Professional Documents
Culture Documents
BMC COVID Anticoagulation Algorithm Update 5 1 20
Uploaded by
Avinash Kumbhar0 ratings0% found this document useful (0 votes)
26 views1 pageBMC
Original Title
BMC-COVID-Anticoagulation-Algorithm-Update-5-1-20
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentBMC
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views1 pageBMC COVID Anticoagulation Algorithm Update 5 1 20
Uploaded by
Avinash KumbharBMC
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
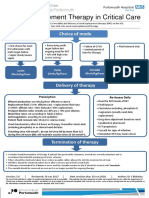
Anticoagulation in COVID-19 at BMC
Low Risk Standard Intensity Enoxaparin Prophylaxis
• No VTE or other indication for CrCL ≥ 30mL/min • 40 mg once daily for BMI ≤40 and weight <120kg
Consider trending D-
anticoagulation • 40 mg twice daily for BMI >40 or weight >120kg
dimer and repeat risk
• D-dimer < 2,000 ng/mL stratification daily
• Milder disease severity Unfractionated SQ Heparin Prophylaxis
• Acceptable bleeding risk with no bleeding or
CrCL < 30mL/min • 5,000 units twice daily for BMI ≤40 and weight <120kg
profound thrombocytopenia (with platelets • 7,500 units twice daily for BMI >40 or weight >120kg
below 25K) or severe coagulopathy
ICU patients at
Intermediate Risk## intermediate risk:
Increased Intensity Enoxaparin Prophylaxis Consider screen for
• Very high D-dimer ≥ 2,000 • 0.5 mg/kg twice daily (with maximum dose of 70 mg
ng/mL (≥ 8x ULN of BMC assay) CrCL ≥ 30mL/min DVT with POCUS
twice daily for >130 kg)
• Moderate to severe disease
severity (i.e. PaO2/FiO2 ≤300, Pregnancy: Refer to
Unfractionated Heparin Infusion BMC’s OB VTE Guideline:
SIC score ≥4, higher SOFA score) CrCL < 30mL/min (No Bolus and Low aPTT Goal 45-65)
• Risk of bleeding deemed to be acceptable for plus may consider 3-6
more intense prophylactic anticoagulation
• No bolus with infusion of 8 units/kg/hr weeks of prophylactic
• Thrombosis risk likely persists beyond lab enoxaparin for symptomatic
findings falling below threshold
COVID postpartum patients
High Risk/Full AC Full Anticoagulation with Enoxaparin
CrCL ≥ 30mL/min • 1 mg/kg twice daily
• Confirmed VTE Consider VTE
• Established reason for screening in patients
Unfractionated Heparin Infusion with rapid increases
therapeutic AC (Afib, prosthetic
(Bolus and Standard aPTT Goal 55-90)
valve, etc.)** in D-dimer (≥ 5-fold
• If not on anticoagulation, 80 units/kg bolus
• HD/CVVHD with clotting of then infusion of 18 units/kg/hr for BMI <30 or
in 48 hours) or
dialysis tubing or lines resulting 15 units/kg/hr for BMI >30 acutely worsening
CrCL< 30mL/min oxygenation/
in repeated interruptions • If transitioning anticoagulation regimens/risk
• High clinical concern for DVT/PE category consider consulting pharmacy (page increased dead space.
