Professional Documents
Culture Documents
Low-Volume High-Intensity Interval Training As A Therapy For Type 2 Diabetes
Uploaded by
Anna BartolomeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Low-Volume High-Intensity Interval Training As A Therapy For Type 2 Diabetes
Uploaded by
Anna BartolomeCopyright:
Available Formats
IJSM/5290/16.5.
2016/MPS Clinical Sciences
Low-Volume High-Intensity Interval Training as a
Therapy for Type 2 Diabetes
Authors C. Alvarez1, R. Ramirez-Campillo2, C. Martinez-Salazar3, R. Mancilla4, M. Flores-Opazo5, J. Cano-Montoya6,
E. G. Ciolac7
Affiliations Affiliation addresses are listed at the end of the article
Key words Abstract blood pressure (3.7 ± 0.5 mmHg), HDL-cholesterol
●
▶ blood pressure
▼ (21.1 ± 2.8 %), triglycerides (17.7 ± 2.8 %), endur-
Downloaded by: Serials Unit - Periodicals. Copyrighted material.
●
▶ body composition
Our purpose was to investigate the effects of low- ance performance (9.8 ±
1.0 %), body weight
●
▶ endurance performance
volume, high-intensity interval training (HIT) on (2.2 ± 0.3 %), BMI (2.1 ± 0.3 %), waist circumference
●
▶ glycemic control
cardiometabolic risk and exercise capacity in (4.0 ± 0.5 %) and subcutaneous fat (18.6 ± 1.4 %)
●
▶ high-intensity interval
exercise women with type 2 diabetes mellitus (T2DM). were found after HIT intervention. Patients of
●
▶ type 2 diabetes mellitus Sedentary overweight/obese T2DM women HIT group also showed reductions in daily dos-
(age = 44.5 ± 1.8 years; BMI = 30.5 ± 0.6 kg/m2) were age of antihyperglycemic and antihypertensive
randomly assigned to a tri-weekly running-based medication during follow-up. No changes were
HIT program (n = 13) or non-exercise control fol- found in any variable of CON group. The HIT-
low-up (CON; n = 10). Glycemic control, lipid and induced improvements occurred with a weekly
blood pressure levels, endurance performance, time commitment 56–25 % lower than the mini-
and anthropometry were measured before and mal recommended in current guidelines. These
after the follow-up (16 weeks) in both groups. findings suggest that low-volume HIT may be a
Medication intake was also assessed throughout time-efficient intervention to treat T2DM
the follow-up. Improvements (P < 0.05) on fasting women.
glucose (14.3 ± 1.4 %), HbA1c (12.8 ± 1.1 %), systolic
Introduction intensity interval training (HIT), which consist of
accepted after revision
March 01, 2016
▼ several bouts of high-intensity exercise inter-
Type 2 diabetes mellitus (T2DM) is a highly prev- spersed with intervals of rest or active recovery
alent disease associated with increased levels of [8], may have superior effects for improving gly-
Bibliography
morbidity, mortality and health care expendi- cemic control [10] and other health-related
DOI http://dx.doi.org/
10.1055/s-0042-104935 ture [28, 39]. Regular physical activity has been markers [5, 8,
37]. For example, HIT showed
Published online: 2016 recognized as an important tool for preventing greater improvements on cardiorespiratory fit-
Int J Sports Med and managing T2DM and its complications, ness [6, 7, 25, 31, 38], endothelial function and its
© Georg Thieme including glycemic control, cardiometabolic risk markers [6, 31], blood lipoprotein and glucose
Verlag KG Stuttgart · New York and psychological well-being [9]. In this context, [31], insulin sensitivity and fasting insulin [31, 32],
ISSN 0172-4622
physical activity is a first-line treatment for markers of sympathetic activity [6, 7] and arterial
T2DM patients, and a minimum of 150 min/wk stiffness [6, 13] compared to energy-expenditure-
Correspondence
(30 min, 5 d/wk) of moderate to vigorous aerobic matched continuous moderate exercise.
Prof. Dr. Emmanuel Gomes
Ciolac exercise, in association with 2–3 sessions per It is noteworthy that only 2 weeks (6 exercise
Departamento de Educação week of resistance training, has been recom- sessions) of low-volume HIT has shown improve-
Física mended in the current American Diabetes Asso- ments in glycemic control of T2DM patients
Faculdade de Ciências ciation and American College of Sports Medicine [20, 27]. Low-volume HIT is also time-efficient,
Universidade Estadual Paulista guidelines [9]. with a weekly time commitment (including
– UNESP
Continuous activities that causes a sustained warm-up, cool-down and rest periods) markedly
Av. Engenheiro Luiz Edmundo
Carrijo Coube 14-06
heart rate (HR) increase (i. e., walking, cycling or lower [10, 12,
20, 27] than current guidelines
17033-360 Bauru jogging at ~55–70 % of maximal HR) has been recommendation [9]. Given that most T2DM
Brazil commonly recommended to meet this aerobic patients are sedentary or insufficiently active
ciolac@fc.unesp.br exercise recommendation [9]. However, high- [24], and lack of time is the most frequently cited
Alvarez C et al. High-Intensity Exercise and Diabetes … Int J Sports Med
Clinical Sciences IJSM/5290/16.5.2016/MPS
barrier to regular exercise participation [33], these findings may mum of 70 % of exercise program compliance was required in
have important implications from a public health perspective. order for the intervention group patients to be included in the
However, low-volume HIT studies with T2DM patients are of final statistical analyses.
short-duration (only 2 weeks), small sample size, and lack an 84 T2DM women (age 35–55 years), with less than 5 years of
appropriate control group [10, 27]. Studies analyzing the effects diagnosis, patients of the Family Healthcare Center Tomas Rojas
of longer periods of low-volume HIT on glycemic control and of Los Lagos (Chile) that answered a telephone call with explana-
others treatments goals in T2DM are lacking (i. e., lipid and blood tions about the study protocol, agreed to participate in the pre-
pressure levels, drug therapy optimization) [9]. Thus, the aim of sent investigation. A structured medical records review and
the present study was to investigate the effects of 4 months of physical examination by a physician were performed in all
low-volume HIT on glycemic control, lipid and blood pressure patients for eligibility criteria assessment. 28 T2DM patients who
levels, endurance performance, medication intake and anthro- met all of the inclusion criteria were included in the present study
pometry of T2DM women. ▶ Fig. 1). Subjects were then randomly assigned in a 1:1 ratio to
( ●
16-week HIT (n = 14, age = 46.0 ± 3.0 years, BMI = 30.8 ± 1.0 kg/m2)
or non-exercise control (CON; n = 14, age = 43.0 ± 2.4 years,
Methods BMI = 30.6 ± 1.0 kg/m2) intervention, using a computer generated
▼ random assignment. Fasting glucose, HbA1c and lipids levels,
Population and study design resting blood pressure, endurance performance and anthropom-
We studied adult overweight or obese (BMI between 25 and etry were assessed before and after the 16-week follow-up in
35 kg/m2) adult women with established diagnosis of T2DM for both groups. All assessments were performed by examiner who
at least 12 months. Eligibility criteria included fasting hypergly- were blinded to the patients’ intervention group. Hypoglycemic
cemia > 126 mg · dL − 1 and glycated hemoglobin (HbA1c) ≥ 6.5 % medication intake was controlled throughout the follow-up and,
Downloaded by: Serials Unit - Periodicals. Copyrighted material.
