Professional Documents
Culture Documents
COVID Clinical Management 14012022
Uploaded by
Naina DesaiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
COVID Clinical Management 14012022
Uploaded by
Naina DesaiCopyright:
Available Formats
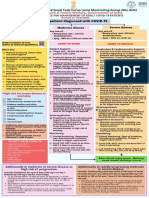
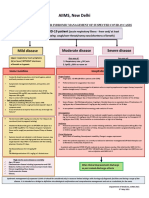
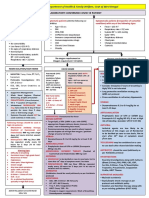
AIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte.
GHS)
Ministry of Health & Family Welfare, Government of India
CLINICAL GUIDANCE FOR MANAGEMENT OF ADULT COVID-19 PATIENTS
Revised on 14/01/2022
Adult patient diagnosed with COVID-19
Mild disease Moderate disease Severe disease
Any one of: Any one of:
Upper respiratory tract symptoms 1. Respiratory rate ≥ 24/min, 1. Respiratory rate >30/min,
and/or fever WITHOUT shortness breathlessness breathlessness
of breath or hypoxia 2. SpO2 < 90% on room air
2. SpO2 : 90% to ≤ 93% on room air
Home Isolation & Care ADMIT IN WARD
(Refer to relevant guideline) ADMIT IN HDU/ICU
MUST DOs Oxygen Support: Respiratory support:
Target SpO2 : 92-96% (88-92% in Consider use of NIV (Helmet or face mask
Physical distancing, indoor mask patients with COPD)
use, strict hand hygiene interface depending on availability) in
Preferred devices for oxygenation: patients with increasing oxygen
Symptomatic management non-rebreathing face mask requirement, if work of breathing is LOW
(hydration, anti-pyretics, anti-
tussive) Awake proning encouraged in all Consider use of HFNC in patients with
patients requiring supplemental increasing oxygen requirement
Stay in contact with treating oxygen therapy (sequential
physician Intubation should be prioritized in
position changes every 2 hours) patients with high work of breathing /if
Monitor temperature and oxygen NIV is not tolerated
saturation (by applying a SpO2 probe
Anti-inflammatory or
to fingers) immunomodulatory therapy: Use institutional protocol for ventilatory
Inj. Methylprednisolone 0.5 to 1 management when required
Seek immediate medical attention if: mg/kg in 2 divided doses (or an
equivalent dose of Anti-inflammatory or
Difficulty in breathing or SpO2 <93% dexamethasone) usually for a immunomodulatory therapy:
High grade fever/severe cough, duration of 5 to 10 days
Inj Methylprednisolone 1 to 2 mg/kg IV in
particularly if lasting for >5 days Patients may be initiated or 2 divided doses (or an equivalent dose of
A low threshold to be kept for those switched to oral route if stable dexamethasone) usually for a duration 5
with any of the high-risk features* and/or improving to 10 days
There is no evidence for benefit for Anti-inflammatory or
injectable steroids in those NOT immunomodulatory therapy (such as
MAY DOs requiring oxygen supplementation, steroids) can have risk of secondary
Therapies based on low certainty of or on continuation after discharge infection such as invasive mucormycosis
evidence especially for those with when used too early, at higher dose or for
high-risk of progression* Anti-inflammatory or
immunomodulatory therapy (such longer than required
as steroids) can have risk of
Inhalational Budesonide (given via secondary infection such as
Metered dose inhaler/ Dry powder invasive mucormycosis when used
inhaler) at a dose of 800 mcg BD for
Supportive measures:
too early, at higher dose or for Maintain euvolemia (if available, use
5 days) to be given if symptoms longer than required
(fever and/or cough) are persistent dynamic measures for assessing fluid
beyond 5 days of disease onset Anticoagulation: responsiveness)
Conventional dose prophylactic If sepsis/septic shock: manage as per
unfractionated heparin or Low existing protocol and local antibiogram
Molecular Weight Heparin (weight
