Professional Documents
Culture Documents
Muscle Strength Testing
Uploaded by
Giselle Chloe Baluya icoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Muscle Strength Testing
Uploaded by
Giselle Chloe Baluya icoCopyright:
Available Formats
MUSCLE STRENGTH TESTING
Lecture Notes
Muscle Strength
Muscle strength testing is an important component of the physical exam that can reveal
information about neurologic deficits. It is used to evaluate weakness and can be
effective in differentiating true weakness from imbalance or poor endurance.
The function of muscle strength testing is to evaluate the complaint of weakness, often
when there is a suspected neurologic disease. It is an integral part of the neurologic
exam, especially for patients with stroke, brain injury, spinal cord injury, neuropathy,
amyotrophic lateral sclerosis, and a host of other neurologic problems.
Assessing the patient’s ability to flex or extend the extremities against resistance
tests muscle strength. Clinicians use a 5-point scale to rate muscle strength. The
most commonly accepted method of evaluating muscle strength is the Medical Research
Council Manual Muscle Testing scale.
GRADE MUSCLE RESPONSE
5 full power of contraction against gravity and resistance or normal muscle strength
_ _
_ _ _
_ 4 _ fair but not full strength against gravity and a moderate amount of resistance or slight
_
_ _ weakness
_ 3 5 just sufficient strength to overcome the force of gravity or moderate weakness
_ 2 ability to move but not to overcome the force of gravity or severe weakness
_ 1 _ minimal contractile power (weak muscle contraction can be palpated but no movement is
_
_ _ _ noted) or very severe weakness
_ _ 0 no movement
_ _
_
__ _ A stick figure may be used to record muscle strength and is a
__ _ precise form of documenting findings. Distal and proximal
_
_
strength in both upper and lower extremities is recorded using
_ the 5-point scale. Assessment of muscle strength may be as
_ detailed as necessary. One may quickly test the strength of the
_ proximal muscles of the upper and lower extremities, always
_ comparing both sides. The strength of the finer muscles that
_ control the function of the hand (hand grasp) and the foot
(dorsiflexion and plantar flexion) can then be assessed.
Proper technique must be employed during testing to ensure valid results. Tight or
restrictive clothing should be removed so that the examiner can visualize the muscles
being tested and observe for muscle twitch. The unaffected or less affected side should
be tested first to gauge contralateral strength for comparison; all four limbs should be
tested for completeness and to help guide the differential diagnosis based on patterns of
weakness, such as upper extremity only, lower extremity only, or proximal muscles
rather than distal.
Procedure Nerve and nerve roots
1. Identify the patient. Introduce yourself.
2. Perform hand hygiene. Don disposable gloves, if necessary.
3. CHECK for factors interfering with communication, ability to respond and
other injuries.
4. Assess upper extremities.
Ask the patient to do the following:
A. Hold out his arms straight and try to bend his fingers as he maintains Radial nerve, C7
the position.
B. Keep his fingers together as you pull them apart. Ulnar nerve, T1
C. Spread his fingers apart as you push them together. Radial & ulnar nerve C7,
T1
D. Turn hands, palm facing upward, and instruct him to touch the base of Median nerve, T1
the small finger using his thumb.
E. Make a fist as you try to put his wrists down. Radial nerve, C6
F. Flex arms upward and try to pull your arms out. Musculocutaneous nerve,
C5, C6
G. In the same position, exert force to the patient’s arms and instruct to Radial nerve, C7
resist it.
H. Raise his arms sideward with his elbows flexed then try to put force by Axillary nerve, C5
pushing it down.
5. Assess lower extremities.
Ask the patient to do the following:
A. Raise your leg and not to put it down and resist the force you exert. Femoral nerve, L3
B. Slightly bend his knees and put force to totally bend his knees as the Femoral nerve, L3, L4
patient resists it.
C. In the same position, put force to straighten his legs as the patient Sciatic nerve, S1
resists the force exerted.
