Professional Documents
Culture Documents
XI. Nursing Care Plan
XI. Nursing Care Plan
Uploaded by
Edelweiss Marie Cayetano0 ratings0% found this document useful (0 votes)
9 views7 pagesOriginal Title
12753198-Nursing-Care-Plan-for-myocardial-infarction.doc
Copyright
© © All Rights Reserved
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views7 pagesXI. Nursing Care Plan
XI. Nursing Care Plan
Uploaded by
Edelweiss Marie CayetanoCopyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 7
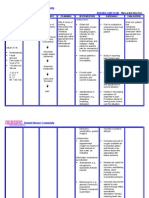
XI.
NURSING CARE PLAN
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective: Acute (Chest) STG: INDEPENDENT: STG:
Within 1 hour 1. assess 1. pain is indication of Within 1 hour of
The client Pain r/t
of nursing characteristics of MI. assisting the client nursing intervention,
reports of chest myocardial chest pain, including in quantifying pain the client had
interventions,
pain radiating toischemia resulting location, duration, may differentiate pre- improved comfort in
the client will
the left arm and from coronary have improved quality, intensity, existing and current chest, as evidenced
neck and back. artery occlusion comfort in chest, presence of radiation, pain patterns as well by:
with as evidenced by: precipitating and as identify States a
loss/restriction of States a alleviating factors, and complications. decrease in the
blood flow to an decrease in as associated rating of the chest
Objective: the rating of symptoms, have client pain.
area of the rate pain on a scale of
Restlessness myocardium and the chest pain. Is able to rest,
Facial Is able to 1-10 and document displays reduced
necrosis of the rest, displays findings in nurse’s tension, and
grimacing myocardium. notes. sleeps
reduced
Fatigue tension, and 2. obtain history of 2. this provides comfortably.
Peripheral sleeps previous cardiac pain information that may Requires
cyanosis comfortably. and familial history of help to differentiate decrease analgesia
Requires cardiac problems. current pain from or nitroglycerin.
Weak pulse
decrease previous problems and Goal was met.
Cold and complications.
analgesia or
clammy skin nitroglycerin. LTG:
Palpitations 3. assess respirations, 3. respirations may be The client had an
Shortness of LTG: BP and heart rate with increased as a result improved feeling of
The client will each episodes of chest of pain and associate control as evidenced
breath
have an pain. anxiety. by verbalizing a
Elevated 4. maintain bedrest 4. to reduce oxygen sense of control over
improved feeling
temperature of control as during pain, with consumption and present situation
Pain scale of evidenced by position of comfort, demand, to reduce and future outcomes
8/10 verbalizing a maintain relaxing competing stimuli and within 2 days of
sense of control environment to reduces anxiety. nursing intervention.
over present promote calmness. Goal was met.
situation and
future outcomes
within 2 days of 5. prepare for the 5.pain control is a
nursing administration of priority, as it indicates
interventions. medications, and ischemia.
monitor response to
drug therapy. Notify
physician if pain does
not abate.
6.istruct patient in 6. to decrease
nitroglycerin SL myocardial oxygen
administration after demand and workload
hospitalization. on the heart.
Instruct patient in
activity alterations
and limitations.
7. to promote
7. instruct knowledge and
patient/family in compliance with
medication effects, therapeutic regimen
side-effects, and to alleviate fear of
contraindications and unknown.
symptoms to report.
DEPENDENT: 1. serial ECG and stat
1. obtain a 12-lead ECGs record changes
ECG on admission, that can give evidence
then each time chest of further cardiac
pain recurs for damage and location
evidence of further of MI.
infarction as
prescribed.
2. Morphine is the
2. administer drug of choice to
analgesics as ordered, control MI pain, but
such as morphine other analgesics may
sulfate, meferidine of be used to reduce
Dilaudid N. pain and reduce the
workload on the heart.
3. administer beta- 3. to block
blockers as ordered. sympathetic
stimulation, reduce
heart rate and lowers
myocardial demand.
4. administer calcium- 4. to increase
channel blockers as coronary blood flow
ordered. and collateral
circulation which can
decrease pain due to
ischemia.
