Professional Documents
Culture Documents
COVID19 Management Algorithm 22042021 v1
Uploaded by
shivani shinde0 ratings0% found this document useful (0 votes)
116 views1 pageCOVID19 Management Algorithm 22042021 v1
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCOVID19 Management Algorithm 22042021 v1
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
116 views1 pageCOVID19 Management Algorithm 22042021 v1
Uploaded by
shivani shindeCOVID19 Management Algorithm 22042021 v1
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
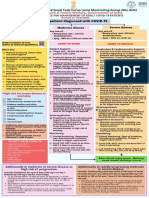
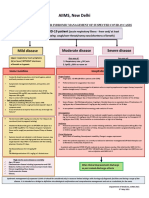
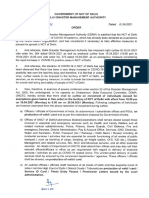
AIIMS/ ICMR-COVID-19 National Task Force/Joint
Monitoring Group (Dte.GHS)
Ministry of Health & Family Welfare, Government of India
CLINICAL GUIDANCE FOR MANAGEMENT OF ADULT COVID-19 PATIENTS
22nd April 2021
COVID-19 patient
Mild disease Moderate disease Severe disease
Upper respiratory tract symptoms Any one of: Any one of:
(&/or fever) WITHOUT shortness 1. Respiratory rate > 24/min, breathlessness 1. Respiratory rate >30/min, breathlessness
of breath or hypoxia 2. SpO2: 90% to < 93% on room air 2. SpO2 < 90% on room air
Home Isolation & Care ADMIT IN WARD ADMIT IN ICU
Oxygen Support: Respiratory support
MUST DOs ➢ Target SpO2: 92-96% (88-92% in patients with COPD). • Consider use of NIV (Helmet or face mask interface
✓ Physical distancing, indoor mask depending on availability) in patients with increasing
use, strict hand hygiene. ➢ Preferred devices for oxygenation: non-rebreathing face oxygen requirement, if work of breathing is LOW.
✓ Symptomatic management mask. • Consider use of HFNC in patients with increasing oxygen
(hydration, anti-pyretics, anti- requirement.
tussive, multivitamins). ➢ Awake proning encouraged in all patients requiring • Intubation should be prioritized in patients with high
✓ Stay in contact with treating supplemental oxygen therapy (sequential position work of breathing /if NIV is not tolerated.
physician. changes every 2 hours). • Use conventional ARDSnet protocol for ventilatory
management.
✓ Monitor temperature and oxygen
Anti-inflammatory or immunomodulatory therapy
saturation (by applying a SpO2
➢ Inj. Methylprednisolone 0.5 to 1 mg/kg in 2 divided Anti-inflammatory or immunomodulatory therapy
probe to fingers).
doses (or an equivalent dose of dexamethasone) usually • Inj Methylprednisolone 1 to 2mg/kg IV in 2 divided
Seek immediate medical attention if: for a duration of 5 to 10 days. doses (or an equivalent dose of dexamethasone) usually
o Difficulty in breathing ➢ Patients may be initiated or switched to oral route if for a duration 5 to 10 days.
o High grade fever/severe cough, stable and/or improving.
particularly if lasting for >5 days Anticoagulation
o A low threshold to be kept for
Anticoagulation • Weight based intermediate dose prophylactic
➢ Conventional dose prophylactic unfractionated heparin unfractionated heparin or Low Molecular Weight
those with any of the high-risk
or Low Molecular Weight Heparin (weight based e.g., Heparin (e.g., Enoxaparin 0.5mg/kg per dose SC BD).
features* enoxaparin 0.5mg/kg per day SC). There should be no There should be no contraindication or high risk of
contraindication or high risk of bleeding. bleeding.
MAY DOs
Monitoring Supportive measures
Therapies based on low certainty of
➢ Clinical Monitoring: Work of breathing, Hemodynamic • Maintain euvolemia (if available, use dynamic measures
evidence
instability, Change in oxygen requirement. for assessing fluid responsiveness).
