Professional Documents
Culture Documents
Lhermitte Duclos Disease - A Case Report: Ramya C, Renuka IV, Durga Prasad B, Pratyusha N
Uploaded by
ajmrdOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lhermitte Duclos Disease - A Case Report: Ramya C, Renuka IV, Durga Prasad B, Pratyusha N
Uploaded by
ajmrdCopyright:
Available Formats
American Journal of Multidisciplinary Research & Development (AJMRD)
Volume 2, Issue 7 (July- 2020), PP 19-22
ISSN: 2360-821X
www.ajmrd.com
Research Paper Open Access
Lhermitte Duclos disease - A case report
Ramya C1, Renuka IV2, Durga Prasad B3, Pratyusha N4
1,23,4
Department of Pathology, NRI Medical college, India
*Corresponding Author:Renuka IV
ABSTRACT:- Lhermitte Duclos disease is a rare cerebellar disease with very few cases published in the
literature. There is no gender predilection and can occur at any age group. We present a rare case of unilateral
LD disease in a young female with a lesion in left cerebellum. Preoperative diagnosis was made by MRI, which
is confirmed on histology. A 32yr old female presented with headache and blurring of vision since two months.
MRI revealed tiger stripped appearance of a lesion in cerebellum measuring 4.5cms× 3.5cm, which on
histopathology showed Lhermitte Duclos disease. Most of the cases can be diagnosed by MRI, but certain
malformations and medulloblastoma can be differential diagnoses on imaging. The prognosis is good with very
few cases of recurrence. Lhermitte Duclos disease is a rare cerebellar disease usually associated with Cowden
syndrome. The patient was screened for other malignancies.
Keywords:- Cerebellum, Dysplastic cerebellar gangliocytoma, Lhermitte Duclos disease
I. INTRODUCTION
Lhermitte Duclos (LD) disease is a rare disease described by French physicians Lhermitte and Duclos
in 1920. [1] There are various synonyms like dysplastic cerebellar gangliocytoma, cerebellar granule cell
hypertrophy, diffuse hypertrophy of cerebellar cortex, gangliomatosis of the cerebellum. [2] Very few cases
have been published from different countries all over the world. Most patients become symptomatic in the third
to fourth decades of life, although the disease may be present in any age group. [3] They are usually confined to
one hemisphere but bilateral cases have also been reported. [4] Clinically, patients may be asymptomatic, or
they may present with symptoms of ataxia, headache, cranial nerve palsy, paroxysm of vertigo, psychic
deterioration and, in severe cases, signs and symptoms of intracranial hypertension secondary to hydrocephalus.
[5, 6]
Magnetic resonance imaging (MRI) is the appropriate technique allowing preoperative diagnosis with the
characteristic striated pattern of exaggerated folia appearance on T2-weighted images.[7] MRI with the newer
imaging capabilities can demonstrate the pathology and pathophysiology in Lhermitte-Duclos disease better.[7]
Neurological deterioration or increase in the size of the cerebellar mass necessitates surgery and removal of the
mass. PTEN mutations have been identified in adult patients with LD disease but not in children. [8]
II. CASE HISTORY:
A 32year old female presented with headache & blurring of vision since 2 months. Headache was in
left temporoparietal region, more in the mornings. On neurological examination, left cerebellar sign was
positive. Fundus examination revealed bilateral papilledema. Complete Blood Picture and renal profile were
normal. Chest X-Ray, Electrocardiogram (ECG), Echocardiography were within normal limits. MRI revealed a
mixed intensity (T1 hypo, T2 heterogenously hyperintense intra axial mass lesion in the left cerebellum and
vermis measuring 4.5cmx 3.5cms in size (Fig 1a & 1b). The lesion was causing mass effect over adjacent
stuctures causing supratentorial ventricular system dilatation with cerebrospinal fluid seepage.
