Professional Documents
Culture Documents
Osteoporosis in Men Suspect Secondary Disease First
Uploaded by
megatOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Osteoporosis in Men Suspect Secondary Disease First
Uploaded by
megatCopyright:
Available Formats
REVIEW
ANGELO LICATA, MD, PhD*
CME
CREDIT
Department of Endocrinology, Diabetes,
and Metabolism, The Cleveland Clinic
Osteoporosis in men:
Suspect secondary disease first
■ A B S T R AC T ONTRARY TO POPULAR NOTIONS, osteo-
C porosis is a disease not only of women. In
Since osteoporosis in men is more often secondary rather fact, men account for about 20% of cases of
than primary (idiopathic), we need to seek the underlying osteoporosis and 25% of hip fractures.
cause through the history and laboratory testing. Treatment But there are differences. The conse-
options are similar to those for women, although data are quences are worse for men than for women.
limited about their efficacy in men. Compared with women, men with hip frac-
tures have higher rates of mortality and mor-
■ KEY POINTS bidity.1,2 More are institutionalized, and 30%
to 50% die within a year of fracture vs about
Prevention is the best approach to treatment of osteoporosis 20% of women.
in men, given the limited options at the moment. Another difference of note: from 50% to
70% of cases of osteoporosis in men are sec-
Glucocorticoids top the list of drugs that can cause ondary to another condition, whereas osteo-
osteoporosis. Prescribe a bisphosphonate prophylactically porosis in women is usually primary (idiopath-
when starting long-term glucocorticoid therapy. ic). Hence, in assessing a man, we should
think of secondary osteoporosis first and pri-
mary second.
Bone densitometry can be problematic in men, as the T Many advances have occurred in the past
score is often indexed to a reference database in young decade, including increased awareness of
women. Men are currently not covered for reimbursement osteoporosis, the technology to diagnose it in
under the Bone Mass Measurement Act, but they should its early, asymptomatic stage, and many new
undergo densitometry as women do. treatments. Osteoporosis is now viewed as a
treatable disease, rather than as an inevitable
The biochemical evaluation tends to be more extensive in consequence of aging. Unfortunately, aware-
men with osteoporosis because the bone loss is usually ness of osteoporosis in men lags behind that in
secondary to another condition. The younger the male women, as do research and rates of detection
patient, the more important the laboratory evaluation. and treatment.
This article outlines the unique features
of osteoporosis in men, including its patho-
Alendronate has been shown to increase skeletal density in physiology, causes, diagnosis, and treat-
men comparably to levels seen in women. It is now ment.
approved for use in men. Teriparatide, a parathyroid
hormone preparation, is now approved to increase bone ■ BIMODAL PREVALENCE BY AGE
mass in men with primary or hypogonadal osteoporosis at
high risk for fracture. The prevalence of osteoporosis by age in men
and in women is quite different (FIGURE 1).
*Theauthor has indicated that he has received grant or research support from Merck, Lilly, Pfizer,
Whereas in women the distribution of osteo-
Aventis, Wyeth Ayerst, and Novartis corporations. This paper discusses treatment that is not porosis with age is skewed toward the later
approved by the US Food and Drug Administration for the use under discussion. years, in men many cases occur before age 50,
CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 70 • NUMBER 3 MARCH 2003 247
OSTEOPOROSIS IN MEN LICATA
Ascertainment bias. Fewer men than
Distribution of osteoporosis cases women undergo bone density measurement,
by age in men and women leading to the incorrect conclusion that men
do not get osteoporosis. However, the third
40
National Health and Nutrition Examination
Men Women Survey,3 using T-score criteria, found that
Percent of total cases
30
28% to 47% of men over age 50 have
osteopenia at the femoral neck, and 36%
have osteoporosis. For a 50-year-old man, the
20 lifetime risk for any fracture of the femur, ver-
tebrae, or distal forearm ranges from 13% to
50%.3
10
■ PRIMARY OSTEOPOROSIS
MAY BE DIFFERENT IN MEN
0
<40 41-50 51-60 61-70 71-80 81-90 >90 Primary osteoporosis is often ascribed to aging.
Some believe that in men it results from tra-
Age (years)
becular thinning rather than from trabecular
FIGURE 1. In women most cases of osteoporosis occur destruction, as seen in women.4
in the later years; in men the distribution is bimodal. With age, a variety of metabolic and
The early peak is mostly due to secondary osteoporosis, endocrine changes combine to weaken the
while the later peak mostly represents primary skeleton.5–10 Production of testosterone and
osteoporosis. growth hormone decreases, and muscles dete-
riorate. Calcium absorption becomes ineffi-
cient. Secondary hyperparathyroidism arises.
with a second peak in the later years. The Ambient parathyroid hormone levels are
Glucocorticoids cases early in life in men tend to be secondary higher in older than in younger patients.
osteoporosis and the later cases tend to be pri- Varying degrees of vitamin D dysfunction
attack the mary, although this is not always true. may be seen, from ineffective function to
skeleton on deficiency.
■ WHY FEWER MEN GET OSTEOPOROSIS
two fronts ■ CAUSES OF SECONDARY OSTEOPOROSIS
Although men do get osteoporosis, they have
a lower prevalence than women, for several Many diseases and drugs can cause secondary
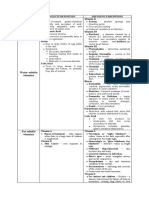
reasons: osteoporosis (TABLE 1).
Men accumulate more bone mass dur-
ing the peak growth years, making the adult Drug-induced bone loss
male skeleton generally stronger. They also Glucocorticoids top the list of drugs that
accumulate more muscle mass during puber- can cause osteoporosis. Although oral gluco-
ty, which contributes to skeletal strength. corticoids are the major culprits, potent
Men do not go through menopause. Male inhaled glucocorticoids may also have sys-
hormone production does not abruptly cease. temic effects on the skeleton.11
Instead, testosterone levels decline slowly Excessive doses of glucocorticoids have
throughout life unless there is an abrupt many bad effects on calcium and bone metab-
change (eg, due to surgical or chemical olism.12 They blunt intestinal calcium absorp-
orchiectomy). tion directly, even with adequate serum levels
Life expectancy for men has been short- of vitamin D, and secondary hyperparathy-
er than for women, so that primary osteoporo- roidism develops. Osteoclasts increase their
sis had less time to develop and cause fragility activity, and skeletal turnover increases. The
fractures. However, more men are now living drugs also directly blunt osteoblastic activity,
long enough to develop primary osteoporosis. thus attacking skeletal integrity on two fronts.
