA Published online March 26, 2020 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/07/2020
JAMA Clinical Guidelines Synopsis Clinical Review & Education
COVID-19 Critical Care Guideline: Additional Resources
This guideline was developed collaboratively between the European critically ill adults with coronavirus disease 2019 (COVID-19).
Society of Intensive Care Medicine (ESCIM) and the Society of Crit Care Med. Published online March 27, 2020. doi:10.1097/CCM.
Critical Care Medicine (SCCM). 0000000000004363.
Guideline publications Additional COVID-19 critical care resources
ESCIM publication: Alhazzani W, Møller MH, Arabi YM, et al. ESCIM: https://www.esicm.org/resources/coronavirus-public-
Surviving Sepsis Campaign: guidelines on the management of health-emergency/
critically ill adults with coronavirus disease 2019 (COVID-19). SCCM: https://www.sccm.org/Disaster
Intensive Care Med. Published online March 28, 2020. doi:10.1007/
s00134-020-06022-5. Related resources
JAMA Network Coronavirus Resource Center
SCCM publication: Alhazzani W, Møller MH, Arabi YM, et al.
Surviving Sepsis Campaign: guidelines on the management of
ARTICLE INFORMATION report of 72 314 cases from the Chinese Center for single-center experience from Wuhan, China.
Author Affiliations: Pulmonary and Critical Care, Disease Control and Prevention. JAMA. Published medRxiv. Preprint posted March 12, 2020.
University of Chicago, Chicago, Illinois (Poston, online February 24, 2020. doi:10.1001/jama.2020. doi:10.1101/2020.03.06.20032342v1
Patel); General Internal Medicine, University of 2648 7. Lansbury L, Rodrigo C, Leonardi-Bee J,
Chicago, Chicago, Illinois (Davis). 2. Surviving Sepsis Campaign. COVID-19 Nguyen-Van-Tam J, Lim WS. Corticosteroids as
Corresponding Author: Jason T. Poston, MD, Guidelines. Published March 20, 2020. https:// adjunctive therapy in the treatment of influenza.
University of Chicago, 850 E 58th St, Chicago, IL www.sccm.org/SurvivingSepsisCampaign/ Cochrane Database Syst Rev. 2019;2:CD010406.
60615 (Jason.Poston@uchospitals.edu). Guidelines/COVID-19 8. Frat JP, Thille AW, Mercat A, et al; FLORALI Study
Section Editor: Edward H. Livingston, MD, Deputy 3. Radonovich LJ Jr, Simberkoff MS, Bessesen MT, Group; REVA Network. High-flow oxygen through
Editor, JAMA. et al; ResPECT investigators. N95 respirators vs nasal cannula in acute hypoxemic respiratory
medical masks for preventing influenza among failure. N Engl J Med. 2015;372(23):2185-2196. doi:
Published Online: March 26, 2020. health care personnel. JAMA. 2019;322(9):824-833. 10.1056/NEJMoa1503326
doi:10.1001/jama.2020.4914 doi:10.1001/jama.2019.11645 9. Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress
Correction: This article was corrected on April 3, 4. Bednarczyk JM, Fridfinnson JA, Kumar A, et al. JP. Effect of noninvasive ventilation delivered by
2020, to include all of the related resources and Incorporating dynamic assessment of fluid helmet vs face mask on the rate of endotracheal
relevant publications. responsiveness into goal-directed therapy: intubation in patients with acute respiratory
Conflict of Interest Disclosures: Dr Patel reports a systematic review and meta-analysis. Crit Care Med. distress syndrome: a randomized clinical trial. JAMA.
receiving grants from Parker B. Francis Career 2017;45(9):1538-1545. doi:10.1097/CCM. 2016;315(22):2435-2441. doi:10.1001/jama.2016.
Development award and from NIH/NHLBI T32 0000000000002554 6338
HL007605 Research Training in Respiratory 5. Bentzer P, Griesdale DE, Boyd J, MacLean K, 10. SIAARTI. Clinical ethics recommendations for
Biology. Dr Poston receiving honoraria for the Sirounis D, Ayas NT. Will this hemodynamically the allocation of intensive care treatments in
CHEST Critical Care Board Review Course. Dr Davis unstable patient respond to a bolus of intravenous exceptional resource-limited circumstances.