but unstable/ otherwise unable 9825 off hours) for adjustment dosing Consider empiric
to undergo confirmatory testing • Consider anti-Xa level if poor response to anti-coagulation if
treatment or additional thrombosis suspected low bleeding risk
** May continue prior anticoagulation regimen if clinically deemed appropriate
## May consider extended prophylaxis for 4 wks upon discharge (potential agent such as apixaban 2.5 mg BID) based upon clinical features
You might also like
- VTE-Prophylaxis-Protocol - MOHDocument13 pagesVTE-Prophylaxis-Protocol - MOHreham ONo ratings yet
- VTE - Prophylaxis - PROTOCOL - V1.1 - With Forms - 07 - Dec - 2023Document20 pagesVTE - Prophylaxis - PROTOCOL - V1.1 - With Forms - 07 - Dec - 2023hatem newishyNo ratings yet
- VTE Prophylaxis PROTOCOL V1.2 Withforms 31 Dec 2023Document19 pagesVTE Prophylaxis PROTOCOL V1.2 Withforms 31 Dec 2023hatem newishyNo ratings yet
- Venous Thromboembolism With Blanks ResidentsDocument9 pagesVenous Thromboembolism With Blanks Residentsapi-648714317No ratings yet
- Thrombosis Risk Factor Assessment (Choose All That Apply) : Deep Vein Thrombosis (DVT) Prophylaxis OrdersDocument2 pagesThrombosis Risk Factor Assessment (Choose All That Apply) : Deep Vein Thrombosis (DVT) Prophylaxis OrdersPutu Gizha Satrya GautamaNo ratings yet
- COVID-19 Drugs & Treatment: BWH Quick-Reference GuideDocument1 pageCOVID-19 Drugs & Treatment: BWH Quick-Reference GuideBoules AtefNo ratings yet
- Anticoagulation Dosing Recommendations COVID 19 PatientsDocument1 pageAnticoagulation Dosing Recommendations COVID 19 PatientsChalwe HowardNo ratings yet
- Renal Replacement Therapy in Critical Care: Choice of ModeDocument15 pagesRenal Replacement Therapy in Critical Care: Choice of ModePeter AgabaNo ratings yet
- NICU Drugs GuideDocument49 pagesNICU Drugs GuideArhanNo ratings yet
- GOOVBEVLD ProtocolDocument6 pagesGOOVBEVLD ProtocolNixon ArchilaNo ratings yet
- DabigatranDocument25 pagesDabigatranNagesh JadavNo ratings yet
- Id 397 TeicoplaninDocument2 pagesId 397 TeicoplaninStacey WoodsNo ratings yet
- (April 2020) : Is The Indication Appropriate For A Doac?Document1 page(April 2020) : Is The Indication Appropriate For A Doac?SNo ratings yet
- Renal Replacement Therapy in Critical Care: Choice of ModeDocument15 pagesRenal Replacement Therapy in Critical Care: Choice of ModeJelena Obrenovic StankovicNo ratings yet
- Anticoagulation Protocol For PostDocument8 pagesAnticoagulation Protocol For PostMohammed IbrahimNo ratings yet
- Antibiotic Pocket GuideDocument19 pagesAntibiotic Pocket GuideNaomi Liang100% (1)
- SHC Vancomycin Dosing GuideDocument8 pagesSHC Vancomycin Dosing GuidePitchya WangmeesriNo ratings yet
- BC Cancer Protocol Summary For Primary Treatment of Visible Residual (Extreme Risk) Invasive Epithelial Ovarian, Fallopian Tube or Peritoneal Cancer Using Carboplatin and PaclitaxelDocument4 pagesBC Cancer Protocol Summary For Primary Treatment of Visible Residual (Extreme Risk) Invasive Epithelial Ovarian, Fallopian Tube or Peritoneal Cancer Using Carboplatin and PaclitaxelraraNo ratings yet
- Vancomycin Dosing and Monitoring in AdultsDocument1 pageVancomycin Dosing and Monitoring in AdultsjulialeoNo ratings yet
- 1.13 Hyper-CVAD-MA Version 2.1Document5 pages1.13 Hyper-CVAD-MA Version 2.1Alina CrissNo ratings yet
- 2013 Vancomycin Do Sing GuideDocument1 page2013 Vancomycin Do Sing GuideaLPHA1No ratings yet
- Medication Administration PolicyDocument76 pagesMedication Administration PolicyJully GaciasNo ratings yet