*High-risk for severe disease or based e.g., enoxaparin 0.5mg/kg per
mortality day SC). There should be no Monitoring:
contraindication or high risk of
Age > 60 years Clinical Monitoring: work of breathing,
bleeding
Cardiovascular disease, Hemodynamic instability, Change in
Monitoring:
hypertension, and CAD oxygen requirement
Clinical Monitoring: breathing rate,
Diabetes mellitus and other Hemodynamic instability, Change Serial CXR; HRCT chest to be done ONLY
immunocompromised states (such in oxygen requirement if there is worsening
as HIV)
Serial CXR; HRCT chest to be done
Active tuberculosis ONLY if there is worsening Lab monitoring: CRP, D-dimer, blood
Chronic lung/kidney/liver disease sugar 48 to 72 hrly; CBC, KFT, LFT 24 to 48
Lab monitoring: CRP, D-dimer, hrly
Cerebrovascular disease blood sugar 48 to 72 hrly; CBC, KFT,
LFT 24 to 48 hrly
Obesity
If cough persists for more than 2-3 weeks, investigate for After clinical improvement, discharge
tuberculosis and other conditions as per revised discharge criteria
EUA/Off label use (based on limited available evidence and only in specific circumstances):
Remdesivir (EUA) may be considered ONLY in patients with
10 days of onset of symptoms, in those having moderate to severe disease (requiring supplemental
oxygen), but who are NOT on IMV or ECMO
Consider remdesivir for 5 days to treat hospitalized patients with COVID-19 (No evidence of benefit for
treatment more than 5 days)
NOT to be used in patients who are NOT on oxygen support or in home setting
Monitor for RFT and LFT (remdesivir not recommended if eGFR <30 ml/min/m2; AST/ALT >5 times UNL) (not
an absolute contraindication)
Recommended dose: 200 mg IV on day 1 followed by 100 mg IV OD for next 4 days
Tocilizumab may be considered when ALL OF THE BELOW CRITERIA ARE MET
Rapidly progressing COVID-19 needing oxygen supplementation or IMV and not responding adequately to
steroids (preferably within 24-48 hours of onset of severe disease/ ICU admission)
Preferably to be given with steroids
No active TB, fungal, systemic bacterial infection
Scan QR Code to access Clinical Long term follow up for secondary infections (such as reactivation of TB, Flaring of Herpes etc.)
guidance for management of adult Significantly raised inflammatory markers (CRP and/or IL-6)
COVID-19 patients
Recommended single dose: 4 to 6 mg/kg (400 mg in 60 kg adult) in 100 ml NS over 1 hour
You might also like
- Drug Study (Haloperidol)Document3 pagesDrug Study (Haloperidol)Mae Ann Bueno CastillonNo ratings yet
- A Text Book of Materia Medica and Therapeutics of Rare Homoeopathic Remedies by Oscar HansenDocument136 pagesA Text Book of Materia Medica and Therapeutics of Rare Homoeopathic Remedies by Oscar Hansensunnyjamiel75% (4)
- Drug Classification Action Indication Contraindication Nursing ResposibilitiesDocument10 pagesDrug Classification Action Indication Contraindication Nursing ResposibilitiesAngelicaNo ratings yet
- 8 Propofol Drug StudyDocument4 pages8 Propofol Drug Studyshadow gonzalez100% (1)
- 90 MCQsDocument18 pages90 MCQsMarielou CoutinhoNo ratings yet
- Pediatric Resucitation Pediatric Resucitation: Pgi Gasataya, Charisse Ann G Pgi Tabobo, Raymee TDocument30 pagesPediatric Resucitation Pediatric Resucitation: Pgi Gasataya, Charisse Ann G Pgi Tabobo, Raymee TCharisse Ann GasatayaNo ratings yet
- Medical Surgical Nursing Review NotesDocument209 pagesMedical Surgical Nursing Review Notesabusaifluay100% (1)
- CpapDocument33 pagesCpapAtikah Putri AtmojoNo ratings yet
- Neonatal and Pediatric Patient Assessment (Study Guide)Document17 pagesNeonatal and Pediatric Patient Assessment (Study Guide)Fatima Sherrisa SaliNo ratings yet
