Professional Documents
Culture Documents
1 Managing Heart Failure
Uploaded by
Quijano GpokskieCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1 Managing Heart Failure
Uploaded by
Quijano GpokskieCopyright:
Available Formats
Managing heart
Downloaded from http://journals.lww.com/nursingmadeincrediblyeasy by BhDMf5ePHKbH4TTImqenVIdHfOa5cT8dx15eYDFPAEs96yrc6Dc4J+PEQP/rmGKrNDcT/qM4Zx8= on 09/13/2020
More than 5 million Americans are living with heart failure and 500,000 more
are diagnosed each year, according to the American Heart Association. That’s
why it’s important for you to understand the disease process and the available
treatment options. We give you the lowdown so you can provide the best care
possible for this growing patient population.
By Lacey Buckler, RN, ACNP-BC, MSN
Acute Care Nurse Practitioner • Inpatient Cardiology • Gill Heart Institute • University of Kentucky • Lexington, Ky.
The author has disclosed that she has no significant relationships with or financial interest in any commercial companies that pertain to this educational activity.
Heart failure is a major public health prob- care of patients who are experiencing an
lem in the United States, and it continues to acute exacerbation of heart failure in the
be the leading cause of hospitalization in hospital and those who are managing
people over age 65. Unfortunately, the chronic heart failure in the outpatient set-
2.5
prognosis for this condition isn’t positive: ting.
ANCC
CONTACT HOURS
50% of patients with heart failure over a 4- Let’s take a closer look at the categories of
year period will die of the disease. More heart failure:
than 287,000 people die yearly of heart fail- • systolic heart failure (pumping prob-
ure, and 40% of patients admitted to the lem)—the inability of the heart to contract
hospital with the condition die or are read- enough to provide blood flow forward
mitted within 1 year. Not to mention that • diastolic heart failure (filling problem)—
the estimated annual cost for the manage- the inability of the left ventricle to relax nor-
ment of heart failure in 2006 was $29.6 bil- mally, resulting in fluid backing up into the
lion dollars. lungs
In this article, I’ll help you understand the • left-sided heart failure—the inability of
pathophysiology, causes, and signs and the left ventricle to pump enough blood,
symptoms of heart failure; important diag- causing fluid to back up into the lungs
nostic tools and treatment options; and • right-sided heart failure—the inefficient
patient-teaching strategies to help your pumping of the right side of the heart, caus-
patient manage his condition. ing congestion or fluid buildup in the ab-
domen, legs, and feet
Back to basics • acute heart failure—an emergency situa-
The basic definition of heart failure, for- tion in which a patient who was completely
merly known as congestive heart failure, is asymptomatic before the onset of heart fail-
the heart’s inability to pump enough blood ure decompensates when there’s an acute
to meet the body’s oxygen and nutrient injury to the heart, such as a myocardial in-
demands. Heart failure can be systolic or farction (MI), impairing its ability to func-
diastolic, left or right sided, and acute or tion
chronic. As a nurse, you’re likely to take • chronic heart failure—a long-term syn-
12 Nursing made Incredibly Easy! May/June 2009
failure
drome in which the patient experiences per-
sistent signs and symptoms over an ex-
tended period of time, likely as a result of a
preexisting cardiac condition.
Cause and effect
There are a variety of conditions that can
lead to the development of heart failure;
however, the progressive process that oc-
curs in response to one of these initiating
events is similar. These conditions include:
• coronary artery disease. Atherosclerosis
of the coronary arteries is the primary
cause of heart failure; it’s found in more
than 60% of patients with the condition.
Hypoxia and acidosis lead to ischemia,
which causes an MI that leads to heart
muscle necrosis, myocardial cell death, and
loss of contractility. The extent of the MI
correlates with the severity of the heart
failure.
• cardiomyopathy. A disease of the my-
ocardium, there are three types of car-
diomyopathy: dilated, hypertrophic, and
restrictive (see Picturing dilated cardiomyopa-
thy). The most common type, dilated car-
diomyopathy may result from an un-
known cause (idiopathic), an inflammatory
process such as myocarditis, or alcohol
abuse; it causes diffuse cellular necrosis
and fibrosis, leading to decreased contrac-
tility (systolic failure). Hypertrophic and
restrictive cardiomyopathy lead to de-
creased distensibility and ventricular filling
(diastolic failure). Heart failure due to car-
diomyopathy usually becomes chronic and
progressive; however, both may resolve if
the cause, such as alcohol use, is removed.