reported no disclosures. fluids? JAMA. 2016;316(12):1298-1309. doi:10.1001/ Published March 16, 2020. Accessed March 23,
jama.2016.12310 2020. http://www.siaarti.it/SiteAssets/News/
REFERENCES COVID19%20-%20documenti%20SIAARTI/
6. Wang Y, Jiang W, He Q, et al Early, low-dose and
1. Wu Z, McGoogan JM. Characteristics of and short-term application of corticosteroid treatment SIAARTI%20-%20Covid-19%20-%20Clinical%
important lessons from the coronavirus disease in patients with severe COVID-19 pneumonia: 20Ethics%20Reccomendations.pdf
2019 (COVID-19) outbreak in China: summary of a
jama.com (Reprinted) JAMA Published online March 26, 2020 E3
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/07/2020
You might also like
- Break Your Leg InternDocument199 pagesBreak Your Leg InternkingNo ratings yet
- Study Guide Emergency and Trauma NursingDocument11 pagesStudy Guide Emergency and Trauma NursingMarie Angelique Cruz Crestani100% (5)
- Anesthaesia and Intensive CareDocument139 pagesAnesthaesia and Intensive CareIvan Kurniadi100% (2)
- Cardiopulmonary PhysiotherapyDocument181 pagesCardiopulmonary PhysiotherapyOana Moza100% (3)
- Management of Life Threatening Asthma. Severe Asthma Series. CHEST 2022Document10 pagesManagement of Life Threatening Asthma. Severe Asthma Series. CHEST 2022carla jazmin cortes rodriguezNo ratings yet
- Guideline For The Prevention of Bronchopulmonary Dysplasia and Assessment of Evolving BPDDocument28 pagesGuideline For The Prevention of Bronchopulmonary Dysplasia and Assessment of Evolving BPDjanfk2000No ratings yet
- Anaesthesia & Intensive Care: For Fcai, Frca EdaicDocument139 pagesAnaesthesia & Intensive Care: For Fcai, Frca EdaicMuhammad Farid100% (2)
- Aprv PDFDocument2 pagesAprv PDFKaterina TsNo ratings yet
- Lecture Anwar Ventilation Managment COVIDDocument28 pagesLecture Anwar Ventilation Managment COVIDمحمدرزازالتبعيNo ratings yet
- BNM Covid FrancesDocument4 pagesBNM Covid FrancesMISSAEL ESPINOZANo ratings yet
- Anaesthesia For Trauma PatientsDocument42 pagesAnaesthesia For Trauma PatientsMerindukan Surga MuNo ratings yet
- BTSICS Guideline For The Ventilatory Management of Acute Hypercapnic Respiratory Failure in Adults.Document21 pagesBTSICS Guideline For The Ventilatory Management of Acute Hypercapnic Respiratory Failure in Adults.Madalina TalpauNo ratings yet
- COVID-19 Management of Critical Care Cases PDFDocument6 pagesCOVID-19 Management of Critical Care Cases PDFLubna AliNo ratings yet
- SSC COVID19GuidelinesRecTable FirstUpdateDocument5 pagesSSC COVID19GuidelinesRecTable FirstUpdatesatya.drNo ratings yet
- Webinar Kuliah Umum Anestesi Joglo Semar 17 Juni 2020Document95 pagesWebinar Kuliah Umum Anestesi Joglo Semar 17 Juni 2020izaNo ratings yet
- Management of COPD2Document55 pagesManagement of COPD2frankozed1No ratings yet
- Riesgo Alto de Manejo de La Vía AereaDocument17 pagesRiesgo Alto de Manejo de La Vía AereaAntonio AlonsoNo ratings yet
- Acute Chest Syndrome (ACS) CCGDocument11 pagesAcute Chest Syndrome (ACS) CCGJessa MaeNo ratings yet
- Anaesthetics NotesDocument15 pagesAnaesthetics NotesnaNo ratings yet
- Airway Covid - 19Document37 pagesAirway Covid - 19Monica Herdiati Rukmana NaibahoNo ratings yet
- Management of ARDS in Adults: JAMA Clinical Guidelines SynopsisDocument2 pagesManagement of ARDS in Adults: JAMA Clinical Guidelines SynopsisEmman AbelardoNo ratings yet
- Secuencia Rapida GuiasDocument29 pagesSecuencia Rapida GuiasToñoGomezNo ratings yet
- Management of Acute Respiratory Failure in COVID-PUI Patient - Updated Feb. 2021Document7 pagesManagement of Acute Respiratory Failure in COVID-PUI Patient - Updated Feb. 2021Abhishek GoelNo ratings yet
- Rapid Sequences InductionDocument3 pagesRapid Sequences InductionNoha AhmedNo ratings yet
- Noninvasive Ventilation in Acute Respiratory Failure in AdultsDocument12 pagesNoninvasive Ventilation in Acute Respiratory Failure in AdultsferrevNo ratings yet