- Long Covid - The Long Covid Book for Clinicians and Sufferers - Away from Despair and Towards UnderstandingFrom EverandLong Covid - The Long Covid Book for Clinicians and Sufferers - Away from Despair and Towards UnderstandingNo ratings yet
- NCLEX Exam: Respiratory System Disorders (60 Questions) : CorrectDocument41 pagesNCLEX Exam: Respiratory System Disorders (60 Questions) : CorrectErica Veluz LuyunNo ratings yet
- Coronary Artery Disease Pathophysiology PDFDocument3 pagesCoronary Artery Disease Pathophysiology PDFMohd Amir Bin Bashir0% (1)
- 004 Practical-Manual PDFDocument72 pages004 Practical-Manual PDFRicardo Domingos100% (1)
- NCP CompilationDocument11 pagesNCP CompilationRene John FranciscoNo ratings yet
- VancomycinDocument1 pageVancomycinE100% (2)
- BudesonideDocument2 pagesBudesonideDiane Bonita HerreraNo ratings yet
- Mcce CanadaDocument436 pagesMcce CanadakabambaNo ratings yet
- NCP Activity IntoleranceDocument1 pageNCP Activity IntoleranceBen David100% (2)
- National Task Force Clinical Guidance for Managing Adult COVID-19 PatientsDocument1 pageNational Task Force Clinical Guidance for Managing Adult COVID-19 PatientsWhiteNo ratings yet
- Adult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAdult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of Indiapramodbankhele3845No ratings yet
- AIIMS COVID Algorithm Ver 2.0Document1 pageAIIMS COVID Algorithm Ver 2.0jimjose antonyNo ratings yet
- COVID19 Management Algorithm 22042021 v1Document1 pageCOVID19 Management Algorithm 22042021 v1shivani shindeNo ratings yet
- AIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaSomnath Das GuptaNo ratings yet
- AIIMS COVID Algorithm 1.5-1 PDFDocument1 pageAIIMS COVID Algorithm 1.5-1 PDFAnutosh BhaskarNo ratings yet
- INTERIM CLINICAL GUIDANCE FOR MANAGEMENT OF COVID-19Document1 pageINTERIM CLINICAL GUIDANCE FOR MANAGEMENT OF COVID-19mbhangaleNo ratings yet
- AIIMS Issues New Guidelines For Treatment of CovidDocument7 pagesAIIMS Issues New Guidelines For Treatment of Covidsenthil kumarNo ratings yet
- AIIMS issues new guidelines for treatment of Covid-19 casesDocument7 pagesAIIMS issues new guidelines for treatment of Covid-19 casessenthil kumarNo ratings yet
- AIIMS Syndromic ApproachDocument1 pageAIIMS Syndromic ApproachRagul VNo ratings yet
- FluticasoneDocument3 pagesFluticasoneAmberNo ratings yet
- Pharm Exam Ii NotesDocument24 pagesPharm Exam Ii Noteskatiana louisNo ratings yet
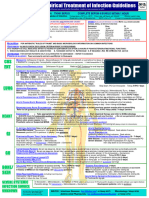
- Recommendation For The Use of Antibiotics For The Treatment of InfectionDocument5 pagesRecommendation For The Use of Antibiotics For The Treatment of InfectionGem BorjaNo ratings yet
- COVID-19 InterimGuidelines Treatment ENGDocument25 pagesCOVID-19 InterimGuidelines Treatment ENGMartin PaturlanneNo ratings yet
- WB Covid Protocol Book 25.09 .20 (1)Document49 pagesWB Covid Protocol Book 25.09 .20 (1)El MirageNo ratings yet
- Treatment Protocol Covid-19Document4 pagesTreatment Protocol Covid-19Shiv singhNo ratings yet
- WB COVID19 Latest Treatment ProtocolDocument1 pageWB COVID19 Latest Treatment ProtocolRahul AwasthiNo ratings yet
- Antibiotics-Generation OperationDocument5 pagesAntibiotics-Generation OperationZamzami Ahmad FahmiNo ratings yet
- COVID-19 InterimGuidelines Treatment ENGDocument24 pagesCOVID-19 InterimGuidelines Treatment ENGHouda LaatabiNo ratings yet
- GHC Lower Respiratory Tract Antimicrobial Guideline V 3 FinalDocument19 pagesGHC Lower Respiratory Tract Antimicrobial Guideline V 3 FinalNicthe Ruiz RodríguezNo ratings yet
- Meropenem Meropenem: (Lexi-Drugs Multinational)Document1 pageMeropenem Meropenem: (Lexi-Drugs Multinational)Jhoann JamanilaNo ratings yet
- Component 3: Pharmacologic TherapyDocument47 pagesComponent 3: Pharmacologic TherapypharmryadNo ratings yet