248 CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 70 • NUMBER 3 MARCH 2003
Renal tubulopathy and calciuria develop (a TA B L E 1
direct effect of the steroids), drawing calcium
from the body and exaggerating the hyper- Causes of secondary osteoporosis
parathyroid state. Sex steroid production Drugs
declines by suppression of gonadal function Alcohol
Anticonvulsants
and pituitary gonadotropin secretion. Antigonadotropins
However, many other drugs can cause Glucocorticoids (oral, inhaled)
osteopenia, osteoporosis, and osteomalacia,13 Nonsteroidal anti-inflammatory drugs
including: Thyroxine
• Anticonvulsants, which enhance vita- Tobacco
min D metabolism and cause calcium malab- Endocrine
sorption and secondary hyperparathyroidism Acromegaly
• Antigonadotropic drugs used in treating Hypercortisolism
Hyperparathyroidism
prostate cancer are known to cause osteope- Hyperprolactinemia
nia, but the true incidence of clinical osteo- Hyperthyroidism
porosis and fracture rates is not known. Hypogonadism
Tobacco and alcohol are both directly Gastrointestinal
toxic to the skeleton. Alcohol use is an inde- Cirrhosis
pendent risk factor for osteoporosis.14 It sup- Inflammatory bowel disease
presses osteoblast activity: intake of as little as Malabsorption
50 g (four standard drinks) per day causes a Genetic and metabolic
dose-dependent decrease in osteocalcin, a Homocystinuria
marker of osteoblastic activity. Higher intakes Hypophosphatasia
(>100 g/day) used for years cause decreased Marfan syndrome
Osteogenesis imperfecta
skeletal mass.15 However, moderate drinking
is not deleterious. Neoplastic
Anemia (vitamin B12 deficiency, thalassemia)
Leukemia
Gastrointestinal diseases Myeloma, benign gammopathies
Gastrointestinal diseases such as primary liver
disease (with or without cirrhosis), ulcers Neurologic
Disuse syndrome
requiring gastrectomy, inflammatory bowel Glucocorticoid, adrenocorticotropin therapy for myasthenia
disease, pancreatic insufficiency, and malab- gravis, multiple sclerosis
sorptive problems cause osteoporosis and, at Immobilization
times, osteomalacia.16–19 Alcoholic cirrhosis, Muscle atrophy
primary biliary cirrhosis, and steroid-treated Paralysis
autoimmune hepatitis lead more to osteoporo- Pulmonary
sis than to osteomalacia. Cystic fibrosis
Drug therapy for asthma, chronic obstructive pulmonary disease
Idiopathic pulmonary fibrosis
Hypercalciuria:
Hyperabsorptive or renal tubular? Renal
Hypercalciuria, with or without stone disease, Chronic renal failure, dialysis
Mineral-losing tubulopathies
is found in 20% of men with osteoporosis eval- Stone disease
uated in our clinic. Often, it is occult and is
not associated with overt stone disease. In my Transplantation bone disease
Lung, liver, heart, kidney
experience, patients with latent calciuria may
have normal calcium excretion because their
calcium intake is low, but if you give them a
calcium supplement for a week and remeasure The hyperabsorptive problem is associated
their calcium excretion, it will be high. with increased or high-normal levels of 1,25
Both hyperabsorptive hypercalciuria and dihydroxyvitamin D. This above-normal level
renal tubular hypercalciuria (renal leak) are increases bone metabolism and, consequently,
associated with osteopenia and osteoporosis. skeletal loss.20–24
CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 70 • NUMBER 3 MARCH 2003 249
OSTEOPOROSIS IN MEN LICATA
In renal tubular hypercalciuria, initially Primary hyperthyroidism is an unlikely
there is a failure to reclaim urinary calcium, cause of osteoporosis because it is usually diag-
and serum levels decline. A sustained com- nosed long before it can destroy the skeleton.
pensatory rise in serum parathyroid hormone The real concern is exogenous hyperthy-
corrects this drop in calcium at the expense of roidism caused by thyroxine supplementation
increased bone turnover. that suppresses thyroid-stimulating hormone.
Renal tubular acidosis is another entity to However, this should not be a clinically signif-
be mindful of.25 icant issue now that we have sensitive assays
for thyroid-stimulating hormone, bone densit-
Endocrine disorders ometry, and therapy to counteract bone loss.
Several endocrine disorders are well-known Acromegaly can lead to osteoporosis para-
causes of osteoporosis. The clinical challenge doxically, apparently when a growing pituitary
is when they occur in an atypical or occult tumor produces less gonadotropin, thus sup-
fashion. pressing testosterone synthesis.
Hypogonadism during puberty is an estab-
lished cause of adult skeletal deficiency, pri- Other causes
marily as it inhibits the development of peak Plasma cell dyscrasias cause osteoporosis
bone mass.26–28 In a young patient, replace- or osteopenia.
ment of sex steroids may reverse the problem. Multiple myeloma and even benign mon-
Abrupt hypogonadism in adult men fol- oclonal gammopathy increase bone
lowing chemical or surgical orchiectomy (eg, turnover.30 This skeletal effect arises from
for the treatment of prostate cancer)29 is increased osteoclastic activity due to the elab-
comparable to menopause in women and is oration of cytokines within the bone marrow.
equally destructive to the skeleton. On the The degree to which these disorders are occult
other hand, the milder forms of hypogo- and go undiagnosed determines the extent of
nadism of aging have not been shown to skeletal destruction.
cause bone loss. Leukemia may also be associated with
Fracture may be Hyperparathyroidism causes bone bone destruction if sufficiently occult and
the only destruction, although skeletal problems such chronic.31
as osteitis fibrosis cystica are rare nowadays Benign hematologic disorders such as
presenting because this disorder is usually discovered thalassemia and vitamin B12 deficiency also
early in routine health care evaluations and contribute to bone loss.32,33
feature in some laboratory testing. More than 80% of patients Focal metastatic disease causes local bone
men with occult with hyperparathyroidism have no symptoms, destruction, not systemic osteoporosis.
however. Secondary and tertiary hyper- Humoral hypercalcemia of malignancy is
endocrine parathyroidism of renal disease is not a diag- not a clinically significant cause of osteoporo-
disorders nostic challenge, but it is often overlooked, sis, since it portends a short prognosis.
even in patients on renal dialysis. Genetic or metabolic disorders known to
Endogenous hypercortisolism can pre- cause osteoporosis or osteopenia include
sent atypically. About 5% of patients present homocystinuria, Marfan syndrome, hypophos-
with osteoporosis and never show the typical phatasia, and osteogenesis imperfecta.34–37 A
features of cortisol excess, such as centripetal family history of any skeletal disorder should
obesity, aberrant deposition of fat, diabetes raise our suspicion, although the rarity of
mellitus, or hypertension. Fractures may be many of these disorders makes them less likely
the only presenting characteristic. considerations in general medical practice.
