Professional Documents
Culture Documents
Abnormalities of The Third Stage of Labor: Dr. Ilarde
Uploaded by
Maikka IlaganOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abnormalities of The Third Stage of Labor: Dr. Ilarde
Uploaded by
Maikka IlaganCopyright:
Available Formats
1.
02
August 14, 2017
Abnormalities of the Third Stage of Labor
Dr. Ilarde
Department of Obstetrics and Gynecology
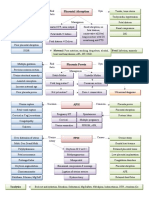
TOPIC OUTLINE Risk Factors for PPH (4T’s)
I. Introduction Tone
a. Post Partum Hemorrhage Tissue
b. Late Post Partum Hemorrhage Trauma
c. Risk Factors for PPH
Thrombin
II. Tissue Related Products of Conception
a. Placenta Accrete Syndrome Tone
b. Retained Placental Membranes Abnormalities of uterine contraction
III. Trauma Etiologic category and process Clinical Risk Factors
a. Lacerations/Genital Tract Trauma
b. Vulvovaginal Overdistention of uterus Polyhdramnios
c. Cervical Multiple gestation
IV. Puerperal Hematoma Macrosomia
V. Uterine Rupture Uterine muscle exhaustion Rapid labor
VI. Uterine Inversion (fatigue) Prolonged labor
VII. Uterine Atony
High parity
Oxytocin use/ augmentation
INTRODUCTION Prior PPH
Postpartum Hemorrhage Intraamniotic infection/ Fever
chorioamnionitis Prolonged rupture of
Blood loss of >500 ml in the first 24 hours after delivery
10% decrease in hemoglobin and hematocrit level membranes (ROM)
>500 ml blood loss in vaginal delivery and >1L for CS Functional/ anatomic Fibroids
delivery distortion of uterus Placenta previa
There is a need for transfusion Uterine relaxing medication Beta mimetics
Treacherous feature: Failure of the pulse rate and blood Bladder distention which may Halogenated anesthetics
pressure to undergo modified alterations until prevent uterine contraction nitroglycerin
large amounts of blood has been lost Tissue
Accreta Prior uterine surgery, placenta
Estimated % Heart Rate Systolic Signs and Increta previa, multiparity
Blood blood Blood symptoms
Percrata
Lost (mL) volum Pressure
e Retained placental membrane Manual placental removal
500 – 1000 10
lost– 15 < 100 Normal None Trauma
Slight Vasocon- of the genital tract
1000 – 1500 15 – 25 100 – 120 decrease striction
restlessness, Laceration of cervix, vagina or Precipitous labor
1500 – 2000 25 – 35 120 – 140 80 – 100 pallor, perineum Macrosomia
oliguria Shoulder dystocia Operative
Anuria delivery Episiotomy
2000 – 3000 35 – 45 > 140 60 – 80 altered Extensions, lacerations at Deep engagement
LOC cesarean section Malposition
Uterine Rupture Previous Uterine Surgery
Late Postpartum Hemorrhage Uterine Inversion High Parity
Bleeding after 24 hours of delivery Fundal Placenta
The following are predisposed to hemorrhage due to Excessive cord traction
low baseline blood volume: Thrombin
o Small women abnormalities of coagulation
o Severe preeclampsia/eclampsia (generalized
Preexisting clot ting History of hereditary
vasoconstriction in the body)
abnormalities coagulopathy or liver disease
o Chronic renal failure
Acquired during pregnancy Bruising, Elevated BP
Idiopathic
thrombocytopenic
Purpura
1 of x [Transcriber 1, Transcriber 2, and so on...]
