Professional Documents
Culture Documents
(IM A) (Hema) IDA and Hypoproliferative Anemias-Dr. Perez 2 (Kim Villanueva)
Uploaded by
Noreen0 ratings0% found this document useful (0 votes)
25 views5 pagesOriginal Title
[IM A] [Hema] IDA and Hypoproliferative Anemias-Dr. Perez 2 (Kim Villanueva)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
25 views5 pages(IM A) (Hema) IDA and Hypoproliferative Anemias-Dr. Perez 2 (Kim Villanueva)
Uploaded by
NoreenCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
IM-A: HEMATOLOGY
1.4 IRON DEFICIENCY ANEM IAS & OTHER HYPOPROLIFERATIVE DISORDERS
Date: August 4, 2015
FEU-NRMF School of Medicine
:--------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
IRON DEFICIENCY ANEMIA FERRITIN HEMOSIDERIN
è Considered Microcytic, Hypochromic type of anemia Water soluble Water insoluble
è There is a reduction in Erythropoietin response. Found in the blood Found in tissues
è MOST COMMON CAUSE OF ANEMIA WORLDWIDE and the (macrophages)
MOST IMPORTANT CAUSE OF MICROCYTIC Correlates roughly with
HYPOCHROMIC ANEMIA total body iron stores (LOW
è 50% of cases SERUM FERRITIN indicates
è In the PHILIPPINES: LOW IRON STORAGE)
o It is a public health concern among 6 months to 1 Adult men: 800-‐1000mg
year old and Pregnant, Lactating women. Adult women: Few hundred
o Prevalence of IDA in the PH (2003), Pregnant mg
Women (43.9%), Lactating Women (42.2%) and Used in the diagnosis of IDA
Infants (66.2%)
PATHOPHYSIOLOGY OF MICROCYTIC HYPOCHROMIC ANEMIA MYOGLOBIN
è Found in the skeletal and cardiac muscle tissues
è Immediate iron stores
è In O2 deprivation, myoglobin IRON is stimulated so the
supply of Iron in the tissues (Cardiac, Skeletal) won’t be
depleted
HEME ENZYMES
è Enzymes that are responsible for metabolism, contains
iron. (e.g. CYTOCHROMES)
TRANSPORT IRON
è Smallest but most active iron compartment.
è Iron normally turns over at least 10x each day.
è Common pathway for interchange of iron between
compartments.
è Bound to transferrin (5% of total binding iron)
è Trans
è There are different elements in the hemoglobin synthesis: BODY IRON DISTRIBUTION and TRANSPORT
HEME and GLOBIN in order to form the hemoglobin è Mediated by 4 PROTEINS:
è If you have a problem with IRON SUPPLEMENTATION;
TRANSFERRIN Transport protein for iron
there will be a decrease in production of Hemoglobin,
TRANSFERRIN Expressed mostly by the red cell and the
Chronic Inflammation and malignancy.
RECEPTOR 1 liver
è Problems in the PROTORPHYRIN will give rise to
FERRITIN Major storage form of IRON
SIDEROBLASTIC TYPE OF ANEMIA
HEPCIDIN Regulator of Iron metabolism
è GLOBIN problems will incur THALASSAEMIA (alpha or beta)
THE IRON CYCLE
METABOLISM OF IRON
TOTAL BODY
COMPARTMENT MALE (g) FEMALE (g)
IRON (%)
HEMOGLOBIN IRON 2.4 1.7 65
STORAGE IRON (Ferritin, 1.0 (0.3-‐1.5) 0.3 (0-‐1.0) 30
Hemosiderin)
MYOGLOBIN IRON 0.15 0.12 3.5
HEME ENZYMES 0.02 0.015 0.5
TRANSPORT IRON 0.004 0.003 0.1
HEME IRON
è The iron in hemoglobin makes up the great bulk of heme
iron. Each gram of HEMOGLOBIN contains 3.4 mg of IRON.
(One ml of PACKED RED CELLS = 1 mg of IRON)
STORAGE IRON:
KIM VILLANUEVA, PTRP (3A) 1
è The Iron that is in the cytoplasm of the cell will cause
acidification because of the hydrogen available in the
cytoplasm.
