Professional Documents
Culture Documents
Community Health Workers For Universal Health-Care Coverage: From Fragmentation To Synergy
Uploaded by
cwag68Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Community Health Workers For Universal Health-Care Coverage: From Fragmentation To Synergy
Uploaded by
cwag68Copyright:
Available Formats
Policy & practice
Community health workers for universal health-care coverage: from
fragmentation to synergy
Kate Tulenko,a Sigrun Møgedal,b Muhammad Mahmood Afzal,c Diana Frymus,d Adetokunbo Oshin,e
Muhammad Pate,e Estelle Quain,d Arletty Pinel,f Shona Wyndg & Sanjay Zodpeyh
Abstract To achieve universal health coverage, health systems will have to reach into every community, including the poorest and hardest to
access. Since Alma-Ata, inconsistent support of community health workers (CHWs) and failure to integrate them into the health system have
impeded full realization of their potential contribution in the context of primary health care. Scaling up and maintaining CHW programmes
is fraught with a host of challenges: poor planning; multiple competing actors with little coordination; fragmented, disease-specific training;
donor-driven management and funding; tenuous linkage with the health system; poor coordination, supervision and support, and under-
recognition of CHWs’ contribution.
The current drive towards universal health coverage (UHC) presents an opportunity to enhance people’s access to health services and
their trust, demand and use of such services through CHWs. For their potential to be fully realized, however, CHWs will need to be better
integrated into national health-care systems in terms of employment, supervision, support and career development. Partners at the global,
national and district levels will have to harmonize and synchronize their engagement in CHW support while maintaining enough flexibility
for programmes to innovate and respond to local needs. Strong leadership from the public sector will be needed to facilitate alignment with
national policy frameworks and country-led coordination and to achieve synergies and accountability, universal coverage and sustainability.
In moving towards UHC, much can be gained by investing in building CHWs’ skills and supporting them as valued members of the health
team. Stand-alone investments in CHWs are no shortcut to progress.
was instrumental in making the case for this paradigm shift
From Alma-Ata to universal health coverage in health care by joining efforts with lead projects in Gua-
From the early years of primary health care, community-based temala, India, Indonesia and elsewhere, among them the
health workers and volunteers (henceforth referred to as com- Comprehensive Rural Health Programme in Jamkhed, India,
munity health workers [CHWs]) have played a key role in sat- established in 1970,4 which continues today. After the Com-
isfying the need and demand for essential health services. The mission’s pioneering work, hundreds of other faith-based
Alma-Ata Declaration states that primary health care “relies, groups and nongovernmental organizations (NGOs) have
at local and referral levels, on health workers, including physi- continued to refine community-based health-care models and
cians, nurses, midwives, auxiliaries and community workers as CHW programmes.
applicable, as well as traditional practitioners as needed, suitably After Alma-Ata, the eagerness of public health authorities
trained socially and technically to work as a health team and to produce national blueprints for the rapid scale-up of pri-
to respond to the expressed health needs of the community”.1 mary health care did, however, generally miss out on creating
The values and principles set down at Alma-Ata continue ample space for community participation. The comprehen-
to be relevant today, even though the primary-health-care siveness and continuity of care – so basic to the model – were
movement has encountered difficulties in many countries and soon replaced by selective interventions for focused results,
at many levels when seeking to put them into practice. With including selected maternal and child health interventions and
the growing momentum for making universal health cover- family planning. Well-intended, top down national planning
age (UHC) a core strategy for shaping the post-2015 global and external support created wave after wave of CHWs in
health agenda, known barriers to coverage and access must the making and reshaping, under different names and with
be overcome.2 This also applies to factors that undermine the different roles. Many countries and many communities can
role of CHWs in the health system. recall a history of training, deployment and failure of several
The path-finding pilots for community-based primary repeating initiatives, such as that in the United Republic of
health care and CHW models took place in nongovernmental Tanzania in the 1980s.5 Caught between the formal health
settings in the beginning of the 1970s. The Christian Medical system and the community and often in a “grey zone” between
Commission of the World Council of Churches, in proactive public, nongovernmental and private health systems, CHWs
engagement with the World Health Organization (WHO),3 were for a long time seen as a stopgap measure and did not
a
CapacityPlus, IntraHealth, 1776 I St, NW, Washington, DC 20006, United States of America (USA).
b
Norwegian Knowledge Center for the Health Services, Oslo, Norway.
c
Global Health Workforce Alliance, Geneva, Switzerland.
d
United States Agency for International Development, Washington, USA.
e
Federal Ministry of Health, Abuja, Nigeria.
f
Genos Global, Panama City, Panama.
g
Joint United Nations Programme on HIV/AIDS, Geneva, Switzerland.
h
Public Health Foundation of India, New Delhi, India.
Correspondence to Kate Tulenko (e-mail: ktulenko@capacityplus.org).
(Submitted: 10 March 2013 – Revised version received: 24 May 2013 – Accepted: 1 July 2013 )
Bull World Health Organ 2013;91:847–852 | doi: http://dx.doi.org/10.2471/BLT.13.118745 847
Policy & practice
Synergy for scaling up CHW programmes Kate Tulenko et al.
receive the adequate support needed for
Box 1. Commonly noted contributions of community health workers (CHWs)
sustainability.
When the epidemic of HIV infec- • CHWs who are properly trained, equipped and supported can take on a range of tasks that
tion set in, community-based care otherwise depend on mid-level health workers.
models found new expressions. The • CHWs extend care to underserved communities, where they enhance access to health
need to act grew organically out of the services and promote people’s trust, demand and use of such services.
affected communities in the early days • CHWs who speak the local language and identify with the local community convey health
of the epidemic. People living with HIV messages more effectively.
infection had no choice but to help one • CHW training and service contribute to capacity for community leadership.
another. What evolved was a system • CHWs recruited from the communities they serve are less likely to go elsewhere because
rooted in the local context and born out of difficult living conditions.
of friendship and a shared experience: • CHWs can help service users avoid trips to health facilities, which translates into saved
mothers supported mothers, gay men transportation costs and time.
supported gay men and grandmoth- • CHWs can meet some of the needs of homebound patients.
ers helped grandmothers. When the
early antiretrovirals became available,
ferent ways, brought in the voices of the In 2012, several initiatives were
projects and programmes funded by
CHWs and their communities and seek implemented to engage the services of
governments, donors and NGOs spotted
to optimize the potential contribution of CHWs and other health workers at the
the opportunity to utilize existing com-
skilled and supported CHWs to primary front line in providing improved ac-
munity HIV support networks and be-
health care (Box 1). cess to life-saving care. Together, these
gan funding training and development
initiatives brought to light a dearth of
for CHW programmes specific to the
operational research and a need for bet-
needs of HIV programmes, yet largely
without being part of the local health
Scale-up and sustainability ter synergies in knowledge management
and operations. They also revealed that
services and clinics. What started out Although some sustainable national
CHW programmes are still fragmented,
as community-based responses began to CHW programmes exist, such pro-
with many different programmes of
evolve into multiple, stand-alone CHW grammes have not achieved the scale-
different origins having evolved over
programmes focused on HIV care with up and sustainability envisioned at
time, and that this fragmentation can
varying degrees of formality, sustain- Alma-Ata. CHWs have traditionally
be linked in part to the way programmes
ability, success, support and reporting.6 been recruited, trained, employed and
and initiatives are funded by external
The use of CHWs for childhood supervised at the periphery of health
partners and coordinated at the country
development and maternal, neonatal ministry structures. Donors have gen-
level.12,13 The Global Health Workforce
and child health care has a long history, erally supported CHW programmes to
Alliance synthesized the findings from
as illustrated in India. The Accredited achieve goals linked to disease-specific
these consultations and has initiated
Social Health Activists (ASHA) model vertical programmes or for the perfor-
work to improve synergies across initia-
for the follow-up of women during mance of specific tasks such as family
tives and partners.
pregnancy, delivery and the postnatal planning, nutrition and immunization.