Abnormalities of the Third Stage of Labor
Disseminated
intravascular
coagulation
Gestational hypertensive Elevated blood pressure
disorder of pregnancy with
adverse conditions
Dead fetus in Fetal demise
utero Fever + neutrophil
Severe infection abn
Abruption Antepartum
Amniotic Fluid Hemorrhage RISK FACTOR
Embolus Sudden collapse Associated previa
Therapeutic anticoagulants History of thrombotic disease Prior cesarian delivery
**Prompt recognition and treatment is critical MATERNAL COMPLICATIONS
A (Assessment) Massive hemorrhage
Hemodynamic Status DIC
Determine Cause of Bleeding Visceral injury
B (Breathing) ARDS
Oxygen Supplementation Renal failure
C (Circulation) Infection
Death
IV access (double line large bore catheter), adequate
Fetal Complications
circulating blood volume thru crystalloids and blood
products Adverse perinatal outcome from preterm delivery and
restricted fetal growth (IUGR)
Management
TISSUE-RETAINED PRODUCTS OF CONCEPTION Adhered placenta during the third stage of labor =
hemorrhage
Placenta Accreta Syndrome
Ideally should be diagnosed antepartum = Best outcome:
Accret, ac + crescere; to grow from adhesion or coalescence, to
planned delivery in a tertiary hospital
adhere, to become attached to
Percreta and Increta
Abnormally firm adherence to myometrium due to
o Almost always mandates hysterectomy
partial/total absence of the decidua basalis, imperfect
Conservative management: reserved from hemodynamically
development of Nitabuch layer
stable patients
Leading cause of intractable PPH
o Leaving the placenta in situ
Closely linked to prior uterine surgery ↑ incidence
after the fetus has been delivered, it may
Histological diagnosis cannot be made from the placenta
be possible to trim the umbilical cord and
alone, and the uterus or curettings with myometrium are
necessary for histopathological confirmation repair the hysterotomy incision but leave
the placenta in situ. This may be wise for
women in whom abnormal placentation
Variants of Placenta Accreta Syndrome
was not suspected before cesarean
villi are attached to the delivery and in whom uterine closure
Placenta accreta myometrium stops bleeding. After this, she can be
transferred to a higher level facility for
villi invade the definitive management.
Placenta increta myometrium Iiwanan lang yung placenta sa loob then
use chemotherapy to “kill” it
villi penetrate through the o Methotrexate therapy
Placenta percreta myometrium and to or Wedge resection – focal accrete
serosa
Retained Placental Membrane
In all three varieties, abnormal adherence may involve;
Retained placental fragments
o Total placenta accreta – involves all lobules o Inspect placenta after delivery for completeness
o Focal - if all or part of a single lobule is abnormally (routine) – cotyledon count
attached o Defect: Uterus is manually explored then fragment
o Partial – few to several cotyledons is removed
Retained succenturiate lobe
o Accessory lobes – located at a distance from the
placenta
2 of x [OBeshies <3: Jayvee, Migs, Ekay, Janzy, Bien, Cams, Lyien]
Abnormalities of the Third Stage of Labor
o Presentation: bleeding Loss of uterine contractility
Abnormal labor or failure to progress
TRAUMA Hemorrhage and shock
Lacerations/Genital Tract Trauma Recession of presenting part (from engaged to -2 or -3)
Suspect if (+) bleeding despite contracted uterus
Second most common of postpartum bleeding Fetal prognosis depends on degree of placental separation
Lacerations of perineum, cervix, vagina, or uterus and magnitude of placental bleeding and hypovolemia, should be
Vulvovaginal delivered within 18 mins
Management
Small, superficial anterior vaginal wall tears: no need for
Definitive management: Fetal delivery (immediate
repair
Extensive tears: intrauterine exploration for possible uterine abdominal delivery)
Conservative management: uterine repair (young, still
tears
o Suture repair with effective analgesia wants to give birth, not extensive and (-) extension of
o Blood replacement rupture
o Capable assistance Rupture of previous scars: revise edges and primary
Cervical closure
Hysterectomy: intractable uterine bleeding, multiple
Superficial - occur in more than half of vaginal deliveries rupture sites, longitudinal to artery
(<0.5 cm) UTERINE INVERSION
Seldom require repair unless extending to upper third of
One of the classic hemorrhagic disasters encountered in
vagina
obstetrics.
Diagnosed with visual inspection with adequate exposure
Risk Factors
Colporrhexis – total or partial avulsion of the cervix from
the vagina, usually from difficult deliveries I. Fundal placental implantation,
Other cervical injuries: II. Delayed-onset or inadequate uterine
o Anterior cervical lip ischemia contractility after delivery of the fetus, that is,
o Annular/ circular detachment of cervix uterine atony,
PUERPERAL HEMATOMA III. Cord traction applied before placental
separation, and
Most often associated with a laceration, episiotomy, or an
operative delivery IV. Abnormally adhered placentation such as with
o Spontaneous rupture of blood vessels the accrete syndromes
o Excruciating pain V. Completely inverted, protrusion of bluish
Tense, fluctauant, tender, swelling of varying site even mass
covered by discolored skin Absence of uterine fundus in palpation
Hallmark symptom: Pelvic pressure Immediate recognition is needed for good outcome
Supralevator extension the hematoma extends upward in Management
the paravaginal space and between the leaves of the broad Immediate recognition for quick resolution and good
ligament. outcome
o The hematoma may escape detection until it can be Once any degree of uterine inversion is recognized,
felt on abdominal palpation or until hypovolemia several steps must be implemented urgently and
develops simultaneously;
Pain or inability to void I. Immediate assistance
Change in vital signs disproportionate to blood loss Immediate assistance is summoned, including
Management obstetrical and anesthesia personnel.