è The amount of Iron absorbed by a normal adult male need
only the small amount that is excreted. (approx 1mg /day)
è A higher iron requirement exists during growth periods or FACTORS FAVOURING IRON FACTORS REDUCING IRON
ABSORPTION ABSORPTION
when there is blood loss.
Heme iron Inorganic iron
è In women, Iron absorbed must be sufficient to replace the Ferrous form Ferric form
loss during menstration or diversion to the fetus during Acids (HCl, Vitamin C) Alkalis – antacids, pancreatic seretions
pregnancy. Solubilizing agents (sugars, amino Precipitating agents – phylates,
è Daily absorbption: acids) phosphates, tea
o 4 mg Reduced serum hepcidin (e.g. IRON Increased serum hepcidin
o Transferrin: 4mg DEFICIENCY)
Ineffective erythropoiesis Decreased erythropoiesis
o Bone marrow: 150mg is present
Pregnancy Inflammation
o Macrophage: 0.5-‐1.5g Hereditary hemochromatosis
o Red Cell: 1.7-‐2.4 g Increased expression of DMT-‐1 in Decreased expressionof DMT-‐1 in
o Liver: 650mg duodenal enterocytes duodenal enterocytes
è In cases of IRON overload; most of the iron is taken up by Gastrectomy, achlorydia: mucosal
the macrophage. absorption
è If the capacity of the macrophage is exceeded, it will then
be transferred to the parenchymal cells of the liver. è Iron is absorbed best without food so take it with an empty
è One of the consequences of IRON OVERLOAD is LIVER stomach
CIRRHOSIS. è Pts with GI diseases, take the PPI in the morning and the
IRON ABSORPTION (REVIEW TO NG BIOCHEM) iron supplement after lunch.
è Iron is absorbed in the duodenal mucosa. If patients have
small bowel surgery, IV supplementation is useful.
LABORATORY EVALUATION OF IRON STATUS
è Direct Measures
o Bone marrow aspiration and biopsy
§ If you are suspecting hereditary
hemochromatosis
o Liver biopsy
è Indirect Measures
o Serrum ferritin, serrum transferrin receptor
concentration
o RBC, zinc, protoporphyrin level
o PBS – Microcytic, hypochromic red cell* may 1
point ka na daw pag kabisado mo ito.
o Serum Iron*
o TOTAL BINDING CAPACITY (TIBC)*
o Transferrin saturation*
§ Serum Iron x 100 / TIBC
è * -‐ request this because they are not affected by infection
è In the intestinal lumen, Fe3 enters to the intestinal mucosa
by undergoing REDUCTION facilitated by Ferric reductase.
è It will then attach to the DIVALENT METAL TRANSPORTER
(DMT1) which facilitate further internalization of iron
è Then it binds to FERROPORTIN, after oxidase reduction this
will then be released to the plasma and then transported
to the cells.
è However, in cases that there is an increase in the activity of
HEPCIDIN the FERROPORTIN will undergo lysis.
è If HEPCIDIN binds to the FERROPORTIN, the release of
IRON will be impeded thus will not be in the circulating
blood.