Multidisciplinary Journal www.ajmrd.com Page | 19
Lhermitte Duclos disease - A case report
Figure 1a: MRI - Axial T2 weighted image showing lesion with striated appearance in left cerebellum
Figure 1b: MRI - Sagittal T2 image showing expansion and striated appearance of lesion in cerebellum
Left retromastoid suboccipital craniotomy with tumour excision was done and sent for histopathological
study. We received multiple grey white tissue bits of total size 2 × 1.5cm. There was relative preservation of
cerebellar folia on gross appearance. Entire tissue was submitted for study. On Microscopy, Normal cerebellar
tissue was also included in the material along with the lesion (Fig 2a &2b). There was an abnormal increase of
dysplastic ganglion cells (Fig 3a, 4a) and myelinated axons of nerve fibers (Fig 3b). There were no areas of
necrosis or increased mitotic activity. Immunohistochemistry (IHC) was positive for synaptophysin in the
ganglion cells (Fig 4b). Post-operative computed tomography (CT) scan showed minimal subarachnoid
haemorrhage along the interhemispheric fissure with minimal hydrocephalus. There is decrease in the size of
ventricles compared to preoperative scan. The patient was screened for malignancies and had no manifestations
of Cowden syndrome.
Figure 2a: Lesion with adjacent normal cerebellar tissue 40X, H&E
Figure 2b: Normal cerebellar tissue 100x, H & E
Multidisciplinary Journal www.ajmrd.com Page | 20
Lhermitte Duclos disease - A case report
Figure 3a: Dysplastic ganglion cells 100X, H&E
Figure 3b: Myelinated axons 100X, H&E
Figure 4a: Dysplastic ganglion cells 400X, H&E
Figure 4b: IHC -Synaptophysin 400X
III. DISCUSSION
Preoperative diagnosis was made by MRI in our case, but few other lesions can mimic LD disease on
radiology. Hyuang et al. revealed characteristic tiger stripped appearance on MRI and histopathological
examination revealed normal cerebellum with arachnoid vascular malformation and partial loss of Purkinje
cells. [9] Nair et al. reported co existing LD disease with Dysembryoplastic Neuroepithelial tumour on
histopathology with characteristic tiger stripping on MRI images.[10] Infiltrating medulloblastomas have also
been reported to mimic LD on imaging.[11]
Sheets of dysplastic ganglionic cells were seen in granular layer in our case. LD disease causes diffuse
enlargement of molecular and internal granular layers of the cerebellum, which are filled by ganglionic cells of
various sizes. [12] Markers of the neoplastic process, such as mitotic activity, necrosis and endothelial
proliferation are characteristically absent as seen in our case. No case of malignant transformation has been
reported. [13] It can recur locally but do not spread to other structures in the brain or outside central nervous
system. [2]
There is no association with Cowden syndrome in our case. In a study of 211 patients with Cowden
syndrome, 32% developed LD disease. [14] Because cerebellar lesions may develop before the appearance of
other features of Cowden syndrome, patients with Lhermitte Duclos disease should be monitored for the
development of additional tumours, including breast cancer in females. [2]
Multidisciplinary Journal www.ajmrd.com Page | 21
Lhermitte Duclos disease - A case report
IV. CONCLUSION:
We are presenting a rare case of unilateral LD disease in young female with a lesion in left cerebellum.
Preoperative diagnosis was made by MRI, which is confirmed on histology. The patient was screened for other
malignancies even though there was no association with Cowden syndrome in our case.
Conflicts of interest : NIL
Acknowledgement : NIL
Sources of support : NIL
REFERENCES:
[1]. Lhermitte J, Duclos P. Sur un ganglioneurome diffus du cortex du cervelet. Bull Assoc Fr Etude
Cancer 1920; 9:99 –107.
[2]. David NL, Hiroko O, Otmar D W, Webster K C. WHO classification of tumours of the central nervous
system. Revised 4th edition IARC press Lyon 2016; 142-143.
[3]. Kumar R, Vaid VK, Kalra SK. Lhermitte-Duclos disease. Childs Nerv Syst. 2007 Jul; 23(7):729-32.
[4]. Bozbuga M, Gulec I, Suslu HT, Bayindir C. Bilateral Lhermitte-Duclos disease. Neurol India. 2010;
58(2):309-11.
[5]. Somagawa C, Ono T, Honda R, Baba H, Hiu T, Ushijima R et al. Frequent vomiting attacks in a patient
with Lhermitte-Duclos disease: a rare pathophysiology of cerebellar lesions?. J Neurosurg
Pediatr. 2017; 20(3):298-301
[6]. Otheman Y, Aalouane R, Aarab C, Rammouz I. A case report of Lhermitte-Duclos disease revealed by
psychiatric disturbances. Ann Gen Psychiatry. 2017; 16:24.