Hyperprolactinemia in men is insidious.
Unrecognized, it decreases testosterone pro- ■ BONE DENSITOMETRY AND T SCORES
duction and libido and in theory can cause
osteoporosis. Whether fractures develop, how- Bone densitometry is the greatest single
ever, depends on other issues, such as chronic- advance that has made possible the awareness,
ity of the disorder, initial peak bone mass, and diagnosis, and early treatment of osteoporosis.
traumatic events. Dual energy x-ray absorptiometry of the spine
250 CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 70 • NUMBER 3 MARCH 2003
and hip can detect osteoporosis in women and TA B L E 2
men quite early in its course.
I believe that bone density evaluation Diagnostic evaluation
should be mandatory for men after age 60 or of osteoporosis in men
65 if there is no specific history of unex- History
plained fracture, and certainly before this age Family history
in any man with a history of low trauma frac- Past medical history (secondary causes identifiable)
ture. Guidelines for its use are likely to be the Health habits (use of alcohol or tobacco, lack of exercise)
same for men as for women, although this has Drug use (bone-toxic agents)
not been clearly delineated. Physical examination
Unfortunately, although the federal Bone Signs of specific diseases
Mass Measurement Act requires Medicare to
pay for bone density measurements for women Initial laboratory evaluation
within certain guidelines, men have not yet Complete blood cell count
Complete chemical profile
been included. One hopes that Congress will
Parathyroid hormone
rectify this omission. 25 vitamin D
24-hour urinary calcium
Caveats about T scores
The T score, used to determine the risk for Follow-up laboratory evaluation
fracture in women, is also used in men, but Urine cortisol
Serum testosterone
with a caveat: a male data base must be used
Protein electrophoresis of serum
for deriving the score. Serum growth hormone
Recall that the T score is the number of Insulin-like growth factor 1
standard deviations (SD) below or above the Prolactin
mean value in a reference population. If a
female data base is used, only 3% to 5% of
men have osteoporosis, whereas 30% of men
over age 50 have osteopenia or osteoporosis Do not
when a male data base is used. Hence, a male dard deviations below the mean) are at greater
data base is mandatory for accurate diagnosis risk than people with higher scores, but the withhold
of osteoporosis in men. score alone does not diagnose osteoporosis: treatment until
The definitions of disease by T scores are the clinician diagnoses osteoporosis on the
the same for men as for women. A T score of basis of the personal and family history, phys- the T score
2.5 or more standard deviations (SD) below ical examination, laboratory values, and bone reaches an
the mean (ie, < –2.5 SD) is classified as osteo- densitometry.
porosis. (Remember that these are negative arbitrary
numbers, so –3.5 is less than –2.5.) A T score ■ CLINICAL AND LABORATORY DIAGNOSIS number
of –1.5 to –2.5 is classified as osteopenia, and OF OSTEOPOROSIS IN MEN
a T score of –1.5 or higher is normal.
But T scores should only be considered as In men, we should consider primary osteo-
guidelines for detection of osteoporosis. porosis only after ruling out a specific cause. In
Treatment should not be withheld until a women, too, we should never assume that
patient’s T score reaches a specific level. osteoporosis is primary: the high incidence of
Rather, the diagnosis and decision to treat primary disease in women often obscures con-
should be based on clinical criteria. sideration of secondary causes, but secondary
Sometimes, treatment should be started before causes do exist and need to be considered.
the T score declines to –2.5, for example, in
patients taking glucocorticosteroids. History and physical examination
Moreover, there is no “safe” T score, ie, no In most men with osteoporosis, the history
discrete cutoff for “osteoporosis” or “no osteo- raises the suspicion of a possible cause, which
porosis.” The scores are a continuum of frac- is then pursued with appropriate laboratory
ture risk. People with lower scores (more stan- and radiologic testing (TABLE 2).
CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 70 • NUMBER 3 MARCH 2003 251
OSTEOPOROSIS IN MEN LICATA
A family history of osteoporosis is as ing, tetracycline-labeled biopsy of the skeleton
important a consideration in men as it is in might be helpful. Histologic study may show
women. Osteoporosis in family members is a unexpected findings, such as hematologic dis-
risk factor, especially in families with a ten- ease or osteomalacia. In our clinical experi-
dency toward small, thin stature. In addition, ence, however, biopsy has not proven as help-
pediatric data show similarities in bone densi- ful as laboratory or clinical data. Nonetheless,
ty of parents and their children.38,39 it should be kept in mind, such as in a patient
The physical examination may reveal with a continuing history of fractures or bone
cushingoid features, acromegaly, or hypogo- pain and no obviously abnormal laboratory
nadism, or evidence of blood dyscrasias or can- tests.
cer, liver disease, or pathognomonic skeletal
abnormalities. ■ TREATING SECONDARY
OSTEOPOROSIS IN MEN
Laboratory testing more extensive in men
The biochemical evaluation tends to be more Treating osteoporosis in men usually implies
extensive in men with osteoporosis because treating the underlying cause. The
the bone loss is usually secondary to another reversibility of osteoporosis after the under-
condition. The younger the male patient, the lying cause is controlled or eliminated
more important the laboratory evaluation. depends on the degree of bone damage.