D. Push knees out and resist the force exerted as you push them together. Sup. Gluteal nerve, L4, L5
E. Push knees together and resist the force exerted as you pull them away Obturator nerve, L2-L4
from each other.
F. Bend foot up towards the face, try to push it down. Deep Peroneal nerve, L5
G. Bend toes up towards the face, try to push it down. Deep Peroneal nerve, L4,
L5
H. Push foot down the floor and try to push it up. Tibial nerve S1, S2
6. Ensure patient safety. Remove gloves and perform hand hygiene.
7. Make the necessary documentation.
Assessing muscle strength for unconscious patients.
Upper Extremity Strength Lower Extremity Strength
Conscious individual Have the patient hold arms out With the patient lying in a supine
horizontally, palms up, with eyes position, bend the knees to 30
closed. If there is upper limb degrees. If there is weakness in
weakness, the affected side will the lower extremities, the
"drift" or pronate within 30 affected leg will drift downward
seconds. within 30 seconds.
With patient in supine position,
flex both knees and support
under one of examiners arms.
Allow one heel to rest on the
bed. Extend the other leg at the
knee and allow it to drop gently
to the bed. Compare the speed
of drop for both legs.
Unconscious individual Lift both patient's arms together. Position patient supine. Flex the
While protecting the limbs from knees with both feet on the
injury, release both arms bed. Release the knees
together. A paralysed arm will fall simultaneously. A paralysed leg
more rapidly. will fall to an extended position
and the hip will rotate externally.
The normal leg will stay flexed for
a few seconds and gradually
assume the previous position.
You might also like
- WK13 CDN - Meningitis, Poliomyelitis, Leprosy, Tetanus, Red TideDocument43 pagesWK13 CDN - Meningitis, Poliomyelitis, Leprosy, Tetanus, Red TidePotato PceeNo ratings yet
- AnesthesiaDocument59 pagesAnesthesiaHasse Hasse100% (1)
- BCLS AclsDocument27 pagesBCLS AclsJanmichael FeliscuzoNo ratings yet
- Riaz Gul AHN Unit 1Document106 pagesRiaz Gul AHN Unit 1Riaz Gul RindNo ratings yet
- DR TahirDocument61 pagesDR TahirRohail GulNo ratings yet
- Viral Exanthem (Main)Document94 pagesViral Exanthem (Main)Starlet Rhonadez Bito-onon OrielNo ratings yet
- 04 - Soft Tissue InjuriesDocument13 pages04 - Soft Tissue InjuriesCielo GriñoNo ratings yet
- Pancreatic Cancer (Cancer of The Pancreas) : Patient Discussions: FindDocument13 pagesPancreatic Cancer (Cancer of The Pancreas) : Patient Discussions: FindMoses ZainaNo ratings yet
- Guidelines For Management of Head InjuryDocument18 pagesGuidelines For Management of Head InjuryChellamani UmakanthanNo ratings yet
- Introduction To Trauma: LSU Medical Student Clerkship, New Orleans, LADocument31 pagesIntroduction To Trauma: LSU Medical Student Clerkship, New Orleans, LAnandangNo ratings yet
- BANDAGINGDocument1 pageBANDAGINGCharisse Viste0% (1)
- Abc of Burns: Kanwal Khan Lecturer ZCPTDocument35 pagesAbc of Burns: Kanwal Khan Lecturer ZCPTKanwal KhanNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Stomach Peptic UlcerDocument38 pagesStomach Peptic UlcermohamedNo ratings yet
- In The Name of Allah, The Most Beneficent and MercifulDocument35 pagesIn The Name of Allah, The Most Beneficent and MercifulAhmedMenshawyNo ratings yet