• hypertension. Systemic or pulmonary hy-
pertension increases the heart’s workload,
leading to hypertrophy of its muscle fibers.
May/June 2009 Nursing made Incredibly Easy! 13
This hypertrophy may impair the heart’s culty moving forward, increasing pressure
ability to fill properly during diastole, and within the heart and cardiac workload and
the hypertrophied ventricle may eventu- leading to heart failure. Degenerative aortic
ally fail (see Picturing left ventricular hyper- stenosis and chronic aortic and mitral regur-
trophy). gitation are often the culprits.
• valvular heart disease. The valves ensure Other conditions that may contribute to
that blood flows in one direction. In valvu- the development and severity of heart failure
lar disorders, blood has an increasing diffi- include:
Picturing dilated cardiomyopathy
Dilated cardiomyopathy primarily affects systolic function. Here’s what happens:
Secondary increased
atrial chamber size
Increased ventricular
chamber size
(dilation)
Decreased muscle
size, but increased
heart size
6
Eventually, all
5 chambers may
dilate, causing
Severe left generalized
4 ventricular
dilation occurs
cardiomegaly
with associated
The as venous risk of arrhyth-
The pathophysiology steps 3 compensatory return and mias and
mechanisms systemic emboli.
Early changes eventually are vascular
2 of heart failure
(increased
unable to
maintain
resistance
increase.
Contractility heart rate and adequate
1 in the left
ventricle
left ventricular
hypertrophy)
cardiac output.
Cardiac decreases, help the heart
muscle fibers lowering stroke to compensate
are extensively volume. functionally.
damaged.
14 Nursing made Incredibly Easy! May/June 2009
• increased metabolic rate
• iron overload
Picturing left ventricular hypertrophy
• hypoxia
Hypertrophy of the left ventricle is one of the heart’s first steps to compensate for
• severe anemia
either increased pressures or increased blood volume.
• electrolyte abnormalities
• cardiac dysrhythmias
• diabetes.
Signs and symptoms
afoot
Often, signs and symptoms of
heart failure are the key to early
Increased
detection because they lead a pa-
cardiac output
tient to seek medical attention. Thickened left
Signs and symptoms of left-
ventricular wall
sided heart failure are related to
pulmonary congestion and
Small left
ventricular
include:
cavity
• dyspnea
• unexplained cough
Thickened
septal wall
• pulmonary crackles
• low oxygen saturation levels
• third heart sound (S3)
• reduced urine output
• altered digestion
• dizziness and light-headedness
• confusion
• restlessness and anxiety assessment is the initial medical history and
• fatigue and weakness. physical exam. The nurse is often the first
Signs and symptoms of right-sided heart person to obtain data from the patient about
failure include: his history. It’s important to gather informa-
• lower extremity edema tion regarding the patient’s risk profile, his-
• enlargement of the liver tory of cardiac events, and response to previ-
• ascites (accumulation of fluid in the peri- ous therapies if this isn’t a new diagnosis.
toneal cavity) There are also many questions you can ask
• anorexia to elicit important clinical data to help the
• abdominal pain healthcare provider determine the cause and
• nausea severity of heart failure and the treatment
• weight gain plan for the patient. See Assessment questions
• weakness. for heart failure for a list of questions devel-
oped by the American Association of Heart
Diagnostically speaking Failure Nurses that can help you complete
When a patient presents with symptoms of the initial assessment.
heart failure, there’s an initial set of assess- Specific blood tests will be ordered to help
ments, lab studies, and diagnostic tests that determine the patient’s diagnosis. One of the
must be done in order to confirm the diag- most specific for heart failure is the measure-
nosis. ment of brain natriuretic peptide (BNP), a
The most important piece of the patient hormone secreted by the heart at high levels
May/June 2009 Nursing made Incredibly Easy! 15
I failed?