Managed according to size, duration of delivery and II. Blood
expansion Blood is brought to the delivery suite in case it may
Expectant: smaller vulvar hematoma (follow-up closely) be needed.
Surgical exploration: severe pain or hematoma continues III. Large bore intravenous system
to enlarge The woman is evaluated for emergency general
Embolization: primarily or secondarily if surgical attempts anesthesia. Large-bore intravenous infusion
for homeostasis have failed systems are secured to begin rapid crystalloid
infusion to treat hypovolemia while awaiting
UTERINE RUPTURE
arrival of blood for transfusion.
Primary previously intact or unscarred uterus IV. Prompt replacement of the uterus
Secondary preexisting myometrial incision, injury, or If the recently inverted uterus has not contracted
anomaly and retracted completely and if the placenta has
Most often site: thinned out lower uterine segment already separated, then the uterus may often be
Classic Signs and Symptoms replaced simply by pushing up on the inverted
Fetal distress (during labor) – decelerated heart rate fundus with the palm of the hand and fingers in the
Diminished baseline uterine pressure direction of the long axis of the vagina.
Abdominal pain V. Leave placenta
3 of x [OBeshies <3: Jayvee, Migs, Ekay, Janzy, Bien, Cams, Lyien]
Abnormalities of the Third Stage of Labor
If the placenta is still attached, it is not removed - Ergot derviatives (methergine & ergonovine):
until infusion systems are operational and a not given in HTN patiens , cause SE include
uterine relaxant drug administered increase in blood pressure
VI. Once repositioned, give uterotonics - E & F series prostaglandin:
Once the uterus is restored to its normal F2 alpha Carboprost
configuration, tocolysis is stopped. Oxytocin is then Pge2 Dinoprostone
infused, and other uterotonics may be given Pge1 Misoprostol (yung mga binebenta sa
Meanwhile, the operator maintains the fundus in its Quiapo para magpalaglag; illegal na sa
normal anatomical position while applying bimanual Philippines)
compression to control further hemorrhage until the
uterus is well. - If unresponsive:
Surgical Intervention I. Bimanual uterine compression
When bimanual compressions fail: - Begin bimanual uterine compression, which is
a) Huntington procedure – Application of easily done and controls most cases of continuing
atraumatic clamps to each round ligament and hemorrhage. This technique is not simply fundal
upward traction. massage. The posterior uterine wall is massaged by
b) Haultian incision – If the constriction ring still one hand on the abdomen, while the other hand is
prohibits repositioning, a longitudinal surgical cut made into a fist and placed into the vagina. This fist
is made posteriorly through the ring to expose the kneads the anterior uterine wall through the
fundus and permit reinversion anterior vaginal wall. Concurrently, the uterus is
c) Hysterectomy – Last resort also compressed between the two hands.
II. Immediately mobilize the emergent-care
UTERINE ATONY obstetrical team to the delivery room and
The most frequent cause of obstetrical hemorrhage call for whole blood or packed red cells
Failure of the uterus to contract sufficiently after III. Request urgent help from the anesthesia
delivery and to arrest bleeding from vessels at the team.
placental implantation site. IV. IV large bore intravenous system
a) Duncan mechanism - Blood from the implantation - Secure at least two large-bore intravenous
site may escape into the vagina immediately catheters so that crystalloid with oxytocin is
continued simultaneously with blood products.
b) Schultze mechanism – blood remains concealed
Insert an indwelling Foley catheter for continuous
behind the placenta and membranes until the
urine output monitoring.
placenta is delivered
V. Begin volume resuscitation with rapid
RISK FACTORS
intravenous infusion of crystalloid.
Uterine overdistention
VI. With sedation, analgesia, or anesthesia
- Large fetus
established and now with optimal
- Multiple fetuses
exposure, once again manually explore the
- Hydramnios
uterine cavity for retained placental
- Retained clots
fragments and for uterine abnormalities,
Labor induction
including lacerations or rupture.
