Professional Documents
Culture Documents
Osteoarthritis and Rheumatoid Arthritis in Practice
Uploaded by
Waseem Khan AfridiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Osteoarthritis and Rheumatoid Arthritis in Practice
Uploaded by
Waseem Khan AfridiCopyright:
Available Formats
lOMoARcPSD|845420
Osteoarthritis AND Rheumatoid Arthritis IN Practice
Applied Practice (University of Sunderland)
StuDocu is not sponsored or endorsed by any college or university
Downloaded by Waseem Afridi (cadetwaseem@hotmail.com)
lOMoARcPSD|845420
OSTEOARTHRITIS AND RHEUMATOID ARTHRITIS IN PRACTICE
Osteoarthritis Rheumatoid Arthritis
Characterised by loss of articular Chronic, progressive, systemic
cartilage and formation of new bone at inflammatory disorder principally
joint margins (osteophytes) affecting synovial joints
Commonly involves knee, hips, small Commonly involves hands, wrists,
hand joints, neck and lower back ankles and toes
Systemic disease Local joint destruction
Osteoarthritis
Risk Factors:
- Increasing age
- Female sex
- Family history (genetic factors)
- Congenital joint abnormalities
- Joint injury
- Prolonged overuse
- Occupation
- Obesity
- Disease that alter normal structure and function of joints e.g. RA, gout
Non-Pharmacological Management:
- Lifestyle e.g. weight loss, exercise, balance activity/rest
- Hot/cold therapies
- Physiotherapy
- Aids/devices e.g. braces, joint supports, insoles, TENS
- Surgery
Pharmacological Management i.e. optimal pain control:
- Paracetamol (first line) – take regularly
- Topical NSAID ahead of oral NSAIDs, COX2 inhibitors or opioids:
Topical NSAID first line then
Ibuprofen 400mg TDS (lowest CV and GI risk) then
Diclofenac/Naproxen (CV vs GI risk)
N.B. consider renal function and other medications patient is on
Co-prescribe PPI
- Adjunctive therapies:
Topical capsaicin for knee and hand OA
Intra-articular steroids for moderate-severe pain
- Do not offer glucosamine, chondroitin or intra-articular hyaluronan injections
Downloaded by Waseem Afridi (cadetwaseem@hotmail.com)
lOMoARcPSD|845420
Rheumatoid Arthritis
Management of Associated Conditions:
Sjörgrens syndrome
- Lubricating eye drops/ointments
- Artificial saliva replacement
Vasculitis
- Steroids
- Cyclophosphamide
Increased cardiovascular risk
- Assessment e.g. QRISK and appropriate medication initiation
Increased osteoporosis risk
- Assessment e.g. FRAX (+/- DXA) and appropriate medication initiation
RA can result in physical disability – help patients manage this via:
- Easy to open containers
- Supportive cutters
- Occupation therapists (support patients to maintain independent living)
General Advice - Vaccinations:
Immunosuppressive therapy e.g. leflunomide, methotrexate, biologics more likely to
suffer clinically significant infections
- Flu, pneumococcal recommended
- Avoid live vaccines (give 2-4 weeks before starting immunosuppressive where
possible)
Downloaded by Waseem Afridi (cadetwaseem@hotmail.com)
lOMoARcPSD|845420
- Avoid contact with chicken pox/shingles/measles
- Ensure household contacts immune to measles: offer MMR
- Significant contact with chicken pox: VZ immunoglobulin can be given within 7
days of contact
- Measles: urgent measles IgG testing
For biologics, reactivation of latent TB is a particular concern; all patients should be
screened before commencing therapy
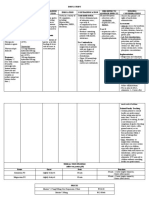
Initial Pharmacological Treatment
- Monotherapy (ASAP)
- Oral MTX, leflunomide or sulfasalazine (Hydroxychloroquine alternative)
- Consider bridging treatment with oral/IM/IA glucocorticoids with initiating
DMARD
If target (ideally remission or low disease activity) not reached, increase dose.