I demand
a retest!
when it’s injured or overworked. See thyroid function tests, a fasting lipid profile,
“Deciphering BNP” in this issue for and testing for offending drug levels.
more information about BNP as a diag- One of the most important diagnostic
nostic tool. Lab tests include a complete tools for heart failure is the echocardio-
blood cell count, complete metabolic gram, or echo. Not only is this an impor-
panel (electrolytes, creatinine, glucose, tant assessment tool when the patient pre-
and liver function studies), and urinaly- sents for the first time with heart failure,
sis. Other lab tests that may be ordered to but it can also provide information periodi-
determine the cause of heart failure include cally on the improvement of his heart’s
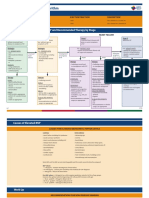
Assessment questions for heart failure
Symptoms • How often do you weigh yourself?
• What symptoms prompted you to seek medical care? When • Have you gained or lost weight recently?
did they begin? • Have you experienced any swelling? Is swelling present all
• Did your symptoms begin suddenly or gradually worsen day or only evenings?
over time? • Have you felt bloated or had edema?
• What makes the symptoms better or worse? • How far up your legs do you have edema?
• Do the symptoms occur continuously or only with certain • Are your clothes, belt, rings, and shoes tighter than 1 week
activities? or 1 month ago?
• Do symptoms improve with rest? • Have you had nausea or abdominal pain?
• Do you have any pain now? Did you recently have pain? Medications
Rate it on a 0-to-10 scale. • Have you taken all prescribed medications?
• Has your heartbeat felt any different than usual, such as rac- • Did you run out of any medications?
ing, fluttering, or skipping? • Have you had diarrhea or vomiting that may have affected
Breathing absorption of medications?
• Have you felt short of breath? Do you wake up short of • Have you taken extra diuretic medications?
breath at night? • Have you changed the dose of any medication?
• Can you speak as much as you like before getting short of • Did any physician or nurse practitioner recently prescribe
breath? different medications for you or change the dose of your med-
• What makes your breathing easier? ications?
• Do you cough? Is it worse than usual? • Do you take any over-the-counter medications or herbal
• Do you cough throughout the day or mostly in the morning? supplements?
• Do you cough up any secretions? Activity
• Do you use oxygen at home? • How far can you walk?
Sleep • Can you dress, bathe, prepare food, and climb stairs with-
• Have symptoms kept you from sleeping? out stopping to rest?
• Do you sleep in bed or in a chair? • What activities could you do recently but not now because
• Are you able to lie flat in bed? of worsened symptoms?
• How many pillows do you use to sleep? Is this more or less • Have you decreased your activity level?
than usual? Other
• Have you recently slept more or less than usual? Do you • Do you have difficulty remembering information or do you
feel rested? have feelings of confusion?
• Does your spouse or significant other tell you that you snore • Have you had other health problems that may make your
or intermittently stop breathing during sleep? heart failure worse?
Diet
• Have you recently eaten more salty foods or drank more
Source: American Association of Heart Failure Nurses. Comprehensive
water than usual? Assessment and Symptoms of Heart Failure—CASH. http://aahfn.org/
• How often do you eat out? assets/Comprehensive_Assessment_and_Symptoms_of_HF-CASH.pdf.
16 Nursing made Incredibly Easy! May/June 2009
function. Echocardiography is a type of
cardiac ultrasound that involves pulsed
Managing the stages of heart failure
and continuous Doppler waves. An echo
The American College of Cardiology/American Heart Association 2005 guide-
provides an accurate assessment of left
line update classifies heart failure into four stages and makes specific recom-
ventricular function while also determining
mendations for each.
whether a patient has systolic or diastolic
Stage A identifies patients at high risk for heart failure because of condi-
dysfunction. The number most frequently
tions such as hypertension, diabetes, and obesity.
quoted from the echo is the ejection frac-
• Treat each comorbidity according to current evidence-based guidelines.
tion (EF). EF is the measurement of how
Stage B includes patients with structural heart disease, such as left ven-
effectively the heart is pumping blood. A
tricular remodeling, left ventricular hypertrophy, or previous MI, but no symp-
normal EF is greater than 55%. That means
toms.
• Provide all appropriate therapies in Stage A.
with every cardiac cycle more than 55% of • Focus on slowing the progression of ventricular remodeling and delaying
the blood is being pumped out of the ven- the onset of heart failure symptoms.
tricle.