Anesthesia or analgesia
- Halogenated agents
B. NON SURGICAL INTERVENTION
- Conduction analgesia with hypotension
- Uterine packing or balloon tamponade
Labor abnormalities
Gauze, foley catheter, sengstaken blakemoore,
- Rapid labor
rush balloons, bakri postpartum balloons
- Prolonged labor
- Augmented labor
C. SURGICAL PROCEDURES
- Chorioamnionitis - Uterine compression sutures/ brace compression
Previous uterine atony sutures (parang suspenders)
PHYSICAL EXAMINATION B-lynch, square suture, hayman & cho
Identified as a soft and boggy uterus by bimanual exam
Uterus is tested by the surgeon first before
(Uterus is usually stone-hard after delivery) application of sutures
Expression of clots during uterine massage - Pelvic vessel ligation (uterus-sparing)
Every after placental delivery, palpate for contracted Uterine artery ligation
uterus, if not, do fundal massage and initiate uterotonics o Marami pang collaterals
MANAGEMENT Internal iliac artery ligation
A. UTERONICS o Decreases BP by 80%; decreases
- Oxytocin (first line) should not be given as a bolus, peripheral pulse rate
may cause hypertension and cardiac arrhythmias - Angiographic embolization
o Pure oxytocin: Intramuscular - Hysterectomy
o Diluted oxytocin: Intravenous
*When the patient is old, management is usually aggressive.
4 of x [OBeshies <3: Jayvee, Migs, Ekay, Janzy, Bien, Cams, Lyien]
Abnormalities of the Third Stage of Labor
*When the patient is young, management is usually conservative.
Answers:
ACTIVE MANAGEMENT 1. 10% decrease in hemoglobin and hematocrit level
Routine administration of oxytocin after delivery of 2. 1500-2000ml
baby IM 10 u 1 amp 3-5. Small women, severe preeclampsia/eclampsia, chronic renal
Delayed cord clamping (1 – 3 mins) or until pulsations failure
stop 6-7. associated previa & Prior caesarian delivery
Controlled cord traction to deliver the placenta 8. Colporrhexis
(support is applied on top) 9. Pelvic Pressure
10. Any of the ff:
EXPECTANT/PHYSIOLOGIC MANAGEMENT Fundal placental implantation,
Wait for signs of placental separation Delayed-onset or inadequate uterine contractility after
Placenta delivered spontaneously or with aid of gravity delivery of the fetus, that is, uterine atony,
and maternal pushing Cord traction applied before placental separation, and
Uterotonics not routinely administered Abnormally adhered placentation such as with the
accrete syndromes
SEQUELAE Completely inverted, protrusion of bluish mass
Hemorrhage 11-12. Huntington Procedure and Haultian Incision
Risk for Infection
13. Any of the following:
Risk for Recurrent PPH
- Uterine compression sutures/ brace compression
Risk for Hysterectomy sutures
Risk for Sheehan’s syndrome B-lynch, square suture, hayman & cho
Risk for multi organ failure
Uterus is tested by the surgeon first before
application of sutures
- Pelvic vessel ligation
Uterine artery ligation
Internal iliac artery ligation
- Angiographic embolization
- Hysterectomy
14. Any of the following
Routine administration of oxytocin after delivery of
baby IM 10 u 1 amp
Delayed cord clamping (1 – 3 mins)
Controlled cord traction to deliver the placenta
15. Ergot derviatives (methergine & ergonovine): not given in
HTN patiens , cause SE include increase in blood pressure
Quiz!!!!
