Professional Documents
Culture Documents
(Anes) 3 - Monitoring of Anesthetized Patient (Dra. Mendoza) ?
Uploaded by
NoreenOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(Anes) 3 - Monitoring of Anesthetized Patient (Dra. Mendoza) ?
Uploaded by
NoreenCopyright:
Available Formats
[ANESTHESIOLOGY] Monitoring the Anesthetized Patient
Lecturer: Tracy C. Mendoza MD
Transcriber: Patrick Angelo R. Bautista August 2020
References and Legends
nd
• {💻} PPT and {📕} Chapter 3 - Anesthesiology Manual 2 Ed 2.1Oxygenation
• {📖} Morgan & Mikhail’s Clinical Anesthesiology 5 Ed
th
• This is to ensure adequate oxygen concentration in the inspired
• {📌} Transcriber’s Note gas and the blood during all anesthetics.
• Methods to measure oxygenation:
Table of Contents
9 Using an oxygen analyzer and oximeter with low concentration
I. Monitoring the Anesthetized Patient 1
1
alarm limit during general anesthesia.
II. ASA Standards for Basic Anesthetic Monitoring
9 Standard I 1
1
2.2Ventilation
9 Standard II
III. Monitoring of Inspired Gases 2 • To guarantee adequate ventilation of patient during all anesthetics.
9 Oxygen Monitoring 2 • Some methods to confirm sufficient ventilation:
9 Pulse Oximetry 2 9 Qualitative clinical signs (e.g. facial cyanosis, pale nail beds)
IV. Monitoring of Expired Gases 2 9 Continual monitoring with capnography
9 Carbon Dioxide 2 • To maintain ventilation, bag-mask ventilation or endotracheal
V. Blood Pressure Monitoring 2 intubation must be performed to sustain oxygen delivery.
9 Invasive Measurement of Vascular Pressure 3 • Endotracheal intubation requires qualitative identification of
9 Non-invasive Measure of Arterial Blood Pressure 3 carbon dioxide in the expired gas.
9 Effect of BP Cuff Width on BP Readings 3 • A continuous end-tidal carbon dioxide analysis is encouraged
9 Central Venous Pressure 4 during general anesthesia.
9 Pulmonary Artery Monitoring 4
9 Transesophageal Echocardiography 4 2.3 Circulation
VI. Monitoring Neurologic Function 4 • To safeguard patient’s circulatory function during all anesthetics
9 Bispectral Monitoring (BIS) 4 the following methods should be exercised:
VII. Monitoring Neuromuscular Blockade 4 9 ECG should be continuously displayed at all times
9 Peripheral Nerve Stimulator 4 9 Check blood pressure and heart rate
VIII. Samplex 4 9 Plus any of the following:
§ Palpation of a pulse
I. MONITORING THE ANESTHETIZED PATIENT § Auscultation of heart sounds
§ Monitoring intra-arterial pressure tracing
• It is a process by which anesthesiologist recognize and evaluate
§ Ultrasound peripheral pulse monitoring or pulse oximetry.
potential physiologic problems in a timely manner.
• Four essentials feature of monitoring:
9 Observation and Vigilance
2.4 Temperature
9 Instrumentation • This aids in the maintenance of appropriate core body heat during
9 Interpretation of Data all anesthetics.
9 Initiation of Corrective Therapy when indicated • Hypothermia is defined as a body temperature <36°.
• These anesthetic agents affect the body temperature and at the
same time, change in body temperature affect anesthetic drug
II. ASA STANDARDS FOR
actions to the body.
BASIC ANESTHETIC MONITORING • When changes in body temperature are intended or anticipated,
• Emphasize the importance of regular and frequent measurements temperature should be continuously measured and recorded on
• Integration of clinical judgement and experience the anesthesia record.
• The potential for extenuating circumstances that can influence the • Indications for body temperature monitoring:
applicability or accuracy of monitoring systems 9 All patients undergoing general anesthesia except when
duration <15 mins
1. Standard I 9 Unintentional hypothermia during anesthesia
• Qualified anesthesia personnel shall be present in the room
Unintentional Hypothermia During General Anesthesia
throughout the conduct of all general anesthetics, regional
• Occurs when there is no attempt to warm an anesthetized patient.
anesthetics and monitored anesthesia care.
• Phase I – Redistribution
9 The body core temperature decreases by 1-2°C for the first
2. Standard II hour of general anesthesia.
• During all anesthetics, the patient’s oxygenation, ventilation, 9 This phase is due to anesthetic vasodilation (heat
circulation and temperature shall be continually evaluated. redistribution) from warm central compartment to cooler
• Focuses attention on continually evaluating the patient’s: peripheral compartment.
9 Oxygenation • Phase II
9 Ventilation 9 After 3-4 hours under general anesthesia, there is continual
9 Circulation heat loss which cause gradual decline of core body temp.
9 Temperature • Phase III
9 Eventually reaching a steady state equilibrium wherein the
heat loss is the same with the metabolic heat production.
Monitoring of the Anesthetized Patient | 1 of 4
Sites for Temperature Monitoring • Capnograph displays a continuous outline of PCO2 in the airway
a. Tympanic membrane versus time.
9 This area reflects the brain temperature. • Capnometer measures and shows only discrete values of partial
9 Use of tympanic thermometer sensors nowadays prevent it from pressure of CO2 (PCO2) called the end-tidal carbon dioxide
possible trauma and insulation by cerumen in auditory canal. changes in PaCO2.
b. Rectal site • It has evolved as an important physiologic and safety monitor.