- PrednisoneDocument3 pagesPrednisoneShaira TanNo ratings yet
- Pedoman Penggunaan Antibiotik Pada PasienDocument5 pagesPedoman Penggunaan Antibiotik Pada PasienErvina Lie100% (1)
- Rheumatic Heart DDocument12 pagesRheumatic Heart DHein HtetNo ratings yet
- Croup Summary PDFDocument2 pagesCroup Summary PDFnurfitriaNo ratings yet
- CortisoneDocument2 pagesCortisoneJulioNo ratings yet
- DrugsDocument2 pagesDrugsgailannreyesNo ratings yet
- DrugsDocument2 pagesDrugsgailannreyesNo ratings yet
- Ventilator: Associated Pneumonia (VAP)Document36 pagesVentilator: Associated Pneumonia (VAP)D. Melba S.S ChinnaNo ratings yet
- Midazolam FinalDocument2 pagesMidazolam FinalAhmad AbqariNo ratings yet
- Adverse Effects of Anti Tubercular Drugs. MDR TBDocument75 pagesAdverse Effects of Anti Tubercular Drugs. MDR TBDr.U.P.Rathnakar.MD.DIH.PGDHM100% (1)
- DIPIRO 9th PHARMACOTHERAPY-PATOPHISIOLOGY APPROACH EDISI 9 (PDF - Io)Document31 pagesDIPIRO 9th PHARMACOTHERAPY-PATOPHISIOLOGY APPROACH EDISI 9 (PDF - Io)NingrumSindayaniNo ratings yet
- COVID-19 Guidelines for Management of PatientsDocument2 pagesCOVID-19 Guidelines for Management of PatientsSpecial OPD SVMCHRCNo ratings yet
- Nutrition and Fluid Therapy: CroupDocument2 pagesNutrition and Fluid Therapy: CroupnasibdinNo ratings yet
- Antibiotic hospital manDocument1 pageAntibiotic hospital manarshiya.manasekiNo ratings yet
- COVID - Management 14 April 2021Document20 pagesCOVID - Management 14 April 2021Zain ZaidiNo ratings yet
- Bronchial AsthmaDocument45 pagesBronchial Asthmaprincesszahra6498No ratings yet
- Drug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrDocument7 pagesDrug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrMary EnsomoNo ratings yet
- COVID MX BsmmuDocument2 pagesCOVID MX BsmmuNuhiat NahreenNo ratings yet
- COVID-19 Infection in Children GuideDocument12 pagesCOVID-19 Infection in Children GuideSutirtha RoyNo ratings yet
- Sedation & Analgesia in PICU: Goals, Tools and Adjuvant TherapyDocument21 pagesSedation & Analgesia in PICU: Goals, Tools and Adjuvant TherapyDr AhmedNo ratings yet
- Covid Drug TherapyDocument35 pagesCovid Drug TherapyNandha KumarNo ratings yet
- Methylprednisolone Drug Profile and Nursing ConsiderationsDocument4 pagesMethylprednisolone Drug Profile and Nursing ConsiderationsadryananestesiNo ratings yet
- Medical Ward Drug StudyDocument9 pagesMedical Ward Drug StudygorgeazNo ratings yet
- ASTHMA RestriveraDocument18 pagesASTHMA RestriveraAoi ShinNo ratings yet
- BNM Covid FrancesDocument4 pagesBNM Covid FrancesMISSAEL ESPINOZANo ratings yet
- Management of Acute Severe Asthma in PediatricsDocument53 pagesManagement of Acute Severe Asthma in PediatricsAmit AnandNo ratings yet
- Drug StudyDocument5 pagesDrug Studyboxed juiceNo ratings yet
- Top 5 Corticosteroids For Use in Emergency SettingsDocument4 pagesTop 5 Corticosteroids For Use in Emergency SettingsIulian Cătălin GrămadăNo ratings yet
- An Approach To Treating Long COVID: First Line TherapiesDocument3 pagesAn Approach To Treating Long COVID: First Line TherapiesflorentinaNo ratings yet
- Summary Antimicrobial Prescribing Guidance - July 21 For BNFDocument31 pagesSummary Antimicrobial Prescribing Guidance - July 21 For BNFbarcanbiancaNo ratings yet
- Drug Study23Document2 pagesDrug Study23Joh Acedo BantingNo ratings yet
- Directorate of Tourism, Govt. of Maharashtra: Mous Signed With Iprcl and MCDCDocument2 pagesDirectorate of Tourism, Govt. of Maharashtra: Mous Signed With Iprcl and MCDCNaina DesaiNo ratings yet
- News Letter World Tourism DayDocument1 pageNews Letter World Tourism DayNaina DesaiNo ratings yet