- Assessing The Thorax and LungsDocument3 pagesAssessing The Thorax and LungsZJ GarcianoNo ratings yet
- Anatomy of The Eye EYE: Extaocular StructuresDocument5 pagesAnatomy of The Eye EYE: Extaocular StructuresfLOR_ZIANE_MAENo ratings yet
- CPR 1Document12 pagesCPR 1Renju JoseNo ratings yet
- Poisoning DecontaminationDocument14 pagesPoisoning DecontaminationadystiNo ratings yet
- Acute Limb Ischemia - WucDocument37 pagesAcute Limb Ischemia - WucOTOH RAYA OMARNo ratings yet
- Otitis MediaDocument9 pagesOtitis MediaMona Santi NainggolanNo ratings yet
- Complications of Intravenous TherapyDocument29 pagesComplications of Intravenous TherapyKrizia BonillaNo ratings yet
- Neurology Lectures 1 5 DR - Rabo 2Document20 pagesNeurology Lectures 1 5 DR - Rabo 2Miguel Cuevas DolotNo ratings yet
- Cardiac Monitoring LectureDocument30 pagesCardiac Monitoring LectureAlma Janella TOSINONo ratings yet
- Nursing Assessment Tool... CardiacDocument7 pagesNursing Assessment Tool... Cardiacjai2xNo ratings yet
- Supracondylar FractureDocument53 pagesSupracondylar Fracturedesire kbpNo ratings yet
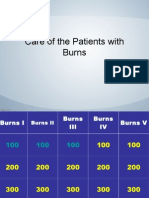
- Jeopardy Game - BurnsDocument42 pagesJeopardy Game - BurnsPC NNo ratings yet
- Principles of Trauma ManagementDocument60 pagesPrinciples of Trauma ManagementDrArish Mahmood100% (1)
- Multiple Choice Question Acn FinalDocument11 pagesMultiple Choice Question Acn FinalIqra rizwanNo ratings yet
- Assessment of The Heart-Neck Vessels-Peripheral Vessels-PULSEDocument27 pagesAssessment of The Heart-Neck Vessels-Peripheral Vessels-PULSEJonah R. MeranoNo ratings yet
- Et IntubateDocument47 pagesEt IntubatectuagentNo ratings yet
- Assisting For Application of POPDocument7 pagesAssisting For Application of POPINSERVICE EDUCATIONNo ratings yet
- HYDROCEPHALUSDocument63 pagesHYDROCEPHALUSAjeng Aristiany Rahawarin100% (2)
- Nasogastric IntubationTechniqueDocument4 pagesNasogastric IntubationTechniqueLip StickNo ratings yet
- Pain Management in The Emergency: Dr. Prathiba Prasad Emergency Physician Masafi HospitalDocument50 pagesPain Management in The Emergency: Dr. Prathiba Prasad Emergency Physician Masafi HospitalPrathiba PrassaddNo ratings yet
- Vaccination or ImmunizationDocument4 pagesVaccination or ImmunizationPrincessNo ratings yet
- Children's Respiratory NursingFrom EverandChildren's Respiratory NursingJanice MightenNo ratings yet
- What Is Traction?Document5 pagesWhat Is Traction?Tweenie DalumpinesNo ratings yet
- Compartment SynDocument51 pagesCompartment SynFIYINFOLUWA ESTHER AYODELENo ratings yet
- Case Study: Exercise 2: Triage 1Document26 pagesCase Study: Exercise 2: Triage 1Chandra DewiNo ratings yet
- Nurse-Directed Interventions To Reduce Catheter-Associated Urinary Tract InfectionsDocument10 pagesNurse-Directed Interventions To Reduce Catheter-Associated Urinary Tract InfectionsAngernani Trias WulandariNo ratings yet
- AppendicitisDocument36 pagesAppendicitisPetro MyronovNo ratings yet
- Traumatic Lesions: Head Injuries: Delano, Alexandra Julianne Duran, Fatima MedrizaDocument31 pagesTraumatic Lesions: Head Injuries: Delano, Alexandra Julianne Duran, Fatima MedrizaFatima Medriza Duran100% (1)
- Assessment of The AbdomenDocument98 pagesAssessment of The Abdomenyanna aNo ratings yet
