Professional Documents
Culture Documents
Critical Care Management of Covid-19 Algorithm-Eng
Uploaded by
Mr CROWOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Critical Care Management of Covid-19 Algorithm-Eng
Uploaded by
Mr CROWCopyright:
Available Formats
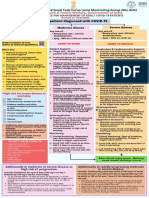
WHO/AFRO: RESPONSE
TO COVID-19 OUTBREAK
CRITICAL CARE MANAGEMENT OF COVID-19 ALGORITHM
• Fitted masks, gloves, gown, eye protection for aerosol generating procedures
INFECTION
• Perform aerosol generating procedures (AGPs) in a negative pressure room
CONTROL
• Surgical masks, gloves ,gown,eye protection for HCWs caring for non-ventilated or venti-
PRINCIPLES lated (closed circuit) COVID-19 patients if non AGPs being performed
• Start supplemental oxygen if SPO₂<90%, target SPO₂ 92-96
• Escalation to HFNC for acute hypoxemic respiratory failure despite conventional oxygen
therapy
• Trial of NIPPV if HFNC unavailable, and there is no urgent indication for intubation (close
monitoring needed for respiratory status deterorioration)
• Intubation for patients with urgent indication to be done by the most experienced, in a
RESPIRATORY negative pressure room
MANAGEMENT • Tidal volume 4-8 ml/kg PBW, for mechanically ventilated adults with ARDS
• Plateau pressure<30 cmH₂O and higher PEEP for mechanically ventilated patients
• Prone ventilation for 12-16 hours in mechanically ventilated patients with moderate-severe
ARDS
• Deep sedation for mechanically ventilated patients with moderate-severe ARDS, with NMBA
as needed to prevent dyssynchrony
• Haemodynamic management:
• Bufferd crystalloids for fluid resuscitation in shock
• Noradrenaline as 1st line vasoactive agent for fluid refractory shock, adrenaline or
vasopressin as alternatives( target MAP 60-65 mmHg)
• Low dose hydrocortisone for catecholamine refractory shock
• Conservative over liberal fluid management strategy
• Paracetamol for pyrexia management
SUPPORTIVE • Empirical antimicrobial/antibacterial therapy for mechanically ventilated patients in
MANAGEMENT respiratory failure (regular assessment for de escalation)
• Nutrition
• Early enteral nutrition (EN), within 12 hrs of intubation or 24-36 hrs of ICU admission;
start low and advance to 80% goal by the end of the 1st week (Incorporate macro and
micronutrients)
• Switch to pareneteral nutrition if EN via gastrc feeding is not an option
• Effective and empathetic communication to critically ill patients with COVID-19; initiating
pyschosocial support strategies
• Venous thrombo- prophylaxis (chemical or mechanical)
ARDS-Acute respiratory distress syndrome; HCWs-Health care workers; HFNC-High flow nasal cannula; ICUIntensive care unit; MAP-Mean arterial pressure;
NIPPV-Non-invasive positive pressure ventilation; NMBANeuromuscular blocking agent; PEEP-Positive end expiratory pressure; PBW-Predicted body weight
Adapted from:
1. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). ESICM2020
2. World Health Organization Clinical Management of COVID-19. Interim Guidance. May 2020
You might also like
- 2021 ACLS Study GuideDocument20 pages2021 ACLS Study GuideShane Brown83% (12)
- FNCP PrioritizationDocument10 pagesFNCP Prioritizationleslie_macasaet100% (6)
- NURS612 Exam 1 Review-Chen Walta - Week1-3Document15 pagesNURS612 Exam 1 Review-Chen Walta - Week1-3A Marie100% (1)
- Bipap Ventilation Basic and MonitoringDocument33 pagesBipap Ventilation Basic and MonitoringPradip ChougaleNo ratings yet