Still not sufficient, add second DMARD.
Inadequate response to conventional DMARDs: biologics (or JAK inhibitors) in
combination with MTX
General Points regarding DMARDs:
- Not analgesics, take weeks/months to work
- Most have a significant side effect profile
- Regular blood tests
- Patient counselling of recognition and awareness of signs/symptoms of
serious adverse effects
- Infections: if patient has an infection that requires antibiotic,
immunosuppressive agents (e.g. MTX) usually stopping until infection has
cleared
- Pregnancy: MTX and Leflunomide are C/I, AZA and Hydroxychloroquine –
benefit outweighs risk if these are used
MTX and NSAIDs:
- NSAIDs reduce renal excretion of MTX therefore increased risk of toxicity
- Avoid inappropriate clinical use of NSAIDs e.g. post-surgical pain relief, OTC/
self-medication
- Benefit may outweigh risk for RA pain control; some patients find it difficult to
manage without therefore commonly used for THIS indication in practice
- Monitoring of bloods and awareness of signs/symptoms of
haem/liver/pulmonary toxicity
MTX Counselling
Seek medical attention (same day):
- Unexplained shortness of breath and dry cough (can occur gradually or over a
few days)
Downloaded by Waseem Afridi (cadetwaseem@hotmail.com)
lOMoARcPSD|845420
- If whites of eyes become yellow or you develop severe itching
- You have fever, chills or severe sore throat/mouth
- You have severe mouth ulcers, bleeding gums, bruising or skin ulcers
- You experience severe sickness or upset stomach
- If you have never had chickenpox and come into close contact with someone
who has chickenpox or shingles
- You think you/your partner have become pregnant whilst on treatment
MTX Rescue Therapy
- Acute toxicity with MTX may require folinic acid (given as calcium folinate)
rescue therapy
- Folinic acid counteracts anti-folate activity of MTX, speeds recovery of
myelosuppression/mucositis etc.
- Granulocyte-colony stimulating factors (G-CSF) e.g. SC filgrastim may be
considered if severe neutropenia (specialist)
- Fluid & electrolyte balance, blood products etc.
Leflunomide
- Dose: 100mg OD for 3 days then 10-20mg OD (most patients do not get
loading dose as poorly tolerated
- C/I in liver impairment or hypoproteinaemia
- Monitoring: blood tests, BP and weight monitoring
- Interactions: increased risk of toxicity with MTX, caution with phenytoin,
warfarin and tolbutamide
Downloaded by Waseem Afridi (cadetwaseem@hotmail.com)
lOMoARcPSD|845420
Leflunomide Wash-out
- In case of serious event or before conception
- Colestyramine 8mg TDS for 11 days (or activated charcoal 50g QDS for 11
days)
- Can measure concentration of active metabolite (should be < 20 microg/L on
two occasions, two weeks apart)
Hydroxychloroquine
- Dose: 200mg OD or BD (depending on weight – max 6.5mg/kg IBW)
- Side effects: GI disturbances, headache, skin reactions, ocular disturbances
- Caution in epilepsy, severe GI disorders, may exacerbate psoriasis
- Assess renal/liver function before therapy but no routine blood monitoring
(unlike other DMARDS)
- Visual acuity tested annually; referral to ophthalmologist if any ocular
problems occur e.g. reduced vision
- Interactions: amiodarone, moxifloxacin (increased risk ventricular arrthymias),