1. PPH is defined as ___% decrease in Hemoglobin and Hematocrit
level
2. Estimated blood volume lost to produce the following
symptoms: restlessness, pallor, oliguria: _______
3-5. Give 3 risk factors that predispose women to hemorrhage
due to low baseline blood volume:
6-7. Risk Factors for placenta accrete syndrome
8. total or partial avulsion of the cervix from the vagina, usually
from difficult deliveries
9. Hallmark symptom of Puerperal Hematoma
10. Give one risk factor for Uterine Inversion
11-12. 2 Surgical Interventions for Uterine Inversion
13. Give 1 surgical intervention for Uterine Atony
14. Give an Active Management for Uterine Atony
15. Uterotonic that causes hypertension
5 of x [OBeshies <3: Jayvee, Migs, Ekay, Janzy, Bien, Cams, Lyien]
Abnormalities of the Third Stage of Labor
6 of x [OBeshies <3: Jayvee, Migs, Ekay, Janzy, Bien, Cams, Lyien]
You might also like
- Obstetrics - Obstretical HemorrhageDocument9 pagesObstetrics - Obstretical HemorrhageJonathanNo ratings yet
- Jose Gerardo Los Baños, M.D.: Topic OutlineDocument15 pagesJose Gerardo Los Baños, M.D.: Topic OutlineMaikka IlaganNo ratings yet
- Uwise HYDocument3 pagesUwise HYJack GuccioneNo ratings yet
- Management of Fracture of The Nasal BonesDocument53 pagesManagement of Fracture of The Nasal BonesMaikka IlaganNo ratings yet
- Placental Abnormalities Normal Placenta: © Mary Andrea G. Agorilla, Ust-Con 2021 - 1Document3 pagesPlacental Abnormalities Normal Placenta: © Mary Andrea G. Agorilla, Ust-Con 2021 - 1Mary AgorillaNo ratings yet
- Complications of Post PartumDocument49 pagesComplications of Post PartumakritiNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Complications of PregnancyDocument24 pagesComplications of PregnancyDeo Olarte100% (1)
- Placenta PreviaDocument6 pagesPlacenta Previamiss RN93% (14)
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionAngel Hernandez100% (1)
- 1.10 CPG For TBDocument9 pages1.10 CPG For TBMaikka IlaganNo ratings yet
- OBSTETRICAL HEMORRHAGE REVISED ScribdDocument34 pagesOBSTETRICAL HEMORRHAGE REVISED Scribdindah.obginuh.jul20No ratings yet
- Complications During Pregnancy - Chapt 5Document93 pagesComplications During Pregnancy - Chapt 5klyde_evangelistaNo ratings yet
- Ostpartum Hemorrhage: Dr. Patiyus Agustiansyah, Spog (K)Document70 pagesOstpartum Hemorrhage: Dr. Patiyus Agustiansyah, Spog (K)JoNo ratings yet
- PATHOPHYSIOLOGY - Placenta PreviaDocument5 pagesPATHOPHYSIOLOGY - Placenta PreviaFretzgine Lou Manuel100% (2)
- Breast CancerDocument4 pagesBreast CancerMaikka IlaganNo ratings yet
- وتين ٥Document26 pagesوتين ٥Mohammad AlrefaiNo ratings yet
- Preeclampsia Case StudyDocument13 pagesPreeclampsia Case StudyBiway RegalaNo ratings yet
- UntitledDocument18 pagesUntitledstuffednurseNo ratings yet
- Placenta ExaminationDocument26 pagesPlacenta ExaminationBharat Thapa100% (1)
- High - Risk Labor and Delivery 2Document106 pagesHigh - Risk Labor and Delivery 2Charmaine Louie Macalanda Lopez-Soriano100% (2)
- Guinitaran, Christine Ann P. BSN 4 Abruptio Placenta Nursing Care PlanDocument19 pagesGuinitaran, Christine Ann P. BSN 4 Abruptio Placenta Nursing Care PlanGemmalene PaclebNo ratings yet
- MCN Exam Gestational ConditionsDocument9 pagesMCN Exam Gestational ConditionsEdith Cabrera Cabigas - SabalboroNo ratings yet
- Perdarahan Pasca SalinDocument36 pagesPerdarahan Pasca SalinbennyrolandnababanNo ratings yet
- Care of Mother, Child at Risks or With Problems: Nursing Care of The High-Risk Postpartal ClientDocument3 pagesCare of Mother, Child at Risks or With Problems: Nursing Care of The High-Risk Postpartal ClientKlendy CasasNo ratings yet