- Critical Care Management of Covid-19 Algorithm-EngDocument1 pageCritical Care Management of Covid-19 Algorithm-EngMr CROWNo ratings yet
- Management of ARDS in AdultsDocument2 pagesManagement of ARDS in AdultsCarlos PalominoNo ratings yet
- Noninvasive Ventilation - Overview, Methods of Delivery, General ConsiderationsDocument30 pagesNoninvasive Ventilation - Overview, Methods of Delivery, General ConsiderationssnezaimNo ratings yet
- Paediatric Advanced Life Support GuidelinesDocument31 pagesPaediatric Advanced Life Support GuidelinesEXODUSGENNo ratings yet
- 2015 S 0034 1393414 PDFDocument15 pages2015 S 0034 1393414 PDFMadalina StoicescuNo ratings yet
- Critical Care of Patient With Covid 19Document32 pagesCritical Care of Patient With Covid 19Anonymous Kv0sHqFNo ratings yet
- Management of Life-Threatening Asthma (@ eDocument10 pagesManagement of Life-Threatening Asthma (@ eLex X PabloNo ratings yet
- Critical Decisions in Airway ManagementDocument43 pagesCritical Decisions in Airway ManagementPablo RamirezNo ratings yet
- Noninvasive Ventilation in Acute Respiratory Failure in Adults - UpToDateDocument27 pagesNoninvasive Ventilation in Acute Respiratory Failure in Adults - UpToDatehugo roblesNo ratings yet
- Medical Management-Critically IllDocument4 pagesMedical Management-Critically IllMiki MykesNo ratings yet
- OVERVIEW Rapid Sequence Intubation (RSI) Is An Airway Management Technique That ProducesDocument7 pagesOVERVIEW Rapid Sequence Intubation (RSI) Is An Airway Management Technique That ProducesOkami PNo ratings yet
- Adult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAdult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of Indiapramodbankhele3845No ratings yet
- 4.-Rapid Sequence Intubation in Adults - Uptodate PDFDocument14 pages4.-Rapid Sequence Intubation in Adults - Uptodate PDFkendramura100% (1)
- Derek C Angus Caring For Patients With AcuteDocument4 pagesDerek C Angus Caring For Patients With AcuteAnanth BalakrishnanNo ratings yet
- Acute Life-Threatening Hypoxemia During Mechanical VentilationDocument8 pagesAcute Life-Threatening Hypoxemia During Mechanical VentilationCesar Rivas CamposNo ratings yet
- MOHFW Critical Care GuidelinesDocument123 pagesMOHFW Critical Care GuidelinesMOHAMMED IQBALNo ratings yet
- Infeksi Bedah & Surviving Sepsis ChampaignDocument22 pagesInfeksi Bedah & Surviving Sepsis ChampaignHafiz AlfarizieNo ratings yet
- European Consensus On The Management of RDSDocument41 pagesEuropean Consensus On The Management of RDSDeddy Supriyadi100% (1)
- Rapid Sequence Intubation: BackgroundDocument8 pagesRapid Sequence Intubation: Backgroundmarsh86No ratings yet
- Presentasi Dr. Basuki Rachmad, Sp. An. KICDocument39 pagesPresentasi Dr. Basuki Rachmad, Sp. An. KICFirdaus FamilyNo ratings yet
- Comparison Sheet Based On 2010 AHA Guidelines For CPR and ECC BLS ChangesDocument5 pagesComparison Sheet Based On 2010 AHA Guidelines For CPR and ECC BLS ChangesCupit NubillisNo ratings yet
- Lab 3. The Management ofDocument6 pagesLab 3. The Management ofMariana UngurNo ratings yet
- Appendix 1: Recommendations and Best Practice StatementsDocument13 pagesAppendix 1: Recommendations and Best Practice StatementsWalter Manuel Yañez CamachoNo ratings yet
- Anaphylaxis - Emergency Treatment - UpToDateDocument49 pagesAnaphylaxis - Emergency Treatment - UpToDatealinaNo ratings yet
- Non-Invasive Ventilation in Acute Respiratory Failure: Bts GuidelineDocument21 pagesNon-Invasive Ventilation in Acute Respiratory Failure: Bts GuidelineddubbNo ratings yet
- 05-2022 CC PulmonaryDisordersIDocument26 pages05-2022 CC PulmonaryDisordersINada AhmedNo ratings yet
- Rapid Sequence Intubation (RSI) - LITFL - CCC AirDocument20 pagesRapid Sequence Intubation (RSI) - LITFL - CCC Airمحمد عقيليNo ratings yet
- Inhaled Vasodilators As Salvage Therapy in ARDS Caused by H1N1 InfectionDocument5 pagesInhaled Vasodilators As Salvage Therapy in ARDS Caused by H1N1 InfectiondarmariantoNo ratings yet
- Retired: AARC Clinical Practice GuidelineDocument16 pagesRetired: AARC Clinical Practice GuidelineAnnisa Rahma SariNo ratings yet