A tiered evaluation is recommended, pro- Treatment of hypercortisolism, hyper-
ceeding from routine to more exotic metabol- parathyroidism, acromegaly, or hyperpro-
ic and endocrine tests. lactinemia can reverse bone loss to varying
Routine biochemical profiles and a com- degrees. Resolution of a deficiency, such as
plete blood cell count may reveal suspicious hypogonadism or vitamin D deficiency, may
findings that should be evaluated further, such be all that is needed.
as abnormalities in calcium, phosphorus, other Skeletal disease due to intestinal or drug-
electrolytes, alkaline phosphatase, liver or kid- induced malabsorption often responds well to
Measure 24- ney function, and blood counts. calcium and vitamin D supplementation.
hour calcium Routine urine testing for 24-hour excre- Drug-related bone loss should, in theory,
tion of calcium is suggested initially in all men respond to stopping the drug, but this may not
excretion in all because hypercalciuria is common. Levels of be easy. For example, the therapeutic need for
men with urinary phosphorus and other substances, such glucocorticoids may preclude stopping them.
as amino acids or sugars, may be evaluated Fortunately, the bisphosphonates alendronate
osteoporosis later if there is suspicion of renal tubulopathy (Fosamax) and risedronate (Actonel) are
and associated bone disease. available for patients using glucocorticoids,
Measurement of parathyroid hormone and and these two drugs should be prescribed pro-
25-hydroxyvitamin D may uncover subtle sec- phylactically when chronic steroid treatment
ondary hyperparathyroidism or vitamin D is started.
deficiency. Thiazide diuretics can stop renal calcium
In rare cases, evaluation for hypophos- loss and reverse skeletal deficiency to varying
phatasia, homocystinuria, or osteogenesis degrees.
imperfecta might be needed. Evaluate for Treatment of various neoplastic diseases
hypophosphatasia in patients with fracture may control the skeletal disease and fractures
and low serum alkaline phosphatase. Evaluate attending these illnesses, but additional bone-
for homocystinuria in those with physical fea- specific therapies are often needed.
tures and a history of fracture. Evaluate for
osteogenesis imperfecta in those with a family ■ TREATING IDIOPATHIC
history, fracture as a child, and physical fea- OSTEOPOROSIS IN MEN
tures.
Idiopathic osteoporosis in men was not satis-
Skeletal biopsy factorily treated until the recent approval of
If no abnormality is found on laboratory test- alendronate for use in men.
252 CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 70 • NUMBER 3 MARCH 2003
Nonpharmacologic measures high cost and parenteral route of administra-
Nonpharmacologic measures alone are not tion are limitations to its widespread use,
sufficient. Nevertheless, calcium and vitamin however.
D supplementation and exercise should be
part of any treatment program for men. A Sodium fluoride
healthy lifestyle with smoking cessation and Sodium fluoride has long been used in women
limited use of alcohol is as important in men as an osteoblastic stimulator, and most studies
as it is in women. of its efficacy have been in women. Its use in
men has not been fully evaluated, but there
Hormonal therapy are limited studies.50 Unfortunately, the safety
Testosterone therapy is marginally effec- margin is narrow.51 In women, excessive doses
tive in the hypogonadism of aging but is more produce dense but poor-quality bone that is
effective in hypogonadism of younger prone to fracture.
men.40,41
Estradiol has been found, in a few rare Bisphosphonates
cases, to have a positive effect on the male Alendronate is the first drug to show effi-
skeleton, although the true clinical signifi- cacy in men in a well-controlled trial, increas-
cance of this is not yet known.42,43 ing skeletal density comparably to levels seen
Calcitonin has not undergone any large in women. Its effects do not appear to depend
studies in men with primary osteoporosis, on testosterone levels. The study was not sta-
although small increases in bone density and a tistically powered to evaluate the efficacy of
reduction in vertebral fractures were seen in fracture reduction, but a tendency in that
major studies in women.44 direction was noted.52
Parathyroid hormone increases skeletal Etidronate in cyclical regimens is used in
density in men,45 but its full potential has not women and, theoretically, should help men.
been explored. A commercial product, teri- Risedronate should also be beneficial.53–55
paratide (Forteo), has received FDA approval
for use in men and women.46 ■ PREVENTION IS BEST TREATMENT Calcium,
Growth hormone increases bone density
in patients with adult growth hormone defi- The take-home message is essentially the
vitamin D,
ciency.47 Since growth hormone secretion same as that for women: prevention is better exercise are
decreases with aging, its use has theoretical than treatment, given the limited treatment
merit in the treatment of osteoporosis.48,49 Its options at the moment.
part of any
treatment plan
■ REFERENCES
1. Diamond TH, Thornley SW, Sekel R, Smerdely P. Hip frac- 8. Gallagher JC, Kinyamu HK, Fowler SE, Dawson-Hughes B, in men
ture in elderly men; prognostic factors and outcomes. Med Dalsky GP, Sherman SS. Calciotropic hormones in bone
J Aust 1997; 167:412–415. markers in the elderly. J Bone Miner Res 1998;
2. Center JN, Nguyen TV, Schneider D, Sambrook PN, Eisman 13:475–482.
JA. Mortality after all major types of osteoporotic fracture 9. Lau KH, Baylink DJ. Vitamin D therapy of osteoporosis:
in men and women: an observational study. Lancet 1999; plain vitamin D therapy vs active vitamin D analog (D-hor-
353:878–882. mone) therapy. Calcif Tissue Int 1999; 65:296–306.
3. Looker AC, Orwoll ES, Johnston CC, et al. Prevalence of 10. Orwoll ES, Meier DE. Alterations in calcium, vitamin D in
low femoral bone density in older US adults from the parathyroid hormone physiology in normal men with
NHANES III. J Bone Miner Res 1997; 12:1761–1783. aging: relationship to the development of senile osteope-
4. Jaron JJ, Makins NB, Sagreiya K. The microanatomy of tra- nia. J Clin Endocrinol Metab 1986; 63:1262–1269.
becular bone loss in normal aging men and women. Clin 11. Lipworth BJ. Systemic adverse effects of inhaled cortico-
Orthop 1987; 215:260–271. steroid therapy: a systematic review and meta analysis.
5. Portale AA, Lonergan ET, Tanney D, Halloran BP. Aging Arch Intern Med 1999; 159:941–955.
alters calcium regulation of serum concentration of 12. Zaqqa D, Jackson R. Diagnosis and treatment of glucocorti-
parathyroid hormone in healthy men. Am J Physiol 1997; coid-induced osteoporosis. Cleve Clin J Med 1999; 63:221–230.
272:139–146. 13. Tannirandom P, Epstein S. Drug-induced bone loss.