è THE IRON that is released in the blood will attach to the
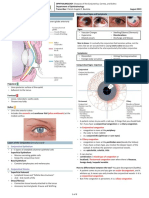
TRANSFERRIN receptor. (Figure: Appearance of red cell in Iron Deficiency Anemia)
è The Transferrin will then facilitate the transport of IRON to è Don’t be confused with Thalassemia
the CYTOPLASM of the CELL. o Poikilocytosis – there’s presence of TARGET CELLS
in Thalassemia
KIM VILLANUEVA, PTRP (3A) 2
EVOLUTION OF IRON DEFICIENCY è Serum Transferrin: 2-‐4 g/L (1 g/L transferrin = 20umol/L
binding capacity)
è Serum Iron: 10-‐30 u mol/L; TIBC: 40-‐75 u mol/L; serum
ferritin: MALE, 40-‐340u g/L, FEMALE: 14-‐150 u g/L)
CAUSES OF IRON DEFICIENCIES
è Blood Loss
o GI Bleeding, GenitoUrinary Tract Bleeding, Respi
Tract, Blood Donation
è Rapid Growth and Devt
è Menstruation
è Pregnancy
è Inadequate Iron Supply
è Dietary deficiency
è Impaired absorption of Iron
CLINICAL PRESENTATION
è Asymptomatic but with Lab signs of IDA
è Features of the underlying disorder responsible for iron
deficiency
o If there’s blood loss, that’s the number 1
complain
o Post-‐surgery
è Non-‐specific manifestations of anemia
o Dizziness, headache, hair loss
è Signs and sx SPECIFIC to IDA
o Pagophagia
o Koilonychia
o Blue Sclera
o Angular cheilosis
o Plummer Vinson’s Syndrome – Esophageal web,
(FIGURE: Lab Studies in evolution of Iron Deficiencies. Take note of dysphagia, IDA because of NODULAR TOXIC
the GREEN HIGHLIGHTED PARTS – CONCENTRATE ON THIS TABLE) GOITER
IRON THERAPY
IRON DEFICIENCY: Stages of development
è Up to 200mg of elemental iron per day is given, usually as
three or four iron tablets
o Each containing 50-‐65 mg elemental iron given
over the course of the day.
è Ideally iron should be taken on an empty stomach
è Reticulocyte count increases within 4-‐7 days after initiation
of therapy (Reticulocytosis)
è Sustained treatment for a period of 6-‐12 months after
correction of the anemia to provide stores of at least 0.5-‐1
gram of IRON.
NON-‐RESPONSIVE TO IRON THERAPY
è Incorrect diagnosis
è Continued loss of iron (occult bleeding etc)
NORMAL VALUES OF SERUM IRON, UIBC and SERUM FERRITIN in è Chronic infection or inflammation
NORMAL SUBJECTS, IRON DEFICIENCY ANEMIA and ANEMIA OF è Mixed deficiency
CHRONIC DISEASE and IRON OVERLOAD è Non-‐compliance of the patient
è Drug perparation
SERUM IRON/UIBC SERUM FERRITIN è Malabsorption of Iron
RATIO QUESTION NI KAT KABIGTING: Gaano katagal maquantify?
NORMAL Serum UIBC is more ANSWER NI DOCTORA: 3-‐4 weeks of OBSERVATION is needed. If the
than Serum IRON patient is non-‐responsive, check the factors affecting it.
IRON DEFICIENCY Decreased SERUM Decreased
IRON, Increase UIBC
ANEMIA OF CHRONIC Decreased SERUM Normal PARENTERAL IRON THERAPY is given if:
DISEASE IRON, Decreased UIBC è Cannot tolerate the side effects of oral iron
IRON OVERLOAD Pure SERUM IRON Over 1000 è PUD; inflammatory bowel disease
è Cannot comply with prescribed dose
è TIBC: made up of serum iron and UIBC è Iron malabsorption
KIM VILLANUEVA, PTRP (3A) 3
è Conditions with rapid loss of iron from continuous bleeding
which cannot be compensated by oral iron (e.g.:
Hereditary telangiectasia)
è FORMULA: Body weight (kg) x 2.3 x (15-‐patient’s
hemoglobin, g/dl) + 500 or 1000 mg (for stores)
è IV Iron dextran: anaphylaxis
o We don’t usually use this because of anaphylaxis
è Iron sucrose (Venofer) is used because of its less adverse
reactions.
è Things to watch out: DO A TEST DOSE. Prior to infusion,
give meds like paracetamol or anti-‐histamine.
