Professional Documents
Culture Documents
Gestational Diabetes Mellitus
Uploaded by
Jobelle Acena0 ratings0% found this document useful (0 votes)
49 views6 pagesThis document discusses gestational diabetes mellitus (GDM), a common type of diabetes that develops during pregnancy. GDM occurs when pregnancy hormones help the body resist insulin, sometimes leading to high blood sugar. Left untreated, GDM can cause complications for both mother and baby, such as large baby size. The document outlines the causes, risk factors, signs and symptoms, diagnostic tests and potential effects of GDM on both mother and fetus. Key points include that GDM develops due to increased pancreatic stimulation during pregnancy, putting both mother and baby at risk for health issues if not properly managed and treated.
Original Description:
Original Title
GESTATIONAL DIABETES MELLITUS
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses gestational diabetes mellitus (GDM), a common type of diabetes that develops during pregnancy. GDM occurs when pregnancy hormones help the body resist insulin, sometimes leading to high blood sugar. Left untreated, GDM can cause complications for both mother and baby, such as large baby size. The document outlines the causes, risk factors, signs and symptoms, diagnostic tests and potential effects of GDM on both mother and fetus. Key points include that GDM develops due to increased pancreatic stimulation during pregnancy, putting both mother and baby at risk for health issues if not properly managed and treated.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
49 views6 pagesGestational Diabetes Mellitus
Uploaded by
Jobelle AcenaThis document discusses gestational diabetes mellitus (GDM), a common type of diabetes that develops during pregnancy. GDM occurs when pregnancy hormones help the body resist insulin, sometimes leading to high blood sugar. Left untreated, GDM can cause complications for both mother and baby, such as large baby size. The document outlines the causes, risk factors, signs and symptoms, diagnostic tests and potential effects of GDM on both mother and fetus. Key points include that GDM develops due to increased pancreatic stimulation during pregnancy, putting both mother and baby at risk for health issues if not properly managed and treated.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 6
GESTATIONAL DIABETES MELLITUS this, this mechanism causes the rise of
placental lactogen, estrogen, and
Gestational Diabetes Mellitus (GDM) is progesterone to cause the following effects:
one of the most common types of diabetes
mellitus and considered the most 1. Antagonizes the effects of insulin
complication of pregnancy. This health 2. Prolong the elevation of stress hormones
problem is like pregnancy-induced (cortisol, epinephrine, and glucagon)
hypertension (PIH) that develops during 3. Degradation of insulin by the placenta
pregnancy and disappears after delivery of
fetus, or as maternal body returns to its pre- The total effect of these mechanisms raises
pregnant state. the maternal glucose level for fetal usage.
Hyperglycemia normally occurs with the
Gestational Diabetes Mellitus may or may protective mechanism that predisposes a
not with co-existing maternal diabetes. It pregnant mother in the triggering of her pre-
heightens the level of diabetes (if with diabetic state, or heightens an existing
previous diabetes) by a notch in response to diabetes mellitus.
the rise in fetal carbohydrate demand. 40%
of pregnant mothers who develops GDM will The effects of pregnancy on diabetes mellitus
eventually develop non-insulin dependent are summarized as:
diabetes mellitus (NIDDM or Type II DM) 1. First Trimester – glucose level is
within 5 years. relatively stable or may decrease
TYPES OF GDM 2. Second Trimester – there is rapid
increase in glucose level
Gestational Diabetes Mellitus (GDM) 3. Third Trimester – there is rapid
Type A1: abnormal oral glucose decrease glucose level and return to its
tolerance test (OGTT) but normal blood pre-pregnant state
glucose levels during fasting and 1-2
FACTS ABOUT INSULIN
hours after meals; diet modification is
sufficient to control glucose levels 1. The insulin is a normal body hormone
Type A2: abnormal OGTT compounded that is produced by the beta cells of the
by abnormal glucose levels during fasting Islets of Langerhans in the pancreas.
and/or after meals; additional therapy 2. The release of insulin is regulated by a
with insulin or other medications is negative feedback in response to high
required glucose level. The high glucose level may
come from excessive glucagon action or
ANATOMY AND PHYSIOLOGY
through high carbohydrate intake.
A normal body uses insulin as a channel for 3. The insulin secretion of the pancreas and
glucose to enter the cells for utilization. This its action on the liver makes it maintain a
process is also applicable with the fetus normal value of 80-120 mg/dL.