6. Cahaupey MC, Durr F, Chapui P. Age-related changes in Osteoporos Int 2000; 11:637–659.
parathyroid hormone and 25 hydroxy cholecalciferol lev- 14. Turner RT. Skeletal response to alcohol. Alcohol Clin Exp
els. J Gerontol 1983; 38: 19–22. Res 2000; 24:1693–1701.
7. Haden ST, Brown VM, Hurwitz S, Scott J, El-Elajj FG. The 15. Diamond T, Stiel D, Lunzer ML, et al. Ethanol reduces
effects of Asian gender on parathyroid hormone dynam- bone formation and may cause osteoporosis. Am J Med
ics. Clin Endocrinol 2000; 52:329–338. 1989; 86:282–288.
CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 70 • NUMBER 3 MARCH 2003 253
OSTEOPOROSIS IN MEN LICATA
16. Valentine F, Snisky CA. Prevention and treatment of osteoporosis in 18:48–51.
patients with inflammatory bowel disease. Am J Gastroenterol 1999; 38. Ferrari S, Rizzoli R, Slosman D, Bonjour TP. Familial resemblance for
94:878–883. bone mineral mass is expressed before puberty. J Clin Endocrinol
17. Vasquez H, Mazure R, Gonzalez D, et al. Risk of fractures in celiac dis- Metab 1998; 83:358–361.
ease patients: a cross-sectional, case control study. Am J 39. Lonzer MD, Imrie R, Rogers D, Worley D, Licata A. Effects of heredity,
Gastroenterol 2000; 95:183–189. age, weight, puberty, activity, and calcium intake on bone mineral
18. Vleggaar FP, VanBuuren HR, Wolfhagen FH, Schalm SW, Pols HA. density in children. Clin Pediatr 1996; 35:185–189.
Prevention and treatment of osteoporosis in primary biliary cirrhosis. 40. Finkelstein JS, Klibanski A, Neer RM, et al. Increase in bone density
Eur J Gastroenterol Hepatol 1999; 11:617–621. during treatment of men with idiopathic hypogonadotropic hypogo-
19. McCaughan W, Feller RB. Osteoporosis in chronic liver disease: patho- nadism. J Clin Endocrinol Metab 1999; 84:1966–1975.
genesis, risk factors and management. Dig Dis 1994; 12:223–231. 41. Snyder PJ, Peachey H, Hannoush P, et al. Effect of testosterone treat-
20. Borghi L, Meschi T, Guerra A, et al. Vertebral mineral content in diet- ment on bone mineral density in men over 65 years of age. J Clin
dependent and diet-independent hypercalciuria. J Urol 1991; Endocrinol Metab 1999; 84:1966–1972.
146:1334–1338. 42. Slemenda CW, Longcope C, Zhou L, et al. Sex steroids and bone mass
21. Bataille P, Achard JM, Fournier A, et al. Diet, vitamin D, and vertebral in older men; positive associations with serum estrogens and negative
mineral density in hypercalciuric calcium stone formers. Kidney Int associations with androgens. J Clin Invest 1997; 100:1755–1759.
1991; 39:1193–1205. 43. Smith EP, Boyd J, Frank GR, et al. Estrogen resistance caused by a
22. Ghazali A, Fuentes V, Desanaint C, et al. Low bone marrow density mutation in the estrogen receptor gene in a man. N Engl J Med 1994;
and peripheral blood monocyte activation profile in calcium stone 331:1059–1061.
formers with idiopathic hypercalciuria. J Clin Endocrinol Metab 1997; 44. Chesnut CH 3rd, Silverman S, Andriano K, et al. A randomized trial of
82:32–38. nasal spray salmon calcitonin in postmenopausal women with estab-
23. Audran M, Legrand E. Hypercalciuria. Joint Bone Spine 2000; lished osteoporosis. PROOF Study Group. Am J Med 2000;
67:509–515. 109:267–276.
24. Pietschrnann F, Bleslau NA, Pak CY. Reduced vertebral bone density 45. Slovik DM, Rosenthal DI, Doppelt SH, et al. Restoration of spinal bone
in hypercalciuric nephrolithiasis. J Bone Miner Res 1992; 7:1383–1388. in osteoporotic men by treatment with human parathyroid hormone
25. Domrongkitchaiporn S, Pongsakul C, Stitchantrakul W, et al. Bone (1-34) and 1,25-dihydroxyvitamin D. J Bone Miner Res 1986;
mineral density and histology in distal renal tubular acidosis. Kidney 1:377–381.
Int 2001; 59:1086–1093. 46. Neer RM, Arnaud CD, Zanchetta JR, et al. Effect of parathyroid hor-
26. Finkelstein JS, Neer RM, Biller B, et al. Osteopenia in men with a his- mone (1-34) on fractures and bone mineral density in post-
tory of delayed puberty. N Engl J Med 1992; 226:600–604. menopausal women osteoporosis. N Engl J Med 2001; 19:1434–1441.
27. Finkelstein JS, Klibanski A, Neer RM. A longitudinal evaluation of 47. Ho KK, Hoffman DM. Aging and growth hormone. Horm Res 1993;
bone mineral density in adult men with histories of delayed puberty. 40:80–86.
J Clin Endocrinol Metab 1996; 81:1152–1155. 48. Lissett CA, Shalet SM. Effects of growth hormone on bone and mus-
28. Berteloni S, Baroncelli G, Battini R, et al. Short-term effective testos- cle. Growth Horm IGF Res 2000; 10(suppl B):95–101.
terone treatment from reduced bone density in boys with constitu- 49. Baurn BM, Biller BMK, Finkelstein JS, et al. Effect of physiological
tional delay of puberty. J Bone Miner Res 1995; 10:140–148. growth hormone therapy on bone density and body composition in
29. Daniell HW. Osteoporosis after orchiectomy for prostate cancer. J patients with adult onset growth hormone deficiency: a randomized
Urol 1997; 157:439–444. placebo-controlled trial. Ann Intern Med 1996; 125:883–890.
30. Pecherstorfer M, Seibel MJ, Woitge HW, et al. Bone resorption in 50. Ringe JD, Rovaati LC. Treatment of osteoporosis in men with fluoride
multiple myeloma and in monoclonal gamrnopathy of undetermined alone or in combination with bisphosphonates. Calcif Tissue Int 2001;
significance: quantification by urinary pyridinium links of collagen. 69:252–255.