[9], unchanged drug therapy during the previous 6 months, sed- if necessary, changes were performed following the recommen-
entary or insufficiently active life style (according to the Interna- dations to continue preventing hypoglycemia events in T2DM
tional Physical Activity Questionnaire previously validated in patients under regular exercise [1]. Patients in HIT group per-
Chilean population) [26], non-involvement in regular physical formed a tri-weekly progressive exercise program, which con-
activity or exercise program during the previous 6 months, and sisted of jogging/running intervals interspersed with recovery
family history of T2DM (mother and/or father). Patients with periods of low-intensity walking. Patients in CON group were
musculoskeletal disorders, cardiovascular contraindications to advised not to engage in any exercise/physical activity programs
exercise, history of stroke, asthma and chronic obstructive pul- during the study. All patients (HIT and CON) were oriented to
monary disease, long-term diabetic complications (history of maintain their daily living physical activity and dietary patterns
foot injury, retinopathy, nephropathy, and diabetic peripheral throughout the 16-week study period. The present study is in
neuropathy), or smokers were not included in the study. A mini- accordance with the ethical standards of the International Jour-
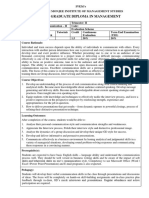
Fig. 1 Study design.
Enrollment Assessed for eligibility (n = 84)
Not included (n = 56)
Without T2DM family history (n = 22)
Musculoskeletal disorders (n = 2)
History of stroke (n = 1)
Asthma (n = 2)
Foot injury or history of foot injury (n = 7)
Altered electrocardiography (n = 4)
Nephropathy (n = 3)
Regular Physical Activity (n = 3)
Age ≥ 60 years (n = 5)
Address in rural areas (n = 7)
Randomization (n = 28)
Allocation
Allocated to HIT (n = 14) Allocated to CON (n = 14)
Follow-Up
Lost to follow-up (n = 4)
Lost to follow-up (n = 1)
Change of residence address (n = 2)
Exercise training compliance < 70 %
Change from health center (n = 2)
Analysis
Analyzed (n = 13) Analyzed (n = 10)
Alvarez C et al. High-Intensity Exercise and Diabetes … Int J Sports Med
IJSM/5290/16.5.2016/MPS Clinical Sciences
nal of Sports Medicine [14], and was approved by the ethics Electro Inc., Kempele, Finland). In order to warrant an accurate
committees of the Department of Physical Activity Sciences of test [19], patients were encouraged to walk faster if their heart
the University of Los Lagos and of the Family Healthcare Center rate was lower than 75 % of maximum age-predicted heart rate.
Tomás Rojas of Los Lagos. All volunteers read a detailed descrip- The time spent in walking the 2 km was measured and used for
tion of the study protocol and provided their written informed analysis. All tests were carried out between 8:00 and 10:00 a.m.
consent.
Exercise training intervention
Blood analyses Participants of HIT group performed a tri-weekly progressive
Blood samples (nearly 3.5 ml) were collected before and after the HIT program for 16 weeks. All exercise sessions were performed
16-week of follow-up, at morning and after a 10 h overnight fast- on a flat surface (indoor sports court), and supervised by an
ing. The post-training blood sampling of HIT patients were per- exercise specialist. The progressive HIT program was based on
formed at least 48 h after the last exercise session to avoid an high-intensity exercise intervals (jogging/running) interspersed
acute effect of exercise. Samples were immediately placed in ice with low-intensity active recovery (walking). Patients’ heart rate
and centrifuged at 4 000 rpm (1 700 × g) for 5 min at − 4 °C. Plasma was continuously monitored (ProTrainer 5™, Polar Electro Inc.,
samples were immediately transferred to pre-chilled microtubes Kempele, Finland). During all HIT sessions, patients were
and stored at − 20 °C for later analysis. HbA1c was analyzed by instructed by the exercise specialist to jog/run and walk using a
high performance liquid chromatography (Variant™ II Turbo steady pace, which should be controlled by maintaining a per-
Hemoglobin Testing System, Bio-Rad Inc., Hercules, CA, USA). ceived exertion between 15–17 (jogging/running) and < 9 (walk-
Plasma glucose, total cholesterol and triglycerides were ana- ing) in the 15-point rating of perceived exertion scale [2]. The
lyzed by enzymatic methods using standard kits (Wiener Lab goal was to reach 90–100 % and less than 70 % of their age pre-
Inc., Rosario, Argentina) on an automatic analyzer (Metrolab dicted reserve heart rate [18] at the end of each jogging/running
Downloaded by: Serials Unit - Periodicals. Copyrighted material.
2 300 Plus™, Metrolab Biomed Inc., Buenos Aires, Argentina). and walking interval, respectively. Thus, all patients were con-
Plasma HDL cholesterol was measured by the same enzymatic tinuously oriented to adjust their jogging/running or walking
method after phosphotungstate precipitation. LDL cholesterol pace, if their heart rate was not in the goal at the end of the pre-
levels were calculated using the Friedewald formula [11]. vious interval. The progressive HIT program started (week 1–2)
with 8 jogging/running intervals of ~30 s interspersed with
Blood pressure and anthropometric measurements ~120 s of low-intensity walking. To promote sufficient workload
Blood pressure measurements were performed one week before for eliciting improvements throughout the follow-up, there was
and after the 16-week follow-up, with an automatic monitor a 7–10 % increase in the high-intensity interval duration and a
(Omron HEM 7114™, Omron Healthcare Inc., Lake Forest, IL, 4 % decrease in the recovery interval duration every 2 weeks.
USA), in triplicate (2 min of interval between measurements), There was also an increase of 2 exercise intervals every 4 weeks
after 15 min of resting, and with the patients in seated position. of follow-up. With the exercise intensity/volume progression,
The blood pressure measurements were repeated in 3 non-con- total working duration ranged from 4 to 13.5 min (week 1–16),
secutive days, at the same time of morning (between 8:00 and total recovery duration ranged from 18 to 24 min (week 1–16)
11:00 a.m.). The mean of the 9 blood pressure measurements, and number of intervals ranged from 8 to 14 (week 1–16). Thus,
performed both before and after the follow-up, were registered the exercise session duration ranged from 22 min to 37.5 min
and used for inter- and intra-group analyses [4]. (week 1–16), totalizing 66 min/wk (week 1) to 112.6 min/wk
Anthropometric measurements were also performed one week (week 16) of exercise. A detailed description of the HIT volume and
before and after the 16-week follow-up in all patients. Body intensity progression during follow-up is showed in ● ▶ Table 1.
mass (kg) was measured (to the nearest of 0.1 kg) by a digital
scale (Omron HBF-INT™, Omron Healthcare Inc., Lake Forest, IL, Statistical analyses
USA), with minimum of clothes and no shoes. Height (m) was Data are reported as mean ± standard error of the mean (SEM) or
measured without shoes, using a standard stadiometer (Health o median and interquartile ranges. Statistical analyses were per-
Meter™ Professional, Sunbeam Products Inc., Chicago, IL, USA), formed using SPSS™ statistical software version 18.0 (SPSS Inc.,
to the nearest of 0.1 m. Body mass index (BMI) was calculated as Chicago, IL, USA). Normality and homoscedasticity of variables
body mass divided by height squared (kg/m2). Waist circumfer- were determined using the Shapiro-Wilk and Levene tests,
ence (cm) was measured to the nearest of 0.1 cm, using a flexible respectively. Two-way ANOVA with repeated measures (group
and inextensible measuring tape (Hoechstmass™, Sulzbach, vs. time) was used to indicate inter- and intra-interventions dif-
Germany). Assessment of skinfolds thickness was performed ferences in the data presenting Gaussian distribution. The Bon-
using a Langue™ skinfold caliper (Beta Technology Inc., Santa ferroni’s post hoc test was performed to identify significant
Cruz, California, USA), according to the International Society for differences indicated by ANOVA.
the Advance of Kinanthropometry [21], in 4 sites (tricipital, sub-
scapular, suprailiac and mid-leg).