[7]. Thomas B, Krishnamoorthy T, Radhakrishnan VV, Kesavadas C. Advanced MR imaging in Lhermitte-
Duclos disease: moving closer to pathology and pathophysiology. Neuroradiology 2007; 49: 733-738.
[8]. Zhou XP, Marsh DJ, Morrison CD, Chaudhury AR, Maxwell M, Reinfenberger G, et al. Germ line
inactivation of PTEN and dysregulation of the phosphoinositol-3-kinase/Akt pathway cause human
Lhermitte Duclos disease in adults. Am J Hum Genet.2003; 73(5) 1191-8.
[9]. Huang S, Zhang G, Zhang J. Similar MR imaging characteristics but different pathological changes: a
misdiagnosis for Lhermitte-Duclos disease and review of the literature. Int J Clin Exp Pathol. 2015;
8(6):7583-7.
[10]. Nair P, Pal L, Jaiswal AK, Behari S. Lhermitte-Duclos disease associated with dysembryoplastic
neuroepithelial tumor differentiation with characteristic magnetic resonance appearance of "tiger
striping". World Neurosurg. 2011; 75(5-6):699-703.
[11]. Mittal P, Gupta K, Saggar K, Kaur S. Adult medulloblastoma mimicking Lhermitte duclos disease: can
diffusion weighted imaging help? Neurol india. 57(2): 203-5
[12]. Abel TW, Baker SJ, Fraser MM, Tihan T, Nelson JS, Yachnis AT, et al. Lhermitte Duclos disease: a
report of 31 cases with immunohistochemical analysis of PTEN/AKT/mTOR pathway. J Neuropathol
Exp Neurol. 64(4): 341-9.
[13]. Giorgianni A, Pellegrino C, De Benedictis A, Mercuri A, Baruzzi F, Minotto R, et al. Lhermitte-Duclos
disease. A case report. Neuroradiol J. 2013; 26(6):655-60.
[14]. Rigert -Johnson DL, Gleeson FC, Roberts M, Tholen K, Youngborg L, Bullock M, et al. cancer and
lhermitte duclos disase are common in cowden syndrome patients. Hered Cancer Clin Pract. 2010;
8(1): 6.
Multidisciplinary Journal www.ajmrd.com Page | 22
You might also like
- Unipack II ManualDocument30 pagesUnipack II ManualMarijaŽaper67% (3)
- ASME B16.5 Flange Rating CalculatorDocument10 pagesASME B16.5 Flange Rating Calculatorfaizal100% (2)
- BX10/BX10 MB: Weighing Terminals Technical ManualDocument60 pagesBX10/BX10 MB: Weighing Terminals Technical Manualfelipezambrano50% (2)
- Follicular Carcinoma of Thyroid Presenting As Brain MetastasisDocument3 pagesFollicular Carcinoma of Thyroid Presenting As Brain MetastasisArif Susilo RahadiNo ratings yet
- Secondary Syphilis Presenting As Diffused Folliculitis: ReferencesDocument3 pagesSecondary Syphilis Presenting As Diffused Folliculitis: ReferencesNazihan Safitri AlkatiriNo ratings yet
- 264 2011 Article 1480Document6 pages264 2011 Article 1480Paul Mendez AguilarNo ratings yet
- A Rare Case of Space Occupying Lesion of Brainstem in An Elderly Male PatientDocument3 pagesA Rare Case of Space Occupying Lesion of Brainstem in An Elderly Male PatientInternational Journal of Clinical and Biomedical Research (IJCBR)No ratings yet
- Neurohistiocytosis: Two Cases of A Rare DiseaseDocument8 pagesNeurohistiocytosis: Two Cases of A Rare DiseaseIJAR JOURNALNo ratings yet
- Extra Renal Rhabdoid Tumor in An Adult Presentin 2024 International JournalDocument5 pagesExtra Renal Rhabdoid Tumor in An Adult Presentin 2024 International JournalRonald QuezadaNo ratings yet
- 1 Neurosurgery Cases and ReviewsDocument5 pages1 Neurosurgery Cases and ReviewsintodoieblissNo ratings yet
- 1109 Case 2Document4 pages1109 Case 2willygopeNo ratings yet
- UntitledDocument13 pagesUntitleddpcamposhNo ratings yet