(during pregnancy) for growth and 4. Insulin is essential in the following
development. As the fetus grows, the actions:
maternal body executes autonomic response a. Carbohydrates – utilization of glucose
by doubling the level of glucose level by the cells
through lowering insulin secretion and with b. Proteins – conversion of amino acids to
the aid of some gestational hormones that replace muscle tissues
antagonizes the effects of insulin a process
known as protective mechanism. Along with
c. Fats – conversion of excess glucose to Higher glucose level (20-30 mg/dL) than the
fatty acids and store them to adipose pre-pregnant level
tissues Very rapid weight gain
d. Endothelial and nerve cells are the only Polyhydramnios
cells/tissues that can use glucose even Recurrent monilial infections
without insulin. Glycosuria
e. Low insulin level causes the rise in Nocturia
plasma glucose concentration and Large for gestational age (LGA) or small for
glycosuria. gestational age (SGA) fetus
f. Diabetes mellitus develops as the body More severe state of edema
secretes low amount or as body cells
rejects its utilization. DM:
Etiology Blurred vision
Vulvar pruritus
Gestational diabetes is a disorder of Paresthasia
late pregnancy (typically), caused by the
Peripheral neuropathy
increased pancreatic stimulation associated
with pregnancy. Weakness
Normal/elevated pulse rate and temperature
Normal/decreased blood pressure
RISK FACTORS Kussmaul’s respiration
1. Obesity Dehydration
2. Family history of DM Recurrent infections
3. Age of >45 years old (when got Non-healing wounds
pregnant)
ASSESSMENT FINDINGS
4. Previous delivery of baby weighing 9 lbs
or more 1. Associated findings include a poor
5. History of any autoimmune disease obstetric history, including spontaneous
6. Belonging to/with ethnic background from abortions, unexplained stillbirth,
unexplained hydramnios, premature
African American, Latino, and native
birth, low birth weight or birth weight
Americans
exceeding 4,000 g (8lb, 13 oz), and birth
7. History of previous GDM of a newborn with congenital anomalies.
8. With any level of hypertension 2. Common clinical
9. With elevated high-density lipoprotein manifestations include:
Glycosuria on two successive
CLINICAL MANIFESTATIONS office visits
Recurrent monilial vaginitis
The clinical manifestations of GDM coincide Macrosomia of the fetus on
with the signs and symptoms of other types ultrasound
of diabetes mellitus. These are popularly Polyhydramnios
known as the “3Ps” or polydipsia, polyuria, 3. Laboratory and diagnostic study
and polyphagia. Aside from these findings.
Fasting blood sugar test will
manifestations, there are also other sign and
reveal elevated blood glucose levels.
symptoms that are general manifestations A 50-g glucose screen (blood
and pregnancy-specific manifestations. glucose level is measured 1 hour
after client ingests a 50-g glucose
GDM: drink) reveals elevated blood
glucose levels. The normal plasma gestation. This is called the
threshold is 135 to 140 mg/dL. diabetogenic effect of pregnancy.
A 3- hour oral glucose tolerance 2. The pancreatic beta cell functions are
test (performed if 50-g glucose
impaired in response to the increased
screen results are abnormal) reveals
elevated blood glucose levels. (Table pancreatic stimulation and induced
1) insulin resistance.
The glycosylated hemoglobin 3. Pregnancy complicated by diabetes
(HbA 1c) test (measures glycemic puts the mother at increased risk for
control in the 4 to 8 weeks before the development of complications,
the test is performed; performed on such as spontaneous abortion,
women with pre-existing diabetes)
hypertensive disorders, and preterm
results reflect enzymatic bonding of
glucose to hemoglobin A amino labor, infection, and birth
acids. This is a useful indicator of complications.
overall blood glucose control. The 4. The effects of diabetes on the fetus
upper normal level of HbA1c is 6% include hypoglycemia, hyperglycemia,
of total hemoglobin. and ketoacidosis. Hyperglycemic
Screens for fetal (and later, effects can include:
neonatal) complications, including:
Congenital defects
Maternal serum alpha-fetoprotein Macrosomia
level to assess risk for neural tube Intrauterine growth restriction
defects in newborn. Intrauterine fetal death
Ultrasonography to detect fetal Delayed lung maturity
structural anomalies, macrosomia, Neonatal hypoglycemia
and hydramnios.
Neonatal hyperbilirubinemia
Nonstress test (as early as 30
weeks), contraction stress test,
COMPLICATIONS
and biophysical profile because of
risk of unexplained intrauterine The chronic effects or the uncontrolled
fetal demise in the antepartum
glucose level during pregnancy would lead to
period.