Results
Endurance performance assessment ▼
Endurance performance was assessed one week before and after Four patients of CON group were lost to follow-up because of
the 16-week follow-up by the 2 km walking test (2KWT) [19]. In failure to communicate a change in residence address (N = 2) or
brief, the test was performed in an indoor sports court (100 m in health center of treatment (N = 2). One patient of HIT group
track), after a 10 min warm-up (low-intensity walking and slow was excluded from final analysis because she did not have the
movements involving the knee and ankle joints). Patients were minimal exercise training compliance of 70 %. Thus, 23 over-
then instructed to walk as fast as possible with a steady pace. weight or obese T2DM patients completed the 16-week follow-
Heart rate was continuously monitored (ProTrainer 5™, Polar up and were included in the final analysis ( ● ▶ Fig. 1). No
Alvarez C et al. High-Intensity Exercise and Diabetes … Int J Sports Med
Clinical Sciences IJSM/5290/16.5.2016/MPS
Variable Weeks Weeks Weeks Weeks Table 1 Characteristics of low-
volume, high-intensity interval
0–4 5–9 10–13 14–16
training during follow-up.
Exercise intensity (% HRRESERVE) 90–100 90–100 90–100 90–100
Exercise duration (s) 30–34 38–44 46–50 52–58
Number of exercise bouts 8 10 12 14
Exercise time commitment/day (min) 4–4.5 6.3–7.3 9.2–10 12.1–13.5
Exercise time commitment/week (min) 12–13.5 19–21,9 27.6–30 36.4–40.6
Exercise method jogging/running jogging/running jogging/running jogging/running
Recovery intensity (% HRRESERVE) ≤ 70 % ≤ 70 % ≤ 70 % ≤ 70 %
Recovery duration (s) 120 108 100 96
Number of recovery bouts * 9 11 13 15
Recovery method walking walking walking walking
Total time commitment/day (min) 22–22.5 26.1–27.1 30.9–31.7 36.1–37.5
Total time commitment/week (min) 66–67.5 78.3–81.3 92.6–95 108.4–112.6
* All sessions started and ended with a recovery bout
Variable HIT (N = 13) CON (N = 10) Table 2 Subjects’ characteristics
before and after the experimental
Pre Post Pre Post
protocol.
Age (y) 45.6 ± 3.1 43.1 ± 1.5
Downloaded by: Serials Unit - Periodicals. Copyrighted material.
Time elapsed from diagnosis (y) 3.4 ± 1.1 3.6 ± 1.1
Height (cm) 1.56 ± 0.02 1.58 ± 0.02
Body mass (kg) 73.8 ± 2 72.2 ± 1.9 * 75.3 ± 1.6 75.3 ± 1.7
Body mass index (kg/m2) 30.6 ± 1.1 29.9 ± 1.1 * 30.4 ± 0.4 30.4 ± 0.4
Waist circumference (cm) 101.1 ± 2.4 97.0 ± 2.1 ** 98.7 ± 1.5 99.3 ± 1.5 †
∑ 4 Skin-folds (mm) 147 ± 6 119 ± 4 *** 144 ± 5 147 ± 5 †††
Endurance performance (min) • 23.2 ± 0.2 21.0 ± 0.3 *** 22.3 ± 0.3 22.4 ± 0.2 †
Blood pressure
Systolic (mmHg) 132 ± 1 129 ± 1 * 130 ± 1 131 ± 1
Diastolic (mmHg) 77 ± 1 77 ± 1 78 ± 1 79 ± 1
Current medication
Metformin (N) (mg/day) 13 (1 700 ± 0) 13 (1 242 ± 122) 10 (1 700 ± 0) 10 (1 700 ± 0)
Glibenclamide (N) (mg/day) 12 (5 ± 0) 12 (3.7 ± 0.4) 8 (5 ± 0) 8 (5 ± 0)
ACE inhibitor (N) (mg/day) 3 (10 ± 0) 0 3 (10 ± 0) 3 (10 ± 0)
Levothyroxine (N) (mg/day) 1 (100 ± 0) 1 (100 ± 0) 1 (100 ± 0) 1 (100 ± 0)
ACE: angiotensin converting enzyme; HIT: high-intensity interval training group. CON: non-exercise control group. T2DM: type 2
diabetes mellitus. • Endurance performance was measured by the time to complete the 2-km walking test. Asterisks denote significant
difference from pre follow-up in the same group (* = P < 0.05; ** = P < 0.01; *** = P < 0.001). Daggers denotes significant difference from
HIT during the same period († = P < 0.05; ††† = P < 0.001)
The exercise program was well tolerated by all patients, and
Table 3 Lipid profile before and after the experimental protocol.
there were no injuries during the training program. The exercise
Variables HIT (N = 13) CON (N = 10) compliance was 89 ± 5 % during the 16-week follow-up. 7
Pre Post Pre Post patients of HIT group reduced their daily dosage of metformin
Fasting total cholesterol 187 ± 4 183 ± 4 197 ± 6 199 ± 6 and glibenclamide during the follow-up. First, the dosage was
(mg/dL) reduced only in the exercise training days (tri-weekly) due to
Fasting HDL cholesterol 50 ± 2 60 ± 1 * 44 ± 2 43 ± 2 † episodes of post-exercise hypoglycemia that started 1 h after the
(mg/dL) exercise session (from the 1st week of follow-up). Then, the dos-
Fasting LDL cholesterol 128 ± 4 126 ± 5 129 ± 5 132 ± 5 age was reduced in all days of week (from the 11th week of fol-
(mg/dL)
low-up) due to increasing episodes of hypoglycemia in the
Fasting triglycerides 129 ± 6 106 ± 6 * 130 ± 10 139 ± 7 †
non-exercise days. The 3 HIT patients under antihypertensive
(mg/dL)
drug therapy before follow-up stopped taking the medication
HIT: high-intensity interval training group. CON: non-exercise control group.
* denotes significant difference from pre follow-up in the same group (P < 0.05).
after physician recommendation at a routine medical consulta-
†
denotes significant difference from HIT during the same period (P < 0.05) tion (from the 11th week of follow-up). There were no changes in
any medication dosage intake in the CON group during follow-
up ( ●▶ Table 2).
significant baseline differences between HIT and CON patients The 2-way ANOVA indicated significant interactions between
▶ Table 2, 3 and ●
were found in any variable ( ● ▶ Fig. 2). There was inter- and intra-intervention in fasting glucose (F1,9 = 87.78,
also no significant differences in baseline characteristics P < 0.001), HbA1c (F1,9 = 128.29, P < 0.001), HDL cholesterol
between patients who completed the follow-up and those who (F1,9 = 57.81, P < 0.001), triglycerides (F1,9 = 20.27, P = 0.001), sys-
did not (data not shown). tolic (F1,9 = 37.29, P < 0.001) and diastolic blood pressure
Alvarez C et al. High-Intensity Exercise and Diabetes … Int J Sports Med
IJSM/5290/16.5.2016/MPS Clinical Sciences
group during follow-up ( ▶ Table 2). HIT group also showed a
●
a reduced body mass (1.6 ± 0.2 kg, P < 0.05), BMI (2.1 ± 0.3 %,
150
P < 0.05), waist circumference (4.1 ± 0.6 cm, P < 0.01) and skinfold
thickness (18.6 ± 1.4 %, P < 0.001) during follow-up ( ●
▶ Table 2).