- BIOPSYDocument8 pagesBIOPSYASHLEY DAWN BUENAFENo ratings yet
- Skin Integrity and Wound CareDocument47 pagesSkin Integrity and Wound CareCHALIE MEQUNo ratings yet
- Day Case Surgery 1LDocument21 pagesDay Case Surgery 1LdrhiwaomerNo ratings yet
- Sepsis Power Point Slide Presentation - The Guidelines - Implementation For The FutureDocument25 pagesSepsis Power Point Slide Presentation - The Guidelines - Implementation For The Futuremontie13No ratings yet
- Poisoning & BitesDocument12 pagesPoisoning & BitesJudy HandlyNo ratings yet
- Triage and Disaster: Nur Masyeerah Abdul JalilDocument22 pagesTriage and Disaster: Nur Masyeerah Abdul JalilnavenNo ratings yet
- Asthma: A. DefinitionDocument6 pagesAsthma: A. DefinitionElvando SimatupangNo ratings yet
- Cerebrovascular AccidentDocument30 pagesCerebrovascular AccidentJaydee Dalay100% (2)
- 3 Session 3 - AbdominalExamDocument15 pages3 Session 3 - AbdominalExamjhk0428No ratings yet
- Operation Theater 1Document24 pagesOperation Theater 1Susmita BeheraNo ratings yet
- Management of A Patient With Acute Abdominal Pain - College of Surgeons of Sri Lanka 2007 PDFDocument30 pagesManagement of A Patient With Acute Abdominal Pain - College of Surgeons of Sri Lanka 2007 PDFRevalitha PutriNo ratings yet
- 8-Wounds and Wound Healing-1Document31 pages8-Wounds and Wound Healing-1Aiden JosephatNo ratings yet
- Tracheostomy SuctioningDocument10 pagesTracheostomy SuctioningJANIEZA ANGEL RA�ISES BALTAZARNo ratings yet
- Meningioma Brain TumorDocument5 pagesMeningioma Brain TumorNikko Melencion100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Heart Failure2Document39 pagesHeart Failure2Giselle Chloe Baluya icoNo ratings yet
- NUR-086-Act-2 4Document2 pagesNUR-086-Act-2 4Giselle Chloe Baluya icoNo ratings yet
- 37420046-Ncp-Head-Injury 2Document3 pages37420046-Ncp-Head-Injury 2Giselle Chloe Baluya icoNo ratings yet
- Fundamentals of NursingDocument13 pagesFundamentals of NursingGiselle Chloe Baluya icoNo ratings yet
- The Surgical Team: Intraoperative NursingDocument4 pagesThe Surgical Team: Intraoperative NursingGiselle Chloe Baluya icoNo ratings yet
- Nursing Classifications and LanguagesDocument12 pagesNursing Classifications and LanguagesGiselle Chloe Baluya ico0% (1)
- Homeostasis, Stress and Adaptation: Types of Stressors: Physiologic Emotional/PsychologicDocument5 pagesHomeostasis, Stress and Adaptation: Types of Stressors: Physiologic Emotional/PsychologicGiselle Chloe Baluya ico100% (1)
- Increased Intracranial Pressure (IICP)Document2 pagesIncreased Intracranial Pressure (IICP)Giselle Chloe Baluya icoNo ratings yet
- Margo Mccaffery, A Nurse and A Pioneer in Pain ManagementDocument7 pagesMargo Mccaffery, A Nurse and A Pioneer in Pain ManagementGiselle Chloe Baluya ico100% (1)
- Anatomy MCQ - Lower Limb PDFDocument30 pagesAnatomy MCQ - Lower Limb PDFnonNo ratings yet
- Nat MurDocument19 pagesNat MurSun BNo ratings yet
- The Peripheral Vascular SystemDocument36 pagesThe Peripheral Vascular SystemTsedkenu CavanNo ratings yet
- Operative Dictations in Plastics PDFDocument583 pagesOperative Dictations in Plastics PDFBrînduşa Ciobanu100% (2)
- Splints and Casts Indications and MethodsDocument9 pagesSplints and Casts Indications and MethodsJay GaneshNo ratings yet