Lung maturity studies (by the development of the following
amniocentesis) to determine complications:
lecithinsphingomyelin (L/S) ratio
and to detect phosphatidylglycerol Preterm labor and delivery
(PG); the adequacy of L/S and PG, Urinary tract infection (UTI)
predictor of the newborn’s ability Infertility
to avoid respiratory distress Stillbirth
PIH – pre-eclampsia – eclampsia
Congenital anomalies
PATHOPHYSIOLOGY
Spontaneous abortion
1. In gestational diabetes mellitus (type
III, GDM), insulin antagonism by Also, a woman who developed or
placental hormones, human placental experienced GDM is expected to have type 2
lactogen, progesterone, cortisol, and diabetes mellitus within 5 years for the rest
prolactin leads to increased blood of her life.
glucose levels. The effect of these DIAGNOSIS
hormones peaks at about 26 weeks of
Blood glucose monitoring—this can baby. Good glucose control throughout
either be done through fasting blood pregnancy will reduce the risk of fetal
sugar (FBS) or randomly. This reveals macrosomia, trauma during birth, induction
the glucose level and indicates the of labour and/or caesarean section, neonatal
plan of care needed. hypoglycaemia and perinatal death (14).
Glucose tolerance test (GTT)—to
Alongside strict monitoring of blood glucose
evaluate the response of insulin to
with input from an endocrinologist, women
loading glucose.
will also be offered an increased antenatal
Glycated haemoglobin
care package including more frequent
(Glycohemoglobin)—measures
ultrasound scans to assess the size and well-
glycemic control by evaluating the
being of the baby and liquor volume.
attachment of glucose to freely
permeable erythrocytes during their Blood glucose monitoring kits should be
whole life cycle. given to women and self-monitoring should
C-peptide Assay (connecting peptide be taught with repeat prescriptions for
assay)—useful when the presence of necessary equipment and medications e.g.
insulin antibodies interferes with direct needles, sharps bins.
insulin assay.
Fructosamine assay—is much more Treatment
useful than glycosylated hemoglobin
The main form of treatment is blood glucose
tests in cases of hemoglobin variants.
control and the initial treatment offered is
Urine glucose and ketone monitoring—
dependent on the results of the OGTT (see
may be performed in cases where
Table 2).
blood glucose monitoring is not
available, but, is not as accurate as Lifestyle changes
the former.
Amniocentesis Simple lifestyle changes are enough in many
Non-stress test women to control their glucose level and all
Sonography women should be referred to a dietician to
review their diet and provide information on
NURSING DIAGNOSES low glycaemic index foods. In addition to
this, exercise has been shown to stabilise
1. Altered nutrition: more or less than
post prandial blood glucose and reduce the
body requirements related to weight
need for insulin.
gain
2. High risk pregnancy: high risk for Metformin
infection, ketosis, fetal demise,
cephalopelvic disproportion, Metformin is a well-established drug that
polyhydramnios, congenital reduces the amount of glucose created in the
anomalies, preterm labor. liver and makes the body more sensitive to
3. Knowledge deficit related to disease insulin. In detail, metformin is a biguanide
and insulin use and interaction. oral antidiabetic medication and it works by
suppressing hepatic gluconeogenesis,
MANAGEMENT increasing insulin sensitivity and decreasing
the absorption of glucose from the
Information is crucial to help women
gastrointestinal tract. This glucose-lowering
understand the importance of good glucose
therapy should be offered first to women
control for her health and the health of her
who have uncontrolled hyperglycaemia glibenclamide and insulin should maintain a
unless contraindicated. blood glucose above 4mmol/l in order to
prevent problematic hypoglycaemias.