• Strongly recommended in appropriate patients: Treat with ACE inhibitors or
Anticipate an order for a chest X-ray to
beta-blockers unless contraindicated; these drugs delay the onset of symp-
evaluate the size of the patient’s heart and
toms and decrease the risk of death and hospitalization.
the basic heart structures and to determine
Stage C includes patients with past or current heart failure symptoms
the amount of fluid buildup in his lung
associated with structural heart disease such as advanced ventricular remod-
fields. An ECG should also be ordered to
eling.
examine the electrical activity of the heart.
• Use appropriate treatments for Stages A and B.
Other diagnostic modalities that may be
• Modify fluid and dietary intake.
ordered include a cardiac stress test, cardiac
• Use additional drug therapies, such as diuretics, aldosterone inhibitors, and
ARBs in patients who can’t tolerate ACE inhibitors, digoxin, and vasodilators.
catheterization (angiogram), a cardiac com- • Treat with nonpharmacologic measures such as biventricular pacing, an
puted tomography scan or magnetic reso- ICD, and valve or revascularization surgery.
nance imaging, radionuclide ventriculogra-
• Avoid drugs known to cause adverse reactions in symptomatic patients,
phy, ambulatory ECG monitoring (Holter
including nonsteroidal anti-inflammatory drugs, most antiarrhythmics, and
monitor), pulmonary function tests, a heart
calcium channel blockers.
biopsy, and exercise testing such as the 6-
• Administer anticoagulation therapy to patients with a history of previous
minute walk.
embolic event, paroxysmal or persistent atrial fibrillation, familial dilated car-
After all the data are obtained, the health-
diomyopathy, and underlying disorders that may increase the risk of throm-
care provider can then determine the cause
boembolism.
and classification of the patient’s heart failure
Stage D includes patients with refractory advanced heart failure having
and the appropriate treatment plan. There are
symptoms at rest or with minimal exertion and frequently requiring interven-
tion in the acute setting because of clinical deterioration.
two well-accepted classification systems used • Improve cardiac performance.
to describe heart failure, focusing on either • Facilitate diuresis.
structural abnormalities or symptoms: the
• Promote clinical stability.
American College of Cardiology/American
Achieving these goals may require I.V. diuretics, inotropic support (milri-
Heart Association stages of heart failure and
none, dobutamine, or dopamine), or vasodilators (nitroprusside, nitroglycerin,
the New York Heart Association (NYHA)
or nesiritide). As heart failure progresses, many patients can no longer toler-
functional classifications (see Managing the
ate ACE inhibitors and beta-blockers due to renal dysfunction and hypoten-
stages of heart failure).
sion and may need supportive therapy to sustain life (a left ventricular assist
device, continuous I.V. inotropic therapy, experimental surgery or drugs, or a
heart transplant) or end-of-life or hospice care.
Treatments 1, 2, 3
The Institute for Healthcare Improvement
Source: Hunt SA, American College of Cardiology, American Heart Association Task
recommends the following bundle, or com-
Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the
Evaluation and Management of Heart Failure). ACC/AHA 2005 guideline update for the
ponents of care, for all patients with heart
diagnosis and management of chronic heart failure in the adult: a report of the American
failure unless contraindicated or the patient
College of Cardiology/American Heart Association Task Force on Practice Guidelines
(Writing Committee to Update the 2001 Guidelines for the Evaluation and Management
can’t tolerate them:
of Heart Failure). J Am Coll Cardiol. 2005;46(6):e1-e82.
May/June 2009 Nursing made Incredibly Easy! 17
• assessment of left ventricular systolic The foundation of heart failure treatment
function is the ACE inhibitor. Unless it’s contraindi-
Ejection
• an angiotensin-converting enzyme (ACE) cated, every patient with an EF of less than
fraction less
than 40% = inhibitor or angiotensin receptor blocker 40% should receive an ACE inhibitor, which
ACE inhibitor. (ARB) at discharge when left ventricular EF has been shown to improve ventricular func-
is less than 40%, indicating systolic dysfunc- tion and patient well-being, reduce hospital-
tion ization, and increase survival. If the patient
• an anticoagulant at discharge if the pa- is intolerant to an ACE inhibitor, an ARB
tient has chronic or recurrent atrial fibrilla- should be initiated.