The experience with CHW pro-
period has been relatively successful in Moreover, CHWs often lack a career
grammes points to six key challenges
overcoming barriers to service delivery ladder or professional associations.
in terms of policy and practice, with
and increasing institutional deliveries.7 Although such vertical approaches may
implications for scale-up and sustain-
The ASHA programme has attained have resulted in short-term gains, pro-
ability. These are discussed in the fol-
roughly 70% coverage of both mothers gramme fragmentation, ownership and
lowing sections.
and neonates in participating areas.8 sustainability have been major concerns.
Lady health workers in Pakistan, The impact of CHWs can no longer
Neglect of CHWs in health
behvarz in the Islamic Republic of Iran, be taken on faith; rigorous effectiveness
workforce planning
agentes communitários de saúde in Bra- and cost-effectiveness data are needed.
zil, BRAC community health workers in Systematic reviews of studies comparing In most countries’ health workforce
Bangladesh, village health volunteers in CHWs with usual practices have shown strategies, district and local authorities
Thailand, and health extension workers the effectiveness of CHWs in promot- are responsible for hiring, managing
in Ethiopia all represent different suc- ing immunization and breastfeeding, and supporting CHWs at the front-line
cessful CHW models.9 Zambia agreed improving tuberculosis treatment out- facility and community levels without
on a national CHW strategy in 2010 comes and reducing child morbidity and strong guidance from the national level.
and implemented a community health mortality. The importance of integrating The creation of CHW programmes in
assistant programme in 2012. In August CHWs into the health system on the multiple “waves” throughout the past
2011 Nigeria held its very first national basis of a core set of skills defined at 30 years has contributed to severe
meeting on human resources for health, the national level and with appropriate fragmentation on the ground. There is
which brought together various partners supervision and support cannot be suf- a need for explicit principles and guid-
and representatives of all levels of gov- ficiently underscored. In this process, ance from the national level on ways of
ernment. Similar national meetings have due attention must be paid to the need integrating and aligning these efforts to
taken place in Kenya in 2011 and in 2013 for diverse training in keeping with the optimize synergies and build sustain-
the United Republic of Tanzania. These various roles and tasks performed by able platforms for the scale-up of CHW
programmes and processes have, in dif- CHWs on the ground.10,11 programmes towards achieving UHC.
848 Bull World Health Organ 2013;91:847–852 | doi: http://dx.doi.org/10.2471/BLT.13.118745
Policy & practice
Kate Tulenko et al. Synergy for scaling up CHW programmes
tives and partners. Although competi- Health Workforce Alliance’s programme
Multiple actors without
tion for funding among international, of Country Coordination and Facilita-
coordination
regional and national NGOs fosters tion for Human Resources for Health.
United Nations partners working in the creativity and momentum, it makes However, these coordination mecha-
sphere of health have direct or indirect competing NGOs disinterested in coop- nisms seldom cover programmes imple-
engagement with CHW programmes erating with one another. When NGOs mented under district-level authority at
and other community-based health ini- bid for contracts they feel compelled the health facility and community levels,
tiatives – often in diverging ways within to offer a product that is different from including CHW programmes.
the same country. Partners engaged what other NGOs offer. It therefore be- With the growing focus on scaling
in supporting CHW and community- hoves donors to incentivize cooperation up CHW programmes of differing scope
based programmes are seldom present among NGOs or to make it mandatory. and fit within the formal health system,
at the district or lower level but work decisive steps to ensure operational
Unclear identity
through contractors and implementers synergies are essential. Such steps must
without national or local mechanisms CHWs often operate in an environment be taken through agreed national poli-
for coordination. Faith-based and NGO- in which it is not clear whether they cies and with guidance and alignment
related private or community-based represent the community, an NGO, by all partners and they must allow for
CHW programmes have their own the health system or a combination flexibility and innovation. The aim must
contracts and arrangements for health of these. This can lead to confused be to optimize a health team approach
workers and barriers to communication responsibilities and accountabilities at the front line of the health system, fit
between public and NGO providers are among the various actors and deprives for the local context, with facility-based
not uncommon. CHWs of the support they need. CHWs and community-based health workers
interface between their communities working together. This approach may
Fragmented, disease-specific
and formal health systems and their result in slower progress at the outset
focus
roles and expectations must therefore be but will ensure long-term results and
Differences in the way interventions – in clarified and understood by all parties. sustainability.
family planning, nutrition, malaria, im- CHWs also face opposition from more It is the responsibility of every
munization, HIV-related care and ma- established health professionals, such national government to establish guide-
ternal and child health – are structured as physicians and nurses, who may see lines for scaling up CHW programmes
and supported add to the complexity them as a potential threat to their job that respond to local needs and realities.
of the situation. Training, management security and salaries. In most countries, A national inventory of ongoing pro-
and incentive structures differ widely. CHWs have never been integrated into grammes and community-based CHW
Results and accountability frameworks the established, salaried team of health initiatives is key to alignment among
for these programmes are not structured system workers, have never been profes- different programmes. The policy
to drive synergies across initiatives. Be sionalized and have never been given a framework for integration and align-
they local and free-standing or part of voice in the affairs of the health system ment of the tasks performed by different
nationwide efforts, programmes and or the non-state health sector.14 types of CHWs across different vertical
initiatives often stimulate piloting and initiatives must be agreed on by both
innovation. Yet because resulting in- funders and implementers. Specifically,
novations are not coordinated, they do Synergy, integration and the question of incorporating CHWs
not spread and programmes are not sustainability into the formal health system and the
scaled up. greater health workforce must be ad-
The challenges identified in this paper dressed, together with the mechanisms
Unclear link to the health system
stem from the “going it alone” approach for regulating their performance – i.e.