OTHER HYPOPROLIFERATIVE ANEMIAS
1. ANEMIA OF CHRONIC DISEASE
è Anemia of underproduction that is usually: (FIGURE: PATHOPHYSIO OF ACD)
o Normocytic, normochromic
o Mild with hemoglobin level above 10g/dL 2. ANEMIA OF RENAL DISEASE
o In 30% of patients anemia can be severe and MCV è NORMOCYTIC NORMOCHROMIC
is reduced o May also present with microcytic
o Decrease in serum iron and TIBC; increase serum o Decreased EPO – dec. erythroid committed
ferritin precursors
o Decrease transferrin saturation. o Effects of uremic toxins – decrease red cell
o FERRITIN IS ELEVATED, SERUM IRON IS survival
DECREASED. o Foliate deficiency
è It can be microcytic anemia in severe cases è Decreased reticulocyte count
è OTHER CAUSES: è Hemolytic anemia
ASSOCIATED DISEASES ESTIMATED PREVALENCE
è Dilutional anemia
Infection (acute and chronic) 18-‐95%
Cancer 30-‐77%
o Pinkish appearance upon PE and yet Hb showed
Autoimmune 8-‐71% decreased value (anemic)
Chronic Rejection after solid organ 8-‐70% o Look at the PBS of the patient
transplantation è Blood loss anemia
CKD and Inflammation 23-‐50% o Mechanically induced because of the
CAUSES OF ACD hemodialysis
Block in reuse of iron by erythrocyte
è 3. ANEMIA OF ENDOCRINE DISORDERS
Shortened erythrocyte survival
è è Mild to moderate normocytic normochromic anemia
Direct inhibition of erythropoiesis
è è A decrease in plasma volume may mask the severity of the
Relative deficiency of erythropoietin
è anemia
è Results of decreased O2 requirement (e.g. hypothyroidism)
MECHANISM OF ANEMIA IN CHRONIC INFLAMMATION è Inappropriate EPO secretion (e.g. Adrenal and Androgen
è Cytokine driven type of anemia where you have at list of Deficiency)
cytokines that is known to inhibit erythropoiesis and the 4. ANEMIA OF LIVER DISEASE
release of erythropoietin DIRECT EFFECTS INDIRECT EFFECTS
è TNK and interferon gamma Toxic effects of ethanol Dilutional anemia – bec. Of Liver
è These cytokines also known to affect hepcidin – decreases failure
Acute and chronic blood loss Hypersplenism – enlargement of
absorption in the GIT
portal veins, portal hypertension
è Hepcidin will block the release of iron by macrophage Hemolytic anemia (SPUR-‐CELL) – 10%
è RBC won’t utilise the iron of patients acquired antibodies,
è Because it is cytokin driven, the effect of the cytokine can there’s (+) coomb’s test
be over drive by high doses of erythropoietin Malnutrition
è ANEMIA OF CHRONIC DISEASE can be treated by Anemia of Chronic inflammation
erythropoietin
SUPPRESION OF ERYTHROPOIESIS BY CYTOKINES
KIM VILLANUEVA, PTRP (3A) 4
5. ANEMIA OF MALIGNANCY
è More on direct effects
DIRECT EFFECTS INDIRECT
Replacement of marrow by malignant
cells (Myelopthisic), Fibrosis
Acute and chronic blood loss
è Anemia of chronic disease
è Anemia of chronic failure
è Malnutrition
è Microangiopathic hemolysis
è Immune hemolytic anemia
TREATMENT ASSSOCIATED ANEMIA
è Chemotherapy
è Radiotherapy
SOURCE:
PPT, 2015 Dra. Perez
Recording
RGAU trans 2014
HI NZG! <3 you
GOOD LUCK SA PRELIMS! #RoadtoClerkship
KIM VILLANUEVA, PTRP (3A) 5
You might also like
- Clinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzDocument31 pagesClinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzNoreenNo ratings yet