- HNLADCF ProtocolDocument5 pagesHNLADCF ProtocolCristina Ștefania RădulescuNo ratings yet
- Antibiotic Protocol 2018Document10 pagesAntibiotic Protocol 2018sumayyah995No ratings yet
- VTE Form - Surgical & Medical PatientsDocument2 pagesVTE Form - Surgical & Medical PatientsNatasha BhasinNo ratings yet
- Commonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFDocument12 pagesCommonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFYannis Zoldenberg100% (1)
- New Oral Anticoagulants Guidelines: Kai YapDocument23 pagesNew Oral Anticoagulants Guidelines: Kai YapMuhammad Reza FirdausNo ratings yet
- Adult Vancomycin Dosing Guidelines DefinitionsDocument2 pagesAdult Vancomycin Dosing Guidelines DefinitionsPhạm DuyênNo ratings yet
- Gocxcrt ProtocolDocument3 pagesGocxcrt ProtocolNovrilia AtikaNo ratings yet
- VTE Prophylaxis GuidelinesDocument1 pageVTE Prophylaxis GuidelinesSylvia Ruth Alisa Nababan100% (1)
- Capecitabine IrinotecanDocument7 pagesCapecitabine Irinotecantanasa adrianNo ratings yet
- Diagnose CKD:: ACE inhibitor/ARB UseDocument2 pagesDiagnose CKD:: ACE inhibitor/ARB UseAman AmanNo ratings yet
- Enoxaparin Info SheetDocument7 pagesEnoxaparin Info SheetjafarkassimNo ratings yet
- Anti CoagulationDocument2 pagesAnti Coagulationsundance127No ratings yet
- General Principles of Antibiotic TherapyDocument44 pagesGeneral Principles of Antibiotic TherapyFadhly SharimanNo ratings yet
- GOOVCATX ProtocolDocument7 pagesGOOVCATX Protocolthanh ngôNo ratings yet
- STEMI NotesDocument8 pagesSTEMI NotesIzzul HafiyNo ratings yet
- Haemorrhage ProtocolDocument1 pageHaemorrhage ProtocolHerwinda GeraldineNo ratings yet
- Heparin Dose Adjustment in The Prescence of Renal ImpairmentDocument5 pagesHeparin Dose Adjustment in The Prescence of Renal ImpairmentRPR KSVNo ratings yet
- Aminoglycoside & VancomycinDocument10 pagesAminoglycoside & VancomycinKhor Chin PooNo ratings yet
- AmiDocument4 pagesAmipurushothama reddyNo ratings yet
- Micormedex NeoFax Essentials 2014Document8 pagesMicormedex NeoFax Essentials 2014Andreia HirtNo ratings yet
- BTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Document2 pagesBTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Corry ApriliaNo ratings yet
- SHC Vancomycin Dosing GuideDocument10 pagesSHC Vancomycin Dosing GuideAlan SmithNo ratings yet
- Newer Oral Anticoagulant: DR Shivaom Chaurasia Resident Internal MedicineDocument57 pagesNewer Oral Anticoagulant: DR Shivaom Chaurasia Resident Internal MedicineMuhammad Reza FirdausNo ratings yet
- HD ComplicationsDocument1 pageHD ComplicationsTyler VintNo ratings yet
- NH Protocol For Covid Management FinalDocument7 pagesNH Protocol For Covid Management FinalhoneyworksNo ratings yet
- Most of Cardiac Care Unit (C.C.U) DrugsDocument57 pagesMost of Cardiac Care Unit (C.C.U) DrugsOsama OmarNo ratings yet
- Management of CAP in Adults - Ontario GovernmentDocument2 pagesManagement of CAP in Adults - Ontario GovernmentSukhvir AujlaNo ratings yet
- Pediatric Acute Sepsis: Physician'S OrdersDocument4 pagesPediatric Acute Sepsis: Physician'S OrdersSughosh MitraNo ratings yet
- Enoxaparin - Prescribing, Administration and MonitoringDocument6 pagesEnoxaparin - Prescribing, Administration and MonitoringFaheem AlsabriaNo ratings yet
- COVID19 Anticoagulation GuidelinesDocument2 pagesCOVID19 Anticoagulation GuidelinesVladut BibanNo ratings yet
- Kegawatan Jantung - MeDocument41 pagesKegawatan Jantung - MeNam Min BinNo ratings yet