There is an urgent need for supervision applied by most funders and implement- setting standards for training, licenc-
and support for CHWs at the level of ers of CHW programmes, which has left ing, scope of work, career ladders and
programme implementation. The role of us with a legacy of parallel initiatives supervision.
the district and subdistrict levels in facili- funded separately, delivering separately District health management teams
tating coordination and ensuring synergy and reporting separately. If the isolated and local governments need to be
among multiple stakeholders and initia- health gains that have been achieved given the authority to bring together the
tives is often unclear. This is also true of through CHW programmes are to be implementing partners to enhance syn-
the accountability of CHW programmes sustained and scaled up to meet UHC ergies and programme alignment in ac-
to the district and community governance targets, a clear strategy for optimizing cordance with national guidance, make
structures for health and development. synergies and integration is needed. full use of the space for innovation,
This lack of clarity in the link of CHW Major steps have been taken at the and facilitate mutual learning. District
programmes to the health system under- national level, through a variety of col- health managers will need to work with
mines overall commitment to and capac- laborative frameworks, plans and strate- their community counterparts as appro-
ity for supervision and support. gies, to harmonize and coordinate the priate to track and act on CHW-related
actions of multiple entities in support of service data, keep coverage maps, ensure
Competing nongovernmental
health system development and service the necessary supervision and guidance,
organizations
delivery. Examples include sector-wide and track performance.
The “NGO challenge” acts as a further support platforms, the International Key to engaging CHWs to attain
barrier to synergy across CHW initia- Health Partnership and the Global UHC is the readiness of global and
Bull World Health Organ 2013;91:847–852 | doi: http://dx.doi.org/10.2471/BLT.13.118745 849
Policy & practice
Synergy for scaling up CHW programmes Kate Tulenko et al.
national partners and implementers to global initiatives, donors and interna- Isolated investment in CHWs is no
(i) value collaboration; (ii) comply with tional NGOs need to closely examine shortcut to progress.
national- and district-level guidance programming, funding and reporting CHWs can be effective, integral
on synergies and integration; (iii) share to minimize fragmentation and dupli- members of the health team. They can go
information; (iv) ensure sufficient local cation and ensure the scale-up of CHW beyond the provision of care and foster
flexibility and (v) monitor established programmes in the context of a trained, community-based action. As the MDG
indicators. As an alliance of key stake- equipped and supported health team. era comes to an end and a new era fo-
holders, the Global Health Workforce cused on UHC begins, the global health
Alliance is well placed to promote a community has a unique opportunity to
health system approach, with coordi-
Conclusion work with CHWs to create lasting health
nation across CHW initiatives, when As was made clear in the Alma-Ata improvements everywhere. ■
seeking programme scale-up at the Declaration and as is valid today, CHWs,
global, national and district levels. In whether hired by the formal health Funding: The views expressed in this
this context, new initiatives such as the system or selected and supported by publication are solely the authors’; they
One Million Community Health Work- communities, cannot be left to serve on do not necessarily reflect the views of the
ers Campaign, hosted by the United their own.15 CHW programmes need United States Agency for International
Nations Sustainable Development Solu- be comprehensive rather than vertical Development or the Government of the
tions Network and the Earth Institute, and they should rely on both the com- United States.
represent important opportunities for munity and the formal health system for
aligned action. Multilateral partners, supplies, communications and referrals. Competing interests: None declared.
ملخص
من التجزئة إىل التآزر:العاملون يف جمال الصحة املجتمعية من أجل التغطية الشاملة يف الرعاية الصحية
سوف، لتحقيق إمكانياهتم بشكل كامل، ومع ذلك.املجتمعية سيتعني عىل النظم الصحية،لكي تتحقق التغطية الصحية الشاملة
يتعني دمج العاملني يف جمال الصحة املجتمعية بشكل أفضل يف نظم بام يف ذلك املجتمعات األكثر فقر ًا وصعوبة،الوصول إىل كل جمتمع
الرعاية الصحية الوطنية فيام يتعلق بالتوظيف واإلرشاف والدعم أدى الدعم املتضارب من، ومنذ إعالن أملا – آتا.يف الوصول إليها
وسوف يتعني عىل الرشكاء عىل املستويات.والتطوير املهني جانب العاملني يف جمال الصحة املجتمعية والفشل يف دجمهم يف
العاملية والوطنية ومستويات املناطق تنسيق ومزامنة مشاركتهم النظام الصحي إىل عرقلة اإلدراك الكامل ملسامهتهم املحتملة يف
يف دعم العاملني يف جمال الصحة املجتمعية مع احلفاظ عىل ويشتمل تعزيز برامج العاملني يف.سياق الرعاية الصحية األولية
مرونة كافية للربامج من أجل االبتكار واالستجابة لالحتياجات ،جمال الصحة املجتمعية واحلفاظ عليها عىل جمموعة من التحديات
وسوف توجد حاجة إىل قيادة قوية من القطاع العام.املحلية سوء التخطيط؛ وتعدد األطراف املتنافسة مع قلة التنسيق فيام:هي
لتسهيل املواءمة مع أطر السياسة الوطنية والتنسيق بقيادة الدولة بينها؛ وتشتت التدريب املحدد لكل مرض؛ واإلدارة والتمويل
.ولتحقيق أوجه التآزر واملساءلة والتغطية الشاملة واالستدامة عن طريق اجلهة املانحة؛ وهشاشة الربط بالنظام الصحي؛ وسوء
يمكن حتقيق،وعند التحرك صوب التغطية الصحية الشاملة ونقص االعرتاف بمسامهة العاملني،التنسيق واإلرشاف والدعم
املزيد عن طريق االستثامر يف بناء مهارات العاملني يف جمال الصحة .يف جمال الصحة املجتمعية
وليست.املجتمعية ودعمهم كأفراد ذوي قيمة يف الفريق الصحي يقدم االجتاه الراهن صوب التغطية الصحية الشاملة فرصة
االستثامرات القائمة بذاهتا يف العاملني يف جمال الصحة املجتمعية لتعزيز وصول األشخاص إىل اخلدمات الصحية وثقتهم وطلبهم
.مسار ًا خمترص ًا إىل التقدم واستخدامهم هلذه اخلدمات من خالل العاملني يف جمال الصحة
摘要
全民医疗保障的社区卫生工作者 : 从零散到协同
为实现全民医疗保障 , 卫生系统必须深入每个社区 , 包 CHW 服务的信任、需求和使用。然而 , 要充分发挥潜
括最贫穷和最偏远的地方。阿拉木图对社区卫生工作 力 ,CHW 需要在就业、监督、支持和职业发展方面更
者 (CHW) 的支持不一致 , 无法将其融入卫生系统 , 因 好地融入国家卫生保健系统。全球、国家以及区域级
而阻碍了卫生工作者在初级卫生保健中充分发挥自身 别的合作者必须协调和同步对 CHW 的支持 , 同时保
的潜力。扩大和维护 CHW 计划充满各种挑战 : 规划 持足够的计划灵活性以便创新和响应地方需求。需要
不周 ; 多个行动者相互竞争、缺乏协调 ; 培训零散且 来自公共部门的强有力领导 , 以便更好地向国家政策
针对特定疾病 ; 管理和融资由捐赠者驱动 ; 卫生系统 框架和国家主导的协作看齐 , 从而实现协同效应和问
联动薄弱 ; 协调、监督和支持不力以及对社区卫生工 责制、全民覆盖和可持续性。在实现 UHC 过程中 , 在
作者的贡献没有充分的认识。 培养 CHW 的技能并支持其成为卫生团队宝贵成员方
当 前 实 现 全 民 医 保 (UHC) 的 动 力 带 来 了 这 样 的 面加大投入力度 , 会有不少收获。对 CHW 的孤立投
机会 : 改善人们使用卫生服务的状况 , 并增强人们对 入不是发展的捷径。
850 Bull World Health Organ 2013;91:847–852 | doi: http://dx.doi.org/10.2471/BLT.13.118745
Policy & practice
Kate Tulenko et al. Synergy for scaling up CHW programmes
Résumé
Les agents sanitaires des collectivités pour la couverture sanitaire universelle: de la fragmentation à la synergie
Pour parvenir à une couverture sanitaire universelle, les systèmes de puisse être pleinement réalisé, les agents sanitaires des collectivités
santé devront étendre leur portée à toutes les communautés, y compris devront toutefois être mieux intégrés dans les systèmes nationaux de