➢ Tab Ivermectin (200 mcg/kg once • If sepsis/septic shock: manage as per existing protocol
➢ Serial CXR; HRCT chest to be done ONLY If there is and local antibiogram.
a day for 3 days). Avoid in
worsening. •
pregnant and lactating women.
Monitoring
OR ➢ Lab monitoring: CRP and D-dimer 48 to 72 hrly; CBC, • Serial CXR; HRCT chest to be done ONLY if there is
➢ Tab HCQ (400 mg BD for 1 day f/b KFT, LFT 24 to 48 hrly; IL-6 levels to be done if worsening.
400 mg OD for 4 days) unless deteriorating (subject to availability). • Lab monitoring: CRP and D-dimer 24-48 hourly; CBC,
contraindicated. KFT, LFT daily; IL-6 to be done if deteriorating (subject to
❖ Inhalational Budesonide (given availability).
via Metered dose inhaler/ Dry
powder inhaler) at a dose of 800
mcg BD for 5 days) to be given if After clinical improvement, discharge
symptoms (fever and/or cough)
as per revised discharge criteria.
are persistent beyond 5 days of
disease onset.
EUA/Off label use (based on limited available evidence and only in specific circumstances):
➢ Remdesivir (EUA) may be considered ONLY in patients with
*High-risk for severe disease or mortality o Moderate to severe disease (requiring SUPPLEMENTAL OXYGEN), AND
✓ Age > 60 years o No renal or hepatic dysfunction (eGFR <30 ml/min/m2; AST/ALT >5 times ULN (Not an
✓ Cardiovascular disease, hypertension, and CAD absolute contradiction), AND
✓ DM (Diabetes mellitus) and other immunocompromised o Who are within 10 days of onset of symptom/s.
states
❖ Recommended dose: 200 mg IV on day 1 f/b 100 mg IV OD for next 4 days.
✓ Chronic lung/kidney/liver disease
o Not to be used in patients who are NOT on oxygen support or in home settings
✓ Cerebrovascular disease
✓ Obesity
➢ Tocilizumab (Off-label) may be considered when ALL OF THE BELOW CRITERIA ARE MET
o Presence of severe disease (preferably within 24 to 48 hours of onset of severe
disease/ICU admission).
o Significantly raised inflammatory markers (CRP &/or IL-6).
o Not improving despite use of steroids.
o No active bacterial/fungal/tubercular infection.
❖ Recommended single dose: 4 to 6 mg/kg (400 mg in 60kg adult) in 100 ml NS over 1
hour.
➢ Convalescent plasma (Off label) may be considered ONLY WHEN FOLLOWING CRITERIA ARE MET
o Early moderate disease (preferably within 7 days of symptom onset, no use after 7 days).
o Availability of high titre donor plasma (Signal to cut-off ratio (S/O) >3.5 or equivalent
Department of Medicine, AIIMS (ND) depending on the test kit being used).