- MalnutritionDocument26 pagesMalnutritionudaybujji100% (1)
- Andrews1999 MetbolDocument10 pagesAndrews1999 Metbolida ayu agung WijayantiNo ratings yet
- AnemiaDocument10 pagesAnemiaBia Payawal100% (2)
- Some Biochemical Reactions Involving Essential MineralsDocument5 pagesSome Biochemical Reactions Involving Essential MineralsLunaNo ratings yet
- Iron Metabolism and Its DisordersDocument10 pagesIron Metabolism and Its DisordersMario AbdiwijoyoNo ratings yet
- CLINPHARMA 6.01 Erythropoiesis and AnemiaDocument3 pagesCLINPHARMA 6.01 Erythropoiesis and AnemiaMonique BorresNo ratings yet
- Iron Deficiency: Review SeriesDocument11 pagesIron Deficiency: Review SeriesWisher PgeNo ratings yet
- Medicines: A Short Review of Iron Metabolism and Pathophysiology of Iron DisordersDocument15 pagesMedicines: A Short Review of Iron Metabolism and Pathophysiology of Iron DisordersClaudiaNo ratings yet
- Deficiency of Iron: First Semester A.Y. 2015-2016Document8 pagesDeficiency of Iron: First Semester A.Y. 2015-2016emely p. tangoNo ratings yet
- Iron Deficiency Anemia: Ijeh LuckyDocument31 pagesIron Deficiency Anemia: Ijeh LuckyLucky ijehNo ratings yet
- Understanding The Logistics For The Distribution of Heme in CellsDocument15 pagesUnderstanding The Logistics For The Distribution of Heme in CellsJosiel Nasc'mentoNo ratings yet
- Biochimica Et Biophysica Acta: Tomas Ganz, Elizabeta NemethDocument10 pagesBiochimica Et Biophysica Acta: Tomas Ganz, Elizabeta NemethAnonymous oUlErgOINo ratings yet
- Pharmacolo Gy of Iron: By: Salma AhmedDocument38 pagesPharmacolo Gy of Iron: By: Salma AhmedSalmaNo ratings yet
- Diagnosis and Management of Iron Deficiency Anemia in The 21st CenturyDocument8 pagesDiagnosis and Management of Iron Deficiency Anemia in The 21st CenturyNur AlamNo ratings yet
- Anemia HypochromicDocument34 pagesAnemia HypochromicRazaz AdilNo ratings yet
- Anemia and Hematologic Drugs - KatzungDocument4 pagesAnemia and Hematologic Drugs - Katzungsarguss14100% (1)
- HEMATOLOGY 1 WEEK 7 PrintDocument4 pagesHEMATOLOGY 1 WEEK 7 PrintRose Neil LapuzNo ratings yet
- Erythroferrone Structure, Function, and PhysiologyDocument24 pagesErythroferrone Structure, Function, and PhysiologyNia AvellanedaNo ratings yet
- Drug Study SacroilliacDocument3 pagesDrug Study SacroilliacRose Ann CuaresmaNo ratings yet
- Disorders of Iron Metabolism Part II Iron Deficiency and Iron OverloadDocument10 pagesDisorders of Iron Metabolism Part II Iron Deficiency and Iron OverloadQistina SudarnotoNo ratings yet
- PIGMENTS Mbbs - Dr. SuchitaDocument53 pagesPIGMENTS Mbbs - Dr. SuchitaRushi VaghelaNo ratings yet
- The Mutual Crosstalk Between Iron and ErythropoiesisDocument10 pagesThe Mutual Crosstalk Between Iron and ErythropoiesisNur Melani Sari WardaniNo ratings yet
- Diseases of Hepatic Iron and Copper MetabolismDocument13 pagesDiseases of Hepatic Iron and Copper Metabolismputri riszaNo ratings yet
- Iron Physiology of IronDocument7 pagesIron Physiology of IronAnna PodsiadłoNo ratings yet
- Chapter 8Document4 pagesChapter 8Jane BacnotanNo ratings yet
- 1 s2.0 S0925443918303235 MainDocument13 pages1 s2.0 S0925443918303235 MainretnoNo ratings yet