- COVID 19 Anticoagulation Algorithm Version Final 1.1Document2 pagesCOVID 19 Anticoagulation Algorithm Version Final 1.1Emi PuspitasariNo ratings yet
- AMLODIPINEDocument3 pagesAMLODIPINESL Hanna NebridaNo ratings yet
- EC Epirubicin Cyclophosphamide Adjuvant Neo-Adjuvant Regimen Protocol V1.0Document5 pagesEC Epirubicin Cyclophosphamide Adjuvant Neo-Adjuvant Regimen Protocol V1.0smokkerNo ratings yet
- Late Dumping SyndromeDocument1 pageLate Dumping SyndromeAvinash KumbharNo ratings yet
- Laws Derived From DefinitionsDocument1 pageLaws Derived From DefinitionsAvinash KumbharNo ratings yet
- SI Unit of ConductivityDocument1 pageSI Unit of ConductivityAvinash KumbharNo ratings yet
- Rectilinear Propagation of LightDocument2 pagesRectilinear Propagation of LightAvinash KumbharNo ratings yet
- Application of Laws of PhysicsDocument1 pageApplication of Laws of PhysicsAvinash KumbharNo ratings yet
- What Is Magnetic Flux?Document2 pagesWhat Is Magnetic Flux?Avinash KumbharNo ratings yet
- Scan 29 Aug 2020Document1 pageScan 29 Aug 2020Avinash KumbharNo ratings yet
- Plaquenil®: Hydroxychloroquine Sulfate, UspDocument8 pagesPlaquenil®: Hydroxychloroquine Sulfate, UspAvinash KumbharNo ratings yet
- The Work Entitled Brahma Jnanavali Mala, by Hearing Which Just OnceDocument3 pagesThe Work Entitled Brahma Jnanavali Mala, by Hearing Which Just OnceAvinash KumbharNo ratings yet
- Covid VaccineDocument1 pageCovid VaccineAvinash KumbharNo ratings yet
- Actemra GL-019952Document11 pagesActemra GL-019952Avinash KumbharNo ratings yet
- Knowledge Is SharingDocument1 pageKnowledge Is SharingAvinash KumbharNo ratings yet
- Img E45f61e63ea9-1Document1 pageImg E45f61e63ea9-1Avinash KumbharNo ratings yet
- Covid 19 A PDFDocument1 pageCovid 19 A PDFAvinash KumbharNo ratings yet
- Helping OthersDocument1 pageHelping OthersAvinash KumbharNo ratings yet
- Scan 29 Aug 2020 PDFDocument1 pageScan 29 Aug 2020 PDFAvinash KumbharNo ratings yet
- Scan 29 Aug 2020Document1 pageScan 29 Aug 2020Avinash KumbharNo ratings yet
- Osho AdviceDocument1 pageOsho AdviceAvinash KumbharNo ratings yet
- Osho AdviceDocument1 pageOsho AdviceAvinash KumbharNo ratings yet
- Scan 29 Aug 2020Document1 pageScan 29 Aug 2020Avinash KumbharNo ratings yet
- Osho AdviceDocument1 pageOsho AdviceAvinash KumbharNo ratings yet
- Sharing ResearchDocument1 pageSharing ResearchAvinash KumbharNo ratings yet
- Working On Documents Will Help Us To Download. Working and Helping Is Important. Share It Is Better. Scribd Has Good Collection of BooksDocument1 pageWorking On Documents Will Help Us To Download. Working and Helping Is Important. Share It Is Better. Scribd Has Good Collection of BooksAvinash KumbharNo ratings yet
- Scan 29 Aug 2020Document1 pageScan 29 Aug 2020Avinash KumbharNo ratings yet
- Working On Documents Will Help Us To Download. Working and Helping Is ImportantDocument1 pageWorking On Documents Will Help Us To Download. Working and Helping Is ImportantAvinash KumbharNo ratings yet
- Corona Discharge-Policy PDFDocument2 pagesCorona Discharge-Policy PDFAvinash KumbharNo ratings yet
- Cor On Va Virus Helpline NumberDocument1 pageCor On Va Virus Helpline NumberAim Softnet IT ProfessionalNo ratings yet
- Swdetuyetr 24Document10 pagesSwdetuyetr 24JPDGLNo ratings yet
- DistrictWiseList324 PDFDocument5 pagesDistrictWiseList324 PDFAvinash KumbharNo ratings yet
- Thrombosis and EmbolismDocument39 pagesThrombosis and Embolismilva100% (1)
- CH3 Patho D&R AgamDocument30 pagesCH3 Patho D&R AgamS Balagopal SivaprakasamNo ratings yet