When metformin was compared to insulin it
was found to have no significant differences NURSING MANAGEMENTS
between outcomes such as shoulder dystocia
and infants born large for gestational age. Assessment
Additionally the administration is considered History taking on:
much easier and preferred compared to
insulin. a. First presentation of the
manifestations of diabetes (3 P’s)
Glibenclamide b. First diagnosis of DM
Glibenclamide is also a well-established c. Family members with DM
medicine that drives the pancreas to produce Review of systems:
more insulin. In more detail, glibenclamide is
a sulphonylurea and acts by stimulating 1. Weight gain, increasing
insulin release from the beta-cells in the fatigue/weakness/tiredness
pancreas. There are no significant 2. Skin lesions, infections, hydration,
differences between the use of insulin and signs of poor wound healing
metformin compared to glibenclamide for the 3. Changes in vision – floaters, halos,
prevention of shoulder dystocia or large for blurred vision, dry/burning eyes,
gestational age, however there is no long- cataract, glaucoma
term data for the effects of glibenclamide in 4. Gingivitis, periodontal disease
pregnancy and therefore metformin and 5. Orthostatic hypotension, cold
insulin are used preferentially. extremities, weal pedal pulses
6. Diarrhea, constipation, early satiety,
Insulin bloating, flatulence, hunger and thirst
When oral medications don't control 7. Frequent urination, nocturia, vaginal
gestational diabetes, insulin is needed. discharge
Exogenous insulin is used in conjunction with 8. Numbness and tingling of the
diet, exercise and metformin if required for extremities, decrease pain and
glucose control. Insulins that are used temperature sensation
preferentially are isophane/detemir insulin INTERVENTIONS
and lispro/aspart insulin as long-acting and
short-acting insulin respectively. It is 1. Nutrition
important to warn women of the effects and Assess timing and content of
prevention of hypoglycaemic events. Users meals
must also be made aware of DVLA guidelines Instruct on importance of a
with insulin use. well-balanced diet
Explain the importance of
Blood glucose aims exercise
Women should record their blood sugar Plan for a weight reduction
monitoring daily. If they have repeatedly course
high blood glucose they should seek medical 2. Insulin use
advice in order to change or increase their Encourage verbalization of
current management. Those on feelings
Demonstrate and explain insulin Monitor daily weight and advice
therapy to report on rapid weight gain
Allow client to do self- 7. Educative
administration Teach on lifestyle modifications
Review mastery of the whole Advice to see psychologists
process with other family members for
3. Injury from hypoglycemia therapies on the possibilities of
Monitor maternal blood glucose fetal abnormalities
level Advice to call emergency
Instruct on insulin-activity-diet response team in case of
interaction emergency
Teach on the signs and Advise to religiously follow the
symptoms of hypoglycemia health instructions
Teach/present the list of
EVALUATION
things/foods that need to be
available at all times (in case of 1. Body weight is within the normal
hypoglycemic attacks) range for the age of gestation.
Have identification band 2. Demonstrates proper technique in
indicating the health condition self-administration of insulin
(DM) for fainting instances 3. No episodes of hypoglycemia as
4. Activity tolerance claimed by the client
Plan for regular exercise 4. No skin problems/lesions.
Increase carbohydrate intake 5. Verbalized readiness on the possible
before exercise fetal defects.
Instruct to avoid exercise of 6. Stable feta heart rate.
blood glucose level exceeds 250
mg/dL and urine ketones are References:
present
Gestational Diabetes Mellitus:
Advise to use abdomen for