- The Role of Iron: Ahmad Sh. Silmi MSC Haematology, FIBMSDocument66 pagesThe Role of Iron: Ahmad Sh. Silmi MSC Haematology, FIBMSMohamed MidoNo ratings yet
- Zinc and Skin BiologyDocument8 pagesZinc and Skin BiologyElva KadarhadiNo ratings yet
- Iron Deficiency Anemia 2023Document46 pagesIron Deficiency Anemia 2023CITLALI YATZIL SANDOVAL CATALAN100% (1)
- Chemical Coordination and IntegrationDocument47 pagesChemical Coordination and IntegrationDebika ChattopadhyayNo ratings yet
- Introduction To Rbcs Disorders: Iron Is Used, Recycled and StoredDocument8 pagesIntroduction To Rbcs Disorders: Iron Is Used, Recycled and StoredAsyeon GhaziNo ratings yet
- Pathophysiology of Iron HomeostasisDocument10 pagesPathophysiology of Iron HomeostasisJoséDantasNo ratings yet
- 1 s2.0 S006512810600122X MainDocument5 pages1 s2.0 S006512810600122X MainKevin MaiseyNo ratings yet
- BLOOD TransesDocument7 pagesBLOOD TransesBianca Paulyn CastilloNo ratings yet
- AnemiaDocument47 pagesAnemiaAjay KumarNo ratings yet
- BLOODDocument4 pagesBLOODariansofia1031No ratings yet
- Role For Ferritin in Hematopoiesis and The Immune SystemDocument5 pagesRole For Ferritin in Hematopoiesis and The Immune SystemStella NoviaNo ratings yet
- Mineral Ebook - TeamEvilGSPDocument50 pagesMineral Ebook - TeamEvilGSPnathanNo ratings yet
- Iron BalanceDocument7 pagesIron BalancegigibesiNo ratings yet
- Copper Toxic Heavy Metals Fact SheetDocument1 pageCopper Toxic Heavy Metals Fact SheetosumexNo ratings yet
- Slide 16 Fisiologi HematoDocument5 pagesSlide 16 Fisiologi Hematomarvin lionelNo ratings yet
- HEMA 2 - Midterm Topic 2 - Iron Metabolism DisordersDocument13 pagesHEMA 2 - Midterm Topic 2 - Iron Metabolism DisordersLowenstein JenzenNo ratings yet
- Hae Matin IcsDocument22 pagesHae Matin IcsAfreen HashmiNo ratings yet
- Biochemical PharmacologyDocument9 pagesBiochemical PharmacologyArifNo ratings yet
- Similarities N Differences of Facilitated Diffusion N Active TransportDocument24 pagesSimilarities N Differences of Facilitated Diffusion N Active TransportEddy LooNo ratings yet
- 04 - Iron Homeostasis in Host DefenceDocument11 pages04 - Iron Homeostasis in Host DefenceMatheus SouzaNo ratings yet
- Subject ChemistryDocument12 pagesSubject ChemistrykottooranjohnbNo ratings yet
- Cold Spring Harb Perspect Med-2013-MillerDocument14 pagesCold Spring Harb Perspect Med-2013-MillerIoana GhenadeNo ratings yet
- Globular Proteins: Dr. Sujin Bao, SJSMDocument27 pagesGlobular Proteins: Dr. Sujin Bao, SJSMethanNo ratings yet
- 1 Anatomy and Physiology of The Circulation of The BloodDocument10 pages1 Anatomy and Physiology of The Circulation of The BloodVladislav KotovNo ratings yet
- Heme Vs Inorganic IronDocument4 pagesHeme Vs Inorganic IronBlanca RuizNo ratings yet
- Food and Nutrition MFN 004 Unit 10Document61 pagesFood and Nutrition MFN 004 Unit 10SHAHI'S CREATIONNo ratings yet
- Pharmacology IBLS SummaryDocument36 pagesPharmacology IBLS Summaryalamri.salah99No ratings yet
- Iron HomeostasisDocument30 pagesIron HomeostasisTony NgNo ratings yet
- Amino Acids & ProteinsDocument12 pagesAmino Acids & ProteinsJearnie Lou Arroyo100% (1)
- 5 2 Microcytic Anemias PDFDocument3 pages5 2 Microcytic Anemias PDFPrabhat GuptaNo ratings yet