tion Another class of drugs that’s important for
• smoking cessation counseling the patient with heart failure is beta-block-
• discharge instructions addressing activity, ers. Unless contraindicated or not tolerated,
diet, medications, follow-up appointments, a beta-blocker should be started for every
weight monitoring, and what heart failure patient with an EF of less than
to do if symptoms worsen 40% due to the mortality benefit as shown in
• seasonal influenza immu- many randomized controlled trials.
nization An aldosterone antagonist may be added
• pneumococcal immunization to the patient’s pharmacologic therapy if his
• optional beta-blocker therapy at EF is less than 35% and he’s on adequate
discharge for stabilized patients with ACE inhibitor therapy. Unlike the first two
left ventricular systolic dysfunction with- categories of drugs, aldosterone antagonists
out contraindications. are approved for NYHA Classes III and IV
The treatment of heart failure can be fur- and must be used cautiously, acknowledg-
ther categorized into three basic strategies: ing renal function and potassium level.
pharmacologic management, devices and These drugs have been shown to decrease
surgical management, and lifestyle manage- hospital admissions for heart failure and also
ment. All three are very important when increase survival when added to existing
combined and provide the best prognosis for therapy.
the patient. Let’s break it down. Other drugs that may be used in heart
failure management include hydralazine/
Pharmacologic isorbide, diuretics, and digoxin. Hydralazine/
Several drugs may be used for the medical isosorbide may be added as an alternative to
management of heart failure, including an ACE inhibitor or ARB if the patient is
ACE inhibitors, beta-blockers, and aldos- intolerant to both drugs or it may be added
terone antagonists. to existing therapy if symptoms continue to
progress. Diuretics are used as symptom
relief agents and are recommended for
Drugs commonly cheat patients who have clinical signs of conges-
used to treat tion. Digoxin can be used in patients with
heart failure and atrial fibrillation to slow
sheet
conduction through the atrioventricular
heart failure
node, which increases left ventricular func-
• ACE inhibitors: captopril, enalapril,
tion and results in increased diuresis, and
lisinopril, ramipril, and trandolapril
to increase the force of myocardial contrac-
• ARBs: candesartan and valsartan
tion. It may also be added to existing thera-
• Aldosterone antagonists: eplerenone
py for a patient with NYHA Class II, III, or
and spironolactone
IV heart failure and an EF of less than 40%
• Beta-blockers: bisoprolol, carvedilol, meto-
prolol succinate, and nebivolol
who’s receiving optimal doses of an ACE
18 Nursing made Incredibly Easy! May/June 2009
Patient teaching for heart failure Teaching your
When teaching a patient with heart failure, be sure to cover: patient doesn’t
• the disorder, diagnosis, and treatment have to be
• signs and symptoms of worsening heart failure exhausting.
• when to notify the healthcare provider
• the importance of follow-up care
• the need to avoid high-sodium foods
• the need to avoid fatigue
• instructions about fluid restrictions
• the need for the patient to weigh himself every morning at the same time, before eating and after
urinating, to keep a record of his weight, and to report a weight gain of 3 to 5 pounds (1.4 to 2.3
kg) in 1 week
• the importance of smoking cessation, if appropriate
• medication dosage, administration, adverse reactions, and monitoring.
inhibitor or ARB, beta-blocker, and aldos- and destination therapy, left ventricular
terone antagonist. assist devices and artificial hearts are gaining
more popularity as technology advances.
Devices and surgical And new technologic developments in heart
management failure devices continue to be made. Devices
There are several therapeutic options in ad- that are implanted under the skin have been
dition to pharmacologic management for developed that help monitor the patient’s
the treatment of heart failure, such as pac- fluid status and then transmit the data back
ing; the use of an implantable cardioverter to the healthcare provider, which is helpful
defibrillator (ICD), ventricular assist device, in monitoring patients remotely. These
or artificial heart; and heart transplantation. devices will hopefully prove to reduce hos-
If the underlying cause of the heart failure pitalizations for heart failure in the future.
is treatable with surgery, then surgical Because the prognosis for patients with
options should be the first explored. One of heart failure is so poor, the option of heart
the most common surgical interventions is transplantation continues to be a viable
biventricular pacing, also known as cardiac choice. When a patient has reached the point
resynchronization therapy. This is recom- of end-stage heart failure, transplantation is
mended for patients who are NYHA Class commonly addressed. There’s a very
III or Class IV with a QRS prolongation of detailed, complex process by which the
greater than 120 ms who continue to experi- patient qualifies for transplantation; there-
ence symptoms despite adequate pharmaco- fore, it may not be an option for every
logic therapy. patient. You can be influential in educating
An ICD may be placed to prevent sudden your patient with heart failure about the
cardiac death caused by symptomatic and option of heart transplantation and the use
asymptomatic arrhythmias, which are seen of a ventricular assist device or artificial
frequently in patients with heart failure. The heart as a bridge to transplant, making sure
ICD is a primary prevention to reduce mor- he understands the magnitude of choosing
tality for patients with an EF of less than one or both of these routes.