- 2020-04-12 Guidance For Conscious ProningDocument6 pages2020-04-12 Guidance For Conscious ProningfrankcoapNo ratings yet
- COVID 19. 4 - 13 KashmerDocument42 pagesCOVID 19. 4 - 13 KashmerIshfaq GanaiNo ratings yet
- Papazian2022 Article PronePositionInMechanicallyVenDocument4 pagesPapazian2022 Article PronePositionInMechanicallyVenA. RaufNo ratings yet
- Anaphylaxis - Emergency Treatment - UpToDateDocument38 pagesAnaphylaxis - Emergency Treatment - UpToDatefentaNo ratings yet
- Terapia Adjunta en SdraDocument23 pagesTerapia Adjunta en SdraMarcoNo ratings yet
- Anaesthesia Management For Bronchoscopic and Surgical Lung Volume ReductionDocument6 pagesAnaesthesia Management For Bronchoscopic and Surgical Lung Volume ReductionRoni ArdianNo ratings yet
- Supportive Care in Clinical ToxicologyDocument13 pagesSupportive Care in Clinical ToxicologyKausal VermaNo ratings yet
- ScapeDocument7 pagesScapeRoshan MathewNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Modern Anaesthesia:: A Concise Guide to the Study and Practice of Anaesthesia.From EverandModern Anaesthesia:: A Concise Guide to the Study and Practice of Anaesthesia.No ratings yet
- Technical Manual GN Advance Neo and TSDocument168 pagesTechnical Manual GN Advance Neo and TSReuel Tacay100% (1)
- ACUTE RESPIRATORY FAILURE QuizDocument3 pagesACUTE RESPIRATORY FAILURE QuizTrish 001950% (2)
- En User Manual Bellavista V4.3 Rev02Document155 pagesEn User Manual Bellavista V4.3 Rev02Thanh TùngNo ratings yet
- Weaning From Mechanical Ventilation in Intensive Care UnitsDocument2 pagesWeaning From Mechanical Ventilation in Intensive Care UnitsKinesiólogos UPC HPMNo ratings yet
- That May Used in Neurological Ward: Miguelito M. GultianoDocument32 pagesThat May Used in Neurological Ward: Miguelito M. GultianoLecery Sophia WongNo ratings yet
- ArdsDocument53 pagesArdslovelots1234No ratings yet
- ABC of Intensive CareDocument49 pagesABC of Intensive CareCurro MirallesNo ratings yet
- Aims of Obstetric Critical Care Management 160303161653 PDFDocument25 pagesAims of Obstetric Critical Care Management 160303161653 PDFNinaNo ratings yet
- Anmedic Service ManualDocument148 pagesAnmedic Service ManualPiotr Okorski0% (1)
- Critical Care Clinical Procedures 2023Document38 pagesCritical Care Clinical Procedures 2023nucahersheyskatNo ratings yet
- Тема 12 Англ Resuscitation Basic ConceptsDocument11 pagesТема 12 Англ Resuscitation Basic ConceptsMihika GuptaNo ratings yet
- Vent Weaning Ped22Document9 pagesVent Weaning Ped22Obed AhumadaNo ratings yet
- Chapter 03Document23 pagesChapter 03alqahtaniabdullah271No ratings yet
- DYSINCRHONY kjccm-2017-00535Document16 pagesDYSINCRHONY kjccm-2017-00535jose torresNo ratings yet
- Case Scenario - Week 4 - Group 2Document34 pagesCase Scenario - Week 4 - Group 2Angel Hannah100% (1)
- Case Study For Acute Respiratory FailureDocument10 pagesCase Study For Acute Respiratory FailureGabbii CincoNo ratings yet
- Anesthesia UnitsDocument92 pagesAnesthesia Unitsbiomedmaulik100% (2)
- Penlon AV-S Ventilator - Service ManualDocument102 pagesPenlon AV-S Ventilator - Service Manualleuman85100% (3)
- Overview Ventilation ModesDocument18 pagesOverview Ventilation ModesDo NodsNo ratings yet
- 10035480AM00 - Product Requirements Document PDFDocument67 pages10035480AM00 - Product Requirements Document PDFgameel alabsiNo ratings yet
- Status Asthmaticus in ChildrenDocument76 pagesStatus Asthmaticus in ChildrenJesterCruzNo ratings yet
- EXPRESS Trial 2008Document10 pagesEXPRESS Trial 2008Dr. Sergio Oscar AlunniNo ratings yet
- 10 1097@CCM 0b013e31818b35f2Document7 pages10 1097@CCM 0b013e31818b35f2omarihuanoNo ratings yet
- Atls by DR Moges - 082701Document64 pagesAtls by DR Moges - 082701moges beletachawNo ratings yet
- CRT Exam Review Guide Chapter 15Document27 pagesCRT Exam Review Guide Chapter 15Dharlyn MungcalNo ratings yet
- Acute Biologic CrisisDocument385 pagesAcute Biologic CrisisSheryl Ann Barit PedinesNo ratings yet