insulin injection if arms and legs https://www.google.com/amp/s/www.rnspea
are used for exercise k.com/gestational-diabetes-mellitus-case-
5. Skin integrity study/amp/
Avoid alcohol use, instead,
lotion https://www.nursinginpractice.com/gestation
Teach on proper foot care al-diabetes-primary-care
Advise to stop smoking and
https://www.rnpedia.com/nursing-
alcohol use
notes/maternal-and-child-nursing-
6. Fetal well-being
notes/gestational-diabetes/
Continuous monitoring of fetal
activities and fetal heart tone
Monitor fetal activities during
maternal activities
Monitor early signs of labor
Advise to report of any
discharge coming from the
vagina
You might also like
- Gestational Diabetes Mellitus Gestational Diabetes Mellitus (GDM) Is One of TheDocument10 pagesGestational Diabetes Mellitus Gestational Diabetes Mellitus (GDM) Is One of TheJobelle AcenaNo ratings yet
- Gestational Diabetes Mellitus PDFDocument7 pagesGestational Diabetes Mellitus PDFMaxenia FaboresNo ratings yet
- Gestational Diabetes Nursing Care PlanDocument28 pagesGestational Diabetes Nursing Care PlanIan MenesesNo ratings yet
- Gestational Diabetes Mellitus Case Study GuideDocument8 pagesGestational Diabetes Mellitus Case Study GuideRHUBY ABENOJANo ratings yet
- Activity Part 1Document7 pagesActivity Part 1xiumethemoneyNo ratings yet
- GDMDocument13 pagesGDMSharmistha DebnathNo ratings yet
- Gestational Diabetes Risks & ManagementDocument2 pagesGestational Diabetes Risks & ManagementAmethystNo ratings yet
- DM in PregnancyDocument35 pagesDM in Pregnancyapule geraldhumbleNo ratings yet
- Pa Tho Physiology of Gestational Diabetes MellitusDocument3 pagesPa Tho Physiology of Gestational Diabetes Mellitus-Aldear Franze MillaNo ratings yet
- Gestational Diabetes MellitusDocument7 pagesGestational Diabetes MellitusYujen0% (1)
- MEDICAL COMPLICATIONS OF PREGNANCY ModuleDocument12 pagesMEDICAL COMPLICATIONS OF PREGNANCY ModuleWynjoy NebresNo ratings yet
- Lesson#7 - Diabetes MellitusDocument22 pagesLesson#7 - Diabetes MellitusKyle Ethan De la RiarteNo ratings yet
- DiabetesDocument41 pagesDiabetesWai Kwong ChiuNo ratings yet
- GDMDocument38 pagesGDMAbhishiktaAbhi100% (1)
- Gestational DiabetesDocument35 pagesGestational DiabetesAnnakay HudsonNo ratings yet
- Seminar 5 - DM in PregnancyDocument19 pagesSeminar 5 - DM in PregnancyHakimah K. SuhaimiNo ratings yet
- Gestational Diabetes 97-03Document9 pagesGestational Diabetes 97-03jaenaroseNo ratings yet
- Gestational DiabetesDocument24 pagesGestational Diabeteshhpr9709No ratings yet
- Current Classification Clinical Characteristics and ClinicalimplicationsDocument7 pagesCurrent Classification Clinical Characteristics and ClinicalimplicationsbeayapNo ratings yet
- GDM CSDocument13 pagesGDM CSADRIATICO JAROSLUVNo ratings yet
- Week 5 Disease Affecting PregnancyDocument143 pagesWeek 5 Disease Affecting Pregnancymico zarsadiazNo ratings yet
- Gestational Diabetes MellitusDocument73 pagesGestational Diabetes Mellitusreniere lagazoNo ratings yet
- Gestational Diabetes Mellitus Third Trimester-There Is Rapid Decrease inDocument5 pagesGestational Diabetes Mellitus Third Trimester-There Is Rapid Decrease inOona Nicole DioricoNo ratings yet
- Pre-Gestational Cardiovascular Conditions in PregnancyDocument29 pagesPre-Gestational Cardiovascular Conditions in PregnancyVyklyn TestaNo ratings yet
- Gestational Diabetes Mellitus (GDM) .TriceDocument47 pagesGestational Diabetes Mellitus (GDM) .TricejerrydanfordfxNo ratings yet
- Diabetes Mellitus & Pregnancy by D.a.mehtaDocument31 pagesDiabetes Mellitus & Pregnancy by D.a.mehtadr.d.a.mehta11No ratings yet
- GDMDocument66 pagesGDMpooja singhNo ratings yet
- 1 DMDocument49 pages1 DMDrMohammad KhadrawyNo ratings yet
- Pregnancy Diseases GuideDocument10 pagesPregnancy Diseases GuideRasco, Allen jayNo ratings yet
- Gestational DiabetesDocument14 pagesGestational Diabetesamena mahmoudNo ratings yet