digoxin (increased dig level), ciclosporin (increased ciclo levels), some
antimalarials
Sulfasalazine
- Dose: 500mg OD 7/7, 500mg BD 7/7, 1g OM and 500mg ON 7/7, 1g BD (can
go up to 3g OD if needed)
- Usually EC, take with water, swallow whole
- Can turn urine and tears orange coloured and soft contact lenses can be
stained yellow
- Side effects: nausea, diarrhoea, stomach upset, dizziness, headache, skin
rash
- Bloods: FBC, LFTs, U&E – regularly in first two years
- Haematological/liver toxicity: report unexplained cough, breathlessness,
abnormal bruising/bleeding, severe sore throat, severe
nausea/dizziness/headache, unexplained acute widespread rash, oral
ulceration
Steroids
- May be used to bridge therapy during flare (but reduce/stop where possible)
- Reduces inflammation, suppresses symptoms
- Oral: prednisolone OM CC
- Steroid injection (IM/IA): not given more often than once per year
- Long term risks:
Osteoporosis
Diabetes
Weight gain
Fluid retention
High BP
Stomach ulcer (infection risk)
Downloaded by Waseem Afridi (cadetwaseem@hotmail.com)
lOMoARcPSD|845420
Biologics
Anti-TNF drugs:
- Adalimumab (SC), Etanercept (SC), certolizumab pegol (SC), golimumab
(SC)
- Infliximab (IV), Others
Others
- Rituximab (IV), tocilizumab (IV), abatacept (IV/SC), sarilumab (SC)
- Anakinra (SC- not recommended unless part of a clinical trial)
N.B. most SC products delivered to patients via Homecare service for injection at
home, IV infusions usually given hospital day unit
- Not painkiller
- Use anti-TNFs in combination with MTX; if intolerant of MTX, some can be
used as monotherapy
- Side effects: infection risk, often withheld for surgery (2 weeks before and
after), reactivation of TB is a concern (screen all patient before initiation)
Biosimilars
- Exists for infliximab, etanercept, rituximab and adalimumab (2018)
- Cost saving, increasing use
- Similar to existing biologics but not exactly the same (large molecules so note
that even within biologic batches there will be some variation)
- NICE guidance applies to biosimilars that have a MA allowing the use of the
biosimilar for the same indication
JAK inhibitors
- Oral immunomodulatory drugs
- E.g. Tofacitinib, Baricitinib
- Can be used according to NICE guidance if severe disease activity if criteria
met
- Withdraw after 6 months if insufficient benefit
Downloaded by Waseem Afridi (cadetwaseem@hotmail.com)
You might also like
- Management of Gout in AdultsDocument3 pagesManagement of Gout in AdultsZubair Mahmood KamalNo ratings yet
- Assignment in Pharma Agasbsn2-ADocument4 pagesAssignment in Pharma Agasbsn2-AMahdiyah AgasNo ratings yet
- Osteoarthritis Learning Objectives PDFDocument8 pagesOsteoarthritis Learning Objectives PDFWaseem Khan AfridiNo ratings yet
- Solu-Cortef (Hydrocortisone)Document3 pagesSolu-Cortef (Hydrocortisone)E100% (2)
- Case 2Document7 pagesCase 2Vineth MartinNo ratings yet
- Ra OaDocument44 pagesRa OaAgustiantyNo ratings yet
- Farmakologi KortikosteroidDocument41 pagesFarmakologi Kortikosteroiddebbyelvira100% (1)
- Rheumatic Heart DDocument12 pagesRheumatic Heart DHein HtetNo ratings yet
- Osteoarthritis: Degenerative Joint Disease - Prevalensi Meningkat Seiring DG Usia, Meningkat 2-10x DR Usia 30-65 THDocument58 pagesOsteoarthritis: Degenerative Joint Disease - Prevalensi Meningkat Seiring DG Usia, Meningkat 2-10x DR Usia 30-65 THbrevmanaNo ratings yet