You might also like
- AIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaSomnath Das GuptaNo ratings yet
- AIIMS COVID Algorithm Ver 2.0Document1 pageAIIMS COVID Algorithm Ver 2.0jimjose antonyNo ratings yet
- INTERIM CLINICAL GUIDANCE FOR MANAGEMENT OF COVID-19Document1 pageINTERIM CLINICAL GUIDANCE FOR MANAGEMENT OF COVID-19mbhangaleNo ratings yet
- AIIMS COVID Algorithm 1.5-1 PDFDocument1 pageAIIMS COVID Algorithm 1.5-1 PDFAnutosh BhaskarNo ratings yet
- Adult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAdult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of Indiapramodbankhele3845No ratings yet
- AIIMS Issues New Guidelines For Treatment of CovidDocument7 pagesAIIMS Issues New Guidelines For Treatment of Covidsenthil kumarNo ratings yet
- AIIMS issues new guidelines for treatment of Covid-19 casesDocument7 pagesAIIMS issues new guidelines for treatment of Covid-19 casessenthil kumarNo ratings yet
- National Task Force Clinical Guidance for Managing Adult COVID-19 PatientsDocument1 pageNational Task Force Clinical Guidance for Managing Adult COVID-19 PatientsWhiteNo ratings yet
- COVID Clinical Management 14012022Document1 pageCOVID Clinical Management 14012022Naina DesaiNo ratings yet
- Laboratory Confirmed Covid 19 Patient: Department of Health & Family Welfare, Govt of West BengalDocument2 pagesLaboratory Confirmed Covid 19 Patient: Department of Health & Family Welfare, Govt of West BengalSujoyDeNo ratings yet
- Treatment Protocol Covid-19Document4 pagesTreatment Protocol Covid-19Shiv singhNo ratings yet
- WB Covid Protocol Book 25.09 .20 (1)Document49 pagesWB Covid Protocol Book 25.09 .20 (1)El MirageNo ratings yet
- COVID MX BsmmuDocument2 pagesCOVID MX BsmmuNuhiat NahreenNo ratings yet
- Brajac - ProtocolDocument13 pagesBrajac - Protocolthanh ngôNo ratings yet
- AIIMS Syndromic ApproachDocument1 pageAIIMS Syndromic ApproachRagul VNo ratings yet
- Management of Status Epilepticus 2022Document8 pagesManagement of Status Epilepticus 2022albert siraitNo ratings yet
- MX Protocol Book FinalDocument42 pagesMX Protocol Book FinalPawan ChoudharyNo ratings yet
- ConnectorDocument4 pagesConnectoryetaung8No ratings yet
- COVID-19 Infection in Children GuideDocument12 pagesCOVID-19 Infection in Children GuideSutirtha RoyNo ratings yet
- Respiratory Tract Infections - Med DidacticsDocument59 pagesRespiratory Tract Infections - Med Didacticsapi-649060644No ratings yet
- Nutrition and Fluid Therapy: CroupDocument2 pagesNutrition and Fluid Therapy: CroupnasibdinNo ratings yet
- Guideline For Management Protocol of Children With Fever and Respiratory SymptomsDocument44 pagesGuideline For Management Protocol of Children With Fever and Respiratory SymptomsKushagr GautamNo ratings yet
- Monkeypox Protocol - V1.0 (2047833421)Document5 pagesMonkeypox Protocol - V1.0 (2047833421)Syed AhmedNo ratings yet
- Bronchial AsthmaDocument45 pagesBronchial Asthmaprincesszahra6498No ratings yet
- Query 1 Modified Systematic ApproachDocument3 pagesQuery 1 Modified Systematic ApproachAntoNo ratings yet
- Evaluation and Management of Status Epilepticus in ChildrenDocument13 pagesEvaluation and Management of Status Epilepticus in ChildrenAyan BiswasNo ratings yet
- PrednisoneDocument3 pagesPrednisoneShaira TanNo ratings yet
- Pediatric Sepsis Topic DiscussionDocument5 pagesPediatric Sepsis Topic Discussionapi-602288180No ratings yet