- Gestational Diabetes: Dr. Oyeyiola Oyebode Registrar Obstetrics and Gynaecology Ola Catholic Hospital, Oluyoro IbadanDocument40 pagesGestational Diabetes: Dr. Oyeyiola Oyebode Registrar Obstetrics and Gynaecology Ola Catholic Hospital, Oluyoro Ibadanoyebode oyeyiolaNo ratings yet
- DM in PregnancyDocument11 pagesDM in Pregnancyميمونه عبد الرحيم مصطفىNo ratings yet
- Diabetes in PrgenancyDocument36 pagesDiabetes in Prgenancynita meliasariNo ratings yet
- Diabetes in PregnancyDocument62 pagesDiabetes in Pregnancykapil khanalNo ratings yet
- Diabetes in Pregnancy: A Guide to ManagementDocument11 pagesDiabetes in Pregnancy: A Guide to ManagementAlana CaballeroNo ratings yet
- Septiya Agestin Cahyaningrum - Complications of Pregnancy, Childbirth and The Postpartum Period, As Well As Maternal Death - WordDocument14 pagesSeptiya Agestin Cahyaningrum - Complications of Pregnancy, Childbirth and The Postpartum Period, As Well As Maternal Death - WordSepty KawaiNo ratings yet
- Gestational Diabetes Mellitus: Case PresentationDocument46 pagesGestational Diabetes Mellitus: Case PresentationATEHAN BORDSNo ratings yet
- Gestational DiabetesDocument52 pagesGestational Diabetestammycristobalmd100% (8)
- Recent Advances in Management of Gestational Diabetes and Pre-EclampsiaDocument36 pagesRecent Advances in Management of Gestational Diabetes and Pre-EclampsiaSyed Zahed AliNo ratings yet
- Gestational DiabetesDocument34 pagesGestational DiabetesAHm'd Metwally100% (1)
- DM in PregDocument32 pagesDM in Pregbryanpei23No ratings yet
- Diabetes Mellitus in PregnancyDocument55 pagesDiabetes Mellitus in Pregnancyapi-3856051100% (2)
- Gestational Diabetes Mellitus (GDM) : Current Concept and A Short ReviewDocument1 pageGestational Diabetes Mellitus (GDM) : Current Concept and A Short ReviewTimothy Ho IINo ratings yet
- dminpregnancy-201109140122 (1)Document76 pagesdminpregnancy-201109140122 (1)EndaleNo ratings yet
- B17M2L8 - Gestational Diabetes MellitusDocument7 pagesB17M2L8 - Gestational Diabetes MellitusLorenzo Dominick CidNo ratings yet
- Pregestational ConditionDocument7 pagesPregestational ConditionCamille UlepNo ratings yet
- Diabetes Mellitus: Medical Complications in PregnancyDocument19 pagesDiabetes Mellitus: Medical Complications in PregnancySenopati KhanjieNo ratings yet
- Diabetes in Pregnancy: Supervisor: DR Rathimalar By: DR Ashwini Arumugam & DR Laily MokhtarDocument21 pagesDiabetes in Pregnancy: Supervisor: DR Rathimalar By: DR Ashwini Arumugam & DR Laily MokhtarHarleyquinn96 DrNo ratings yet
- Gestational Diabetes MellitusDocument16 pagesGestational Diabetes Mellitusarjunr19910% (1)
- Manju Project NWDocument15 pagesManju Project NWBiju Jacob JohnNo ratings yet
- Diabetes in PregnancyDocument5 pagesDiabetes in Pregnancybluecrush1No ratings yet
- Pre Gestational ConditionsDocument17 pagesPre Gestational Conditionslarissedeleon100% (2)
- Gestational diabetes mellitus nursing careDocument29 pagesGestational diabetes mellitus nursing careWed LodNo ratings yet
- OB CH20 NotesDocument16 pagesOB CH20 NotesVeronica EscalanteNo ratings yet
- #2-NCM 109 - TransesDocument19 pages#2-NCM 109 - TransesJaimie BanaagNo ratings yet
- Complicated Midwifery - 1Document28 pagesComplicated Midwifery - 1nafisatmuhammed452No ratings yet
- Li Ruzhi Ob&Gy Hospital, Fudan UniversityDocument40 pagesLi Ruzhi Ob&Gy Hospital, Fudan UniversityJenny A. BignayanNo ratings yet
- Diabetes in Pregnancy: Umar Zein FK Unpri MedanDocument22 pagesDiabetes in Pregnancy: Umar Zein FK Unpri Medanyukmin rotamaNo ratings yet
- Smoothies for Diabetics: Reverse Diabetes and Lower Blood Sugar with 36 Quick & Easy Delicious Diabetic Smoothie RecipesFrom EverandSmoothies for Diabetics: Reverse Diabetes and Lower Blood Sugar with 36 Quick & Easy Delicious Diabetic Smoothie RecipesRating: 5 out of 5 stars5/5 (2)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- NCM 107 Leadership and Management RLEDocument4 pagesNCM 107 Leadership and Management RLEJobelle AcenaNo ratings yet