- Ctoij MS Id 555925Document8 pagesCtoij MS Id 555925lucasnegromonte0001No ratings yet
- Raval PDFDocument5 pagesRaval PDFdebby claudiNo ratings yet
- Kimura DiseaseDocument4 pagesKimura DiseasewitariNo ratings yet
- Cerebellar Hemangioblastoma-A Rare EntityDocument10 pagesCerebellar Hemangioblastoma-A Rare EntityJay LeheriNo ratings yet
- Orbital Pathology: W. Müller-Forell, S. PitzDocument38 pagesOrbital Pathology: W. Müller-Forell, S. PitzArif Rahman WardhaniNo ratings yet
- Tumefactive Demyelinating Lesions: Nine Cases and A Review of The LiteratureDocument9 pagesTumefactive Demyelinating Lesions: Nine Cases and A Review of The LiteraturePS NeuroNo ratings yet
- A Case Report of Eruptive Syringoma: Clinical, Dermoscopic and Histological FeaturesDocument5 pagesA Case Report of Eruptive Syringoma: Clinical, Dermoscopic and Histological FeaturesIJAR JOURNALNo ratings yet
- Medi 101 E28665Document5 pagesMedi 101 E28665S Francisco MotNo ratings yet
- Brain Imaging in Colloid CystDocument5 pagesBrain Imaging in Colloid CystMohamed Farouk El-FaresyNo ratings yet
- Merkel Cell Carcinoma: A Case ReportDocument6 pagesMerkel Cell Carcinoma: A Case ReportIJAR JOURNALNo ratings yet
- Jhua16000143 PDFDocument3 pagesJhua16000143 PDFsamiratumananNo ratings yet
- AsianJNeurosurg102126-4310714 115827 PDFDocument3 pagesAsianJNeurosurg102126-4310714 115827 PDFSucipto HartonoNo ratings yet
- Tum DemDocument2 pagesTum DemKota AnuroopNo ratings yet
- Vertebral Hydatidosis: Unusual Cause of Medullary CompressionDocument4 pagesVertebral Hydatidosis: Unusual Cause of Medullary CompressionIJAR JOURNALNo ratings yet
- TJN 44370 Images in Clinical Neurology Aggarwal (A)Document3 pagesTJN 44370 Images in Clinical Neurology Aggarwal (A)VisshwajeetNo ratings yet
- 0909 Case 2Document2 pages0909 Case 2willygopeNo ratings yet
- 18 Extra-GuptaNDocument3 pages18 Extra-GuptaNGalih rarang gatiNo ratings yet
- Spectrum of Mri Findings in Pediatric Epilepsy Medical and Surgical Causes of Epilepsy in Children and Its Radiological CorrelatioDocument4 pagesSpectrum of Mri Findings in Pediatric Epilepsy Medical and Surgical Causes of Epilepsy in Children and Its Radiological CorrelatioImroatul hafidzahNo ratings yet
- Radio Logical Finding PCNSLDocument12 pagesRadio Logical Finding PCNSLKhushalchand KanjiNo ratings yet
- Collagenous Fibroma (Desmoplastic Fibroblastoma) : Clinical, Pathological and Imaging FindingsDocument41 pagesCollagenous Fibroma (Desmoplastic Fibroblastoma) : Clinical, Pathological and Imaging FindingsAnonymous bE4VegCcNo ratings yet
- Abdominal Wall Extraskeletal Ewing Sarcoma - Case ReportDocument3 pagesAbdominal Wall Extraskeletal Ewing Sarcoma - Case ReportInternational Organization of Scientific Research (IOSR)No ratings yet
- J Surneu 2007 07 059Document4 pagesJ Surneu 2007 07 059lucasnegromonte0001No ratings yet
- Giant Solitary Cutaneous Angiosarcoma of The Forearm Occurring Outside The Setting of LymphedemaDocument5 pagesGiant Solitary Cutaneous Angiosarcoma of The Forearm Occurring Outside The Setting of LymphedemaIJAR JOURNALNo ratings yet
- 1208 Case 1Document2 pages1208 Case 1willygopeNo ratings yet
- Brainstem CysticercoseDocument4 pagesBrainstem CysticercoseDr. R. SANKAR CITNo ratings yet
- Acute Dorsal Myelopathy Resulting From Intramedullary Cysticercus: A Case ReportDocument5 pagesAcute Dorsal Myelopathy Resulting From Intramedullary Cysticercus: A Case ReportElison J PanggaloNo ratings yet