35%; it’s a secondary prevention for patients
who’ve survived a ventricular tachycardic Lifestyle management
event. As a nurse, the most important piece of
Approved for both bridge-to-transplant heart failure management is helping your
May/June 2009 Nursing made Incredibly Easy! 19
Following the treatment
plan, a healthy diet,
and not smoking—now
that’s a good start.
patients understand the lifestyle modifica- to an oncoming exacerbation, he’ll know to
tions that are necessary when living with call the healthcare provider. Other topics
this disease. Nurses must help patients you should address include alcohol cessa-
learn how to change their lives to benefit tion, smoking cessation, weight loss, physi-
their health. The first step is to stress the cal activity, sexual activity, and pregnancy.
importance of adherence to the treatment By empowering the patient to embrace self-
regimen. In order to successfully treat management, you can make the difference in
heart failure, the patient must follow your patient’s prognosis (see Patient teaching
through with taking medications and com- for heart failure).
ing to follow-up appointments. Data have
shown that 20% to 60% of patients with Nursing interventions
heart failure don’t adhere to their pre- on parade
scribed treatment plan. You play an impor- In both inpatient and outpatient settings,
tant role in educating your patients on this nursing interventions for the patient with
topic. heart failure include the following:
You must also educate heart failure • administer medications and assess the
patients about symptom recognition, weight patient’s response to them
monitoring, diet and nutrition, and fluid • assess fluid balance, including intake and
intake. Intensive nursing-based education output, with a goal of optimizing fluid vol-
programs help patients understand these ume
concepts and how they relate to treating • weigh the patient daily at the same time
their disease. For example, if the patient on the same scale, usually in the morning
understands which symptoms can alert him after the patient urinates (a 2- to 3-pound
[0.9- to 1.4-kg] gain in a day or a 5-pound
[2.3 kg] gain in a week indicates trouble)
Assessing for pitting edema • auscultate lung sounds to detect an in-
crease or decrease in pulmonary crackles
• determine the degree of jugular vein dis-
tension
• identify and evaluate the severity of
edema (see Assessing for pitting edema)
• monitor the patient’s pulse rate and BP
and check for postural hypotension due to
dehydration
• examine skin turgor and mucous mem-
branes for signs of dehydration
• assess for symptoms of fluid overload.
Evidence-based
and on the ball
Heart failure is a complex disease process
that affects millions of Americans. As a
A B nurse, you play an integral role in both
the management and treatment of this
disease. Understanding the mechanisms
(A) Apply finger pressure to an area near the ankle.
of heart failure and the evidence-based
therapies used to treat it continues to be a
(B) When the pressure is released, an indentation remains in the
edematous tissue.
priority. ■
20 Nursing made Incredibly Easy! May/June 2009
of the American College of Cardiology/American Heart
Learn more about it Association Task Force on Practice Guidelines (Writing
American Association of Heart Failure Nurses. Compre- Committee to Update the 2001 Guidelines for the Evalua-
hensive Assessment and Symptoms of Heart Failure— tion and Management of Heart Failure). J Am Coll Cardiol.
CASH. http://aahfn.org/assets/Comprehensive_ 2005;46(6):e1-e82.
Assessment_and_Symptoms_of_HF-CASH.pdf. Institute for Healthcare Improvement. Deliver reliable,
Centers for Disease Control and Prevention. Heart failure evidence-based care for congestive heart failure. http://
fact sheet. http://www.cdc.gov/dhdsp/library/fs_heart_ www.ihi.org/IHI/Programs/Campaign/CHF.htm.
failure.htm. Mayo Clinic. Heart failure. http://mayoclinic.com/print/
Gardetto NJ, Greaney K, Arai L, et al. Critical pathway heart-failure/DS00061/DSECTION=all&METHOD=print.
for the management of acute heart failure at the Veterans Smeltzer SC, Bare BG, Hinkle JL. Brunner and Suddarth’s
Affairs San Diego Healthcare System: transforming per- Textbook of Medical-Surgical Nursing. 11th ed. Philadelphia,
formance measures into cardiac care. Crit Pathw Cardiol. PA: Lippincott Williams & Wilkins; 2007:946-957.