- PHARM CARE PD SLE NewDocument58 pagesPHARM CARE PD SLE NewbrevmanaNo ratings yet
- Management of Rheumatoid ArthritisDocument48 pagesManagement of Rheumatoid ArthritisAlexNo ratings yet
- SR 3Document30 pagesSR 3hussein alnasryNo ratings yet
- Pharmacology HESI Study Guide 2013Document16 pagesPharmacology HESI Study Guide 2013naijababy89100% (12)
- Management of HyperuricemiaDocument23 pagesManagement of HyperuricemiaSoad ShedeedNo ratings yet
- Icu Drug StudyDocument23 pagesIcu Drug StudyApril LebrilloNo ratings yet
- Musculoskeletal Drugs 2020Document34 pagesMusculoskeletal Drugs 2020Anna Lin YeeNo ratings yet
- MedSurg Medication Study Guide Test 1Document12 pagesMedSurg Medication Study Guide Test 1Sarah PlunkettNo ratings yet
- Farmakoterapi Gout and HipeurisemiaDocument54 pagesFarmakoterapi Gout and HipeurisemiaIrvan Firmansyah Adi SutrisnoNo ratings yet
- Disease Study: A. Myasthenia GravisDocument6 pagesDisease Study: A. Myasthenia GravisMark Lemuel AbadaNo ratings yet
- Czarina Drug Study JuneDocument20 pagesCzarina Drug Study JuneNicoh AvilaNo ratings yet
- DR - Girish Meravanige College of Medicine, KFUDocument28 pagesDR - Girish Meravanige College of Medicine, KFUNOT ZUXNo ratings yet
- PARACETAMOLDocument2 pagesPARACETAMOLMonica JubaneNo ratings yet
- Toxic Effects of DrugsDocument6 pagesToxic Effects of DrugsBern NerquitNo ratings yet
- Overview and Recommendations: BackgroundDocument46 pagesOverview and Recommendations: BackgroundRubén Casas BenítezNo ratings yet
- Pharmacology: By: Jan Michael Khalid L. Macarambon, RNDocument164 pagesPharmacology: By: Jan Michael Khalid L. Macarambon, RNJan MacarambonNo ratings yet
- Medication Work Sheet For MedSurgDocument5 pagesMedication Work Sheet For MedSurgRyanMitchell100% (2)
- Dexamethasonetab PDFDocument8 pagesDexamethasonetab PDFFaizaNadeemNo ratings yet
- Dental MedicineDocument59 pagesDental Medicinechh56k6tndNo ratings yet
- Hydralazine 1Document3 pagesHydralazine 1BrittanyNo ratings yet
- Seminar On DMARDSDocument57 pagesSeminar On DMARDSusamadaifallahNo ratings yet
- Clinical PharmacyDocument4 pagesClinical PharmacysadiaNo ratings yet
- Gout and HyperuricemiaDocument35 pagesGout and HyperuricemiaMarwan KurdishNo ratings yet
- 2023 MSSDocument34 pages2023 MSSmerga wekwayaNo ratings yet
- Definitions OF DiagnosisDocument25 pagesDefinitions OF DiagnosisGlaire ZarateNo ratings yet
- INDOMETACINDocument5 pagesINDOMETACINteslimolakunlerajiNo ratings yet
- PEDIADRUGDocument6 pagesPEDIADRUGPatrice LimNo ratings yet
- Pharm RemediationDocument5 pagesPharm RemediationAudrey WatsonNo ratings yet
- GOUT PresentationDocument24 pagesGOUT Presentationtasneemsofi100% (1)
- (Brand Name) : Generic Name Classificati ON Indications Side Effects Nursing ResponsibilitiesDocument5 pages(Brand Name) : Generic Name Classificati ON Indications Side Effects Nursing ResponsibilitiesMeriam Angelita Robles AlfaroNo ratings yet
- Lect 7Document30 pagesLect 7eslambasuony98No ratings yet
- 1 Osteo and Rheumatoid ArthritisDocument62 pages1 Osteo and Rheumatoid ArthritisIbrahim BarhamNo ratings yet