- Laryngeal Plasmacytoma in Kahlers Disease: A Case ReportDocument6 pagesLaryngeal Plasmacytoma in Kahlers Disease: A Case ReportIJAR JOURNALNo ratings yet
- Vol-1, Issue-1 Prospective Study of Peripheral Nerve Tumors Over A Period of 2 YearsDocument4 pagesVol-1, Issue-1 Prospective Study of Peripheral Nerve Tumors Over A Period of 2 YearsijhrmimsNo ratings yet
- Krabbe DiseaseDocument6 pagesKrabbe DiseaseUrko GoroquietaNo ratings yet
- Cureus 0012 00000008855 PDFDocument11 pagesCureus 0012 00000008855 PDFAlberto BrahmNo ratings yet
- Dupuytren's Disease: Sharon Dickmann, PT, CHTDocument18 pagesDupuytren's Disease: Sharon Dickmann, PT, CHTBogdan TudorNo ratings yet
- Imaging Findings of Intraventricular and Ependymal LesionsDocument16 pagesImaging Findings of Intraventricular and Ependymal Lesionsanggi abNo ratings yet
- PosterDocument1 pagePosterRaif RizqullahNo ratings yet
- PROCEEDINGS OF THE PAEDlATRlC NEURO-ONCOLOGY TUMOUR BOARDDocument9 pagesPROCEEDINGS OF THE PAEDlATRlC NEURO-ONCOLOGY TUMOUR BOARDfriiday.qNo ratings yet
- 1009 Case 2Document4 pages1009 Case 2willygopeNo ratings yet
- Extragenital Lichen Sclerosus Et Atrophicus: A Case ReportDocument3 pagesExtragenital Lichen Sclerosus Et Atrophicus: A Case ReportIJAR JOURNALNo ratings yet
- Epithelioid Hemangioendothelioma of The Infundibular-Hypothalamic Region: Case Report and Literature ReviewDocument6 pagesEpithelioid Hemangioendothelioma of The Infundibular-Hypothalamic Region: Case Report and Literature ReviewcarlosNo ratings yet
- Tuberculoma of the Brain: Rare Case of Multiple Lesions and Meningeal PlaquesDocument9 pagesTuberculoma of the Brain: Rare Case of Multiple Lesions and Meningeal PlaquessanatthhNo ratings yet
- Hon 2005Document2 pagesHon 2005Andana TrisaviNo ratings yet
- Abstract: Kimura Disease Is A Rare Form of Chronic Inflammatory Disorder InvolvingDocument4 pagesAbstract: Kimura Disease Is A Rare Form of Chronic Inflammatory Disorder InvolvingpriyokNo ratings yet
- EsclerodermiaDocument15 pagesEsclerodermiaIvette Andrea HQNo ratings yet
- Anaplastic Large Cell Lymphoma Alk Negative of The Mandible As The First Clinical Manifestation of Acquired Immunodeficiency SyndromeDocument5 pagesAnaplastic Large Cell Lymphoma Alk Negative of The Mandible As The First Clinical Manifestation of Acquired Immunodeficiency SyndromeIJAR JOURNALNo ratings yet
- Bulbo-Medullary Ependymoma in An Adult: Case ReportDocument6 pagesBulbo-Medullary Ependymoma in An Adult: Case ReportIJAR JOURNALNo ratings yet
- Diastematomyelia: A Case Report With Review of LiteratureDocument4 pagesDiastematomyelia: A Case Report With Review of LiteraturePasupulati GnaneshwarNo ratings yet
- Extra Cranial MetastasesDocument5 pagesExtra Cranial MetastasesJayendra Kumar AryaNo ratings yet
- EPIDURIALDocument3 pagesEPIDURIALALBERTO URIEL MONTAÑO CERVANTESNo ratings yet
- 2020 - Jie Wei - Criptococoma Imitando Una Enfermedad DesmielinizanteDocument4 pages2020 - Jie Wei - Criptococoma Imitando Una Enfermedad DesmielinizanteEduardo RodriguezNo ratings yet
- Chapter 2Document11 pagesChapter 2fiskiyeyikimkirdi06No ratings yet
- Primary Intracranial Leiomyoma: A Case Report and Literature ReviewDocument3 pagesPrimary Intracranial Leiomyoma: A Case Report and Literature ReviewcandiddreamsNo ratings yet