2008;7(3):153-172.
Task Force for Diagnosis and Treatment of Acute and
Heart Failure Society of America. The stages of heart Chronic Heart Failure 2008 of the European Society of Car-
failure—NYHA classification. http://www.abouthf.org/ diology, Dickstein K, Cohen-Solal A, Filippatos G, et al.
questions_stages.htm. ESC guidelines for the diagnosis and treatment of acute
Hunt SA, American College of Cardiology, American and chronic heart failure 2008: the Task Force for the Diag-
Heart Association Task Force on Practice Guidelines nosis and Treatment of Acute and Chronic Heart Failure
Want more
(Writing Committee to Update the 2001 Guidelines for 2008 of the European Society of Cardiology. Developed in CE? You
the Evaluation and Management of Heart Failure). collaboration with the Heart Failure Association of the ESC
ACC/AHA 2005 guideline update for the diagnosis and (HFA) and endorsed by the European Society of Intensive got it!
management of chronic heart failure in the adult: a report Care Medicine (ESICM). Eur Heart J. 2008;29(19):2388-2442.
within minutes.
May/June 2009 Nursing made Incredibly Easy! 21
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Chapter 25 - Substantive Test of LiabilitiesDocument10 pagesChapter 25 - Substantive Test of LiabilitiesQuijano GpokskieNo ratings yet
- Points To PonderDocument9 pagesPoints To PonderQuijano GpokskieNo ratings yet
- Physiologic Changes in Aging Affecting Various Systems: Mrs. Joji B. Castellano, R.N.,ManDocument11 pagesPhysiologic Changes in Aging Affecting Various Systems: Mrs. Joji B. Castellano, R.N.,ManQuijano GpokskieNo ratings yet
- Good Moaning ?: Gem Eunice B, QuijanoDocument9 pagesGood Moaning ?: Gem Eunice B, QuijanoQuijano GpokskieNo ratings yet
- Unadjusted Book Balance (1.) 504,000 (2.) 735,000 (3.) 700,000 (4.) 539,000Document2 pagesUnadjusted Book Balance (1.) 504,000 (2.) 735,000 (3.) 700,000 (4.) 539,000Quijano GpokskieNo ratings yet
- Abraham Maslow'S Hierarchy of Basic Human NeedsDocument8 pagesAbraham Maslow'S Hierarchy of Basic Human NeedsQuijano GpokskieNo ratings yet
- Official Study Load Student'S Copy: Section Descriptive Title Days Time Lec Lab UnitsDocument1 pageOfficial Study Load Student'S Copy: Section Descriptive Title Days Time Lec Lab UnitsQuijano GpokskieNo ratings yet
- 3a Competency Assessment - Patient Controlled AnalgesiaDocument2 pages3a Competency Assessment - Patient Controlled AnalgesiaQuijano GpokskieNo ratings yet
- One True KingDocument5 pagesOne True KingQuijano GpokskieNo ratings yet
- ABCDE Assessment Exam: Eunice QuijanoDocument3 pagesABCDE Assessment Exam: Eunice QuijanoQuijano GpokskieNo ratings yet
- Operating and Delivery Room Cases: Data SheetDocument9 pagesOperating and Delivery Room Cases: Data SheetQuijano GpokskieNo ratings yet
- 2 Myocardial Infarction Nursing Care Management and Study GuideDocument13 pages2 Myocardial Infarction Nursing Care Management and Study GuideQuijano Gpokskie100% (2)
- 1 Pain AssessmentDocument13 pages1 Pain AssessmentQuijano GpokskieNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- TTTTDocument26 pagesTTTTMoataz TrabehNo ratings yet
- Angiotensin Converting Enzyme Inhibitors: Properties and Side EffectsDocument6 pagesAngiotensin Converting Enzyme Inhibitors: Properties and Side EffectselvishmicroNo ratings yet