- FluticasoneDocument3 pagesFluticasoneAmberNo ratings yet
- Carboprost 1Document3 pagesCarboprost 1angerson5100% (1)
- Bone and Joint Infection Treatment GuidelinesDocument3 pagesBone and Joint Infection Treatment GuidelinesDanissa Fidia PuteriNo ratings yet
- DIARRHEADocument12 pagesDIARRHEAtintin srgpnNo ratings yet
- Croup Summary PDFDocument2 pagesCroup Summary PDFnurfitriaNo ratings yet
- Antibiotic Guidelines For BONE AND JOINT INFECTIONSDocument3 pagesAntibiotic Guidelines For BONE AND JOINT INFECTIONSKhurram NadeemNo ratings yet
- COVID-19 Quick Reference Guide for Drugs & TreatmentDocument1 pageCOVID-19 Quick Reference Guide for Drugs & TreatmentBoules AtefNo ratings yet
- Paediatric Guidelines Nephrotic Syndrome 2018Document8 pagesPaediatric Guidelines Nephrotic Syndrome 2018lilydariniNo ratings yet
- General Principles of Antibiotic TherapyDocument44 pagesGeneral Principles of Antibiotic TherapyFadhly SharimanNo ratings yet
- CASE PRESENTATION PneumoniaDocument13 pagesCASE PRESENTATION PneumoniaHari Singh RathoreNo ratings yet
- COVID-19 Treatment GuidelinesDocument26 pagesCOVID-19 Treatment GuidelinesStonefalconNo ratings yet
- COVID-19 Positive Patient - Dexamethasone GuidanceDocument2 pagesCOVID-19 Positive Patient - Dexamethasone GuidanceLe Hoang TuanNo ratings yet
- PARGAD - CON1A - Module 11 Assignment (Endocrine Drugs and Diabetes Mellitus Drugs)Document9 pagesPARGAD - CON1A - Module 11 Assignment (Endocrine Drugs and Diabetes Mellitus Drugs)Samantha PargadNo ratings yet
- Methylprednisolone Drug Profile and Nursing ConsiderationsDocument4 pagesMethylprednisolone Drug Profile and Nursing ConsiderationsadryananestesiNo ratings yet
- 4_5780761539279587778Document2 pages4_5780761539279587778ጉራማይሌ TubeNo ratings yet
- Child With Fits in ED - Srl.Document2 pagesChild With Fits in ED - Srl.azeemNo ratings yet
- CH 040 Evaluation and Management of Status Epilepticus in ChildrenDocument7 pagesCH 040 Evaluation and Management of Status Epilepticus in Childrensuheena.CNo ratings yet
- GHC Lower Respiratory Tract Antimicrobial Guideline V 3 FinalDocument19 pagesGHC Lower Respiratory Tract Antimicrobial Guideline V 3 FinalNicthe Ruiz RodríguezNo ratings yet
- NIV ProformaDocument10 pagesNIV ProformaWael N Sh GadallaNo ratings yet
- Suspected COVID-19 Cases Management in Triage HospitalsDocument6 pagesSuspected COVID-19 Cases Management in Triage HospitalsMuhamed RamadanNo ratings yet
- Ynhhs - Covid-19 Treatment Adult Algorithm 4.3.20Document10 pagesYnhhs - Covid-19 Treatment Adult Algorithm 4.3.20Ren SNo ratings yet
- Case Presentation Station 3B Drug Study ClinidineDocument6 pagesCase Presentation Station 3B Drug Study ClinidinehahahahaaaaaaaNo ratings yet
- Material, Vincent M. (Types of Anesthesia Used in Cesarean Section)Document22 pagesMaterial, Vincent M. (Types of Anesthesia Used in Cesarean Section)Vincent Maralit MaterialNo ratings yet
- Medications for Pain ManagementDocument8 pagesMedications for Pain ManagementapalestiNo ratings yet
- Status Epilepticus Pediatric DR - RPDocument4 pagesStatus Epilepticus Pediatric DR - RPAdnin NugrohoNo ratings yet
- Ncma 219 Rle ReviewerDocument7 pagesNcma 219 Rle ReviewerAngelica AdlawanNo ratings yet
- Recommendation For The Use of Antibiotics For The Treatment of InfectionDocument5 pagesRecommendation For The Use of Antibiotics For The Treatment of InfectionGem BorjaNo ratings yet