Blood 1997; 103:743–750. 51. Ringe JD, Rovati LC. Treatment of osteoporosis in men with fluoride
31. Hoorweg-Numan J, Kardos G, Roos JC, et al. Bone mineral density alone or in combination with bisphosphonates. Calcif Tissue Int 2001;
and markers of bone turnover in young adult survivors of childhood 69:252–255.
lymphoblastic leukemia. Clin Endocrinol 1999; 50:227–244. 52. Orwoll E, Ettinger M, Weiss S, et al. Alendronate for the treatment of
32. Wonke B, Jensen C, Hanslip JJ, et al. Genetic and acquired predispos- osteoporosis in men. N Engl J Med 2000; 343: 604–610.
ing factors in treatment of osteoporosis and thalassemia major. J 53. Haguenauer D, Welch V, Shea B, Tugwell P, Adachi JD, Wells G.
Pediatr Endocrinol Metab 1998; 11:795–801. Fluoride for the treatment of postmenopausal osteoporotic fractures:
33. Goerss JB, Kim CH, Atkinson EJ, et al. Risk of fractures in patients a meta-analysis. Osteoporos Int 2000; 11:727–738.
with pernicious anemia. J Bone Miner Res 1992; 7:573–579. 54. Cortet B, Vasseur J, Grardel B, et al. Management of male osteo-
34. Brenton DP, Dow CJ. Homocystinuria and Marfan syndrome: a com- porosis. Joint Bone Spine 2001; 68:252–256.
parison. J Bone Joint Surg 1972; 54:277–298. 55. Miller PD, Watts NB, Licata AA, et al. Cyclical etidronate in the treat-
35. Magid D, Pyeritz R, Fishman EK. Musculoskeletal manifestations of ment of postmenopausal osteoporosis: efficacy and safety after seven
the Marfan syndrome. Am J Roentgenol 1990; 155:99–104. years of treatment. Am J Med 1997; 103:468–476.
36. Weinstein RS, Whyte MP. Management of adult hypophosphatasia:
report of severe and mild cases. Arch Intern Med 1981; 141:727–731. ADDRESS: Angelo Licata, MD, PhD, Department of Endocrinology,
37. Bischoff H, Freitag P, Jundt G, Steinmann B, Tyndall A, Theiler R. Type Diabetes, and Metabolism, A30, The Cleveland Clinic Foundation, 9500
1 osteogenesis imperfecta: diagnostic difficulties. Clin Rheumatol 1999; Euclid Avenue, Cleveland, OH 44195.
INTERNAL
INTERNAL Clinical vignettes and questions on the differential
diagnosis and treatment of medical conditions
MEDICINE
MEDICINE likely to be encountered on the Qualifying IN THIS ISSUE
BOARD
BOARD Examination in Medicine — as well as in practice. PAGE 192
Take the challenge.
REVIEW
REVIEW
254 CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 70 • NUMBER 3 MARCH 2003
You might also like
- Osteoporosis: How To Treat Osteoporosis: How To Prevent Osteoporosis: Along With Nutrition, Diet And Exercise For OsteoporosisFrom EverandOsteoporosis: How To Treat Osteoporosis: How To Prevent Osteoporosis: Along With Nutrition, Diet And Exercise For OsteoporosisNo ratings yet
- 2014 OsteoporosisInMen ThematicReport EnglishDocument24 pages2014 OsteoporosisInMen ThematicReport EnglishTatia TsnobiladzeNo ratings yet
- Mayo Clinic Guide to Preventing & Treating Osteoporosis: Keeping Your Bones Healthy and Strong to Reduce Your Risk of FractureFrom EverandMayo Clinic Guide to Preventing & Treating Osteoporosis: Keeping Your Bones Healthy and Strong to Reduce Your Risk of FractureRating: 2 out of 5 stars2/5 (1)
- New and Developing Pharmacotherapy For Osteoporosis in Men: Expert Opinion On PharmacotherapyDocument13 pagesNew and Developing Pharmacotherapy For Osteoporosis in Men: Expert Opinion On Pharmacotherapyarber mulolliNo ratings yet
- Osteoporosis Men 10Document7 pagesOsteoporosis Men 10Claudia IrimieNo ratings yet
- Osteoporosis in The Aging Male: Treatment Options: BackgroundDocument16 pagesOsteoporosis in The Aging Male: Treatment Options: BackgroundcumbredinNo ratings yet
- The Pharmacological Management of OsteoporosisDocument6 pagesThe Pharmacological Management of Osteoporosisarber mulolliNo ratings yet
- Osteoporosis Self-Tool (OST) and Other Interventions At: Rural Promising Practice Issue BriefDocument6 pagesOsteoporosis Self-Tool (OST) and Other Interventions At: Rural Promising Practice Issue Briefaldex10No ratings yet
- Osteoprosis PDFDocument6 pagesOsteoprosis PDFsaeed hasan saeedNo ratings yet
- OsteoporosisDocument8 pagesOsteoporosisSoraya FadhilahNo ratings yet
- Screening, Diagnosis and Treatment of Osteoporosis: A Brief ReviewDocument7 pagesScreening, Diagnosis and Treatment of Osteoporosis: A Brief ReviewraffellaNo ratings yet
- Osteoporosis A ReviewDocument8 pagesOsteoporosis A ReviewAliza MustafaNo ratings yet
- Osteoporosis: Best PracticeDocument7 pagesOsteoporosis: Best PracticePerez Wahyu PurnasariNo ratings yet
- Osteoporosis: The Increasing Role of The Orthopaedist: ClassificationDocument10 pagesOsteoporosis: The Increasing Role of The Orthopaedist: ClassificationMila RevalinaNo ratings yet
- Osteoporosis A ReviewDocument8 pagesOsteoporosis A ReviewIga AmanyzNo ratings yet
- Osteoporosis and Periodontal Disease: History and Physical ExaminationDocument15 pagesOsteoporosis and Periodontal Disease: History and Physical ExaminationYenniy IsmullahNo ratings yet
- Osteoporosis: A Review: June 2016Document8 pagesOsteoporosis: A Review: June 2016Yolan TiaraNo ratings yet