Finally, the HIT group improved its endurance performance as
140
shown by a reduced time (9.8 ± 1.0 %, P < 0.001) to complete the
2KWT. The CON group did not change any variable during fol-
Fasting Glucose (mg/dL)
low-up. With these results, the HIT group displayed improved
130 levels of fasting glucose, HbA1c, HDL cholesterol, triglycerides,
endurance performance, waist circumference and skinfold
thickness compared to the CON group after the experimental
120 protocol.
Discussion
110
▼
The present study investigated the effects of a low-volume HIT
program in T2DM women. The primary finding was that the HIT
100 program was effective for reducing fasting glucose and HbA1c
HIT CON levels during 16 weeks of follow-up, which occurred even with a
b
8.5 reduction in the daily dosage of antihyperglycemic medication.
Downloaded by: Serials Unit - Periodicals. Copyrighted material.
In addition, the HIT program was also effective for improving
lipid profile, blood pressure levels, endurance performance and
8.0
body composition of T2DM women. To the best of our knowl-
edge, this is the first randomized controlled study that evaluated
7.5 the effects of a long-term (> 12 weeks) low-volume HIT program
in T2DM women.
7.0 Aerobic and resistance exercise training have shown improve-
HbA1c (%)
ments over the glycemic control in T2DM patients [3, 29, 35, 36].
Although a pioneer meta-analysis showed that exercise inten-
6.5 sity was a stronger predictor for HbA1c improvements than exer-
cise volume [3], recent meta-analyses did not confirm this
6.0 association [35, 36]. For example, an absolute 0.89 % (95 %
CI, − 1.26 % to − 0.51 %) reduction in HbA1c levels has been found
after exercise programs with volume > 150 min/wk, which were
5.5
greater than the absolute 0.36 % (95 % CI, − 0.50 % to − 0.23 %)
reduction observed after exercise programs with vol-
5.0 ume < 150 min/wk [35]. Accordingly, a minimum of 150 min/wk
HIT CON (30 min, 5 d/wk) of moderate to vigorous aerobic exercise, in
Pre Post association with 2–3 sessions per week of resistance training,
has been recommended in the current American Diabetes Asso-
Fig. 2 Fasting glucose a and HbA1c b before and after the experimental ciation and American College of Sports Medicine guidelines [9].
protocol. HIT: high-intensity interval training group. CON: non-exercise
However, recent studies with HIT programs have suggested that
control group. *** denotes significant difference from pre follow-up in the
exercise intensity may have a key role in T2DM management.
same group (P < 0.001). †denotes significant difference from HIT during
the same period (P < 0.05).
When compared to energy expenditure-matched continuous
moderate exercise, HIT programs have shown greater improve-
ments in HbA1c [23], fasting insulin [17, 23], glucose control
(F1,9 = 18.25, P = 0.002), body mass (F1,9 = 31.98, P < 0.001), waist assessed by continuous glucose monitoring [17] and others car-
circumference (F1,9 = 38.88, P < 0.001), BMI (F1,9 = 35.05, P < 0.001), diovascular risk factors [17, 23] in T2DM patients. In the present
skinfold thickness (F1,9 = 64.81, P < 0.001) and endurance perfor- study, it was shown for the first time that a 16-week progressive
mance (F1,9 = 104.5, P < 0.001). low-volume HIT program, with a weekly time commitment
Post hoc analysis showed that there were significant improve- 56–25 % (66–112.6 min/wk divided in 3 exercise sessions) lower
ments in biochemical, hemodynamic, anthropometric and than the minimum recommended by current guidelines [9],
endurance performance variables of HIT group during follow- resulted in improvements of glycemic control (HbA1c and fasting
up. Fasting glucose and HbA1c were reduced (P < 0.001) glucose levels), lipid profile, blood pressure, endurance perfor-
19.8 ± 1.9 mg/dL and 0.9 ± 0.1 % (9.9 ± 1.0 mmol/mol) after the HIT mance and body composition (BMI, waist circumference and sub-
program, respectively ( ● ▶ Fig. 2). Although total and LDL choles- cutaneous fat) in T2DM women. It is noteworthy that the mean
terol did not change significantly, the HIT group showed an absolute reduction of 0.9 % on HbA1c levels was similar to the
increase in HDL cholesterol (10.1 ±
1.1
mg/dL, P < 0.05) and reductions found in exercise programs with volume > 150 min/wk
decrease in triglycerides (22.9 ± 3.4 mg/dL, P < 0.05) during fol- [35], and occurred even with a reduction in daily dosage of dia-
low-up ( ▶ Table 3). Systolic blood pressure, but not diastolic
● betes medication. These results confirm the time-efficiency of
blood pressure, was reduced 3.7 ± 0.5 mmHg (P < 0.05) in HIT low-volume HIT to T2DM management, which has been sug-
Alvarez C et al. High-Intensity Exercise and Diabetes … Int J Sports Med
Clinical Sciences IJSM/5290/16.5.2016/MPS
gested by uncontrolled studies with short-duration (only 2 Clinical implications
weeks) and small sample size [20, 27]. It is well known that T2DM is becoming increasingly prevalent
The mechanism involved in the superior effects of HIT on glyce- worldwide; it is also known that not only an improvement in
mic control of T2DM patients is not completely understood. One glycemic control but a reduction in cardiovascular risk factors
might speculate that the ~1.6 kg reduction on body mass, which can positively affect disease morbidity, mortality and health
was probably due to the reductions on visceral (~4.1 cm reduc- care expenditures [22, 28, 34, 39]. For example, decreases of
tion on waist circumference) and subcutaneous fat (~28.0 mm 2.1/0.9 mmHg on systolic/diastolic blood pressure reduced
reduction on sum of 4 skinfold thickness), may be involved in major cardiovascular events by 10 % in T2DM patients [34].
the glycemic control improvements found after the low-volume Decreases of 2–3 % in the risk for developing coronary artery dis-
HIT program. However, a previous study showed that a greater ease has been suggested for each 1 mg/dL increase in HDL cho-
HIT-induced reduction on body mass (~4.2 kg), which was due to lesterol [22]. In this context, the HIT-induced improvements in
reduction on fat mass (no changes on fat free mass was found), systolic blood pressure ( − 3.7 mmHg) and HDL cholesterol
accounted for maximally 25 % of the glycemic control improve- ( + 10.1 mg/dL) may have important clinical implications. More
ments found after a HIT program [16]. Therefore, improvements over, the low-volume HIT program resulted in low daily dosage
on skeletal muscle insulin sensitivity, explained by increased of diabetes medication in 54 % (7 patients) of the trained popula-
peripheral glucose disposal probably due to increased GLUT4 tion, and the 3 HIT patients taking anti-hypertensive medication
protein content and mitochondrial capacity [16, 20], appears to before training stopped taking it during follow-up. Thus, the
be involved in the low-volume HIT-induced improvements on present low-volume HIT program also has important implica-
glycemic control found in the present study. In addition, the tions for reducing health care expenditures for medication.