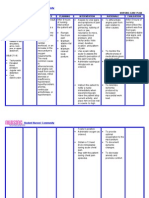
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
INDEPENDENT:
Subjective: Activity STG: 1. monitor heart rate, 1.changes in VS assist STG:
rhythm, respirations with monitoring Within 3 days of
The client Intolerance Within 3 days and blood pressure for physiologic responses to
reports of r/t cardiac of nursing abnormalities. Notify increase in activity.
nursing
increased dysfunction, interventions, physician of significant interventions,
work of changes in the client will be changes in VS. the client tolerated
breathing oxygen able to tolerate 2. Alleviation of factors activity without
2. Identify causative that are known to create excessive dyspnea
associated supply and activity without factors leading to intolerance can assist with
with feelings consumption excessive intolerance of activity. development of an
and had been able
of weakness as dyspnea and will activity level program. to utilize breathing
and tiredness. evidenced be able to utilize 3. encourage patient to 3. to help give the patient techniques and
by shortness breathing assist with planning a feeling of self-worth and energy
activities, with rest well-being. conservation
Objective: of breath. techniques and periods as necessary.
Increased energy 4. instruct patient in 4. to decrease energy
techniques
heart conservation energy conservation expenditure and fatigue. effectively.
rate techniques techniques. Goal was met.
Increased effectively. 5. assist with active or 5.to maintain joint
passive ROM exercises mobility and muscle tone. LTG:
blood at least QID.
pressure LTG: 6.to improve respiratory Within 5 days of
Dyspnea Within 5 days 6. turn patient at least function and prevent skin nursing
with of nursing every 2 hours, and prn. breakdown. interventions, the
exertion interventions, client increased
7. instruct patient in 7. to improve breathing and achieved
Pallor the client will be isometric and breathing and to increase activity
Fatigue and able to increase exercises. level. desired activity
weaknes and achieve level,
s desired activity 8. provide 8. to promote self-worth progressively, with
patient/family with and involves patient and no intolerance
Decreased level,
exercise regimen, with his family with self-care. symptoms noted,
oxygen progressively, written instructions.
saturatio with no such as respiratory
n intolerance DEPENDENT: compromise.
Ischemic symptoms 1.Assisst patient with 1. to gradually increase Goal was met.
ambulation, as ordered, the body to compensate
ECG noted, such as
with progressive for the increase in
changes respiratory increases as patient’s overload.
compromise. tolerance permits.
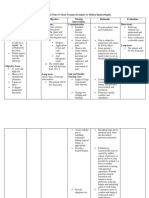
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
INDEPENDENT:
Subjective: Deficient STG: 1. monitor patient’s 1. to promote optimal STG:
readiness to learn and learning environment The client
The client Knowledge r/t The client will determine best methods when patient show
verbalizes new diagnosis be able to to use for teaching. willingness to learn.
verbalized and
questions and lack of verbalize and 2. provide time for 2. to establish trust. demonstrated
regarding understanding demonstrate individual interaction with understanding of
problems and of medical understanding patient. information given
3. instruct patient on 3. to provide information regarding condition,
misconceptions condition. of information procedures that may be to manage medication
about his given regarding performed. regimen and to ensure
medications, and
condition. condition, Instruct patient on compliance. treatment regimen
medications, medications, dose, within 3 days of
Objective: and treatment effects, side effects, nursing
contraindications, and interventions.
Lack of regimen within signs/symptoms to report 4. client may need to
improvement 3 days of to physician. increase dietary
Goal was met.
of previous nursing 4. instruct in dietary potassium if placed on
regimen interventions. needs and restrictions, diuretics; sodium should LTG:
Inadequate such as limiting sodium be limited because of The client had
or increasing potassium. the potential for fluid been able to
follow-up on LTG: retention.
instructions The client will 5. provide printed 5. to provide reference correctly perform all
given. able to correctly materials when possible for the patient and tasks prior to
Anxiety perform all for patient/family to family to refer. discharge.
tasks prior to reviews. Goal was met.
Lack of
6. have patient 6. to frovide information
understan- discharge. demonstrate all skills that that patient has gained
ding. will be necessary for a full understanding of
postdischarge. instruction.
7. instruct exercises to be 7. these are helpful in
performed, and to avoid improving cardiac
overtaxing activities. function.
DEPENDENT:
1. refer patient to cardiac 1. to provide further
rehabilitation as ordered improvement and
rehabilitation
postdischarge.
.