- Human Anatomy For Artists Eliot GoldfingerDocument231 pagesHuman Anatomy For Artists Eliot GoldfingerQueen B100% (2)
- Epidemiology of Football Injuries of The German Bundesliga A Media-Based, Prospective Analysis Over 7 Consecutive SeasonsDocument14 pagesEpidemiology of Football Injuries of The German Bundesliga A Media-Based, Prospective Analysis Over 7 Consecutive SeasonsAndressaNo ratings yet
- Adductor Magnus An EMG Investigation Into Proximal and Disctal Portions and Direction Specific ActionDocument9 pagesAdductor Magnus An EMG Investigation Into Proximal and Disctal Portions and Direction Specific ActionElaine CspNo ratings yet
- Enumeration of Human Body Parts According To AyurvedaDocument13 pagesEnumeration of Human Body Parts According To AyurvedaKrishna Venkat VNo ratings yet
- Bio Mechanical Analysis of FootballDocument54 pagesBio Mechanical Analysis of FootballMunesh kumar srivastava58% (12)
- Fascia Iliaca GuidelineDocument12 pagesFascia Iliaca GuidelineSyahrul Mubarak Danar SumantriNo ratings yet
- Effect of Core Stability Exercises Versus Surya Namaskar On Hamstring Tightness in Healthy Adults Using Active Knee Extension Test at The End of 6 Weeks: A Comparative StudyDocument5 pagesEffect of Core Stability Exercises Versus Surya Namaskar On Hamstring Tightness in Healthy Adults Using Active Knee Extension Test at The End of 6 Weeks: A Comparative StudysaniyaNo ratings yet
- Neuro AssessmentDocument13 pagesNeuro AssessmentOrlea Francisco-Sisio100% (2)
- TST LRS 3Document9 pagesTST LRS 3Norel Nicolae BalutaNo ratings yet
- Lower Limb: Muscle Table + PicturesDocument3 pagesLower Limb: Muscle Table + Picturesrichard_yin_397% (32)
- Short Right Leg 2Document11 pagesShort Right Leg 2Simo Aster100% (2)
- Orthobullets TraumaDocument549 pagesOrthobullets TraumaKaustubh Keskar100% (9)
- Hip Muscle Imbalances and Their Effects: Anterior Pelvic Tilt PostureDocument4 pagesHip Muscle Imbalances and Their Effects: Anterior Pelvic Tilt PostureRizki DianraNo ratings yet
- As Above So Below AcupunctureDocument5 pagesAs Above So Below AcupunctureDarren StarwynnNo ratings yet
- Jis B 9708 e 2002Document10 pagesJis B 9708 e 2002josephkirbyNo ratings yet
- Aai Mobility Program: Knee To Walls Lumbar RotationsDocument1 pageAai Mobility Program: Knee To Walls Lumbar RotationsAdarshNo ratings yet
- The Arches of The Feet Part 1Document6 pagesThe Arches of The Feet Part 1leoNo ratings yet
- Pediatric Radiography Radiographic PositioningDocument36 pagesPediatric Radiography Radiographic PositioningMenna KhNo ratings yet
- Box Jump From A Static Start: ExecutionDocument34 pagesBox Jump From A Static Start: Executioncoach_noeNo ratings yet
- Weight Loss ExcercisesDocument5 pagesWeight Loss ExcercisesTwisha KuhadaNo ratings yet
- Closed Intramedullary Nailing of Femoral Fractures PDFDocument12 pagesClosed Intramedullary Nailing of Femoral Fractures PDFAnuta GiurgiNo ratings yet
- Exploratory Latin Body PartsDocument11 pagesExploratory Latin Body PartsKari Kristine Hoskins Barrera100% (1)
- Practice Questions 1Document51 pagesPractice Questions 1Lucille Isidro CruzNo ratings yet
- Urinary System - Gross 2016Document73 pagesUrinary System - Gross 2016dawnparkNo ratings yet
- Butler - Neurodynamic TechniquesDocument55 pagesButler - Neurodynamic Techniquesmszlazak4179100% (3)