~14.3 mg/dL reduction on plasma fasting glucose observed after Finally, the current low-volume HIT program resulted in glyce-
low-volume HIT, but not after CON intervention, does not allow mic control improvements similar to those observed with
Downloaded by: Serials Unit - Periodicals. Copyrighted material.
to rule out a training-induced improvement on hepatic glucose greater volumes of exercise ( > 150 min/wk) [35]. Given that
output. most T2DM patients are sedentary or insufficiently active [24],
The present low-volume HIT program also resulted in significant and lack of time is the most frequently cited barrier to regular
reduction of systolic (but not diastolic) blood pressure exercise participation [33], these findings may have important
(~3.7 mmHg), which occurred even after the 3 patients who implications for a public health perspective.
were under antihypertensive drug therapy prior to the interven- In summary, the low-volume HIT program was effective to
tion stopped taking the medication during the follow-up. improve glycemic control, lipid and blood pressure levels, endur-
Although there is a study showing a greater HIT-induced systolic ance performance, medication dosage used and anthropometry
blood pressure reduction (~13 mmHg) compared to the one in T2DM women with a weekly time commitment 56–25 %
found in the present study [23], others HIT intervention studies lower than the minimal recommended in current guidelines [9].
in T2DM patients have shown no training-induced improve- These findings suggest that low-volume HIT may be a time-effi-
ments on blood pressure [15, 17]. HIT-induced improvements on cient intervention to treat T2DM women.
lipid profile in T2DM patients has also been inconsistent in the
literature. There are studies showing improvements only in LDL
cholesterol [17], in both LDL and HDL cholesterol [23], or no Acknowledgements
improvements [30]. The same studies also showed no HIT- ▼
induced improvements on triglycerides in T2DM patients The present research project was funded primarily by the Family
[17, 23, 30]. In the present study, we showed improvements on Healthcare Center Tomas Rojas (2014 Annual Grant), and by the
HDL cholesterol and triglycerides levels, but not in LDL cholesterol 2014 Health Promotion Program of Los Ríos Health Service.
levels, after the 16-week low-volume HIT. Differences in exercise
intensity and volume of HIT protocol, as well as in intervention Conflict of interest: There are no conflicts of interest to declare.
duration may explain discrepancies between studies on training-
induced improvements in blood pressure and lipid profile. Affiliations
The training-induced improvements observed in the present 1
Cardiovascular Health Program, Centro de Salud Familiar, Los Lagos, Chile
2
study occurred after a HIT protocol of jogging/running and walk- Department of Physical Activity Sciences, Universidad de Los Lagos, Osorno,
Chile
ing over ground that was prescribed using an easy and inexpen- 3
Department of Physical Education and Recreation, Faculty of Education,
sive method [18]. This is an unique strength of the present study, Social Sciences and Humanities, Universidad de la Frontera, Temuco, Chile
4
because most of intervention studies in T2DM patients have Department of Human Movement Science, Faculty of Health, Medicine and
Life Sciences, Maastricht University, Maastricht, Netherlands
based HIT prescription on cardiopulmonary exercise testing 5
Department of Physiology, Faculty of Medicine, Dentistry and Health
[17, 20, 23, 27] and using ergometers for training [20, 23, 27], Sciences, University of Melbourne, Victoria, Australia
6
which are expensive and may reduce HIT access to general pop- Rehabilitation, Public Hospital of Los Lagos, Los Lagos, Chile
7
Exercise and Chronic Disease Research Laboratory, Physical Education
ulation [8]. However, the present study investigated only over- Department, School of Sciences, São Paulo State Univiersity - UNESP,
weight or obese women with less than 5 years of diagnosis and
with no disease-related complications. This limitation makes it
References
difficult to extrapolate present findings for other populations, 1 Albright A, Franz M, Hornsby G, Kriska A, Marrero D, Ullrich I, Verity
mainly long-standing T2DM patients with complications. We LS. American College of Sports Medicine position stand. Exercise and
did not provide any control for dietary changes during the study type 2 diabetes. Med Sci Sports Exerc 2000; 32: 1345–1360
and for physical activity during daily life after the intervention. 2 Borg GAV. Psychophysical bases of perceived exertion. Med Sci Sports
Exerc 1982; 14: 377–381
However, both HIT and CON groups were instructed to maintain 3 Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on
their dietary and daily physical activity patterns throughout the glycemic control and body mass in type 2 diabetes mellitus: a meta-
16-week study period. analysis of controlled clinical trials. JAMA 2001; 286: 1218–1227
Alvarez C et al. High-Intensity Exercise and Diabetes … Int J Sports Med
IJSM/5290/16.5.2016/MPS Clinical Sciences
4 Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones 22 Maron DJ. The epidemiology of low levels of high-density lipoproteins
DW, Materson BJ, Oparil S, Wright JT, Roccella EJ, Committee tNHBPEPC. cholesterol in patients with and without coronary artery disease. Am
Seventh report of the joint national committee on prevention, detec- J Cardiol 2000; 86: 11l–14l
tion, evaluation, and treatment of high blood pressure. Hypertension 23 Mitranun W, Deerochanawong C, Tanaka H, Suksom D. Continuous vs
2003; 42: 1206–1252 interval training on glycemic control and macro and microvascular
5 Ciolac EG. High-intensity interval training and hypertension: maxi- reactivity in type 2 diabetic patients. Scand J Med Sci Sports 2014;
mizing the benefits of exercise? Am J Cardiovasc Dis 2012; 2: 102–110 24: E69–E76
6 Ciolac EG, Bocchi EA, Bortolotto LA, Carvalho VO, Greve JMD, Guimaraes 24 Morrato EH, Hill JO, Wyatt HR, Ghushchyan V, Sullivan PW. Physical
GV. Effects of high-intensity aerobic interval training vs. moderate activity in U.S. adults with diabetes and at risk for developing diabetes,
exercise on hemodynamic, metabolic and neuro-humoral abnormali- 2003. Diabetes Care 2007; 30: 203–209
ties of young normotensive women at high familial risk for hyperten- 25 Rognmo O, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity
sion. Hypertens Res 2010; 33: 836–843 aerobic interval exercise is superior to moderate intensity exercise for
7 Ciolac EG, Bocchi EA, Greve JM, Guimaraes GV. Heart rate response to increasing aerobic capacity in patients with coronary artery disease.
exercise and cardiorespiratory fitness of young women at high familial Eur J Cardiovasc Prev Rehabil 2004; 11: 216–222
risk for hypertension: effects of interval vs continuous training. Eur J 26 Seron P, Munoz S, Lanas F. Levels of physical activity in an urban
Cardiovasc Prev Rehabil 2011; 18: 824–830 population from Temuco, Chile. Rev Med Chile 2010; 138: 1232–1239
8 Ciolac EG, Mantuani SS, Neiva CM, Verardi C, Pessoa-Filho DM, Pimenta 27 Shaban N, Kenno KA, Milne KJ. The effects of a 2-week modified high
L. Rating of perceived exertion as a tool for prescribing and self regu- intensity interval training program on the homeostatic model of insu-
lating interval training: a pilot study. Biol Sport 2015; 32: 103–108 lin resistance (HOMA-IR) in adults with type 2 diabetes. J Sports Med
9 Colberg SR, Albright AL, Blissmer BJ, Braun B, Chasan-Taber L, Fernhall Phys Fitness 2014; 54: 203–209
B, Regensteiner JG, Rubin RR, Sigal RJ. Exercise and type 2 diabetes: 28 Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of
American College of Sports Medicine and the American Diabetes Asso- diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010; 87: 4–14
ciation: joint position statement. Exercise and type 2 diabetes. Med 29 Snowling NJ, Hopkins WG. Effects of different modes of exercise train-
Sci Sports Exerc 2010; 42: 2282–2303 ing on glucose control and risk factors for complications in type 2 dia-
10 Francois ME, Little JP. Effectiveness and safety of high-intensity inter- betic patients: a meta-analysis. Diabetes Care 2006; 29: 2518–2527
val training in patients with type 2 diabetes. Diabetes Spectr 2015; 30 Terada T, Friesen A, Chahal BS, Bell GJ, McCargar LJ, Boule NG. Feasibility
28: 39–44 and preliminary efficacy of high intensity interval training in type 2
Downloaded by: Serials Unit - Periodicals. Copyrighted material.