- Kelainan Morfologi EritrositDocument19 pagesKelainan Morfologi EritrositAdel shbelNo ratings yet
- Kangen Water The Miracle Life ProviderDocument29 pagesKangen Water The Miracle Life ProviderSattly100% (1)
- Def Besi Andrews 2005Document2 pagesDef Besi Andrews 2005Amirah FirdausyNo ratings yet
- Biologically Active Amines Found in Man: Their Biochemistry, Pharmacology, and Pathophysiological ImportanceFrom EverandBiologically Active Amines Found in Man: Their Biochemistry, Pharmacology, and Pathophysiological ImportanceNo ratings yet
- (GYNE) 2018 April Midterms Ratio (Pucca)Document31 pages(GYNE) 2018 April Midterms Ratio (Pucca)NoreenNo ratings yet
- (Gyne) Family Planning (Dra Ona - Dra Castro) Updated Version (2022)Document14 pages(Gyne) Family Planning (Dra Ona - Dra Castro) Updated Version (2022)NoreenNo ratings yet
- (Anes) 5 - Local Anesthetics (Dra. Bonoan-Chan) ?Document5 pages(Anes) 5 - Local Anesthetics (Dra. Bonoan-Chan) ?NoreenNo ratings yet
- (Cardio B) 1 - Acute Rheumatic Fever and Rheumatic Heart Disease (Dr. Antolin, 2019)Document4 pages(Cardio B) 1 - Acute Rheumatic Fever and Rheumatic Heart Disease (Dr. Antolin, 2019)NoreenNo ratings yet
- Case 9 Section EDocument12 pagesCase 9 Section ENoreenNo ratings yet
- (Anes) 3 - Monitoring of Anesthetized Patient (Dra. Mendoza) ?Document4 pages(Anes) 3 - Monitoring of Anesthetized Patient (Dra. Mendoza) ?NoreenNo ratings yet
- (IM A) (Com Dse) Typhoid Fever (Strawberry)Document4 pages(IM A) (Com Dse) Typhoid Fever (Strawberry)NoreenNo ratings yet
- (IM A) (Com Dse) Typhoid Fever-Dr. Salandanan, Dr. Tan (Trisha Oberio, Kristine Navarro, Aisle Paler)Document4 pages(IM A) (Com Dse) Typhoid Fever-Dr. Salandanan, Dr. Tan (Trisha Oberio, Kristine Navarro, Aisle Paler)NoreenNo ratings yet
- (Anes) 1 - Preanesthetic Evaluation (Dra. Luna-Gomez) ?Document5 pages(Anes) 1 - Preanesthetic Evaluation (Dra. Luna-Gomez) ?NoreenNo ratings yet
- Clinical Therapeutics: Case 1Document17 pagesClinical Therapeutics: Case 1NoreenNo ratings yet
- (IM A) (Com Dse) Rabies-Dr. Coronel (Vision)Document7 pages(IM A) (Com Dse) Rabies-Dr. Coronel (Vision)Noreen100% (1)
- (MED) 3.05 Approach To Edema, Chest Pain, & Palpitations - AzaresDocument18 pages(MED) 3.05 Approach To Edema, Chest Pain, & Palpitations - AzaresNoreenNo ratings yet
- (Ophtha) 7 - Diseases of The Conjunctiva, Cornea, and Sclera (2019)Document8 pages(Ophtha) 7 - Diseases of The Conjunctiva, Cornea, and Sclera (2019)NoreenNo ratings yet
- Cardiology: Normal and Abnormal Myocardial Function: LendldeornmanDocument2 pagesCardiology: Normal and Abnormal Myocardial Function: LendldeornmanNoreenNo ratings yet
- (Pedia 3A) NEPHRO COMPILED PDFDocument40 pages(Pedia 3A) NEPHRO COMPILED PDFNoreenNo ratings yet
- (Pedia 3A) Immunology-Dr. de Jesus (Pinky Square)Document6 pages(Pedia 3A) Immunology-Dr. de Jesus (Pinky Square)NoreenNo ratings yet
- (MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)Document11 pages(MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)NoreenNo ratings yet
- Hypovolemic Shock & DIC (Bernabe)Document4 pagesHypovolemic Shock & DIC (Bernabe)NoreenNo ratings yet