celles qui sont les plus pauvres et les plus difficiles d’accès. Depuis la soins de santé en termes d’embauche, de supervision, de soutien et
Déclaration de Alma-Ata, le soutien inégal des agents sanitaires des d’évolution de carrière. Les partenaires au niveau du monde, du pays
collectivités et l’échec de leur intégration dans les systèmes de santé ont et du district devront harmoniser et synchroniser leurs engagements
empêché la pleine réalisation de leur contribution potentielle dans le dans le soutien aux agents sanitaires des collectivités tout en maintenant
contexte des soins de santé primaires. Le développement et le maintien suffisamment de flexibilité pour permettre aux programmes d’innover
des programmes des agents sanitaires des collectivités se heurtent à et de répondre aux besoins locaux. Un leadership fort du secteur public
une multitude de défis à relever: mauvaise planification; multitude sera nécessaire pour faciliter l’alignement avec les cadres politiques
d’acteurs concurrents avec peu de coordination; formation fragmentée nationaux et la coordination dirigée par le pays et pour réaliser des
et spécifique aux maladies; gestion et financement à l’initiative synergies et des responsabilités, la couverture universelle et la durabilité.
des donateurs; lien ténu avec le système de santé; coordination, En avançant vers la couverture sanitaire universelle, il y a beaucoup à
supervision et soutien de mauvaise qualité, et sous-reconnaissance de gagner en investissant dans l’acquisition de compétences des agents
la contribution des agents sanitaires des collectivités. sanitaires des collectivités et en les soutenant en tant que membres à
La campagne actuelle vers une couverture sanitaire universelle offre part entière des équipes de santé. Les investissements autonomes au
une opportunité d’améliorer l’accès des personnes à des services de bénéfice des agents sanitaires des collectivités ne sont pas des raccourcis
santé, ainsi que leur confiance, demande et utilisation de tels services vers le progrès.
par le biais des agents sanitaires des collectivités. Pour que leur potentiel
Резюме
Роль местных медработников в деле обеспечения всеобщего охвата медико-санитарной помощью: от
отдельных инициатив к взаимодействию
Для обеспечения всеобщего охвата медико-санитарной повысить доверие, уровень спроса и использование таких
помощью системы здравоохранения должны быть внедрены служб через ММР. Тем не менее, чтобы в полной мере
во всех сообществах, включая самые бедные слои населения реализовать свой потенциал, местные медработники должны
и жителей, проживающих в труднодоступных регионах. быть в большей степени интегрированы в национальные
Кроме Алматы, отсутствует стабильная поддержка местных системы здравоохранения в вопросах трудоустройства, надзора,
медицинских работников (ММР), как и их полная интеграция поддержки и карьерного роста. Организации-партнеры на
в систему здравоохранения, что препятствует полноценной глобальном, национальном и региональном уровнях должны
реализации их полноценного вклада в оказание первичной гармонизировать и синхронизировать свою деятельность по
медико-санитарной помощи. Расширение охвата и программ поддержке ММР, сохраняя при этом достаточную гибкость
поддержки ММР усложняется значительным количеством для программ по внедрению инициатив и реагирования на
проблем: несовершенное планирование; множество локальные потребности. Понадобится проявление руководящей
конкурирующих участников, практически не координирующих воли со стороны государственных служб, чтобы обеспечить
между собой свою деятельность; фрагментированная подготовка, согласованность данных усилий с положениями национальной
специализирующаяся только на определенных заболеваниях; политики и координацию в масштабах страны для достижения
значительная зависимость управления и финансирования от взаимодействия и контролируемости, всеобщего охвата и
спонсоров; непрочные связи с системой здравоохранения; устойчивого развития. На пути внедрения всеобщего охвата
недостаточный уровень координации, надзора и поддержки, а медико-санитарной помощью много можно достигнуть путем
также недооценка вклада ММР. инвестиций в развитие профессиональных навыков у ММР и
Текущая тенденция к внедрению всеобщего охвата медико- поддержки их как ценных членов системы здравоохранения.
санитарной помощью предоставляет возможности улучшить Отдельные инвестиции в ММР не так перспективны для
доступ населения к службам здравоохранения, а также ускорения прогресса в данном направлении.
Resumen
Los trabajadores comunitarios de salud en la cobertura universal de la salud: de la fragmentación a la sinergia
A fin de lograr la cobertura universal de la salud, los sistemas sanitarios enfermedades específicas, la gestión y la financiación impulsadas
deben llegar a todas las comunidades, incluidas las más pobres y de por los donantes, la escasa unión con el sistema sanitario, la falta de
difícil acceso. Desde la conferencia de Alma-Ata, el apoyo inconstante coordinación, supervisión y apoyo, y la infravaloración de la contribución
de los trabajadores comunitarios de salud (TCS) y la falta de integración de los trabajadores comunitarios de la salud.
de estos en el sistema sanitario han impedido la plena realización de su El avance actual hacia la cobertura universal de la salud (CUS) ofrece
contribución potencial en el contexto de la atención primaria de la salud. una oportunidad para mejorar el acceso de la población a los servicios
La ampliación y el mantenimiento de los programas de trabajadores de salud, así como para aumentar la confianza, la demanda y el uso de
comunitarios de salud suponen muchos desafíos: la mala planificación, dichos servicios a través de los trabajadores comunitarios de salud. Sin
los agentes múltiples que compiten con insuficiente coordinación, la embargo, es necesario integrar mejor a los trabajadores comunitarios
fragmentación en los programas de capacitación orientados a combatir de salud, en términos de empleo, supervisión, apoyo y desarrollo
Bull World Health Organ 2013;91:847–852 | doi: http://dx.doi.org/10.2471/BLT.13.118745 851
Policy & practice
Synergy for scaling up CHW programmes Kate Tulenko et al.
profesional, en los sistemas nacionales sanitarios para aprovechar nacionales y la coordinación dirigida por el país, y para lograr sinergias
plenamente su potencial. Los socios a nivel mundial, nacional y local y la rendición de cuentas, la cobertura universal y la sostenibilidad. En
deben armonizar y sincronizar su compromiso a favor de los trabajadores la consecución de la cobertura universal de la salud, pueden obtenerse
comunitarios de salud, manteniendo la flexibilidad suficiente para que grandes beneficios si se invierte en el desarrollo de competencias de
los programas tengan capacidad de innovación y respuesta frente a los trabajadores comunitarios de salud, y se les apoya como miembros
las necesidades locales. Se requiere un fuerte liderazgo por parte del valiosos del equipo sanitario. Por el contrario, las inversiones aisladas
sector público para facilitar la alineación con los marcos de las políticas en trabajadores comunitarios de salud no son atajos hacia el progreso.