- Geriatric Case StudyDocument15 pagesGeriatric Case StudyJobelle AcenaNo ratings yet
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale Evaluation Short Term Goal Independent: Short Term GoalDocument5 pagesAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale Evaluation Short Term Goal Independent: Short Term GoalJobelle AcenaNo ratings yet
- Pediatric Case StudyDocument21 pagesPediatric Case StudyJobelle AcenaNo ratings yet
- Date/Schedule Activities Expected Output Verified/Checked by Area in ChargeDocument2 pagesDate/Schedule Activities Expected Output Verified/Checked by Area in ChargeJobelle AcenaNo ratings yet
- Case StudyDocument10 pagesCase StudyJobelle AcenaNo ratings yet
- Case Study (ACS)Document12 pagesCase Study (ACS)Kristel Joy Cabarrubias Acena100% (1)
- Union Christian College School of Health and Sciences City of San Fernando La UnionDocument11 pagesUnion Christian College School of Health and Sciences City of San Fernando La UnionJobelle AcenaNo ratings yet
- NCM 107 SY 2020-2021: Legal and Ethical Consideration of Euthanasia in India: A Choice Between Life and DeathDocument8 pagesNCM 107 SY 2020-2021: Legal and Ethical Consideration of Euthanasia in India: A Choice Between Life and DeathJobelle AcenaNo ratings yet
- GC ncp1Document2 pagesGC ncp1Jobelle AcenaNo ratings yet
- DRUG STUDY (Lung Cancer)Document10 pagesDRUG STUDY (Lung Cancer)Jobelle AcenaNo ratings yet
- GC ncp1 and 2Document4 pagesGC ncp1 and 2Jobelle AcenaNo ratings yet
- Difference Between Mechanism of Action of Cell Mediated Immune System and Humoral Mediated Immune SystemDocument4 pagesDifference Between Mechanism of Action of Cell Mediated Immune System and Humoral Mediated Immune SystemJobelle AcenaNo ratings yet
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationDocument10 pagesAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationJobelle Acena100% (2)
- Subjective: Ventilation AssistanceDocument3 pagesSubjective: Ventilation AssistanceJobelle Acena100% (2)
- Normal Cell GrowthDocument5 pagesNormal Cell GrowthJobelle AcenaNo ratings yet
- PHARMAfdDocument7 pagesPHARMAfdJobelle AcenaNo ratings yet
- Case Study (Lung Cancer)Document17 pagesCase Study (Lung Cancer)Jobelle Acena100% (1)
- Online LectureDocument9 pagesOnline LectureJobelle AcenaNo ratings yet
- Er Drugs StudyDocument80 pagesEr Drugs StudyJobelle AcenaNo ratings yet
- Nursing Care Plans for Fever, Wound Healing and Pressure UlcerDocument11 pagesNursing Care Plans for Fever, Wound Healing and Pressure UlcerJobelle AcenaNo ratings yet
- Diagnostic Tests Guide for NursesDocument2 pagesDiagnostic Tests Guide for NursesBenedict AlvarezNo ratings yet
- SummaryDocument1 pageSummaryJobelle AcenaNo ratings yet
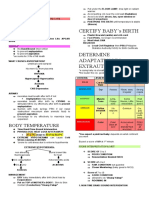
- Certify Baby'S Birth: Body TemperatureDocument9 pagesCertify Baby'S Birth: Body TemperatureJobelle Acena100% (1)
- Notes On Obstetrics: Normal Labor (Theories of Labor Onset)Document22 pagesNotes On Obstetrics: Normal Labor (Theories of Labor Onset)Jobelle Acena100% (1)
- Psychiatric Nursing Michael Jimenez, PENTAGON Slovin'S Formula: N 1 + NeDocument10 pagesPsychiatric Nursing Michael Jimenez, PENTAGON Slovin'S Formula: N 1 + NeJobelle AcenaNo ratings yet
- ER Protocols in The PhilippinesDocument9 pagesER Protocols in The PhilippinesJobelle Acena100% (1)
- Bioethics in Nursing Practice: Principles of Autonomy and Informed ConsentDocument5 pagesBioethics in Nursing Practice: Principles of Autonomy and Informed ConsentVhinny Macabontoc100% (1)
- Nursing: Core Values of NursingDocument14 pagesNursing: Core Values of NursingJobelle AcenaNo ratings yet
- Anti Psychotic DrugsDocument2 pagesAnti Psychotic DrugscalfornianursingacadNo ratings yet
- Assisted Fertilization Techniques ExplainedDocument180 pagesAssisted Fertilization Techniques ExplainedPaul Kevin Mendoza67% (3)