You might also like
- Nursing Care Plan For Myocardial Infarction NCPDocument8 pagesNursing Care Plan For Myocardial Infarction NCPderic87% (15)
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For Hypertensionmariejo89% (84)
- Nursing Care Plan (Bell's Palsy)Document3 pagesNursing Care Plan (Bell's Palsy)Yessamin Paith Roderos100% (3)
- Case Study Acute Myocardial InfarctionDocument11 pagesCase Study Acute Myocardial InfarctionChristine Elaine Batusin Ilagan91% (23)
- Decreased Cardiac Output Nursing Care PlanDocument4 pagesDecreased Cardiac Output Nursing Care Planjudssalangsang86% (7)
- Psych Nursing Complete Edited Royal PentagonDocument32 pagesPsych Nursing Complete Edited Royal PentagonRichard Ines Valino100% (68)
- Nursing Care Plan For Upper Resrpiratory Tract InfectionDocument2 pagesNursing Care Plan For Upper Resrpiratory Tract Infectionmariejo87% (31)
- Nursing Care Plan For HypocalcemiaDocument1 pageNursing Care Plan For Hypocalcemiamariejo78% (18)
- NURSING CARE PLAN For Myocardial InfarctionDocument13 pagesNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- Nursing Care Plan For Coronary Artery DiseaseDocument3 pagesNursing Care Plan For Coronary Artery DiseaseLorraineAnneSantiagoCandelario91% (22)
- NCP Chest PainDocument2 pagesNCP Chest PainDOni Corleone85% (40)
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Nursing Care PlansDocument21 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Nursing Care PlansCarl Elexer Cuyugan Ano100% (1)
- Angina Pectoris Nursing Care PlanDocument1 pageAngina Pectoris Nursing Care PlanjamieboyRN86% (7)
- Acute Myocardial InfarctionDocument35 pagesAcute Myocardial Infarctionvirnzrobz80% (10)
- Nursing Care Plan For Angina Pectoris NCPDocument2 pagesNursing Care Plan For Angina Pectoris NCPderic73% (15)
- Myocardial Infarction Case StudyDocument19 pagesMyocardial Infarction Case Studyapi-312992151No ratings yet
- Nursing Care Plan Congestive Heart FailureDocument2 pagesNursing Care Plan Congestive Heart FailureRalph Dumawaa60% (5)
- Nursing Care Plan - Myocardial InfarctionDocument3 pagesNursing Care Plan - Myocardial Infarctionderic80% (10)
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- NURSING CARE PLAN For Myocardial InfarctionDocument16 pagesNURSING CARE PLAN For Myocardial InfarctionFreisanChenMandumotan100% (1)
- Care Plan Unstable AnginaDocument4 pagesCare Plan Unstable Anginaالغزال الذهبي50% (6)
- Acute Myocardial Infarction - CSDocument49 pagesAcute Myocardial Infarction - CSMASII94% (17)
- Buergers Disease NCPDocument5 pagesBuergers Disease NCPNikko Dela Cruz100% (2)
- Nursing Care Plan - Pericarditis PatientDocument2 pagesNursing Care Plan - Pericarditis Patientsandie_best78% (9)
- NCP For Pain OBDocument2 pagesNCP For Pain OBMao100% (18)
- Carotid Sinus Massage LeafletDocument3 pagesCarotid Sinus Massage LeafletGil Doy AlizerNo ratings yet
- Nerve ExpressDocument43 pagesNerve Expressrogneves100% (1)
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial InfarctionjamieboyRN88% (8)
- NURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument4 pagesNURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale Evaluationsweethoney220% (1)
- Case Study Myocardial InfarctionDocument23 pagesCase Study Myocardial InfarctionJester GalayNo ratings yet
- Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationsDocument3 pagesAssessment Nursing Diagnosis Planning Interventions Rationale EvaluationsAjay SupanNo ratings yet
- NCP Myocardial InfarctionDocument1 pageNCP Myocardial InfarctionjamieboyRN88% (8)
- Myocardial InfarctionDocument5 pagesMyocardial InfarctionDharline Abbygale Garvida AgullanaNo ratings yet
- NCP For Acute Coronary SyndromeDocument3 pagesNCP For Acute Coronary Syndromesarahtot75% (4)