11 Friedewald WT, Levy RI, Fredrickson DS. Estimation of the Concentra- diabetes. Diabetes Res Clin Pract 2013; 99: 120–129
tion of Low-Density Lipoprotein Cholesterol in Plasma, Without Use of 31 Tjonna AE, Lee SJ, Rognmo O, Stolen TO, Bye A, Haram PM, Loennechen
the Preparative Ultracentrifuge. Clin Chem 1972; 18: 499–502 JP, Al-Share QY, Skogvoll E, Slordahl SA, Kemi OJ, Najjar SM, Wisloff U.
12 Gibala MJ, Little JP, Macdonald MJ, Hawley JA. Physiological adaptations Aerobic interval training versus continuous moderate exercise as a
to low-volume, high-intensity interval training in health and disease. treatment for the metabolic syndrome – A pilot study. Circulation
J Physiol 2012; 590: 1077–1084 2008; 118: 346–354
13 Guimaraes GV, Ciolac EG, Carvalho VO, D’Avila VM, Bortolotto LA, Boc- 32 Trapp EG, Chisholm DJ, Freund J, Boutcher SH. The effects of high-inten-
chi EA. Effects of continuous vs. interval exercise training on blood sity intermittent exercise training on fat loss and fasting insulin levels
pressure and arterial stiffness in treated hypertension. Hypertens Res of young women. Int J Obes (Lond) 2008; 32: 684–691
2010; 33: 627–632 33 Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’
14 Harriss DJ, Atkinson G. Ethical Standards in Sport and Exercise Science participation in physical activity: review and update. Med Sci Sports
Research: 2016 Update. Int J Sports Med 2015; 36: 1121–1124 Exerc 2002; 34: 1996–2001
15 Hollekim-Strand SM, Bjorgaas MR, Albrektsen G, Tjonna AE, Wisloff U, 34 Turnbull F, Neal B, Algert C, Chalmers J, Chapman N, Cutler J, Woodward
Ingul CB. High-intensity interval exercise effectively improves cardiac M, MacMahon S. Effects of different blood pressure-lowering regimens
function in patients with type 2 diabetes mellitus and diastolic dys- on major cardiovascular events in individuals with and without dia-
function: a randomized controlled trial. J Am Coll Cardiol 2014; 64: betes mellitus: results of prospectively designed overviews of rand-
1758–1760 omized trials. Arch Intern Med 2005; 165: 1410–1419
16 Karstoft K, Winding K, Knudsen SH, James NG, Scheel MM, Olesen J, Holst 35 Umpierre D, Ribeiro PA, Kramer CK, Leitao CB, Zucatti AT, Azevedo MJ,
JJ, Pedersen BK, Solomon TPJ. Mechanisms behind the superior effects Gross JL, Ribeiro JP, Schaan BD. Physical activity advice only or struc-
of interval vs continuous training on glycemic control in individu- tured exercise training and association with HbA1c levels in type 2
als with type 2 diabetes: a randomized controlled trial. Diabetologia diabetes: a systematic review and meta-analysis. JAMA 2011; 305:
2014; 57: 2081–2093 1790–1799
17 Karstoft K, Winding K, Knudsen SH, Nielsen JS, Thomsen C, Pedersen BK, 36 Umpierre D, Ribeiro PAB, Schaan BD, Ribeiro JP. Volume of supervised
TPJ Solomon. The Effects of Free-Living Interval Walking Training on exercise training impacts glycemic control in patients with type 2
Glycemic Control, Body Composition, and Physical Fitness in Type 2 diabetes: a systematic review with meta-regression analysis. Diabe-
Diabetic Patients A randomized, controlled trial. Diabetes Care 2013; tologia 2013; 56: 242–251
36: 228–236 37 Weston KS, Wisloff U, Coombes JS. High-intensity interval training in
18 Karvonen J, Vuorimaa T. Heart rate and exercise intensity during patients with lifestyle-induced cardiometabolic disease: a systematic
sports activities. Practical application. Sports Med 1988; 5: 303–311 review and meta-analysis. Br J Sports Med 2014; 48: 1227–1234
19 Laukkanen RM, Kukkonen-Harjula TK, Oja P, Pasanen ME, Vuori IM. 38 Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM,
Prediction of change in maximal aerobic power by the 2-km walk Tjonna AE, Helgerud J, Slordahl SA, Lee SJ, Videm V, Bye A, Smith GL, Naj-
test after walking training in middle-aged adults. Int J Sports Med jar SM, Ellingsen O, Skjaerpe T. Superior cardiovascular effect of aerobic
2000; 21: 113–116 interval training versus moderate continuous training in heart failure
20 Little JP, Gillen JB, Percival ME, Safdar A, Tarnopolsky MA, Punthakee patients – A randomized study. Circulation 2007; 115: 3086–3094
Z, Jung ME, Gibala MJ. Low-volume high-intensity interval training 39 Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J, Nichols G. Global
reduces hyperglycemia and increases muscle mitochondrial capac- healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res
ity in patients with type 2 diabetes. J Appl Physiol 1985 2011; 111: Clin Pract 2010; 87: 293–301
1554–1560
21 Marfell-Jones M, Olds T, Stewart A, Carter L. International standards for
anthropometric assessment: ISAK. 1st ed. Potchefstroom, South Africa:
The International Society for the Advancement of Kinanthropometry
(ISAK); 2006
Alvarez C et al. High-Intensity Exercise and Diabetes … Int J Sports Med
You might also like
- Compiled UPCAT Questions 2Document18 pagesCompiled UPCAT Questions 2Anna Bartolome100% (12)
- Efficacy of Lifestyle Interventions in Patients With Type 2 Diabetes - A Systematic Review and Meta-AnalysisDocument11 pagesEfficacy of Lifestyle Interventions in Patients With Type 2 Diabetes - A Systematic Review and Meta-AnalysisDara Agusti MaulidyaNo ratings yet
- List of All ProjectsDocument152 pagesList of All ProjectsMhm ReddyNo ratings yet
- B2 Unit 4 Reading Plus LessonDocument2 pagesB2 Unit 4 Reading Plus LessonIruneNo ratings yet
- Types of Plant MaintenanceDocument7 pagesTypes of Plant MaintenanceTHEOPHILUS ATO FLETCHERNo ratings yet
- Ix-karmapa-The Chariot For Traveling The Supreme PathDocument54 pagesIx-karmapa-The Chariot For Traveling The Supreme Pathssm100% (1)
- High Intensity Interval Training Is Safe, Feasible and Efficacious in Nonalcoholic Steatohepatitis: A Randomized Controlled TrialDocument17 pagesHigh Intensity Interval Training Is Safe, Feasible and Efficacious in Nonalcoholic Steatohepatitis: A Randomized Controlled TrialFabricio BoscoloNo ratings yet
- Effectiveness and Safety of High-Intensity Interval Training in Patients With Type 2 DiabetesDocument6 pagesEffectiveness and Safety of High-Intensity Interval Training in Patients With Type 2 DiabetesMumtaz Maulana HidayatNo ratings yet