References
1. World Health Organization. Declaration of Alma-Ata. Geneva: WHO; 1978. 10. Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X,
Available from: http://www.who.int/publications/almaata_declaration_ van Wyk BE et al. Lay health workers in primary and community health care
en.pdf [accessed 19 July 2013]. for maternal and child health and the management of infectious diseases.
2. World Health Organization [Internet]. Universal health coverage: five Cochrane Database Syst Rev 2010;3:CD004015. PMID:20238326
questions. Geneva: WHO; 2013. Available from: http://www.who.int/ 11. Corluka A, Walker DG, Lewin S, Glenton C, Scheel IB. Are vaccination
health_financing/universal_health_coverage_5_questions.pdf [accessed programmes delivered by lay health workers cost-effective? A systematic
15 July 2013]. review. Hum Resour Health 2009;7:81. doi: http://dx.doi.org/10.1186/1478-
3. Litsios S. The Christian Medical Commission and the development of the 4491-7-81 PMID:19887002
World Health Organization’s primary health care approach. Am J Public 12. Naimoli JF, Frymus DE, Quain EE, Roseman EL. Community and formal health
Health 2004;94:1884–93. doi: http://dx.doi.org/10.2105/AJPH.94.11.1884 system support for enhanced community health worker performance: a US
PMID:15514223 Government evidence summit, final report. Washington: United States Agency
4. Mann V, Eble A, Frost C, Premkumar R, Boone P. Retrospective comparative for International Development; 2012.
evaluation of the lasting impact of a community-based primary health 13. Regional Network on Equity in Health in Southern Africa [Internet].
care programme on under-5 mortality in villages around Jamkhed, India. Consultation on improving access to health worker at the frontline for
Bull World Health Organ 2010;88:727–36. doi: http://dx.doi.org/10.2471/ better maternal and child survival: report. South Africa: EQUINET; 2012.
BLT.09.064469 PMID:20931057 Available from: http://www.equinetafrica.org/bibl/docs/Consultation%20
5. Heggenhougen KV, Muhondwa E, Rutabanzibwa-ngaiza J. Community FrontlineHW%20Rep%20June%202012.pdf [accessed 15 June 2013].
health workers: the Tanzanian experience. Oxford: Oxford Medical 14. CapacityPlus [Internet]. Professionalization of under-recognized health
Publications; 1987. pp. 154-71. worker cadres. Washington: United States Agency for International
6. Hermann K, Van Damme W, Pariyo GW, Schouten E, Assefa Y, Cirera A Development & CapacityPlus; 2010. Available from: http://www.
et al. Community health workers for ART in sub-Saharan Africa: learning capacityplus.org/files/resources/under-recognized-cadres-overview.pdf
from experience–capitalizing on new opportunities. Hum Resour Health [accessed 15 June 2013].
2009;7:31. doi: http://dx.doi.org/10.1186/1478-4491-7-31 PMID:19358701 15. Jaskiewicz W, Tulenko K. Increasing community health worker productivity
7. Gopalan SS, Mohanty S, Das A. Assessing community health workers’ and effectiveness: a review of the influence of the work environment. Hum
performance motivation: a mixed-methods approach on India’s Accredited Resour Health 2012;10:38. doi: http://dx.doi.org/10.1186/1478-4491-10-38
Social Health Activists (ASHA) programme. BMJ Open 2012;2:e001557. doi: PMID:23017131
http://dx.doi.org/10.1136/bmjopen-2012-001557 PMID:23019208
8. Sundararaman T, Ved R, Gupta G. Determinants of functionality and
effectiveness of community health workers: results from evaluation of ASHA
programme in eight Indian states. BMC Proc 2012;6(Suppl 5):O30.
9. Global Health Workforce Alliance [Internet]. Global experience of
community health workers for delivery of health related Millennium
Development Goals: a systematic review, country case studies, and
recommendations for integration into national health systems. Geneva:
World Health Organization; 2010. Available from: http://www.who.
int/workforcealliance/knowledge/themes/community/en/index.html
[accessed 14 July 2013].