- Bombay High Court building opens for heritage walksDocument2 pagesBombay High Court building opens for heritage walksNaina DesaiNo ratings yet
- Press Note On New Adventure Tourism Policy Gets ApprovalDocument2 pagesPress Note On New Adventure Tourism Policy Gets ApprovalNaina DesaiNo ratings yet
- Press Note - Agri Tourism Traininge - EnglishDocument3 pagesPress Note - Agri Tourism Traininge - EnglishNaina DesaiNo ratings yet
- Format For Vendor/Service Provider Details (On Letter Head of Vendor Only)Document1 pageFormat For Vendor/Service Provider Details (On Letter Head of Vendor Only)Naina DesaiNo ratings yet
- Form GST REG-25: Government of India and Government of GujaratDocument1 pageForm GST REG-25: Government of India and Government of GujaratNaina DesaiNo ratings yet
- Vendor Code Vendor Name Vendor Code Vendor NameDocument2 pagesVendor Code Vendor Name Vendor Code Vendor NameNaina DesaiNo ratings yet
- COVID HOME CARE en 05012022Document1 pageCOVID HOME CARE en 05012022Deepak RanakotiNo ratings yet
- D) Ûfp G/P Z (B (0) T BFT (NFZ CF (JF V/U (GF (NFB, F (D (/JJF Afat: S, (S8Z SR (ZL4Document7 pagesD) Ûfp G/P Z (B (0) T BFT (NFZ CF (JF V/U (GF (NFB, F (D (/JJF Afat: S, (S8Z SR (ZL4Naina DesaiNo ratings yet
- Case ReportDocument14 pagesCase ReportJalalludin AnNo ratings yet
- Right-Sided Heart Failure: College of NursingDocument30 pagesRight-Sided Heart Failure: College of NursingMatelyn OargaNo ratings yet
- Mater PIR - Dr. Siti Chandra W., SP - KFR-K High Intensity Laser For Post COVID RehabilitationDocument20 pagesMater PIR - Dr. Siti Chandra W., SP - KFR-K High Intensity Laser For Post COVID RehabilitationGhea Putri HendrianiNo ratings yet
- Husel Lawsuit Against Mount Carmel-Trinity 12.26.19Document52 pagesHusel Lawsuit Against Mount Carmel-Trinity 12.26.19WOSUNo ratings yet
- P1 P2 Mastery Examination Reviewer in FNP LECTUREDocument34 pagesP1 P2 Mastery Examination Reviewer in FNP LECTUREMary Ann G. CorsanesNo ratings yet
- Palliative CareDocument82 pagesPalliative Carejoycebrenda348No ratings yet
- RT Skills ChecklistDocument3 pagesRT Skills ChecklistMond SantosNo ratings yet
- Correct Answer: 4. Premedicate The Client With An Analgesic Before AmbulatingDocument49 pagesCorrect Answer: 4. Premedicate The Client With An Analgesic Before AmbulatingPortage ExamsNo ratings yet
- History of Present IllnessDocument7 pagesHistory of Present IllnessBena GichiaNo ratings yet
- Massachusetts General Hospital (MGH) COVID-19 Treatment GuidanceDocument24 pagesMassachusetts General Hospital (MGH) COVID-19 Treatment Guidancerajesh BNo ratings yet
- Modern Management of Cardiogenic Pulmonary Edema: Amal Mattu, MD, Joseph P. Martinez, MD, Brian S. Kelly, MDDocument21 pagesModern Management of Cardiogenic Pulmonary Edema: Amal Mattu, MD, Joseph P. Martinez, MD, Brian S. Kelly, MDJoni MokodoNo ratings yet
- Implanted Venous Access Device (IVAD) - "Dome" or "Port"Document12 pagesImplanted Venous Access Device (IVAD) - "Dome" or "Port"JunkNo ratings yet
- Heart Failure Nursing Care Management - A Study GuideDocument16 pagesHeart Failure Nursing Care Management - A Study GuideJOSHUA DICHOSONo ratings yet
- COVID-19 visitor screening logDocument1 pageCOVID-19 visitor screening logۦۦ ۦۦNo ratings yet
- FU-M2-CU6 LEC Planning Phase-Towards Goals and Outcomes.Document6 pagesFU-M2-CU6 LEC Planning Phase-Towards Goals and Outcomes.Shiro KagomeNo ratings yet
- 04 MSDS Catalyst (Vandium Penta Oxide)Document6 pages04 MSDS Catalyst (Vandium Penta Oxide)Furqan SiddiquiNo ratings yet
- CVD Diagnosis and Clinical ManifestationsDocument4 pagesCVD Diagnosis and Clinical ManifestationsIca JustitiaNo ratings yet
- Respiratory System: Haitham N.KhalidDocument71 pagesRespiratory System: Haitham N.KhalidJockerNo ratings yet