- Exercise in ObesityDocument8 pagesExercise in ObesitywidyaNo ratings yet
- HolidaysDocument12 pagesHolidaysGabriela PopescuNo ratings yet
- Metabolic Risk Management, Physical Exercise and Lifestyle Counselling in Low-Active Adults: Controlled Randomized Trial (BELLUGAT)Document15 pagesMetabolic Risk Management, Physical Exercise and Lifestyle Counselling in Low-Active Adults: Controlled Randomized Trial (BELLUGAT)adrianNo ratings yet
- BMC Endocrine DisordersDocument8 pagesBMC Endocrine DisordersJose Luis JaimeNo ratings yet
- HIIT - Different Methods ComparisonDocument7 pagesHIIT - Different Methods Comparisonbonifax1No ratings yet
- Row 7Document3 pagesRow 7Anna BartolomeNo ratings yet
- Colberg 2009 2511457365Document8 pagesColberg 2009 2511457365fedelarru9No ratings yet
- Sam-Kit Tin T. Et Al. (2019)Document7 pagesSam-Kit Tin T. Et Al. (2019)Andrés MenesesNo ratings yet
- Jurnal 444Document7 pagesJurnal 444rizalmantaNo ratings yet
- Apnm 2014 0357Document8 pagesApnm 2014 0357adri20121989No ratings yet
- JFMK 05 00070 v2Document11 pagesJFMK 05 00070 v2Santy OktavianiNo ratings yet
- Resistance Training For Glycemic Control, Muscular Strength, and Lean Body Mass in Old Type 2 Diabetic Patients - A Meta-Analysis (Lee & Kim, 2017)Document15 pagesResistance Training For Glycemic Control, Muscular Strength, and Lean Body Mass in Old Type 2 Diabetic Patients - A Meta-Analysis (Lee & Kim, 2017)Gonzalo GonzalesNo ratings yet
- Research Article: Acute Whole Body Vibration Decreases The Glucose Levels in Elderly Diabetic WomenDocument8 pagesResearch Article: Acute Whole Body Vibration Decreases The Glucose Levels in Elderly Diabetic WomenStefanny AmahorsejaNo ratings yet
- Effects of Exercising Before Breakfast On The Health of T2DM Patients-A Randomized Controlled TrialDocument7 pagesEffects of Exercising Before Breakfast On The Health of T2DM Patients-A Randomized Controlled TrialAna Carolina Chacon GonzalezNo ratings yet
- Hansen 2016 Impact of Endurance Exercise Training in The Fasted StateDocument14 pagesHansen 2016 Impact of Endurance Exercise Training in The Fasted StateYo Vivo Fit Pablo y KarlaNo ratings yet
- Reljic Et Al., 2021Document14 pagesReljic Et Al., 2021AILEENNo ratings yet
- Wewege2017 PDFDocument12 pagesWewege2017 PDFHelton PereiraNo ratings yet
- Milanović2015 Article EffectivenessOfHigh-IntensityIDocument13 pagesMilanović2015 Article EffectivenessOfHigh-IntensityICamilo RinconNo ratings yet
- 2006 20 1 Two Short Daily Activity Bouts VS One LongDocument6 pages2006 20 1 Two Short Daily Activity Bouts VS One LongVictor Hugo VeraNo ratings yet
- Fatone 2010Document7 pagesFatone 2010Blake d souzaNo ratings yet
- Effects of Low Versus High Volume High Intensity Interval - 2023 - Journal of EDocument10 pagesEffects of Low Versus High Volume High Intensity Interval - 2023 - Journal of ESherriNo ratings yet
- HIIT Andando Melhora Glicemia e LDLDocument9 pagesHIIT Andando Melhora Glicemia e LDLbonifax1No ratings yet
- 2019 Article 7554Document9 pages2019 Article 7554LeoSilvaRctNo ratings yet
- Ishiguro 2015Document11 pagesIshiguro 2015Andrés Araneda VásquezNo ratings yet
- Low-Volume High-Intensity Interval Training Reduces Hyperglycemia and Increases Muscle Mitochondrial Capacity in Patients With Type 2 DiabetesDocument7 pagesLow-Volume High-Intensity Interval Training Reduces Hyperglycemia and Increases Muscle Mitochondrial Capacity in Patients With Type 2 DiabetesSafira Ridha UlyaNo ratings yet
- 19417381221139343Document8 pages19417381221139343Thiago SartiNo ratings yet
- Interval Endurance and Resistance Training As Part of A Community-Based Secondary Prevention Program For Patients With Diabetes Mellitus and Coronary Artery DiseaseDocument7 pagesInterval Endurance and Resistance Training As Part of A Community-Based Secondary Prevention Program For Patients With Diabetes Mellitus and Coronary Artery DiseaseMarcos Túlio de SáNo ratings yet
- Prediabetes ExcsDocument8 pagesPrediabetes ExcsKamal JindalNo ratings yet
- Clinical Study: Obesity, Physical Function, and Training Success in Community-Dwelling Nonsarcopenic Old AdultsDocument11 pagesClinical Study: Obesity, Physical Function, and Training Success in Community-Dwelling Nonsarcopenic Old AdultsPeriyasami GovindasamyNo ratings yet
- Journal of Clinical TrialsDocument10 pagesJournal of Clinical TrialsRodrigo DelgadoNo ratings yet
- Exercise TherapyDocument16 pagesExercise Therapylailatul azizahNo ratings yet
- Exercise and Fitness in The Prevention of Atherosclerotic Cardiovascular DiseaseDocument23 pagesExercise and Fitness in The Prevention of Atherosclerotic Cardiovascular DiseaseJessica BarcelonaNo ratings yet
- Lakka 2007Document13 pagesLakka 2007Neha RauhilaNo ratings yet
- Walking and T2DDocument9 pagesWalking and T2DstarmittNo ratings yet
- Slide Rehab MedikDocument18 pagesSlide Rehab MedikElfan Mahfuzh SmavenNo ratings yet
- Manage HypertensionDocument15 pagesManage HypertensionjaqueberenyiNo ratings yet
- Aerobic WalkingDocument17 pagesAerobic WalkingKedokteran Komunitas21No ratings yet
- Munan, 2020 - CGM T2DDocument17 pagesMunan, 2020 - CGM T2DPedroNo ratings yet
- Jurnal DiabetesDocument15 pagesJurnal DiabetesJupriadiVillaNo ratings yet
- The Importance of Exercise For Glycemic Control in Type 2 DiabetesDocument10 pagesThe Importance of Exercise For Glycemic Control in Type 2 DiabetesAhmed AmerNo ratings yet
- Efectos Del Ejercicio en Pacientes Mayores Con Diabetes ECADocument13 pagesEfectos Del Ejercicio en Pacientes Mayores Con Diabetes ECAAndrés Araneda VásquezNo ratings yet
- Impact of High-Intensity Interval Training On Hba1C in Patients With Type 2 Diabetes MellitusDocument8 pagesImpact of High-Intensity Interval Training On Hba1C in Patients With Type 2 Diabetes MellitusKostas LiougkosNo ratings yet
- Jurnal NataDocument9 pagesJurnal Natadr. siti alfiana RS PELNINo ratings yet
- Inter HugoDocument10 pagesInter HugorizkaNo ratings yet
- The Effect of Exercise On Visceral Adipose Tissue in Overweight Adults: A Systematic Review and Meta-AnalysisDocument10 pagesThe Effect of Exercise On Visceral Adipose Tissue in Overweight Adults: A Systematic Review and Meta-AnalysisEdd ContrerasNo ratings yet