852 Bull World Health Organ 2013;91:847–852 | doi: http://dx.doi.org/10.2471/BLT.13.118745
You might also like
- Efficacy, Effectiveness And Efficiency In The Management Of Health SystemsFrom EverandEfficacy, Effectiveness And Efficiency In The Management Of Health SystemsNo ratings yet
- Primary Health CareDocument20 pagesPrimary Health CareofficialmidasNo ratings yet
- Public Health Nursing: Scope and Standards of PracticeFrom EverandPublic Health Nursing: Scope and Standards of PracticeRating: 5 out of 5 stars5/5 (1)
- PHC HistoryDocument7 pagesPHC HistoryShafie Osman AliNo ratings yet
- 1 s2.0 S0020729215001356 MainDocument8 pages1 s2.0 S0020729215001356 MainRisky AchmadzNo ratings yet
- Strengthening Community Participation To Improve PHC in Rural NigeriaDocument14 pagesStrengthening Community Participation To Improve PHC in Rural NigeriaabdulrazzaqfctconsNo ratings yet
- Community Nursing and Care Continuity LEARNING OUTCOMES After CompletingDocument23 pagesCommunity Nursing and Care Continuity LEARNING OUTCOMES After Completingtwy113100% (1)
- Public Health Care and Community Strategy.: by MuokiDocument115 pagesPublic Health Care and Community Strategy.: by MuokisamiirNo ratings yet
- Community Oriented Primary Care COPC in District Health Services of Gauteng South AfricaDocument4 pagesCommunity Oriented Primary Care COPC in District Health Services of Gauteng South AfricaKim G. SarongNo ratings yet
- Chnii Updates@c16Document81 pagesChnii Updates@c16Avomah Ludger AvomahNo ratings yet
- NCM 104 Lecture Chapter 2.2 - PHC and UhcDocument50 pagesNCM 104 Lecture Chapter 2.2 - PHC and UhcWilma Nierva Beralde0% (1)
- Essentials of primary healthcareDocument13 pagesEssentials of primary healthcareHannah Villavicencio100% (1)
- Community Health WorkersDocument42 pagesCommunity Health WorkersGeethaNambiar100% (1)
- Concept of PHCDocument43 pagesConcept of PHCVantrigaru Veeresh Bangi93% (14)
- GiziiDocument56 pagesGiziisiti israwatiNo ratings yet
- CHN Chap 3-4Document68 pagesCHN Chap 3-4Kyla MoretoNo ratings yet
- The Contribution of Family Medicine To Community-ODocument3 pagesThe Contribution of Family Medicine To Community-OFarah FarahNo ratings yet
- Junal Inter 4Document10 pagesJunal Inter 4adi qiromNo ratings yet
- Lab ModuleDocument6 pagesLab ModulenicamarshmayNo ratings yet
- Community-Oriented Primary Care (COPC) in District Health Services of Gauteng, South AfricaDocument4 pagesCommunity-Oriented Primary Care (COPC) in District Health Services of Gauteng, South AfricaAileyIrvetteNo ratings yet
- Primary Health Care I 2021Document13 pagesPrimary Health Care I 2021Galakpai KolubahNo ratings yet
- Challenges & Achievements of NRHMDocument3 pagesChallenges & Achievements of NRHMRenu R NairNo ratings yet
- Community Health Nursing PrinciplesDocument9 pagesCommunity Health Nursing PrinciplesKimberly Marie BayangNo ratings yet
- Journal Reading 5Document6 pagesJournal Reading 5Ronaly Angalan TinduganNo ratings yet
- UNDP Issue Brief - Universal Health Coverage For Sustainable DevelopmentDocument16 pagesUNDP Issue Brief - Universal Health Coverage For Sustainable DevelopmentbabubvNo ratings yet
- Achieving Better Health for All Through Primary Health CareDocument6 pagesAchieving Better Health for All Through Primary Health CareRem Alfelor100% (1)
- Health Policy Review and Analysis (1) 1Document25 pagesHealth Policy Review and Analysis (1) 1Keebeek S ArbasNo ratings yet
- Primary Health CareDocument34 pagesPrimary Health CareOcquli VictorNo ratings yet
- Primary Health Care Approach and Alma Ata DeclarationDocument2 pagesPrimary Health Care Approach and Alma Ata DeclarationAmethystNo ratings yet
- Welcome To The Seminar On: Primary Health Care and Modes of PreventionDocument38 pagesWelcome To The Seminar On: Primary Health Care and Modes of PreventionTom ThomasNo ratings yet
- Recife Declaration 13nov PDFDocument4 pagesRecife Declaration 13nov PDFSá LealNo ratings yet
- Primary Health Notes Care 2019Document4 pagesPrimary Health Notes Care 2019Galakpai KolubahNo ratings yet
- Primary Health CareDocument14 pagesPrimary Health CareAprille SgrrNo ratings yet
- Implementation Strategy of Primary Health Care in Ovia CommunitiesDocument7 pagesImplementation Strategy of Primary Health Care in Ovia CommunitiesPuttryNo ratings yet
- Primary Health Care (PHC) Is An Essential Health Care Made UniversallyDocument9 pagesPrimary Health Care (PHC) Is An Essential Health Care Made UniversallyAlimyon Abilar MontoloNo ratings yet
- Care. Nurs Res. 1992 May-Jun 41 (3) :138-43. PMID: 1584655Document3 pagesCare. Nurs Res. 1992 May-Jun 41 (3) :138-43. PMID: 1584655Chelzie LasernaNo ratings yet
- PHC 1Document11 pagesPHC 1christine gisembaNo ratings yet
- Issue Brief 5 CHWsDocument2 pagesIssue Brief 5 CHWsNay Lin HtikeNo ratings yet
- Primary Health Care (PHC)Document35 pagesPrimary Health Care (PHC)Hope CarenaNo ratings yet
- Public Health: Electra KashyapDocument21 pagesPublic Health: Electra KashyapAyush HazarikaNo ratings yet
- NCM 104 Primary Healthcare ChuchuDocument6 pagesNCM 104 Primary Healthcare ChuchuSharina Marie CoderaNo ratings yet
- Midterm - CHN Lec NotesDocument24 pagesMidterm - CHN Lec NotesdeguzmanpaulalbertfNo ratings yet
- Pharmacist As Primary Health Care ProviderDocument8 pagesPharmacist As Primary Health Care ProviderRUTH AFUNWANo ratings yet
- Health Systems Strengthening: Brief)Document2 pagesHealth Systems Strengthening: Brief)MusaNo ratings yet
- Commision On Macroeconomic and Health Primary Health Care in India Review of Policy Plan and Committee ReportsDocument4 pagesCommision On Macroeconomic and Health Primary Health Care in India Review of Policy Plan and Committee Reportsasha_qr100% (3)
- Essentials of Primary Health CareDocument40 pagesEssentials of Primary Health CareSpislgal PhilipNo ratings yet
- CHN1 Lec Session 9 SASDocument10 pagesCHN1 Lec Session 9 SASFrances PaqueoNo ratings yet
- Activity 2 Global Health SituationDocument4 pagesActivity 2 Global Health SituationSarah Jane MaganteNo ratings yet
- Introducing Family MedicineDocument16 pagesIntroducing Family MedicineEndah SusantiNo ratings yet
- Community Health Nursing Review NotesDocument5 pagesCommunity Health Nursing Review NotesMaria Ana AguilarNo ratings yet
- Reviewer in CHNDocument6 pagesReviewer in CHNMerald PerdigonNo ratings yet