- NCP Heart BlockDocument3 pagesNCP Heart BlockEköw Santiago Javier33% (3)
- Myocardial InfarctionDocument20 pagesMyocardial Infarction* mokhtar !!50% (2)
- Micu Case Study d1Document28 pagesMicu Case Study d1jmarc_2180% (5)
- Nursing Care PlanDocument7 pagesNursing Care PlanGem Ma100% (7)
- Myocardial Infarction NCPDocument3 pagesMyocardial Infarction NCPlapistolero33% (3)
- NCP - Acute Pain Related Myocardial IschemiaDocument2 pagesNCP - Acute Pain Related Myocardial IschemiaKian HerreraNo ratings yet
- NURSING CARE PLAN Decreased Cardiac Output FnaDocument2 pagesNURSING CARE PLAN Decreased Cardiac Output FnaAce Dioso Tubasco100% (1)
- CAD NCP Decreased Cardiac OutputDocument3 pagesCAD NCP Decreased Cardiac OutputLeizel Apolonio100% (3)
- NCP Chest PainDocument2 pagesNCP Chest PainLinsae Troy50% (2)
- Decreased Cardiac OutputDocument2 pagesDecreased Cardiac OutputDheza Rodis Santos0% (1)
- Case Presentation ON Myocardial Infarction: Bandana Budhathoki BSC Nursing 4 Year Roll No. 06Document32 pagesCase Presentation ON Myocardial Infarction: Bandana Budhathoki BSC Nursing 4 Year Roll No. 06Damin Fye100% (2)
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial InfarctionRocelyn CristobalNo ratings yet
- Assessment Diagnoses: Planning Intervention Rationale EvaluationDocument13 pagesAssessment Diagnoses: Planning Intervention Rationale EvaluationdaleaimeeNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument6 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationBalloonsRus PHNo ratings yet
- Diagnostic TestsDocument5 pagesDiagnostic TestsKathleen DimacaliNo ratings yet
- ACUTE PAIN BSN III KOLCABA NCP 8th ROTATIONDocument4 pagesACUTE PAIN BSN III KOLCABA NCP 8th ROTATIONKrisheille Amano MirandaNo ratings yet
- Nursing Care Plan For Myocardial Infarction NCPDocument8 pagesNursing Care Plan For Myocardial Infarction NCPRhomyrose CampanaNo ratings yet
- Cues and Objectives Explanation of The Problem Goals and Objectives Interventions Rationale EvaluationDocument4 pagesCues and Objectives Explanation of The Problem Goals and Objectives Interventions Rationale EvaluationShaina Fe RabaneraNo ratings yet
- N U R S I N G Care Plan For AterosclerosiDocument2 pagesN U R S I N G Care Plan For AterosclerosiRoxy TofyNo ratings yet
- NCPDocument2 pagesNCPDarien AquinoNo ratings yet
- Nursing Care Plan: Defining The Assessment Diagnosis Scientific Explanation Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Defining The Assessment Diagnosis Scientific Explanation Objectives Interventions Rationale EvaluationLovella Gonzales LimNo ratings yet
- Acute Pain!!!!!!!!!!!!!!!Document3 pagesAcute Pain!!!!!!!!!!!!!!!ahz_kerian2No ratings yet
- Angina PectorisDocument22 pagesAngina Pectorismacoy08No ratings yet
- NCPDocument4 pagesNCPfairwoods90% (10)
- NCP 3 in ER Module (Bernales, JLE)Document3 pagesNCP 3 in ER Module (Bernales, JLE)Jan Lianne BernalesNo ratings yet
- NCP - BSN12F - Pumbaya (Module 4)Document3 pagesNCP - BSN12F - Pumbaya (Module 4)Ellah PumbayaNo ratings yet
- NCP #1 Acute PainDocument3 pagesNCP #1 Acute PainJheanAlphonsineT.MeansNo ratings yet
- Final Zollinger-Ellison SyndromeDocument9 pagesFinal Zollinger-Ellison SyndromeGLYDEL CORDERONo ratings yet
- Nursing Care Plan: Subjective Cues: Sakit IndependentDocument4 pagesNursing Care Plan: Subjective Cues: Sakit IndependentalambatinjrrNo ratings yet
- Nursing Care Plan Age: 60 Years OldDocument4 pagesNursing Care Plan Age: 60 Years OldLouise GudmalinNo ratings yet
- NCP 2Document2 pagesNCP 2Loreily ShyreenNo ratings yet
- Nursing Care Plans: Vasovagal Response, Decreasing BP and Heart RateDocument3 pagesNursing Care Plans: Vasovagal Response, Decreasing BP and Heart RateRachelle Ann DomingoNo ratings yet