- 673 FullDocument4 pages673 FullIba SuprasabaNo ratings yet
- JurnalDocument30 pagesJurnalnurul sya'binNo ratings yet
- Villelabeitia Jaureguizar 2016 Journal of Cardiopulmonary Rehabilitation and PreventionDocument10 pagesVillelabeitia Jaureguizar 2016 Journal of Cardiopulmonary Rehabilitation and PreventionPablo Damian LeivaNo ratings yet
- Physiology & Behavior: SciencedirectDocument8 pagesPhysiology & Behavior: SciencedirectScottNo ratings yet
- Van Dijk, 2013Document6 pagesVan Dijk, 2013Gebyar CaturNo ratings yet
- Reversal of Early Atherosclerosis in Metabolic Syndrome by Yoga A Randomized Controlled Trial 2157 7595.1000132Document3 pagesReversal of Early Atherosclerosis in Metabolic Syndrome by Yoga A Randomized Controlled Trial 2157 7595.1000132Roja VaranasiNo ratings yet
- Diabetes and Multimorbidity Case StudyDocument4 pagesDiabetes and Multimorbidity Case StudyLouiseNo ratings yet
- Jurnal Ebcr DMDocument15 pagesJurnal Ebcr DMNabella PutriNo ratings yet
- Intermittent High-Intensity Exercise For Pre - To eDocument18 pagesIntermittent High-Intensity Exercise For Pre - To eThiago SartiNo ratings yet
- Progressive Muscle Relaxation (PMR) Is Effective To Lower Blood Glucose Levels of Patients With Type 2 Diabetes MellitusDocument7 pagesProgressive Muscle Relaxation (PMR) Is Effective To Lower Blood Glucose Levels of Patients With Type 2 Diabetes Mellituseno wijayaNo ratings yet
- Progressive Muscle Relaxation (PMR) Is Effective To Lower Blood Glucose Levels of Patients With Type 2 Diabetes MellitusDocument7 pagesProgressive Muscle Relaxation (PMR) Is Effective To Lower Blood Glucose Levels of Patients With Type 2 Diabetes Mellituseno wijayaNo ratings yet
- Ephilid Appointment SlipDocument1 pageEphilid Appointment SlipAnna BartolomeNo ratings yet
- Protein Metabolism Part 1Document7 pagesProtein Metabolism Part 1Anna BartolomeNo ratings yet
- Protein Metabolism Part 2Document11 pagesProtein Metabolism Part 2Anna BartolomeNo ratings yet
- Row 7Document3 pagesRow 7Anna BartolomeNo ratings yet
- Review Evaluation of Glycosylated Hemoglobin in Diabetic PatientsDocument5 pagesReview Evaluation of Glycosylated Hemoglobin in Diabetic PatientsAnna BartolomeNo ratings yet
- High-Intensity Aerobic Interval Training Improves Aerobic Fitness and Hba1C Among Persons Diagnosed With Type 2 DiabetesDocument13 pagesHigh-Intensity Aerobic Interval Training Improves Aerobic Fitness and Hba1C Among Persons Diagnosed With Type 2 DiabetesAnna BartolomeNo ratings yet
- The Concept of Monetary PolicyDocument60 pagesThe Concept of Monetary PolicyAnna BartolomeNo ratings yet
- Parameter 0 1 2 Activity Pulse GrimaceDocument2 pagesParameter 0 1 2 Activity Pulse GrimaceAnna BartolomeNo ratings yet
- Money AND Monetary PolicyDocument17 pagesMoney AND Monetary PolicyAnna BartolomeNo ratings yet
- January 25, 2012: Click To Edit Master Subtitle StyleDocument31 pagesJanuary 25, 2012: Click To Edit Master Subtitle StyleAnna BartolomeNo ratings yet
- A Study On Supply Chain and Logistics Managemernt For K.M.B GraniteDocument50 pagesA Study On Supply Chain and Logistics Managemernt For K.M.B GraniteRaja Thrisangu100% (1)
- Dead Poets SocietyDocument1 pageDead Poets SocietyNagy ZenteNo ratings yet
- Lindsey Position PaperDocument14 pagesLindsey Position PaperRamil DumasNo ratings yet
- Print Book FinalDocument25 pagesPrint Book FinalKhurram AliNo ratings yet
- Surfactants and Emulsifying Agents: January 2009Document7 pagesSurfactants and Emulsifying Agents: January 2009Jocc Dee LightNo ratings yet
- 6to Present Continuous AllDocument1 page6to Present Continuous AllEliana VogtNo ratings yet
- The Three Dimensions of Belief Differentiating Religions: Jungguk Cho, Yang LeeDocument5 pagesThe Three Dimensions of Belief Differentiating Religions: Jungguk Cho, Yang LeeMauren NaronaNo ratings yet
- The Role of Customer Knowledge Management (CKM) in Improving Organization-Customer RelationshipDocument7 pagesThe Role of Customer Knowledge Management (CKM) in Improving Organization-Customer RelationshipAbdul LathifNo ratings yet
- GST Compensation CessDocument2 pagesGST Compensation CessPalak JioNo ratings yet
- Bank of South Sudan Act, 2011 - Bank of South SudanDocument59 pagesBank of South Sudan Act, 2011 - Bank of South SudanAnnadevaraNageswararaoNo ratings yet
- WWDC 2020 Viewing GuideDocument13 pagesWWDC 2020 Viewing GuidejuniorNo ratings yet
- Business Communication - IIDocument3 pagesBusiness Communication - IIprachi100% (1)
- FRC Team 2637, Phatnom Catz, Techbinder 2023 - 2024 CrescendoDocument17 pagesFRC Team 2637, Phatnom Catz, Techbinder 2023 - 2024 CrescendoShrey Agarwal (Drago Gaming)No ratings yet
- A Brief History of DerivativesDocument12 pagesA Brief History of DerivativesPranab SahooNo ratings yet
- Bacc Form 02Document2 pagesBacc Form 02Jeanpaul PorrasNo ratings yet
- Laws Releated To Honour KillingDocument2 pagesLaws Releated To Honour KillingMukul Singh RathoreNo ratings yet
- Pre-Intermediate Tests Audio Script: Track 1Document25 pagesPre-Intermediate Tests Audio Script: Track 1arifsahidNo ratings yet
- E Id - Like - To - BeDocument9 pagesE Id - Like - To - BeNatalia IlhanNo ratings yet
- HS-193070003 Exxon Oil Mobilgrease 28 CertificatesDocument3 pagesHS-193070003 Exxon Oil Mobilgrease 28 Certificatesflacuchento2013No ratings yet
- Quantitative Reasearch KINDS OF RESEARCHDocument1 pageQuantitative Reasearch KINDS OF RESEARCHEivie SonioNo ratings yet
- CW-80 ManualDocument12 pagesCW-80 ManualBrian YostNo ratings yet
- Syllabus (Economic Analysis For Business)Document5 pagesSyllabus (Economic Analysis For Business)S TMNo ratings yet
- Grade 11 Reco ScriptDocument2 pagesGrade 11 Reco ScriptCecill Nicanor LabininayNo ratings yet
- PD2017 013 PDFDocument36 pagesPD2017 013 PDFChico Hermanu BrillianNo ratings yet
- LY Adverbs Combined ListDocument1 pageLY Adverbs Combined ListcarmencrisanNo ratings yet
- Islam in The Middle Ages - WORKSHEETDocument4 pagesIslam in The Middle Ages - WORKSHEETcrabbydreamerNo ratings yet