- Community Health Nursing UpdatesDocument6 pagesCommunity Health Nursing UpdatesLoyloy D ManNo ratings yet
- Module 5 Unit 5 Introduction To Primary Health Care 3Document25 pagesModule 5 Unit 5 Introduction To Primary Health Care 3Alyanna AlcantaraNo ratings yet
- 44-Article Text-775-1-10-20140406Document10 pages44-Article Text-775-1-10-20140406breastcancer.globaleventsNo ratings yet
- Intersectoral Coordination in India For Health Care AdvancementDocument26 pagesIntersectoral Coordination in India For Health Care Advancementshijoantony100% (1)
- Primary Health Care: A Comparison of Approaches and PrinciplesDocument4 pagesPrimary Health Care: A Comparison of Approaches and PrinciplesDenver SignabenNo ratings yet
- Inbound 5566500222241268010Document38 pagesInbound 5566500222241268010Hazel Jane MillamaNo ratings yet
- Chapter 7Document9 pagesChapter 7Lawrence Ryan DaugNo ratings yet
- Implementation Research For Malaria Prevention andDocument17 pagesImplementation Research For Malaria Prevention andLammeessaa Assefa AyyaanaNo ratings yet
- CHN Notes2Document12 pagesCHN Notes2PAOLA LUZ CRUZNo ratings yet
- How to Play the Cypher SystemDocument434 pagesHow to Play the Cypher SystemMNo ratings yet
- Arctic Terrain Shop RulesDocument28 pagesArctic Terrain Shop Rulescwag68No ratings yet
- Drive AI-Powered Innovation and Intelligent Action: Data Cloud SummitDocument24 pagesDrive AI-Powered Innovation and Intelligent Action: Data Cloud Summitcwag68No ratings yet
- SampleDocument13 pagesSamplecwag68No ratings yet
- TermpaperDocument22 pagesTermpapercwag68No ratings yet
- Google Cloud Database Strategy: Solving for the futureDocument30 pagesGoogle Cloud Database Strategy: Solving for the futurecwag68No ratings yet
- Solving for the future with Intelligent Data and Analytics FabricDocument18 pagesSolving for the future with Intelligent Data and Analytics Fabriccwag68No ratings yet
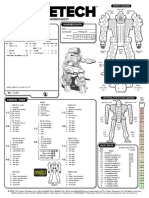
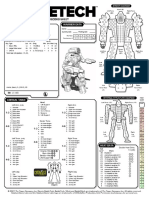
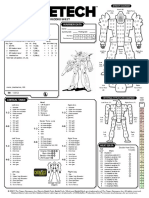
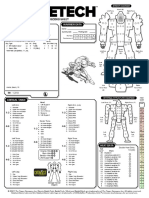
- Battlemech Record Sheet: 'Mech Data Warrior DataDocument1 pageBattlemech Record Sheet: 'Mech Data Warrior Datacwag68No ratings yet
- Magical World BuilderDocument69 pagesMagical World BuilderRyan D Hall83% (6)
- Omnimech Record Sheet: 'Mech Data Warrior DataDocument1 pageOmnimech Record Sheet: 'Mech Data Warrior Datacwag68No ratings yet
- Plot FormulasDocument2 pagesPlot FormulasIgor Airoides100% (12)
- Omnimech Record Sheet: 'Mech Data Warrior DataDocument1 pageOmnimech Record Sheet: 'Mech Data Warrior Datacwag68No ratings yet
- Data and Analytics Sharing at Equifax: Immediate, Interconnected, Scalable, and SecureDocument30 pagesData and Analytics Sharing at Equifax: Immediate, Interconnected, Scalable, and Securecwag68No ratings yet
- Choosing the Right Database on Google CloudDocument30 pagesChoosing the Right Database on Google Cloudcwag68No ratings yet
- MessageDocument3 pagesMessagecwag68No ratings yet
- Starfinder Auto Fill Sheet PDFDocument3 pagesStarfinder Auto Fill Sheet PDFnotgonna tellyouNo ratings yet
- Battlemech Record Sheet: 'Mech Data Warrior DataDocument1 pageBattlemech Record Sheet: 'Mech Data Warrior Datacwag68No ratings yet
- Draw As Many Level 1 Treasure Cards As The Number of HeroesDocument1 pageDraw As Many Level 1 Treasure Cards As The Number of Heroescwag68No ratings yet
- Run One B&E Extraction: Meet TagsDocument3 pagesRun One B&E Extraction: Meet Tagscwag68No ratings yet
- Main Exploration TableDocument2 pagesMain Exploration Tablecwag68No ratings yet
- ReadmeDocument1 pageReadmecwag68No ratings yet
- Sequence of Play BG WWIIDocument3 pagesSequence of Play BG WWIIcwag68No ratings yet
- Sharing Desktop Via Skype SoftwareDocument1 pageSharing Desktop Via Skype Softwarecwag68No ratings yet
- BtechDocument2 pagesBtechcwag68No ratings yet
- Omnimech Record Sheet: 'Mech Data Warrior DataDocument1 pageOmnimech Record Sheet: 'Mech Data Warrior Datacwag68No ratings yet
- HistoryDocument1 pageHistorycwag68No ratings yet
- Setup Sequence: Corellian CorvetteDocument2 pagesSetup Sequence: Corellian Corvettecwag68No ratings yet
- Omnimech Record Sheet: 'Mech Data Warrior DataDocument1 pageOmnimech Record Sheet: 'Mech Data Warrior Datacwag68No ratings yet
- Battlemech Record Sheet: 'Mech Data Warrior DataDocument1 pageBattlemech Record Sheet: 'Mech Data Warrior Datacwag68No ratings yet
- Battlemech Record Sheet: 'Mech Data Warrior DataDocument1 pageBattlemech Record Sheet: 'Mech Data Warrior Datacwag68No ratings yet
- Case - Liberia Case Study, Leadership and Policy DevelopmentDocument10 pagesCase - Liberia Case Study, Leadership and Policy Developmentwhoosh2008No ratings yet
- Namulaba TRAINING OF CH WORKERSDocument6 pagesNamulaba TRAINING OF CH WORKERSSamuel KalibalaNo ratings yet
- Report 2: Essential Package of Health Services Somalia 2009Document104 pagesReport 2: Essential Package of Health Services Somalia 2009Anisa AbdullahiNo ratings yet
- GNN Dec 2011 - Case Study - MongoliaDocument3 pagesGNN Dec 2011 - Case Study - MongoliaADBGADNo ratings yet
- Lions Aid Norway Zambia - 2011 Annual ReportDocument16 pagesLions Aid Norway Zambia - 2011 Annual ReportlanzambiaNo ratings yet
- CHW Core Competencies Manual Participants Guide 2013Document106 pagesCHW Core Competencies Manual Participants Guide 2013Parsaant SinghNo ratings yet
- Moyo Wa Bana: A Novel Approach To Reducing Child Mortality in ZambiaDocument40 pagesMoyo Wa Bana: A Novel Approach To Reducing Child Mortality in ZambiaCAREZAMBIANo ratings yet
- Accessible healthcare for allDocument53 pagesAccessible healthcare for allecossich123No ratings yet
- Vacancies - PACT 2021Document2 pagesVacancies - PACT 2021mgvs eduNo ratings yet
- Community Health WorkersDocument42 pagesCommunity Health WorkersSathya PalanisamyNo ratings yet
- Task Shifting Mental Health in South Africa 2-Lmbnuh001Document11 pagesTask Shifting Mental Health in South Africa 2-Lmbnuh001Nuha LimbadaNo ratings yet
- Community Health Nurse RolesDocument4 pagesCommunity Health Nurse Rolescoy008No ratings yet
- BMJ k4884Document8 pagesBMJ k4884Asela SubhasingheNo ratings yet
- Ashraf Et Al 2020 (AER)Document40 pagesAshraf Et Al 2020 (AER)Jose CamposNo ratings yet
- Capstone Proposal Tanauan GroupDocument9 pagesCapstone Proposal Tanauan GroupburdeosmaelnoraNo ratings yet