- RFH COVID-19 ICU Resource Pack FULL PDFDocument15 pagesRFH COVID-19 ICU Resource Pack FULL PDFQuique GarciaNo ratings yet
- Congenital AnomaliesDocument54 pagesCongenital Anomaliesthiruilayavan83% (6)
- Module 9 Mechanical Ventilation PDFDocument46 pagesModule 9 Mechanical Ventilation PDFChabboo SutabrataNo ratings yet
- AIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaSomnath Das GuptaNo ratings yet
- Jama Poston 2020 Gs 200003Document3 pagesJama Poston 2020 Gs 200003Alex Fernando Páez VallejoNo ratings yet
- SSC COVID19GuidelinesRecTable FirstUpdateDocument5 pagesSSC COVID19GuidelinesRecTable FirstUpdatesatya.drNo ratings yet
- Lecture Anwar Ventilation Managment COVIDDocument28 pagesLecture Anwar Ventilation Managment COVIDمحمدرزازالتبعيNo ratings yet
- AIIMS COVID Doc 1.6.1-1Document1 pageAIIMS COVID Doc 1.6.1-1mbhangaleNo ratings yet
- AIIMS COVID Algorithm 1.5-1 PDFDocument1 pageAIIMS COVID Algorithm 1.5-1 PDFAnutosh BhaskarNo ratings yet
- COVID19 Management Algorithm 22042021 v1Document1 pageCOVID19 Management Algorithm 22042021 v1shivani shindeNo ratings yet
- Prehospital Protocol Handbook: Dr.V.P.Chandrasekharan M.D., Dip (A&E)Document70 pagesPrehospital Protocol Handbook: Dr.V.P.Chandrasekharan M.D., Dip (A&E)Sudhir PaulNo ratings yet
- NCM 118 Lec Prelim 2Document13 pagesNCM 118 Lec Prelim 2SammNo ratings yet
- Critical Decisions in Airway ManagementDocument43 pagesCritical Decisions in Airway ManagementPablo RamirezNo ratings yet
- TRANS - UGIB CPG - PSG - Philippine Consensus Statements On The Management of NonDocument3 pagesTRANS - UGIB CPG - PSG - Philippine Consensus Statements On The Management of NonNonoy JoyaNo ratings yet
- NIV (Non-Invasive Ventilation) : Dr.S.MagimaiguberanDocument38 pagesNIV (Non-Invasive Ventilation) : Dr.S.MagimaiguberanDr mahi sNo ratings yet
- Recovery Room Care: BY Rajeev KumarDocument50 pagesRecovery Room Care: BY Rajeev Kumarramanrajesh83No ratings yet
- BNM Covid FrancesDocument4 pagesBNM Covid FrancesMISSAEL ESPINOZANo ratings yet
- Module 8 SepsisDocument44 pagesModule 8 SepsisEstefania Cuta HernandezNo ratings yet
- Auto-Peep (Intrinsic Peep)Document49 pagesAuto-Peep (Intrinsic Peep)Spring Bommie100% (1)
- Acute Chest Syndrome (ACS) CCGDocument11 pagesAcute Chest Syndrome (ACS) CCGJessa MaeNo ratings yet
- Practice Guidelines For Juniors 01 June 2016Document3 pagesPractice Guidelines For Juniors 01 June 2016ElaineNo ratings yet
- Acute Respiratory Distress SyndromeDocument26 pagesAcute Respiratory Distress Syndromethea waaniNo ratings yet
- Case Discussion - MombaelDocument29 pagesCase Discussion - MombaelLouije MombzNo ratings yet
- Society For Obesity and Bariatric Anaesthesia: OS-MRS Calculator Tools - Farmacologiaclinica.infoDocument1 pageSociety For Obesity and Bariatric Anaesthesia: OS-MRS Calculator Tools - Farmacologiaclinica.infoHizami Norddin100% (2)
- Appendix 4b - NIV Algorithm (ICHT)Document1 pageAppendix 4b - NIV Algorithm (ICHT)Josi JeremiaNo ratings yet
- Aspiration Pneumo GuidelinesDocument3 pagesAspiration Pneumo GuidelinesBlessing KelechiNo ratings yet
- Infeksi Bedah & Surviving Sepsis ChampaignDocument22 pagesInfeksi Bedah & Surviving Sepsis ChampaignHafiz AlfarizieNo ratings yet
- Prone Position Guidelines-2Document14 pagesProne Position Guidelines-2SAMINo ratings yet
- Aerovent, Apovent Atronase, Ipraxa, Ipvent Rhinovent, Rinatecrinovagos, Atrovent, Atrovent HfaDocument4 pagesAerovent, Apovent Atronase, Ipraxa, Ipvent Rhinovent, Rinatecrinovagos, Atrovent, Atrovent HfaGwyn RosalesNo ratings yet