- Research On Curriculum DevelopmentDocument16 pagesResearch On Curriculum Developmentmariejo100% (8)
- Research On Curriculum DevelopmentDocument16 pagesResearch On Curriculum Developmentmariejo100% (8)
- Republic Act 7305Document28 pagesRepublic Act 7305mariejoNo ratings yet
- Front Page of Our ThesisDocument13 pagesFront Page of Our Thesismariejo100% (4)
- Principles of Managent of Hypovolemic Shock in ADocument43 pagesPrinciples of Managent of Hypovolemic Shock in Aasi basseyNo ratings yet
- International Journal of Biological & Medical Research: Case ReportDocument3 pagesInternational Journal of Biological & Medical Research: Case ReportAndreea Diana DrăgoiNo ratings yet
- Dominga A. Salmone vs. Employees' Compensation Commission and Social Security SystemDocument3 pagesDominga A. Salmone vs. Employees' Compensation Commission and Social Security SystemmarielNo ratings yet
- Animal TestingDocument39 pagesAnimal TestingU2103586 STUDENTNo ratings yet
- Electrophysiological Foundations of Cardiac Arrhythmias - A Bridge Between Basic Mechanisms and Clinical Electrophysiology (PDFDrive)Document689 pagesElectrophysiological Foundations of Cardiac Arrhythmias - A Bridge Between Basic Mechanisms and Clinical Electrophysiology (PDFDrive)drdpkrims100% (1)
- 31 - B - C SCIENCE PPPPPPPPDocument27 pages31 - B - C SCIENCE PPPPPPPPsandeep40694069No ratings yet
- Oleander PoisoningDocument26 pagesOleander PoisoningDr. Shatdal Chaudhary100% (3)
- QuestionsDocument9 pagesQuestionsDennis Dane AngelesNo ratings yet
- Time Frame BSN 33Document2 pagesTime Frame BSN 33CiaraNo ratings yet
- NS1p1 Theory and Clinical Workbook FALL 13 07-12-13 - CLeeDocument98 pagesNS1p1 Theory and Clinical Workbook FALL 13 07-12-13 - CLeefranciaeleazarNo ratings yet
- Jumpshot - DawinDocument3 pagesJumpshot - DawinFaith WangNo ratings yet
- Jurnal 2Document8 pagesJurnal 2AnggunbokingsNo ratings yet
- MTP 3 45-4 15hDocument15 pagesMTP 3 45-4 15hRohit Velury100% (1)
- 10th Ecc Uk Annual Congress Course Notes 2013 PDFDocument334 pages10th Ecc Uk Annual Congress Course Notes 2013 PDFdwiNo ratings yet
- Cardio DrillDocument22 pagesCardio DrillDemuel Dee L. BertoNo ratings yet
- Dr. Sagar Shah: Dept of Accident & Emergency Kokilaben Dhirubhai Ambani Hospital and Medical Research InstituteDocument21 pagesDr. Sagar Shah: Dept of Accident & Emergency Kokilaben Dhirubhai Ambani Hospital and Medical Research InstituteSagar ShahNo ratings yet
- VasoactivosDocument8 pagesVasoactivosrogelio cruzNo ratings yet
- Respiratory and Circulatory Systems: Activity Sheet No. 1Document7 pagesRespiratory and Circulatory Systems: Activity Sheet No. 1alexNo ratings yet
- BIOL 108 Syllabus 2017Document15 pagesBIOL 108 Syllabus 2017zakiyah rahimNo ratings yet
- Activity Intolerance YAp ER NCPDocument2 pagesActivity Intolerance YAp ER NCPmecz26100% (2)
- Comparative Anatomy - Circulatory SystemDocument78 pagesComparative Anatomy - Circulatory SystemElaine MacasaetNo ratings yet
- Jaring, Josephine Rivera 1816085500Document3 pagesJaring, Josephine Rivera 1816085500Analiza Rivera JaringNo ratings yet
- Greatest Kan Li - Gathering The Cosmic Energy PDFDocument47 pagesGreatest Kan Li - Gathering The Cosmic Energy PDFAlexandra Ioana NiculescuNo ratings yet
- Hypertenion EpidemiologyDocument10 pagesHypertenion Epidemiologyororac_nyamoriNo ratings yet
- Heart AttackDocument5 pagesHeart AttackSherilNo ratings yet
- Nursing Pharmacology Study GuideDocument53 pagesNursing Pharmacology Study Guidezsazsageorge100% (5)
- Bams Ug Syllabus 2010Document19 pagesBams Ug Syllabus 2010prince1900No ratings yet
- (Harsh Mohan) Textbook of Pathology (6th Ed.) - 433-476Document44 pages(Harsh Mohan) Textbook of Pathology (6th Ed.) - 433-476Ananta DasNo ratings yet