- 16 - Perdarahan PostpartumDocument39 pages16 - Perdarahan PostpartumZhafir RahmanNo ratings yet
- Obstetrics and GyenacologyDocument37 pagesObstetrics and GyenacologySharoon KumarNo ratings yet
- Revisi Bidan Mei 2021 HPPDocument78 pagesRevisi Bidan Mei 2021 HPPNurye MsglowbeautyNo ratings yet
- Obstetrical HemorrhageDocument107 pagesObstetrical HemorrhageShael ZoletaNo ratings yet
- Obstetrics 2: Obstetric Hemorrhage (Part 2)Document4 pagesObstetrics 2: Obstetric Hemorrhage (Part 2)Dasha VeeNo ratings yet
- Post Partum Haemorrhage 1 - LoadDocument47 pagesPost Partum Haemorrhage 1 - Loadkalpananstl100% (1)
- Abnormalities of The Third Stage of LaborDocument7 pagesAbnormalities of The Third Stage of LaborDianne GalangNo ratings yet
- Mat 1Document5 pagesMat 1Shainnie IsmaelNo ratings yet
- Hemorragia Obstetric 425677 Downloadable 3667181Document22 pagesHemorragia Obstetric 425677 Downloadable 3667181maykeling garciaNo ratings yet
- Ob2 Sas 13Document8 pagesOb2 Sas 13Ralph Louie ManagoNo ratings yet
- Perdarahan Pasca SalinDocument36 pagesPerdarahan Pasca Salinnaldi raufNo ratings yet
- 12 Emergency Obstetric Postpartum Hemorrhage ICM IBI Mercure Mangga Dua 2018 (English) - Min PDFDocument49 pages12 Emergency Obstetric Postpartum Hemorrhage ICM IBI Mercure Mangga Dua 2018 (English) - Min PDFLiaNo ratings yet
- Module 5 - MCN TransesDocument6 pagesModule 5 - MCN TransesCarl UyNo ratings yet
- 3 March 6, 2022 Postpartum Complications: Module No. Date: TopicDocument10 pages3 March 6, 2022 Postpartum Complications: Module No. Date: Topicanon ymousNo ratings yet
- Postpatum Obstetric EmergenciesDocument46 pagesPostpatum Obstetric EmergenciesSooryaNo ratings yet
- PathophysiologyDocument8 pagesPathophysiologyEarly SaribaNo ratings yet
- Third Stage of Labor: by Feyisa T. (Obstetrician and Gynecologist)Document51 pagesThird Stage of Labor: by Feyisa T. (Obstetrician and Gynecologist)Haleluya LeulsegedNo ratings yet
- OBII - 14 Postpartum HemorrhageDocument8 pagesOBII - 14 Postpartum HemorrhageFelina CabadingNo ratings yet
- Uterine AtonyDocument14 pagesUterine AtonyLady Jane CaguladaNo ratings yet
- Preterm Labor and Pprom: Michelle Schroeder, MD Busitema University Faculty of Health SciencesDocument39 pagesPreterm Labor and Pprom: Michelle Schroeder, MD Busitema University Faculty of Health SciencesMwanja MosesNo ratings yet
- Step Wise Pelvic DevascularisationDocument35 pagesStep Wise Pelvic DevascularisationFatimaMalazaiNo ratings yet
- Generic NameDocument3 pagesGeneric NameSittie Nashieva A. UsmanNo ratings yet
- POSTPARTUM HAEMORRHAGE CME FinalDocument14 pagesPOSTPARTUM HAEMORRHAGE CME FinalAdaha AngelNo ratings yet
- NCM - Part 6 Postpartum PDFDocument92 pagesNCM - Part 6 Postpartum PDFJianne CaloNo ratings yet
- Abruptio Vs PreviaDocument2 pagesAbruptio Vs PreviaMinette EmmanuelNo ratings yet
- Postpartum ComplicationsDocument6 pagesPostpartum ComplicationsALCANTARA ALYANNANo ratings yet
- Obstetrics - Antepartum HemorrhageDocument4 pagesObstetrics - Antepartum HemorrhageJonathanNo ratings yet
- AIP Chap6 PPHDocument58 pagesAIP Chap6 PPHrohitNo ratings yet
- Postpartal ComplicationDocument4 pagesPostpartal ComplicationHanna AligatoNo ratings yet
- Post Partum Hemorrhage: HR BP Oxygen SaturationDocument4 pagesPost Partum Hemorrhage: HR BP Oxygen SaturationErjen Alexandria SiaNo ratings yet
- DR Ward ClassDocument36 pagesDR Ward ClassChristy Mutia AlumbroNo ratings yet
- PATHOPHYSIOLOGY of ECTOPIC PREGNANCYDocument2 pagesPATHOPHYSIOLOGY of ECTOPIC PREGNANCYrye100% (2)
- Preterm LaborDocument52 pagesPreterm LaborSandi IrvantaNo ratings yet