- 2018 Update On OsteoporosisDocument16 pages2018 Update On OsteoporosisManel PopescuNo ratings yet
- What Is Osteoporosis?: Osteoposis Is A Disease ofDocument48 pagesWhat Is Osteoporosis?: Osteoposis Is A Disease ofTaruna GargNo ratings yet
- AAFP - Diagnosis and Management of Osteoporosis PDFDocument10 pagesAAFP - Diagnosis and Management of Osteoporosis PDFEvelyn LeonieNo ratings yet
- The Worldwide Problem of Osteoporosis: Insights Afforded by EpidemiologyDocument7 pagesThe Worldwide Problem of Osteoporosis: Insights Afforded by EpidemiologymgobiNo ratings yet
- A Review On Some Physiological Studies Related To OsteoporosisDocument14 pagesA Review On Some Physiological Studies Related To OsteoporosisAndy KumarNo ratings yet
- Health Teaching Plan - OsteoporosisDocument9 pagesHealth Teaching Plan - OsteoporosisAudrie Allyson Gabales100% (2)
- OsteoporosisDocument12 pagesOsteoporosisAzharul Islam ArjuNo ratings yet
- Orthopedic May 2013Document11 pagesOrthopedic May 2013javi222222No ratings yet
- Menopause: Medical Author: Medical EditorDocument4 pagesMenopause: Medical Author: Medical EditorJanethcita SencaraNo ratings yet
- Div Class Title Diet Nutrition and The Prevention of Osteoporosis DivDocument17 pagesDiv Class Title Diet Nutrition and The Prevention of Osteoporosis DivLucas Oliveira MouraNo ratings yet
- Osteoporosis: Current Concepts: Ibrahim Akkawi Hassan ZmerlyDocument6 pagesOsteoporosis: Current Concepts: Ibrahim Akkawi Hassan ZmerlyDimas M IlhamNo ratings yet
- Osteoporosis GTDocument15 pagesOsteoporosis GTZelalem AbrhamNo ratings yet
- Osteoporosis The Evolution in DiagnosisDocument12 pagesOsteoporosis The Evolution in DiagnosisPakistan RevolutionNo ratings yet
- General - OsteoporosisDocument9 pagesGeneral - OsteoporosisAsma NazNo ratings yet
- Shoolar Ederly OsteoDocument9 pagesShoolar Ederly OsteoBayu Surya AwalludinNo ratings yet
- Anchala Mahilange - jemds-ORADocument4 pagesAnchala Mahilange - jemds-ORAdrpklalNo ratings yet
- 1042 FullDocument9 pages1042 Fulloki harisandiNo ratings yet
- Treatment of Low Bone Density or Osteoporosis To Prevent Fractures in Men and Women: A Clinical Practice Guideline Update From The American College of PhysiciansDocument28 pagesTreatment of Low Bone Density or Osteoporosis To Prevent Fractures in Men and Women: A Clinical Practice Guideline Update From The American College of PhysiciansRoberto López MataNo ratings yet
- Osteoarthritis in Women: Effects of Estrogen, Obesity and Physical ActivityDocument15 pagesOsteoarthritis in Women: Effects of Estrogen, Obesity and Physical ActivitypakemainmainNo ratings yet
- Osteoporosis PaperDocument7 pagesOsteoporosis Paperapi-558387899No ratings yet
- Osteoporosis in Older AdultsDocument12 pagesOsteoporosis in Older AdultsJuan Diego Sandoval RojasNo ratings yet
- Osteoporosis PHD ThesisDocument5 pagesOsteoporosis PHD Thesislizsimswashington100% (2)
- Osteoporosis Essay ThesisDocument8 pagesOsteoporosis Essay Thesisnatalieparnellcolumbia100% (2)
- Osteoporosis PEDocument51 pagesOsteoporosis PENitin BansalNo ratings yet
- Patogenesis Osteoporosis V PDFDocument15 pagesPatogenesis Osteoporosis V PDFaji pangestuNo ratings yet
- Patogenesis Osteoporosis VDocument15 pagesPatogenesis Osteoporosis Vaji pangestuNo ratings yet
- Nutrition and Osteoporosis PreventionDocument9 pagesNutrition and Osteoporosis PreventionElizabeth DesiNo ratings yet
- 0059 The Osteoporosis RXDocument8 pages0059 The Osteoporosis RXJason YunNo ratings yet
- Clinical Review: OsteoarthritisDocument4 pagesClinical Review: OsteoarthritismarindadaNo ratings yet
- Menopause Di Puskesmas Stabat Kabupaten Langkat: Analisis Faktor Yang Memengaruhi Osteoporosis Pada IbuDocument13 pagesMenopause Di Puskesmas Stabat Kabupaten Langkat: Analisis Faktor Yang Memengaruhi Osteoporosis Pada IbuRun CapNo ratings yet
- ARTIGO OsteoporoseDocument25 pagesARTIGO OsteoporoseIndiara Lorena Barros Ribeiro Da SilvaNo ratings yet
- Group 5 OsteoporosisDocument17 pagesGroup 5 OsteoporosisFranchezka BeltranNo ratings yet
- Primary Osteoporosis in Postmenopausal WomenDocument5 pagesPrimary Osteoporosis in Postmenopausal WomenAzmi FarhadiNo ratings yet
- Osteoarthritis in Women Effects of Estrogen, Obesity and Physical ActivityvDocument15 pagesOsteoarthritis in Women Effects of Estrogen, Obesity and Physical ActivityvKanliajie Kresna KastiantoNo ratings yet
- Osteoporosis - 2022 CanvasDocument61 pagesOsteoporosis - 2022 CanvasSHEILA HADIDNo ratings yet
- Mpu3313 - v2 Mohamad Shafik Bin Supaat 821022145381001Document12 pagesMpu3313 - v2 Mohamad Shafik Bin Supaat 821022145381001محمد شافق ابنو شافعتNo ratings yet
- Effectiveness of Structured Teaching Programme On Knowledge Regarding Osteoporosis and Its Management Among Menopausal WomenDocument12 pagesEffectiveness of Structured Teaching Programme On Knowledge Regarding Osteoporosis and Its Management Among Menopausal WomenEditor IJTSRDNo ratings yet
- Public Health Nut8Document17 pagesPublic Health Nut8Fiki FerindraNo ratings yet
- Epid 1Document4 pagesEpid 1Annafiatu zakiahNo ratings yet
- AndrologyDocument298 pagesAndrologyPrakash JanakiramanNo ratings yet