- Infections AntibioticsDocument4 pagesInfections AntibioticsMatthieu FortinNo ratings yet
- Drug Monograph AssignmentDocument5 pagesDrug Monograph AssignmentAdam BannonNo ratings yet
- Medication Card CelebrexDocument2 pagesMedication Card CelebrexTSPAN100% (1)
- Drug StudyDocument9 pagesDrug StudyAlexander Chavez Alto100% (1)
- Crystal Induced Arthropathies: BY: DR Mehrunnisa Umar Assisstant Profesor Department of MedicineDocument25 pagesCrystal Induced Arthropathies: BY: DR Mehrunnisa Umar Assisstant Profesor Department of MedicinedrusmanjamilhcmdNo ratings yet
- Drug Study TramadolDocument14 pagesDrug Study TramadolBianca Freya Porral85% (13)
- Steroids in DentistryDocument4 pagesSteroids in DentistryrazasiddiqueNo ratings yet
- Problems With Chemotherapy of Lymphoma - How To Cope - WSAVA2008 - VINDocument5 pagesProblems With Chemotherapy of Lymphoma - How To Cope - WSAVA2008 - VINAridai RJNo ratings yet
- 07 - 10 - 21 Treatment of Covid 19 InfectionDocument26 pages07 - 10 - 21 Treatment of Covid 19 InfectionStonefalconNo ratings yet
- Drug Study ArvinDocument6 pagesDrug Study ArvinArvin BeltranNo ratings yet
- Infectious Disese & IntegumentaryDocument11 pagesInfectious Disese & IntegumentaryJayvee Montoya-PujanteNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Comprehensive Treatment of Knee Osteoarthritis: Recent AdvancesFrom EverandComprehensive Treatment of Knee Osteoarthritis: Recent AdvancesNo ratings yet
- Oestoarthritis Oestoarthritis: Physiotherapy (Cardiff University) Physiotherapy (Cardiff University)Document3 pagesOestoarthritis Oestoarthritis: Physiotherapy (Cardiff University) Physiotherapy (Cardiff University)Waseem Khan AfridiNo ratings yet
- Osteoarthritis Summary Pathophysiology PDFDocument5 pagesOsteoarthritis Summary Pathophysiology PDFWaseem Khan AfridiNo ratings yet
- Osteogenesis Imperfecta: by DR - Naveed Khan Mphil Scholar Oral PathologyDocument20 pagesOsteogenesis Imperfecta: by DR - Naveed Khan Mphil Scholar Oral PathologyWaseem Khan Afridi100% (1)
- Chapter 2. Acute and Chronic InflammationDocument6 pagesChapter 2. Acute and Chronic InflammationWaseem Khan AfridiNo ratings yet
- Comparison of Rheumatoid and OsteoarthritisDocument4 pagesComparison of Rheumatoid and OsteoarthritisWaseem Khan AfridiNo ratings yet
- Osteoarthritis Clinical Pattern Sheet PDFDocument5 pagesOsteoarthritis Clinical Pattern Sheet PDFWaseem Khan AfridiNo ratings yet
- Pathology: Osteoarthritis Pathology: OsteoarthritisDocument4 pagesPathology: Osteoarthritis Pathology: OsteoarthritisWaseem Khan AfridiNo ratings yet
- Disease Summary: Osteoarthritis Disease Summary: OsteoarthritisDocument3 pagesDisease Summary: Osteoarthritis Disease Summary: OsteoarthritisWaseem Khan AfridiNo ratings yet
- Discussion Osteoarthritis Discussion OsteoarthritisDocument3 pagesDiscussion Osteoarthritis Discussion OsteoarthritisWaseem Khan AfridiNo ratings yet
- Dental CariesDocument32 pagesDental CariesWaseem Khan AfridiNo ratings yet
- OsteoarthritisDocument7 pagesOsteoarthritisWaseem Khan AfridiNo ratings yet
- In Vitro in Vivo Correlation 4Document31 pagesIn Vitro in Vivo Correlation 4GANESH KUMAR JELLANo ratings yet
- MAALOX (Drug Study)Document3 pagesMAALOX (Drug Study)Kian HerreraNo ratings yet
- Cardiac Pharmacology WorkbookDocument5 pagesCardiac Pharmacology WorkbookPhotios ZervasNo ratings yet