- Causes: What Is Post Partum Hemorrhage ?Document1 pageCauses: What Is Post Partum Hemorrhage ?Dan DanNo ratings yet
- Complications in Pregnancy & Labour 3: Pre-EclampsiaDocument1 pageComplications in Pregnancy & Labour 3: Pre-EclampsiajockorrNo ratings yet
- Drug Study Format OxytocinDocument1 pageDrug Study Format OxytocinKimberly GonzalesNo ratings yet
- Obstetric BleedingDocument1 pageObstetric BleedingZiyadNo ratings yet
- Post-Partum Hge - @medicine - Way2Document6 pagesPost-Partum Hge - @medicine - Way2saeed hasan saeedNo ratings yet
- Hemorragic Post PartumDocument35 pagesHemorragic Post PartumMuhammad AsrizalNo ratings yet
- Antepartum Haemorrhage: Prepared By: Nurul Syazwani Binti RamliDocument26 pagesAntepartum Haemorrhage: Prepared By: Nurul Syazwani Binti RamliNurul Syazwani RamliNo ratings yet
- Askep Komplikasi PostpartumDocument55 pagesAskep Komplikasi PostpartumfarizkaNo ratings yet
- Placental AbnormalitiesDocument5 pagesPlacental AbnormalitiesNica Lopez FernandezNo ratings yet
- GLM0021 Postpartum Haemorrhage PDFDocument15 pagesGLM0021 Postpartum Haemorrhage PDFRubiahSheBiachNo ratings yet
- Ectopic PregnancyDocument76 pagesEctopic PregnancyVivian Jean TapayaNo ratings yet
- Konsep SCDocument16 pagesKonsep SCAndar GuswiraNo ratings yet
- MCN 80 114Document35 pagesMCN 80 114Jianne CaloNo ratings yet
- Postpartum Hemorrhage (PPH) : Prakash Thakulla InternDocument38 pagesPostpartum Hemorrhage (PPH) : Prakash Thakulla InternPrakash ThakullaNo ratings yet
- Complication On Labor and DeliveryDocument5 pagesComplication On Labor and DeliveryMeryville JacildoNo ratings yet
- Protocol For The Examination of Specimens From Patients With Plasma Cell NeoplasmsDocument12 pagesProtocol For The Examination of Specimens From Patients With Plasma Cell NeoplasmsMaikka IlaganNo ratings yet
- 2.08 Binge Eating DisorderDocument1 page2.08 Binge Eating DisorderMaikka IlaganNo ratings yet
- PSYCH-1.1C Quick Review Table-Schizo - Other Psychotic DisorderDocument1 pagePSYCH-1.1C Quick Review Table-Schizo - Other Psychotic DisorderMaikka IlaganNo ratings yet
- Family Planning: Presented By: Pgis Ilagan, Javier, PenaDocument115 pagesFamily Planning: Presented By: Pgis Ilagan, Javier, PenaMaikka IlaganNo ratings yet
- Acupuncture and Complentary & Alternative Medicine: Department of Pharmacology & ToxicologyDocument10 pagesAcupuncture and Complentary & Alternative Medicine: Department of Pharmacology & ToxicologyMaikka IlaganNo ratings yet
- Children Part I Continuation TABLEDocument5 pagesChildren Part I Continuation TABLEMaikka IlaganNo ratings yet
- Pediatric CardiologyDocument7 pagesPediatric CardiologyMaikka IlaganNo ratings yet
- 1.09 Food and Waterborne Diseases Prevention and Control ProgramDocument12 pages1.09 Food and Waterborne Diseases Prevention and Control ProgramMaikka IlaganNo ratings yet
- Gastrointestinal Disorders in Children Part Ii: Dra. Ruby Ann PunongbayanDocument8 pagesGastrointestinal Disorders in Children Part Ii: Dra. Ruby Ann PunongbayanMaikka IlaganNo ratings yet
- Acquired Heart ConditionsDocument9 pagesAcquired Heart ConditionsMaikka IlaganNo ratings yet
- 1.08 National Filariasis Elimination ProgramDocument11 pages1.08 National Filariasis Elimination ProgramMaikka IlaganNo ratings yet
- Disorders of The PleuraDocument7 pagesDisorders of The PleuraMaikka IlaganNo ratings yet
- Obstructive LesionsDocument7 pagesObstructive LesionsMaikka IlaganNo ratings yet
- Transfusion MedicineDocument4 pagesTransfusion MedicineMaikka IlaganNo ratings yet