- Pediatric Acute Sepsis: Physician'S OrdersDocument4 pagesPediatric Acute Sepsis: Physician'S OrdersSughosh MitraNo ratings yet
- COVID-19 TREATMENT ADULT Algorithm 4.3.20Document10 pagesCOVID-19 TREATMENT ADULT Algorithm 4.3.20luizfelipenobresc5492100% (1)
- Dexamethasone Brand Name, Classifications, Indications and Nursing ConsiderationsDocument8 pagesDexamethasone Brand Name, Classifications, Indications and Nursing ConsiderationsChristine Joy CamachoNo ratings yet
- VVM Brochure 2021 Last Final - Low ResDocument24 pagesVVM Brochure 2021 Last Final - Low Resshivani shindeNo ratings yet
- AS243Document2 pagesAS243shivani shindeNo ratings yet
- MR AustraliareturnsworksofarttoindiaDocument2 pagesMR Australiareturnsworksofarttoindiashivani shindeNo ratings yet
- 2021 Manufacturing Risk IndexDocument17 pages2021 Manufacturing Risk Indexshivani shindeNo ratings yet
- Letter To CS UP 06.08.2021Document3 pagesLetter To CS UP 06.08.2021shivani shindeNo ratings yet
- Effects (Physical, Behavioural and Psycho-Social) of Using Mobile Phones and Other Devices With Internet Accessibility by ChildrenDocument42 pagesEffects (Physical, Behavioural and Psycho-Social) of Using Mobile Phones and Other Devices With Internet Accessibility by Childrenshivani shindeNo ratings yet
- Up AtsDocument2 pagesUp Atsshivani shindeNo ratings yet
- D STR Gci.01 2021 PDF eDocument172 pagesD STR Gci.01 2021 PDF enitsuga71No ratings yet
- 5 6334319687714734579Document4 pages5 6334319687714734579RepublicNo ratings yet
- India Embassy in AfghanistanDocument3 pagesIndia Embassy in Afghanistanshivani shindeNo ratings yet
- Delhi Court Grants Bail To Accused Deep Sidhu in Red Fort Violence CaseDocument20 pagesDelhi Court Grants Bail To Accused Deep Sidhu in Red Fort Violence Caseshivani shindeNo ratings yet
- PR Mallya Nirav and MehulfinalDocument2 pagesPR Mallya Nirav and Mehulfinalshivani shindeNo ratings yet
- Suspension Cum Showcause Notice Copy 396095Document6 pagesSuspension Cum Showcause Notice Copy 396095shivani shindeNo ratings yet
- Gangubai KathiawadiDocument4 pagesGangubai Kathiawadishivani shinde50% (2)
- Madras High Court Dismisses Dmks Plea Challenging Postal Ballots Provision in RP Act 390766Document55 pagesMadras High Court Dismisses Dmks Plea Challenging Postal Ballots Provision in RP Act 390766shivani shindeNo ratings yet
- ODNI Threat Assessment - 2021Document27 pagesODNI Threat Assessment - 2021Victor I NavaNo ratings yet
- In Re: Updated Terms of Service and Privacy Policy For Whatsapp UsersDocument21 pagesIn Re: Updated Terms of Service and Privacy Policy For Whatsapp Usersshivani shindeNo ratings yet
- Arin Khan Death Penalty Order Batla House EncounterDocument22 pagesArin Khan Death Penalty Order Batla House Encountershivani shindeNo ratings yet
- 4 AppleDocument9 pages4 AppleSam Peter GeorgieNo ratings yet
- Automotive Transmission-ShaftDocument7 pagesAutomotive Transmission-Shaftfileuse.fNo ratings yet
- Motor Vehicles and Road Traffic Regulation 48.50Document411 pagesMotor Vehicles and Road Traffic Regulation 48.50Clayton AllenNo ratings yet
- "Hybrid" Light Steel Panel and Modular Systems PDFDocument11 pages"Hybrid" Light Steel Panel and Modular Systems PDFTito MuñozNo ratings yet