- COPARDocument57 pagesCOPARBernardita Timbreza Hernandez100% (4)
- Addressing Stunting in Geita RegionDocument6 pagesAddressing Stunting in Geita RegionPaschal Kunambi100% (1)
- II Pioneers of Community Health Worker ProgrammesDocument7 pagesII Pioneers of Community Health Worker Programmesvr_ramanNo ratings yet
- Pivot FY21 Impact ReportDocument23 pagesPivot FY21 Impact ReportPivotNo ratings yet
- Merlin Community Based Health ProgrammingDocument93 pagesMerlin Community Based Health ProgrammingDoris OoNo ratings yet
- Annual Report 2010-2011Document60 pagesAnnual Report 2010-2011Feinstein International CenterNo ratings yet
- Community Health WorkersDocument20 pagesCommunity Health WorkersrevronrobinsonNo ratings yet
- BHW Trainings On TESDADocument8 pagesBHW Trainings On TESDAKap JPNo ratings yet
- Ballard and Perry Et Al 2023Document11 pagesBallard and Perry Et Al 2023Ramiro LlanqueNo ratings yet
- CHW Roles and TasksDocument30 pagesCHW Roles and TasksdanielNo ratings yet
- 10-Emergency Health ServicesDocument38 pages10-Emergency Health ServicesXimena Ibañez RodriguezNo ratings yet
- Ochieng - Factors Influencing Community Participation in Healthcare Programs SiayaDocument93 pagesOchieng - Factors Influencing Community Participation in Healthcare Programs SiayaALU MOTUNROLA FOLASADENo ratings yet
- Costs and Cost Effectiveness of Community Health WorkersDocument16 pagesCosts and Cost Effectiveness of Community Health WorkersMike TeeNo ratings yet
- 09 CHW SupervisionDocument26 pages09 CHW SupervisionPabhat Kumar100% (1)
- The Ghana Essential Health Interventions Program: A Plausibility Trial of The Impact of Health Systems Strengthening On Maternal & Child SurvivalDocument12 pagesThe Ghana Essential Health Interventions Program: A Plausibility Trial of The Impact of Health Systems Strengthening On Maternal & Child SurvivalTizoon FaeyzaNo ratings yet
- High-Risers: Cabrini-Green and the Fate of American Public HousingFrom EverandHigh-Risers: Cabrini-Green and the Fate of American Public HousingNo ratings yet
- Not a Crime to Be Poor: The Criminalization of Poverty in AmericaFrom EverandNot a Crime to Be Poor: The Criminalization of Poverty in AmericaRating: 4.5 out of 5 stars4.5/5 (37)
- Workin' Our Way Home: The Incredible True Story of a Homeless Ex-Con and a Grieving Millionaire Thrown Together to Save Each OtherFrom EverandWorkin' Our Way Home: The Incredible True Story of a Homeless Ex-Con and a Grieving Millionaire Thrown Together to Save Each OtherNo ratings yet
- When Helping Hurts: How to Alleviate Poverty Without Hurting the Poor . . . and YourselfFrom EverandWhen Helping Hurts: How to Alleviate Poverty Without Hurting the Poor . . . and YourselfRating: 5 out of 5 stars5/5 (36)
- Poor Economics: A Radical Rethinking of the Way to Fight Global PovertyFrom EverandPoor Economics: A Radical Rethinking of the Way to Fight Global PovertyRating: 4.5 out of 5 stars4.5/5 (263)
- Fucked at Birth: Recalibrating the American Dream for the 2020sFrom EverandFucked at Birth: Recalibrating the American Dream for the 2020sRating: 4 out of 5 stars4/5 (173)
- Charity Detox: What Charity Would Look Like If We Cared About ResultsFrom EverandCharity Detox: What Charity Would Look Like If We Cared About ResultsRating: 4 out of 5 stars4/5 (9)
- Same Kind of Different As Me Movie Edition: A Modern-Day Slave, an International Art Dealer, and the Unlikely Woman Who Bound Them TogetherFrom EverandSame Kind of Different As Me Movie Edition: A Modern-Day Slave, an International Art Dealer, and the Unlikely Woman Who Bound Them TogetherRating: 4 out of 5 stars4/5 (685)
- The Great Displacement: Climate Change and the Next American MigrationFrom EverandThe Great Displacement: Climate Change and the Next American MigrationRating: 4.5 out of 5 stars4.5/5 (32)
- Hillbilly Elegy: A Memoir of a Family and Culture in CrisisFrom EverandHillbilly Elegy: A Memoir of a Family and Culture in CrisisRating: 4 out of 5 stars4/5 (4277)
- The Great Displacement: Climate Change and the Next American MigrationFrom EverandThe Great Displacement: Climate Change and the Next American MigrationRating: 4 out of 5 stars4/5 (19)
- Heartland: A Memoir of Working Hard and Being Broke in the Richest Country on EarthFrom EverandHeartland: A Memoir of Working Hard and Being Broke in the Richest Country on EarthRating: 4 out of 5 stars4/5 (188)
- Nickel and Dimed: On (Not) Getting By in AmericaFrom EverandNickel and Dimed: On (Not) Getting By in AmericaRating: 4 out of 5 stars4/5 (186)
- The Meth Lunches: Food and Longing in an American CityFrom EverandThe Meth Lunches: Food and Longing in an American CityRating: 5 out of 5 stars5/5 (5)
- Superclass: The Global Power Elite and the World They Are MakingFrom EverandSuperclass: The Global Power Elite and the World They Are MakingRating: 3.5 out of 5 stars3.5/5 (32)
- Nickel and Dimed: On (Not) Getting By in AmericaFrom EverandNickel and Dimed: On (Not) Getting By in AmericaRating: 3.5 out of 5 stars3.5/5 (197)
- When Helping Hurts: How to Alleviate Poverty Without Hurting the Poor . . . and YourselfFrom EverandWhen Helping Hurts: How to Alleviate Poverty Without Hurting the Poor . . . and YourselfRating: 4 out of 5 stars4/5 (126)
- Alienated America: Why Some Places Thrive While Others CollapseFrom EverandAlienated America: Why Some Places Thrive While Others CollapseRating: 4 out of 5 stars4/5 (35)
- Sons, Daughters, and Sidewalk Psychotics: Mental Illness and Homelessness in Los AngelesFrom EverandSons, Daughters, and Sidewalk Psychotics: Mental Illness and Homelessness in Los AngelesNo ratings yet
- Heartland: A Memoir of Working Hard and Being Broke in the Richest Country on EarthFrom EverandHeartland: A Memoir of Working Hard and Being Broke in the Richest Country on EarthRating: 4 out of 5 stars4/5 (269)
- The Injustice of Place: Uncovering the Legacy of Poverty in AmericaFrom EverandThe Injustice of Place: Uncovering the Legacy of Poverty in AmericaRating: 4.5 out of 5 stars4.5/5 (2)
- Dark Days, Bright Nights: Surviving the Las Vegas Storm DrainsFrom EverandDark Days, Bright Nights: Surviving the Las Vegas Storm DrainsNo ratings yet
- Out of the Red: My Life of Gangs, Prison, and RedemptionFrom EverandOut of the Red: My Life of Gangs, Prison, and RedemptionNo ratings yet