- Jose Gerardo Los Baños, M.D.: AppendixDocument3 pagesJose Gerardo Los Baños, M.D.: AppendixMaikka IlaganNo ratings yet
- Lung Cancer: Dr. Lou Jorel TiaDocument6 pagesLung Cancer: Dr. Lou Jorel TiaMaikka IlaganNo ratings yet
- Psychiatry Ii Schizophreniform and Other DisordersDocument16 pagesPsychiatry Ii Schizophreniform and Other DisordersMaikka IlaganNo ratings yet
- Med2 1.06FDocument5 pagesMed2 1.06FMaikka IlaganNo ratings yet
- FCM Childhood IllnessesDocument12 pagesFCM Childhood IllnessesMaikka IlaganNo ratings yet
- Adolescent and Youth Health Development Program: Accidents and Accident-Prone Activities Among AdolescentsDocument4 pagesAdolescent and Youth Health Development Program: Accidents and Accident-Prone Activities Among AdolescentsMaikka IlaganNo ratings yet
- FCM National-Rabies-Control-ProgramDocument15 pagesFCM National-Rabies-Control-ProgramMaikka IlaganNo ratings yet
- FCM 2.06Document4 pagesFCM 2.06Maikka IlaganNo ratings yet
- Middle - Mortality Areas: Integrated Management of Childhood IllnessesDocument12 pagesMiddle - Mortality Areas: Integrated Management of Childhood IllnessesMaikka IlaganNo ratings yet
- 04.02-01 Endocrine IIDocument6 pages04.02-01 Endocrine IIMaikka IlaganNo ratings yet
- Clinical Infections: Three FormsDocument2 pagesClinical Infections: Three FormsMaikka IlaganNo ratings yet
- Rene Luis F. Filarca, M.D.: February 5, 2014Document8 pagesRene Luis F. Filarca, M.D.: February 5, 2014Maikka IlaganNo ratings yet
- Practice Essentials: Abruptio PlacentaeDocument2 pagesPractice Essentials: Abruptio PlacentaeNurnajwa PahimiNo ratings yet
- Antepartum HeamorrhageDocument23 pagesAntepartum HeamorrhageOlumide OlowoseluNo ratings yet
- Bleeding in PregnancyDocument4 pagesBleeding in Pregnancyrame_badiNo ratings yet
- Anestesia EXIT 2021 Anae.15423Document6 pagesAnestesia EXIT 2021 Anae.15423joseNo ratings yet
- Abruptio PlacentaDocument10 pagesAbruptio PlacentaDoc DudayNo ratings yet
- Placental Development - Implantation - Transfer - Clinical RelevanceDocument3 pagesPlacental Development - Implantation - Transfer - Clinical RelevanceLiridon SopajNo ratings yet
- Preterm Labour: Introduction and Causes by Humna AnisDocument19 pagesPreterm Labour: Introduction and Causes by Humna AnisManjunath VankadariNo ratings yet
- MATERNALDocument14 pagesMATERNALjhenwilliamsNo ratings yet
- Antepartum Haemorrhage: Learning ObjectivesDocument12 pagesAntepartum Haemorrhage: Learning Objectivesياسر كوثر هانيNo ratings yet
- Antepartum Haemorrhage - CTM Guideline 2020Document20 pagesAntepartum Haemorrhage - CTM Guideline 2020Kvy OngNo ratings yet
- APH&PPHDocument77 pagesAPH&PPHKåbåñå TürüñåNo ratings yet
- Surprised Samples With Coaching Samples (1) 2Document55 pagesSurprised Samples With Coaching Samples (1) 2EmmanuellaNo ratings yet
- 1 Chapter 21 Pregnancy Complication BLEEDING DURING PREGNANCYDocument76 pages1 Chapter 21 Pregnancy Complication BLEEDING DURING PREGNANCYCAÑADA, JOHANNELYN M.No ratings yet
- Copy3-Obgyn Final Base LvivtechDocument3,466 pagesCopy3-Obgyn Final Base LvivtechHart ElettNo ratings yet
- Intrapartum NCM 109 Rle 2Document8 pagesIntrapartum NCM 109 Rle 2Ardic j. AgapitoNo ratings yet
- Np2 Recalls 4Document7 pagesNp2 Recalls 4AhrisJeannine EscuadroNo ratings yet
- OB-GYN 250 2 (Block 3) DignityDocument19 pagesOB-GYN 250 2 (Block 3) DignityRommel OliverasNo ratings yet
- Dystocia Due To Abnormalities of PowerDocument9 pagesDystocia Due To Abnormalities of PowerTJ Aquino AddunNo ratings yet
- Emergencies ObsDocument7 pagesEmergencies ObsAshish GuptaNo ratings yet
- Antepartum BleedingDocument7 pagesAntepartum Bleedingbluecrush1No ratings yet