- International Journal of Surgery Case ReportsDocument3 pagesInternational Journal of Surgery Case ReportsYipno Wanhar El MawardiNo ratings yet
- Survey For The Expression Levels of Drought Tolerant Genes in Cassava Varieties in TanzaniaDocument15 pagesSurvey For The Expression Levels of Drought Tolerant Genes in Cassava Varieties in TanzaniaajmrdNo ratings yet
- Models Regulation of Room Microclimate Parameters Storage of Agricultural ProductsDocument9 pagesModels Regulation of Room Microclimate Parameters Storage of Agricultural ProductsajmrdNo ratings yet
- The Influence of Leadership, Supervision and Organizational Climate of Madrasas On Students' Extracurricular Achievements State Aliyah Madrasah in Jambi ProvinceDocument18 pagesThe Influence of Leadership, Supervision and Organizational Climate of Madrasas On Students' Extracurricular Achievements State Aliyah Madrasah in Jambi ProvinceajmrdNo ratings yet
- The Effect of Solfège Syllable Indications On Sight-Reading Skills of Undergraduate Music MajorsDocument6 pagesThe Effect of Solfège Syllable Indications On Sight-Reading Skills of Undergraduate Music Majorsajmrd100% (1)
- Singing The Songs: Towards Elder S.K. Ampiah's Lyrical IntentDocument9 pagesSinging The Songs: Towards Elder S.K. Ampiah's Lyrical IntentajmrdNo ratings yet
- Impact of Trade On Employment and Wages in The Manufacturing Industry Considering The Heterogeneous Character of Workers: The Case of Sri LankaDocument16 pagesImpact of Trade On Employment and Wages in The Manufacturing Industry Considering The Heterogeneous Character of Workers: The Case of Sri LankaajmrdNo ratings yet
- Developing Civic Education E-Module Based On Project Based Learning To Improve Students in Civic LiteracyDocument6 pagesDeveloping Civic Education E-Module Based On Project Based Learning To Improve Students in Civic LiteracyajmrdNo ratings yet
- Understanding Different Models of Adult Learning: The Australia Residency Education Extension Immersion Case StudyDocument5 pagesUnderstanding Different Models of Adult Learning: The Australia Residency Education Extension Immersion Case StudyajmrdNo ratings yet
- Lahai Koroma, L.M. Kamara Andronnie Freezer-WilliamsDocument11 pagesLahai Koroma, L.M. Kamara Andronnie Freezer-WilliamsajmrdNo ratings yet
- A Brief Empirical Analysis of United States Marine Corps Commissioning Program EffectivenessDocument4 pagesA Brief Empirical Analysis of United States Marine Corps Commissioning Program EffectivenessajmrdNo ratings yet
- Real-Time and Automated Flood Detection &early Warning Systems For The Municipality of San Leonardo, Nueva Ecija: A Case StudyDocument11 pagesReal-Time and Automated Flood Detection &early Warning Systems For The Municipality of San Leonardo, Nueva Ecija: A Case StudyajmrdNo ratings yet
- The Impact of Environmental Regulation On Industrial Structure Upgrading - Based On Panel Threshold EvidenceDocument15 pagesThe Impact of Environmental Regulation On Industrial Structure Upgrading - Based On Panel Threshold EvidenceajmrdNo ratings yet
- Adaptogens: New Age Healing Gems For Physical Wellbeing: Rehaan Sharma, Pawan Sharma, Renu BhardwajDocument10 pagesAdaptogens: New Age Healing Gems For Physical Wellbeing: Rehaan Sharma, Pawan Sharma, Renu BhardwajajmrdNo ratings yet