- BSN II Comprehensive Examination 2nd Sem 2017Document12 pagesBSN II Comprehensive Examination 2nd Sem 2017Andrea Broccoli100% (1)
- Soal 3 Diagnosis PK 1 LatenDocument12 pagesSoal 3 Diagnosis PK 1 LatenMade SuryaNo ratings yet
- Journal Pre-Proof: Seminars in PerinatologyDocument17 pagesJournal Pre-Proof: Seminars in Perinatologymarcela quirosNo ratings yet
- STEP-UP Family MedicineDocument556 pagesSTEP-UP Family MedicineGala Bozzano VukićNo ratings yet
- Maternity Blues: II. A Comparison Between Post-Operative Women and Post-Natal WomenDocument4 pagesMaternity Blues: II. A Comparison Between Post-Operative Women and Post-Natal WomenParamita Angkin SaputriNo ratings yet
- Lta AskebDocument116 pagesLta AskebDiana NoviantiNo ratings yet
- 5a's 5R's Motivational InterviewingDocument2 pages5a's 5R's Motivational Interviewingbkano100% (1)
- Skilled Birth Attendant (SBA) and Home Delivery in India: A Geographical StudyDocument8 pagesSkilled Birth Attendant (SBA) and Home Delivery in India: A Geographical StudyInternational Organization of Scientific Research (IOSR)No ratings yet
- Postnatal AssessmentDocument9 pagesPostnatal Assessmentsaleha sultanaNo ratings yet
- Assessing preterm labor risk in a pregnant patientDocument3 pagesAssessing preterm labor risk in a pregnant patientCathy Marie Constante100% (1)
- Davao Medical School Foundation Inc. College of MidwiferyDocument2 pagesDavao Medical School Foundation Inc. College of MidwiferyMon DoceNo ratings yet
- The Challenged ChildDocument17 pagesThe Challenged ChildAmy Lalringhluani Chhakchhuak50% (2)
- Child Birth and The Natural BirthDocument10 pagesChild Birth and The Natural BirthMohan Perera100% (17)
- Normal Spontaneous DeliveryDocument4 pagesNormal Spontaneous Deliveryvivian magnoNo ratings yet
- PCOG CPG - Normal Labor and DeliveryDocument51 pagesPCOG CPG - Normal Labor and Deliveryquixoticdreamer90% (10)
- Effect of Normal Childbirth on Labor PainDocument8 pagesEffect of Normal Childbirth on Labor PainAyu MarhamahNo ratings yet
- Genitourinary Fistulas GuideDocument46 pagesGenitourinary Fistulas GuidePrabhakar KumarNo ratings yet
- Maternal AssignmentDocument3 pagesMaternal AssignmentJoule PeirreNo ratings yet
- Lower Genital Tract Bleeding Causes and PreventionDocument6 pagesLower Genital Tract Bleeding Causes and PreventionRiza RsNo ratings yet
- Star Comprehensive Policy ClauseDocument16 pagesStar Comprehensive Policy ClauseGopinath PuralachettyNo ratings yet
- nsg-436 Resume FinalDocument2 pagesnsg-436 Resume Finalapi-491461037No ratings yet
- Membuat Sitasi dan Daftar Pustaka Menggunakan MendeleyDocument4 pagesMembuat Sitasi dan Daftar Pustaka Menggunakan MendeleyAnisa DillaNo ratings yet
- Antipartum Heamorrhage: Presenter Nsubuga Ivan MBCHB Stud 3.2 Kiu Lira Center Date 23 / 2 /2022Document49 pagesAntipartum Heamorrhage: Presenter Nsubuga Ivan MBCHB Stud 3.2 Kiu Lira Center Date 23 / 2 /2022Nsubuga IvanNo ratings yet
- ToS & Ospe Final Year MbbsDocument99 pagesToS & Ospe Final Year MbbsAdnanNo ratings yet
- NLE ReviewerDocument247 pagesNLE ReviewerDiana Rose DC0% (1)
- Case Study On OligoDocument22 pagesCase Study On Oligopriyanka100% (8)
- Engaging Men in Maternal Health Strategies and Outcomes From Fort Portal Regional Referral Hospital, UgandaDocument15 pagesEngaging Men in Maternal Health Strategies and Outcomes From Fort Portal Regional Referral Hospital, UgandaKIU PUBLICATION AND EXTENSIONNo ratings yet
- Induction of Labor Algorithm: Appendix RDocument1 pageInduction of Labor Algorithm: Appendix RBrolie BarsebaNo ratings yet
- Efektifitas Pijat Oksitosin Dan Senam Nifas Terhadap Proses: Involusio Uteri Ibu Postpartum Spontan Di Rs Pku TemanggungDocument13 pagesEfektifitas Pijat Oksitosin Dan Senam Nifas Terhadap Proses: Involusio Uteri Ibu Postpartum Spontan Di Rs Pku TemanggungeliNo ratings yet