- Form Stok OpnameDocument5 pagesForm Stok OpnameSsagitaNo ratings yet
- Practice Bullet In: Obstetric Analgesia and AnesthesiaDocument17 pagesPractice Bullet In: Obstetric Analgesia and AnesthesiaKatherine ReyesNo ratings yet
- Cosili West Inventory of VaccinatedDocument28 pagesCosili West Inventory of VaccinatedLeigh BriosoNo ratings yet
- Introduction To Pharmacology DefinitionDocument4 pagesIntroduction To Pharmacology DefinitionMaicha PestañoNo ratings yet
- AripripazoleDocument13 pagesAripripazoleOneng IfayaniNo ratings yet
- AgonistsDocument25 pagesAgonistsOfficially RandomNo ratings yet
- Drug Study 1Document2 pagesDrug Study 1Kim Glaidyl BontuyanNo ratings yet
- Handbook of Pharmaceutical Excipients 8th Edition DownloadDocument2 pagesHandbook of Pharmaceutical Excipients 8th Edition DownloadPipe Rodriguez33% (3)
- Glargine Insulin For Veterinary UseDocument3 pagesGlargine Insulin For Veterinary Use13No ratings yet
- Meropenem - Drug Information - UpToDate-2Document8 pagesMeropenem - Drug Information - UpToDate-2Vh TRNo ratings yet
- Yovita - The Role of Clinical Pharmacist On Safe Administration AntibioticDocument48 pagesYovita - The Role of Clinical Pharmacist On Safe Administration AntibioticRois HasyimNo ratings yet
- MRM COLLEGE OF PHARMACY 5th Year ClerkshipDocument13 pagesMRM COLLEGE OF PHARMACY 5th Year ClerkshipkushalNo ratings yet
- Spontaneous ReportingDocument14 pagesSpontaneous Reportingmatin5No ratings yet
- Adults Parenteral Dilution Manual: Yousef AlomiDocument55 pagesAdults Parenteral Dilution Manual: Yousef AlomiAmeng GosimNo ratings yet
- Pharmacology II OutlineDocument52 pagesPharmacology II Outlinerjones53No ratings yet
- Microbiology Newlab سالى ابو السعود 0864986Document1 pageMicrobiology Newlab سالى ابو السعود 0864986Mohammed TahounNo ratings yet
- Forbes - Ten Misleading Drug AdsDocument8 pagesForbes - Ten Misleading Drug AdsrdandapsNo ratings yet
- The National Drugs List: of Syrian Arab RepublicDocument72 pagesThe National Drugs List: of Syrian Arab RepublicportosinNo ratings yet
- Hepagress LBLDocument4 pagesHepagress LBLAbhinavNo ratings yet
- Antiplatelet Antikoagulan Fibrinolitik Edit 2016Document18 pagesAntiplatelet Antikoagulan Fibrinolitik Edit 2016Katharina Marlyna BaniNo ratings yet
- Beclomethasone DipropionateDocument3 pagesBeclomethasone Dipropionateapi-3797941No ratings yet
- (Ebook PDF) Julien'S Primer of Drug Action: A Comprehensive Guide To The Actions, Uses, and Side Effects of Psychoactive Drugs 14Th EditioDocument42 pages(Ebook PDF) Julien'S Primer of Drug Action: A Comprehensive Guide To The Actions, Uses, and Side Effects of Psychoactive Drugs 14Th Editiocandace.binegar878100% (37)
- AMINOPHYLLINEDocument2 pagesAMINOPHYLLINEmusiclover017100% (1)
- Dhanushiya A-P Saravanan (0359079) Classification of NSAIDsDocument12 pagesDhanushiya A-P Saravanan (0359079) Classification of NSAIDsaurtho sadaaf sharrarNo ratings yet
- Anti Inflammatory DrugsDocument90 pagesAnti Inflammatory Drugsdrnasim2008817160% (5)
- Pediatric Drug Dosage - All in OneDocument15 pagesPediatric Drug Dosage - All in OneBJ Tiew100% (1)
- Daftar Harga 2019-2Document87 pagesDaftar Harga 2019-2Niken Claudya EcfrencylieNo ratings yet