- International Journal of Biopharmaceutics: Formulation and Evaluation of Ibuprofen Loaded Maltodextrin Based ProniosomeDocument7 pagesInternational Journal of Biopharmaceutics: Formulation and Evaluation of Ibuprofen Loaded Maltodextrin Based ProniosomeNeng NurtikaNo ratings yet
- Electrical design for proposed residential buildingDocument24 pagesElectrical design for proposed residential buildingMALABIKA MONDALNo ratings yet
- Power Converters Simulation Lab Manual - (2015-2016)Document41 pagesPower Converters Simulation Lab Manual - (2015-2016)Leela KrishnaNo ratings yet
- The Threat Landscape Quiz ResultsDocument5 pagesThe Threat Landscape Quiz ResultsKaskusemail88 EmailNo ratings yet
- Project Report ON: "Brand Preference of Onida Colour TV in Coastal OrissaDocument66 pagesProject Report ON: "Brand Preference of Onida Colour TV in Coastal OrissaApurba KhanduriNo ratings yet
- 802 11 Qos OverviewDocument38 pages802 11 Qos Overviewswapnil tiwariNo ratings yet
- 11.30 Imran Akram IA CementDocument12 pages11.30 Imran Akram IA CementParamananda SinghNo ratings yet
- Modified Castigliano TheoremDocument10 pagesModified Castigliano Theoremmszlazak4179No ratings yet
- BIM Implementation - Brenner Base Tunnel ProjectDocument10 pagesBIM Implementation - Brenner Base Tunnel ProjectHichemNo ratings yet
- Test Bank For Web Development and Design Foundations With Html5 6 e 6th Edition 0132783398Document9 pagesTest Bank For Web Development and Design Foundations With Html5 6 e 6th Edition 0132783398Thomas White100% (23)
- Gmail - DFA Passport Appointment System - Confirmation Notification PDFDocument2 pagesGmail - DFA Passport Appointment System - Confirmation Notification PDFGarcia efrilNo ratings yet
- The Ultimate Press Release Swipe File by Pete Williams - SAMPLEDocument20 pagesThe Ultimate Press Release Swipe File by Pete Williams - SAMPLEPete Williams100% (9)
- GPS Consent and TrackingDocument3 pagesGPS Consent and TrackingJoel KionisalaNo ratings yet
- Harvard Algorithms cs124 NotesDocument6 pagesHarvard Algorithms cs124 NotesYamini DasguptaNo ratings yet
- Activity#tachometer - MEC 0326.1-2Document4 pagesActivity#tachometer - MEC 0326.1-2MarkJude MorlaNo ratings yet
- LG AnalysisDocument4 pagesLG AnalysisAnkit MishraNo ratings yet
- Join in SQLDocument9 pagesJoin in SQLSugeenaNo ratings yet
- Motion in A Straight Line: Initial PositionDocument7 pagesMotion in A Straight Line: Initial PositionEngelbert Bicoy AntodNo ratings yet
- Exercise Application Linear EquationDocument4 pagesExercise Application Linear EquationWong Zhen FengNo ratings yet
- Insurance AppraisersDocument8 pagesInsurance AppraisersTanu Singh MBA-18No ratings yet
- Haslinda Mohd Anuar Senior Lecturer School of Law ColgisDocument24 pagesHaslinda Mohd Anuar Senior Lecturer School of Law ColgisSHAHEERANo ratings yet
- Strategic Human Resources Planning 5th Edition Belcourt Solutions ManualDocument25 pagesStrategic Human Resources Planning 5th Edition Belcourt Solutions ManualMarioAbbottojqd100% (52)
- Plaintiff's Original Petition: Uber Ridesharing DefendantDocument8 pagesPlaintiff's Original Petition: Uber Ridesharing DefendantWigingtonRumleyDunnBlairLLPNo ratings yet
- Copier CoDocument9 pagesCopier CoHun Yao ChongNo ratings yet
- Laptop PolicyDocument2 pagesLaptop PolicyKamal SharmaNo ratings yet
- Oracle Forms Developer 10G Student Guide - 1Document440 pagesOracle Forms Developer 10G Student Guide - 1Jayant Agarwal100% (3)