- Adult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAdult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of Indiapramodbankhele3845No ratings yet
- NIPPVDocument35 pagesNIPPVAnusha VergheseNo ratings yet
- Critical Care of Patient With Covid 19Document32 pagesCritical Care of Patient With Covid 19Anonymous Kv0sHqFNo ratings yet
- NIV ProformaDocument10 pagesNIV ProformaWael N Sh GadallaNo ratings yet
- Management Guidelines For COVID 19 in Resource Limited Settings - MOH - NUG July 2021Document11 pagesManagement Guidelines For COVID 19 in Resource Limited Settings - MOH - NUG July 2021MYo OoNo ratings yet
- COVID 19 MG Protocol FinalDocument13 pagesCOVID 19 MG Protocol FinalajiNo ratings yet
- Cpap - IanDocument20 pagesCpap - IananggrainiNo ratings yet
- Noninvasive Ventilation in Acute Respiratory Failure in AdultsDocument12 pagesNoninvasive Ventilation in Acute Respiratory Failure in AdultsferrevNo ratings yet
- Application of Bipap Through Endotracheal Tube in Comatose Patients With Copd ExacerbationDocument5 pagesApplication of Bipap Through Endotracheal Tube in Comatose Patients With Copd ExacerbationMayco BiasibettiNo ratings yet
- Satuan Acara Bermain OrigamiiiiiiiiiiiiiDocument14 pagesSatuan Acara Bermain OrigamiiiiiiiiiiiiiatikaNo ratings yet
- Management of Acute Respiratory Failure in COVID-PUI Patient - Updated Feb. 2021Document7 pagesManagement of Acute Respiratory Failure in COVID-PUI Patient - Updated Feb. 2021Abhishek GoelNo ratings yet
- Slaid CNE Basics of Parenteral Nutrition & Its AdministrationDocument32 pagesSlaid CNE Basics of Parenteral Nutrition & Its AdministrationMohammad Nidzam Badrul HishamNo ratings yet
- Perioperatif NORADocument26 pagesPerioperatif NORAHeru Fajar SyaputraNo ratings yet
- Terapi Oxygen Pada Pasien Covd-19Document24 pagesTerapi Oxygen Pada Pasien Covd-19normamNo ratings yet
- AnaConda Device in Critical CareDocument14 pagesAnaConda Device in Critical CaredistopicmagNo ratings yet
- Non-Invasive Ventilation in Acute Respiratory Failure: Bts GuidelineDocument21 pagesNon-Invasive Ventilation in Acute Respiratory Failure: Bts GuidelineddubbNo ratings yet
- Anticoagulatio N Asra Guidelines: Sravya VemuriDocument62 pagesAnticoagulatio N Asra Guidelines: Sravya VemuriSiva Prasad AspNo ratings yet
- Nutrition and Fluid Therapy: CroupDocument2 pagesNutrition and Fluid Therapy: CroupnasibdinNo ratings yet
- TivaDocument38 pagesTivasunny kumar100% (1)
- Non-Invasive Ventilation 2Document25 pagesNon-Invasive Ventilation 2Ramanesh DNo ratings yet
- Anaesthesia For Trauma PatientsDocument42 pagesAnaesthesia For Trauma PatientsMerindukan Surga MuNo ratings yet
- I Putu Pramana ERAS in NeuroAnesthesiaDocument46 pagesI Putu Pramana ERAS in NeuroAnesthesiaPutuNo ratings yet
- Id 1300Document11 pagesId 1300ShadowruneNo ratings yet
- TASH Empirical Antibiotic Treatment Guidelines - 2018 Hospital and Ventilator Associated Pneumonia (HAP and VAP)Document2 pagesTASH Empirical Antibiotic Treatment Guidelines - 2018 Hospital and Ventilator Associated Pneumonia (HAP and VAP)ጉራማይሌ TubeNo ratings yet
- Airway Covid - 19Document37 pagesAirway Covid - 19Monica Herdiati Rukmana NaibahoNo ratings yet
- Noninvasive Ventilation in ChildrenDocument96 pagesNoninvasive Ventilation in ChildrenbhongskirnNo ratings yet
- WB Covid Protocol Book 25.09 .20 (1)Document49 pagesWB Covid Protocol Book 25.09 .20 (1)El MirageNo ratings yet