- OsteoporosisDocument10 pagesOsteoporosisSandra Arely Rodriguez EscobarNo ratings yet
- Dental Radiography Associated With Term Low Birth Weight: RD 2.1 Radiasi Pada KehamilanDocument4 pagesDental Radiography Associated With Term Low Birth Weight: RD 2.1 Radiasi Pada KehamilanAnastasia PinkyNo ratings yet
- OsteopeniaDocument9 pagesOsteopeniaMohamed EssallaaNo ratings yet
- Conclusion Motor ControlDocument1 pageConclusion Motor ControlmegatNo ratings yet
- Background AthletesDocument1 pageBackground AthletesmegatNo ratings yet
- Casal2017 PDFDocument11 pagesCasal2017 PDFmegatNo ratings yet
- Informative Speech Template: (Describing Chart(s) And/or Graph(s) )Document2 pagesInformative Speech Template: (Describing Chart(s) And/or Graph(s) )megatNo ratings yet
- Notes Aerobic SystemDocument2 pagesNotes Aerobic SystemmegatNo ratings yet
- Advantages and Disadvantage Lactate SystemDocument1 pageAdvantages and Disadvantage Lactate SystemmegatNo ratings yet
- Lactate SystemDocument1 pageLactate SystemmegatNo ratings yet
- Vitamins, Minerals, Antioxidants, Phytonutrients, Functional FoodsDocument32 pagesVitamins, Minerals, Antioxidants, Phytonutrients, Functional Foodssatrijo salokoNo ratings yet
- Radical Longevity - Ann Louise GittlemanDocument444 pagesRadical Longevity - Ann Louise Gittlemandjole100% (3)
- Food and NutritionDocument7 pagesFood and NutritionprashantdhanvijayNo ratings yet
- Osteoporosis PowerpointDocument45 pagesOsteoporosis PowerpointAgustina Anggraeni Purnomo100% (1)
- Primal Hormones Made by Aesthetic Primal 1Document59 pagesPrimal Hormones Made by Aesthetic Primal 1enzopark776No ratings yet
- Drug Study Medcor AguinaldoDocument6 pagesDrug Study Medcor AguinaldoYana PotNo ratings yet
- NCM 105 Prelims NotesDocument24 pagesNCM 105 Prelims NotesJustine FloresNo ratings yet
- Oleh Ilham Syifaur Pembimbing Dr. Rahmad Syuhada, Sp. MDocument20 pagesOleh Ilham Syifaur Pembimbing Dr. Rahmad Syuhada, Sp. MMeta MedianaNo ratings yet
- Images - SupportArticles - PRODUCT PPT New 2018Document48 pagesImages - SupportArticles - PRODUCT PPT New 2018Shailendra Singh ChouhanNo ratings yet
- Case Study 1 Nut 116alDocument6 pagesCase Study 1 Nut 116alapi-249635202No ratings yet
- Centenarian inDocument155 pagesCentenarian inViktória MolnárNo ratings yet
- Covid Protocol DetoxDocument20 pagesCovid Protocol DetoxAlfred Sambulan83% (6)
- Vitamin D FracturesDocument11 pagesVitamin D FracturesHolger LundstromNo ratings yet
- Supplement Reference Guide: 1 Edition 2009Document234 pagesSupplement Reference Guide: 1 Edition 2009domNo ratings yet
- Pathogenesis of Osteoporosis 2: Cli Ord J. RosenDocument13 pagesPathogenesis of Osteoporosis 2: Cli Ord J. RosenRonald TejoprayitnoNo ratings yet
- Vitamin D and CalciumDocument33 pagesVitamin D and CalciumAkhmadRoziNo ratings yet
- Vitamin D and Skin DiseasesDocument32 pagesVitamin D and Skin DiseasesShree ShresthaNo ratings yet
- L37 - FPSC Saharanpur 4 G-36, Parshvnath Plaza, Court Road, SAHARANPUR-247001, Cont. - 9319141888Document13 pagesL37 - FPSC Saharanpur 4 G-36, Parshvnath Plaza, Court Road, SAHARANPUR-247001, Cont. - 9319141888Saurabh SinghNo ratings yet
- The Relationship of Nutrition and HealthDocument31 pagesThe Relationship of Nutrition and Healthcoosa liquorsNo ratings yet
- 2015 Evidence Analysis Library Evidence-Based Nutrition Practice Guideline For The Management of Hypertension in AdultsDocument31 pages2015 Evidence Analysis Library Evidence-Based Nutrition Practice Guideline For The Management of Hypertension in AdultscrackintheshatNo ratings yet
- BalanceOil Plus Premium enDocument4 pagesBalanceOil Plus Premium enTóthné MónikaNo ratings yet
- Water Soluble Vitamins: Vitamins Toxicity/Definition Deficiency/Definition Niacin Vitamin ADocument3 pagesWater Soluble Vitamins: Vitamins Toxicity/Definition Deficiency/Definition Niacin Vitamin ARoshin TejeroNo ratings yet
- Nutrition DietaryDocument35 pagesNutrition DietaryAbdul Quyyum100% (2)
- CV DR Aysha Habib KhanDocument18 pagesCV DR Aysha Habib KhanJumadil MakmurNo ratings yet
- Mcqs Upse 2007 Part 2Document14 pagesMcqs Upse 2007 Part 2Jasmine KumarNo ratings yet
- B2 - Effects of UV-C Treatment and Cold Storage On Ergosterol and Vitamin D2 Contents in Different Parts of White and Brown Mushroom (Agaricus Bisporus)Document6 pagesB2 - Effects of UV-C Treatment and Cold Storage On Ergosterol and Vitamin D2 Contents in Different Parts of White and Brown Mushroom (Agaricus Bisporus)Nadya Mei LindaNo ratings yet
- A Functional Approach Vitamins and MineralsDocument15 pagesA Functional Approach Vitamins and MineralsEunbi J. ChoNo ratings yet
- Orthopedics 5 1085Document8 pagesOrthopedics 5 1085Renata YolandaNo ratings yet
- Calcium and Oral Health: A Review: International Journal of Scientific Research September 2013Document3 pagesCalcium and Oral Health: A Review: International Journal of Scientific Research September 2013Maqbul AlamNo ratings yet
- Chap 18 Musculoskeletal SystemDocument29 pagesChap 18 Musculoskeletal SystemAna Dominique Espia100% (1)