- Vermicompost and Biourine Doses Effect On Soil PH, Shallot Growth, and Yield in UltisolDocument10 pagesVermicompost and Biourine Doses Effect On Soil PH, Shallot Growth, and Yield in UltisolajmrdNo ratings yet
- The Perception of Hospital Stakeholders On Cardiacintervention Based On The Theory of Consumer Perceived Value Indonesia CaseDocument6 pagesThe Perception of Hospital Stakeholders On Cardiacintervention Based On The Theory of Consumer Perceived Value Indonesia CaseajmrdNo ratings yet
- Sci-Art: Visual Art Approach in Astronomy of Teacher Education StudentsDocument8 pagesSci-Art: Visual Art Approach in Astronomy of Teacher Education StudentsajmrdNo ratings yet
- Pharaoh Tutankhamun, Queen Tawananna III and King Jian Jia Saw The Extremely Bright Supernova 1355 BCDocument21 pagesPharaoh Tutankhamun, Queen Tawananna III and King Jian Jia Saw The Extremely Bright Supernova 1355 BCajmrdNo ratings yet
- The Effect of Return On Assets, Debt To Equity Ratio and Current Ratio On Earning Per Share (Study On LQ45 Index Banking Group Companies Listed On The Indonesia Stock Exchange 2015-2019)Document8 pagesThe Effect of Return On Assets, Debt To Equity Ratio and Current Ratio On Earning Per Share (Study On LQ45 Index Banking Group Companies Listed On The Indonesia Stock Exchange 2015-2019)ajmrdNo ratings yet
- Physical Activity Level and Its Correlationwith Quality of Life Among Undergraduates in University of Peradeniya During Covid-19 PandemicDocument8 pagesPhysical Activity Level and Its Correlationwith Quality of Life Among Undergraduates in University of Peradeniya During Covid-19 PandemicajmrdNo ratings yet
- Value Added Tax and Economic Growth in NIGERIA 2004-2018Document5 pagesValue Added Tax and Economic Growth in NIGERIA 2004-2018ajmrdNo ratings yet
- Examining The Relationship Between Corporate Social Responsibility (CSR) and Competitive Advantage (CA) in The Commercial Banking Sector /case Study of JordanDocument5 pagesExamining The Relationship Between Corporate Social Responsibility (CSR) and Competitive Advantage (CA) in The Commercial Banking Sector /case Study of JordanajmrdNo ratings yet
- The Growth and Yield of Sweet Corn As Affected by Palm-Oil Sludge and Liquid Organic FertilizerDocument6 pagesThe Growth and Yield of Sweet Corn As Affected by Palm-Oil Sludge and Liquid Organic FertilizerajmrdNo ratings yet
- Socio-Economic Issues of Urban Small-Scale Fisherfolks in Cagayan de Oro City, PhilippinesDocument6 pagesSocio-Economic Issues of Urban Small-Scale Fisherfolks in Cagayan de Oro City, PhilippinesajmrdNo ratings yet
- Employability of Tesda Scholars Graduates: A Tracer Study: Manie Rose D. Duaman, Fely A. Habla, Ed.DDocument4 pagesEmployability of Tesda Scholars Graduates: A Tracer Study: Manie Rose D. Duaman, Fely A. Habla, Ed.DajmrdNo ratings yet
- Climate Change Global Warming Effects and Implications in Warri, NigeriaDocument14 pagesClimate Change Global Warming Effects and Implications in Warri, NigeriaajmrdNo ratings yet
- Audience Perception of TVC News Coverage of Buhari'S War Against Corruption in NigeriaDocument9 pagesAudience Perception of TVC News Coverage of Buhari'S War Against Corruption in NigeriaajmrdNo ratings yet
- Artris Feronika Korompot, Sri Setya HandayaniDocument12 pagesArtris Feronika Korompot, Sri Setya HandayaniajmrdNo ratings yet
- Anti-Domination Number of A Graph: MallikarjunbasannakattimaniDocument5 pagesAnti-Domination Number of A Graph: MallikarjunbasannakattimaniajmrdNo ratings yet