- Bio310 Written Report Anemia AS1205B PDFDocument23 pagesBio310 Written Report Anemia AS1205B PDFFahmy AmyNo ratings yet
- Roth 10e Nclex Chapter 01Document5 pagesRoth 10e Nclex Chapter 01Marc FresNo ratings yet
- SMPC Iron SucroseDocument9 pagesSMPC Iron SucroseshrikantmsdNo ratings yet
- Low Hemoglobin Food and DietDocument8 pagesLow Hemoglobin Food and Dietdg_samrat6595No ratings yet
- Vegetarian Athelte, NutritionDocument16 pagesVegetarian Athelte, NutritionccciiipppNo ratings yet
- J1-T5 Anemia FerropénicaDocument12 pagesJ1-T5 Anemia FerropénicaGoblin HunterNo ratings yet
- ABP3 IntoxmetalespesadosDocument18 pagesABP3 IntoxmetalespesadosFernandoLuyoNo ratings yet
- Nutritional Deficiency For ClassDocument74 pagesNutritional Deficiency For ClassBelayneh TadesseNo ratings yet
- Approached in Diagnosis of AnemiaDocument41 pagesApproached in Diagnosis of AnemiaAlqodri SetiawanNo ratings yet
- Paediatrica Indonesiana: Intan Alita Putri Tumbelaka, Hardiono D Pusponegoro, Rinawati RohsiswatmoDocument7 pagesPaediatrica Indonesiana: Intan Alita Putri Tumbelaka, Hardiono D Pusponegoro, Rinawati RohsiswatmoWilliamNo ratings yet
- NCSF Chapter 8 Nutrition-Non Energy NutientsDocument22 pagesNCSF Chapter 8 Nutrition-Non Energy NutientsJessie Tang0% (1)
- Parrillo Sports Nutrition Guide Part 2Document299 pagesParrillo Sports Nutrition Guide Part 2shawn hogan100% (1)
- AnemiaDocument33 pagesAnemiaDiwiasti Firdausi YasminNo ratings yet
- Iron Deficiency AnaemiaDocument132 pagesIron Deficiency AnaemiaHectorNo ratings yet
- Lecture 3 - Iron Homeostasis, AnemiaDocument30 pagesLecture 3 - Iron Homeostasis, AnemiaJoanna BrumaruNo ratings yet
- 2019 - Chelation Therapy in Medicine - Derrick Lonsdale Hormones MatterDocument9 pages2019 - Chelation Therapy in Medicine - Derrick Lonsdale Hormones MatterSimon SaundersNo ratings yet
- Nutritional Anemias in ChildrenDocument64 pagesNutritional Anemias in Childrendasaradharamireddy80% (5)
- Drug Treatment of AnemiaDocument36 pagesDrug Treatment of Anemiadoctorneha66No ratings yet
- Feeding Toddlers and Pre-School Children 1 To 5 YearsDocument23 pagesFeeding Toddlers and Pre-School Children 1 To 5 YearsclaireNo ratings yet
- Metabolisme Zat BesiDocument33 pagesMetabolisme Zat BesiFetria MelaniNo ratings yet
- Iron Deficiency AnemiaDocument12 pagesIron Deficiency AnemiaMargarita TorresNo ratings yet
- Nutrition & BrainDocument33 pagesNutrition & BrainRegina HershaaNo ratings yet
- Frater Albertus - EssentiaDocument316 pagesFrater Albertus - Essentiatravellerfellow100% (4)
- Archer Review Note 5Document11 pagesArcher Review Note 5karan SinghNo ratings yet
- Functions and Deficiency Symptoms of MineralsDocument12 pagesFunctions and Deficiency Symptoms of MineralsAshley Sparkles100% (1)
- Manchester Anaemia GuideDocument13 pagesManchester Anaemia Guidemubzy14No ratings yet
- Minerals and Trace ElementsDocument35 pagesMinerals and Trace ElementsMary Faith MadayagNo ratings yet
- 1 - Iron Content, Bioavailability & Factors Affecting Iron Status of IndiansDocument12 pages1 - Iron Content, Bioavailability & Factors Affecting Iron Status of IndiansDivyesh AmarsedaNo ratings yet
- Trace ElementsDocument5 pagesTrace ElementsFaithNo ratings yet