- Surgery RemediationDocument14 pagesSurgery RemediationDrbee10No ratings yet
- Tutorials in Surgery For 4th Medical StudentsDocument180 pagesTutorials in Surgery For 4th Medical StudentsAnonymous jSTkQVC27bNo ratings yet
- Paget Schroetter ReviewDocument5 pagesPaget Schroetter ReviewHacheNo ratings yet
- Practical General Practice Ebook Guidelines For E... - (PG 219 - 224)Document6 pagesPractical General Practice Ebook Guidelines For E... - (PG 219 - 224)Sarah UddinNo ratings yet
- Pulm Embolism Pearls Pitfalls Protocols 1Document60 pagesPulm Embolism Pearls Pitfalls Protocols 1Gordana PuzovicNo ratings yet
- Vascular+ Endocrine- (breast) Quiz 2 تجميعةDocument32 pagesVascular+ Endocrine- (breast) Quiz 2 تجميعةlclkNo ratings yet
- Clsi H49 ADocument44 pagesClsi H49 ACristian Gutiérrez VeraNo ratings yet
- Product Information Ultravist: 130829ultravistpi Page 1 of 1Document20 pagesProduct Information Ultravist: 130829ultravistpi Page 1 of 1Jasmeet Singh AroraNo ratings yet
- Recommandations Anticoagulante 2015 court-ENDocument17 pagesRecommandations Anticoagulante 2015 court-ENcatalin petreNo ratings yet
- Initial Assessment and Management of Acute StrokeDocument49 pagesInitial Assessment and Management of Acute StrokeIrina DuceacNo ratings yet
- Pharmacological Review of AnticoagulantsDocument16 pagesPharmacological Review of AnticoagulantsDiplomski Seminarski RadoviNo ratings yet
- 10.1007@s00266 019 01576 2Document10 pages10.1007@s00266 019 01576 2Antonio CardenasNo ratings yet
- Post Operative Care of Patients (30!1!10)Document57 pagesPost Operative Care of Patients (30!1!10)suleman2009No ratings yet
- Lec 1disorders of Vascular Flow and ShockDocument91 pagesLec 1disorders of Vascular Flow and ShockMohid AhmedNo ratings yet
- PIIS1542356523003166Document14 pagesPIIS1542356523003166josephNo ratings yet
- Perioperative Medication Management - UpToDateDocument51 pagesPerioperative Medication Management - UpToDateAlex Kulia100% (1)
- Society of Obstetric Anesthesia and Perinatology (SOAP) Enhanced Recovery After Cesarean (ERAC) Consensus StatementDocument23 pagesSociety of Obstetric Anesthesia and Perinatology (SOAP) Enhanced Recovery After Cesarean (ERAC) Consensus StatementCarlos Emilio Paz IllescasNo ratings yet
- TX of Pulmonary Embolism - Knowledge at AMBOSSDocument8 pagesTX of Pulmonary Embolism - Knowledge at AMBOSSLogan Zara100% (1)
- Pertemuan 7 LiyanaDocument36 pagesPertemuan 7 LiyanaLiyana SafitriNo ratings yet
- Thrombosis: Pgi Ricky G. JalecoDocument34 pagesThrombosis: Pgi Ricky G. JalecoRicky JalecoNo ratings yet
- CMQCC - Maternal Early Warning SystemDocument3 pagesCMQCC - Maternal Early Warning SystemDesi WildayaniNo ratings yet
- HeparinDocument2 pagesHeparinNinoska Garcia-Ortiz100% (4)
- New Zealand Data Sheet: Primolut N® Qualitative and Quantitative CompositionDocument13 pagesNew Zealand Data Sheet: Primolut N® Qualitative and Quantitative CompositionMohammed ShakilNo ratings yet
- Case-Control Study DesignDocument36 pagesCase-Control Study DesignPrince AlexNo ratings yet
- Thrombosis and EmbolismDocument86 pagesThrombosis and EmbolismanviNo ratings yet
- Cid en AdultosDocument38 pagesCid en AdultosJosephGabrielNo ratings yet
- CDC Birth Control ChartDocument2 pagesCDC Birth Control ChartCaitlin StrohlNo ratings yet
- Pradaxa, Only Noac: Prescribe THE With A Specific Reversal AgentDocument2 pagesPradaxa, Only Noac: Prescribe THE With A Specific Reversal AgentCodruț DragomirescuNo ratings yet