- Guidelines TX of HPNDocument3 pagesGuidelines TX of HPNjheyfteeNo ratings yet
- Congestive Heart FailureDocument89 pagesCongestive Heart FailureMuhammad Mustafa Ijaz100% (3)
- Galappatthy2016 Article LegEdemaWithS-amlodipineVsConvDocument10 pagesGalappatthy2016 Article LegEdemaWithS-amlodipineVsConvPathiwat M ChantanaNo ratings yet
- Cenforce 100mgDocument2 pagesCenforce 100mgjean greyNo ratings yet
- Beta BlockersDocument70 pagesBeta BlockersIrina Cabac-PogoreviciNo ratings yet
- UkpdsDocument100 pagesUkpdsBeny Rilianto0% (1)
- Articulo COVID 19Document9 pagesArticulo COVID 19Omaira TovarNo ratings yet
- Heart Failure Treatment Algorithm: Diagnosis and ClassificationDocument7 pagesHeart Failure Treatment Algorithm: Diagnosis and ClassificationLorreine Elisa FaruqNo ratings yet
- Bhagani 2018Document7 pagesBhagani 2018rifky kurniawanNo ratings yet
- Antihypertensive DrugsDocument62 pagesAntihypertensive DrugsYeshaa MiraniNo ratings yet
- 01-09 2022 Pharm Chronic Care in Cardiology 2022 R4Document62 pages01-09 2022 Pharm Chronic Care in Cardiology 2022 R4Amira HelayelNo ratings yet
- IRIS CAT Treatment Recommendations 2023Document17 pagesIRIS CAT Treatment Recommendations 2023Haniel MonteiroNo ratings yet
- ACE InhibitorsDocument26 pagesACE Inhibitorsali mohammedNo ratings yet
- Case Study: A Patient With Type 2 Diabetes Working With An Advanced Practice Pharmacist To Address Interacting ComorbiditiesDocument8 pagesCase Study: A Patient With Type 2 Diabetes Working With An Advanced Practice Pharmacist To Address Interacting ComorbiditiessamanNo ratings yet
- Cardiology Handbook Gondar University Hospital: Management GuidelinesDocument42 pagesCardiology Handbook Gondar University Hospital: Management Guidelinessky nutsNo ratings yet
- Leite de Ovelha - TrabalhoDocument30 pagesLeite de Ovelha - Trabalhodorde1234No ratings yet
- Pharma Compre SamplexDocument19 pagesPharma Compre SamplexStephanie BragatNo ratings yet
- MS 16Document7 pagesMS 16Ferdinand TerceroNo ratings yet
- Hypertensive Emergency PDFDocument14 pagesHypertensive Emergency PDFOsiithaa CañaszNo ratings yet
- Hyperkalemia: Dr. K. K. Gupta Associate Prof. Department of Medicine, KgmuDocument23 pagesHyperkalemia: Dr. K. K. Gupta Associate Prof. Department of Medicine, KgmuPrass Ekasetia PoetraNo ratings yet
- Cardiovascular Drugs: Dr. April Dawn R. LuceroDocument122 pagesCardiovascular Drugs: Dr. April Dawn R. LuceroRjDNo ratings yet
- Heartfailure Management in PlabDocument7 pagesHeartfailure Management in PlabShimmering MoonNo ratings yet
- Acute Renal FailureDocument14 pagesAcute Renal FailuredrtpkNo ratings yet
- Hypertension: Dr. Lucia Mazur-Nicorici Md. PHDDocument34 pagesHypertension: Dr. Lucia Mazur-Nicorici Md. PHDValerianBîcosNo ratings yet
- Heart Failure: Zelalem T., MD Yr III Resident, PediatricsDocument65 pagesHeart Failure: Zelalem T., MD Yr III Resident, PediatricsChalie MequanentNo ratings yet
- Drug Interactions-Principles Examples and ClinicalDocument13 pagesDrug Interactions-Principles Examples and ClinicalRaudhatul JannahNo ratings yet
- Hypertensive Crisis: Instructor'S Guide To Changes in This EditionDocument6 pagesHypertensive Crisis: Instructor'S Guide To Changes in This Editionnurmaliarizky100% (1)
- ACE InhibitorsDocument2 pagesACE InhibitorsJosephine Irena100% (1)