- The Sonic Brain: A Musical Subculture in Akropong School For The Blind, GhanaDocument8 pagesThe Sonic Brain: A Musical Subculture in Akropong School For The Blind, GhanaajmrdNo ratings yet
- Prince or Shoemaker: Jian GaoDocument9 pagesPrince or Shoemaker: Jian GaoajmrdNo ratings yet
- Nikon Nivo C Series Instruction ManualDocument65 pagesNikon Nivo C Series Instruction ManualBambang Deriyanto100% (1)
- Medical Power PointDocument124 pagesMedical Power PointPhysiology by Dr Raghuveer75% (4)
- THE LIVING MATRIX: A MODEL FOR THE PRIMARTY RESPIRATORY MECHANISMDocument69 pagesTHE LIVING MATRIX: A MODEL FOR THE PRIMARTY RESPIRATORY MECHANISMRukaphuongNo ratings yet
- India TodayDocument76 pagesIndia TodaySanket RaveendraNo ratings yet
- 0972 June 2021 QP 41 Cie Igcse Physics - Pdfquestion7Document2 pages0972 June 2021 QP 41 Cie Igcse Physics - Pdfquestion7Kareem YouakimNo ratings yet
- Validity and ReliabilityDocument13 pagesValidity and ReliabilityZarnigar AltafNo ratings yet
- 0210 Pop Labels BSDocument1 page0210 Pop Labels BSThe London Free PressNo ratings yet
- SpaceX ProposalDocument6 pagesSpaceX ProposalTexas WatchdogNo ratings yet
- Animal Names in English and Telugu - 20170912 - 182216545Document17 pagesAnimal Names in English and Telugu - 20170912 - 182216545karimulla goraNo ratings yet
- Ecosystem Components and InteractionsDocument31 pagesEcosystem Components and InteractionsBirraa TajuNo ratings yet
- Cost Control ReviewerDocument13 pagesCost Control ReviewerMatthew Ivan HerreraNo ratings yet
- School and CentreDocument24 pagesSchool and CentreThrilling PrinceNo ratings yet
- Oil Record Book InstructionsDocument6 pagesOil Record Book InstructionsNamal Fernando100% (1)
- Individual Differences and Personality in "Ugly Betty", S01E01Document6 pagesIndividual Differences and Personality in "Ugly Betty", S01E01Starling HunterNo ratings yet
- 4140DE Data SheetDocument1 page4140DE Data SheetNabeel AmeerNo ratings yet
- 2009 IECC Residential Code Requirements Apr 14 Draft InspectorsDocument4 pages2009 IECC Residential Code Requirements Apr 14 Draft Inspectorsbcap-oceanNo ratings yet
- MYK Grout Card 2Document2 pagesMYK Grout Card 2Abdul Raheem SyedNo ratings yet
- Vrs PresentationDocument24 pagesVrs PresentationshrutipalkarNo ratings yet
- What Is A PronounDocument9 pagesWhat Is A PronounFanera JefferyNo ratings yet
- Duarte Et Al - Resin CementsDocument28 pagesDuarte Et Al - Resin Cementsjfrascarolo100% (4)
- Jear C PB 2018 PDFDocument174 pagesJear C PB 2018 PDFArasu RajendranNo ratings yet
- Jadwal Oral Presentation Peserta FIT-VIIIDocument26 pagesJadwal Oral Presentation Peserta FIT-VIIIKlinik FellitaNo ratings yet
- Chapter III Pharmacokinetics: Durge Raj GhalanDocument64 pagesChapter III Pharmacokinetics: Durge Raj GhalanDurge Raj Ghalan100% (3)
- Mind Power SecretsDocument38 pagesMind Power SecretsIan Faian92% (52)
- 20090716FoxReiki PDFDocument40 pages20090716FoxReiki PDFAgustina RomeroNo ratings yet
- Silver Rain Svetlana Perevalova PDFDocument9 pagesSilver Rain Svetlana Perevalova PDFAndrea Koumarian100% (1)
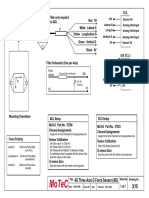
- Filter and wiring schematic for 3-axis ADL G-force sensorDocument1 pageFilter and wiring schematic for 3-axis ADL G-force sensorJuan Ramón Pérez LorenzoNo ratings yet