- SOPProningNonIntubated PatientFinal - 05182020 PDFDocument12 pagesSOPProningNonIntubated PatientFinal - 05182020 PDFzaenab anissaNo ratings yet
- Pharmacology for Student and Pupil Nurses and Students in Associated ProfessionsFrom EverandPharmacology for Student and Pupil Nurses and Students in Associated ProfessionsNo ratings yet
- Modern Anaesthesia:: A Concise Guide to the Study and Practice of Anaesthesia.From EverandModern Anaesthesia:: A Concise Guide to the Study and Practice of Anaesthesia.No ratings yet
- Tachypnea Is A Useful Predictor of Pneumonia in Children With Acute Respiratory InfectionDocument2 pagesTachypnea Is A Useful Predictor of Pneumonia in Children With Acute Respiratory InfectionAli BabaNo ratings yet
- A Small Measure of Peace Hans ZimmerDocument4 pagesA Small Measure of Peace Hans Zimmercrystaltouch123No ratings yet
- Vaccination Harm Part 1Document13 pagesVaccination Harm Part 1Roberto FortuNo ratings yet
- Radiological SignDocument3 pagesRadiological SignMuhammad BilalNo ratings yet
- Primay Health CentresDocument100 pagesPrimay Health CentresBirupakshya RoutNo ratings yet
- GHP Part 1 - Brown Dog TickDocument8 pagesGHP Part 1 - Brown Dog TickDigitalGeeksNo ratings yet
- Essay HI 4 LIADocument4 pagesEssay HI 4 LIANorbertus MarcellNo ratings yet
- Philippines Microplanning Guide: Reaching Every Purok Measles EliminationDocument30 pagesPhilippines Microplanning Guide: Reaching Every Purok Measles EliminationBe NjNo ratings yet
- BHI Homeopathic TherapyDocument132 pagesBHI Homeopathic Therapysanjay100% (4)
- Impact of Covid-19Document9 pagesImpact of Covid-19adane yehualawNo ratings yet
- Eap Academic Writing SkillsDocument59 pagesEap Academic Writing SkillsSiti Maisarah Mohamad Hadzri100% (2)
- Tugas Jurnal 2Document12 pagesTugas Jurnal 2RahmaNo ratings yet
- Sera, Maryam S. Bsce2B CW 101 Final Exam: 1. Will COVID-19 Kill Globalization?Document2 pagesSera, Maryam S. Bsce2B CW 101 Final Exam: 1. Will COVID-19 Kill Globalization?Maryam SeraNo ratings yet
- Onychomycosis Guidelines 2014 PDFDocument22 pagesOnychomycosis Guidelines 2014 PDFChayagon MongkonsawatNo ratings yet
- Integrating The "3 Minute" Tobacco Cessation Intervention in DAILY PracticeDocument50 pagesIntegrating The "3 Minute" Tobacco Cessation Intervention in DAILY PracticeNurses For Tobacco ControlNo ratings yet
- Pasa-BUY: " " Opportunity SectionDocument3 pagesPasa-BUY: " " Opportunity SectionPeter Cranzo MeisterNo ratings yet
- Micro para - CompiledDocument94 pagesMicro para - CompiledJanie-Vi GorospeNo ratings yet
- Republic Act No 11332Document6 pagesRepublic Act No 11332AnnyleneMauricioNo ratings yet
- IMPH Pandemic Report 2022Document96 pagesIMPH Pandemic Report 2022Sophie Keyes HogeNo ratings yet
- CF Recipes BangladeshDocument36 pagesCF Recipes BangladeshJoelyn Fatima BurnardNo ratings yet
- Prometric 29-2015Document9 pagesPrometric 29-2015asma .sassiNo ratings yet
- The African Post Covid-19 RealityDocument2 pagesThe African Post Covid-19 RealityJeremiah IgwurubeNo ratings yet
- Ode of The Jade Dragon Yu Long Fu PDFDocument10 pagesOde of The Jade Dragon Yu Long Fu PDFAikido EurogetNo ratings yet
- MiasmsDocument12 pagesMiasmswhiteyasmin100% (1)
- Frankincense Essential Oil - 25 Ways To Use ItDocument2 pagesFrankincense Essential Oil - 25 Ways To Use ItTrenkc VyrsNo ratings yet
- Indro HandojoDocument8 pagesIndro Handojonur syofiNo ratings yet
- Pediatric Appendicitis ScoreDocument6 pagesPediatric Appendicitis ScorePinandhito LatukolanNo ratings yet