9 Not ideal since it has a slow response to changes in body core • CO2 is usually sampled near the endotracheal-gas delivery
temperature. interface.
c. Nasopharyngeal site • Alterations in ventilation, cardiac output, distribution of pulmonary
9 Accurate but poses danger of epistaxis due to instrumentation. blood flow, and metabolic activity influence PECO2 and the
d. Axillary site capnograph display obtained during quantitative expired gas
9 The most common area to measure body temperature. analysis which also uses the Beer Lambert law.
9 However, this has variable correlation between axillary and
core temperature. V. BLOOD PRESSURE MONITORING
e. Esophageal site
9 Most ideal (best of economy, performance and safety) and
• The most important indicator of the adequacy of circulation.
usually incorporated to esophageal stethoscope. • It is an indirect measurement of arterial blood pressure.
rd
9 This is positioned behind the distal 3 of the esophagus or
the level of cardiac region. • The rhythmic contraction of the left ventricle, ejecting blood into
9 This may give falsely low readings if not inserted too deep.
the vascular system, results in pulsatile arterial pressures.
9 Systolic BP – the peak pressure generated during systolic
contraction (in the absence of aortic valve stenosis).
III. MONITORING OF INSPIRED GASES 9 Diastolic BP – the lowest arterial pressure during diastolic
relaxation.
1. Oxygen Monitoring
9 Pulse pressure – the difference between the SBP and DBP.
• Gas machine manufacturers place oxygen sensors on the inspired 9 Mean arterial pressure (MAP) – time-weighted average of
limb of the anesthesia circuit to ensure that hypoxic gas mixtures arterial pressures during a pulse cycle.
are never delivered to patients.
2. Pulse Oximetry
• The standard of care for monitoring O2 during anesthesia. • As a pulse moves peripherally through the arterial tree, wave
• Measures pulse rate and oxygen saturation of hemoglobin on a reflection distorts the pressure waveform, leading to an
noninvasive continuous basis
exaggeration of systolic and pulse pressures.
• Combined technology of plethysmography and spectrophotometry.
9 A plethysmography produces a pulse trace that is helpful in
tracking circulation.
9 Oxygen saturation is determined by spectrophotometry,
which is based on the Beer-Lambert Law.
• Pulse oximetry has the capability for detecting desaturation before
it is clinically-apparent.
• Normal values:
9 Adults: 95% (for those with no lung disease)
9 Children: 96%
How Does a Pulse Oximeter Work?
Figure: Changes in configuration as a waveform moves peripherally.
• The level of the sampling site relative to the heart affects the
It measures 2 types of Hemoglobin by measurement of blood pressure because of the effect of gravity.
Spectrophotometry or Absorbance
of Light:
• Oxygenated or Saturated Hgb
absorbs the infrared band.
• Deoxygenated or Unsaturated
Hgb absorbs the red band.
IV. MONITORING OF EXPIRED GASES
1. Carbon Dioxide
• ETCO2 reflects changes in PaCO2
9 ETCO2 – the amount of carbon dioxide (CO2) in exhaled air,
which assesses ventilation.
9 PaCO2 – partial pressure of CO2 in arterial blood Figure: The difference in blood pressure (mm Hg) at two different sites of
• Capnograph is an essential element in determining the placement measurement equals the height of an interposed column of water (cm
of endotracheal tubes. H2O) multiplied by a conversion factor (1 cm H2O = 0.74 mm Hg).
9 Presence of three consecutive waveforms in the capnograph
confirms that the ET tube traversed the glottic airway opening.
Monitoring of the Anesthetized Patient | 2 of 4
1. Invasive Measurement of Vascular Pressure 2.4Oscillometry
• Permits the opportunity to monitor arterial BP continuously and to • Arterial pulsations cause oscillation of the inflating cuff.
have vascular access for arterial blood sampling. • Microprocessor interprets measurement thru an algorithm.
• This can be done through direct arterial cannulation. 9 A microprocessor derives systolic, mean, and diastolic
• Indications: pressures using an algorithm.
9 Induced current or anticipated hypotension or wide blood 9 Machines that require identical consecutive pulse waves for
pressure deviations measurement confirmation may be unreliable during
9 End-organ disease necessitating precise beat-to-beat blood arrhythmias (eg, atrial fibrillation).
pressure regulation • In automated BP monitors electronically measure the pressures at
9 Need for multiple arterial blood gas measurements which the oscillation amplitudes changes.
• Contraindications:
9 If possible, catheterization should be avoided in smaller end
arteries with inadequate collateral blood flow or in extremities
where there is a suspicion of preexisting vascular insufficiency.
2. Non-invasive Measurement of Arterial Blood Pressure
2.1 Palpation
• SBP can be determined by:
1) Locating a palpable peripheral pulse
2) Inflating a blood pressure cuff proximal to the pulse until flow is
occluded
3) Releasing cuff pressure by 2 or 3 mm Hg per heartbeat
4) Measuring the cuff pressure at which pulsations are again
Figure: Oscillometric determination of blood pressure.
palpable.
• Disadvantages:
2.5Arterial Tonometry
9 No diastolic/mean arterial blood pressure measurement
9 Possible underestimation of systolic blood pressure • It measures beat-to-beat arterial BP by sensing pressure required
to partially flatten a superficial artery that is supported by a bony
2.2 Doppler Probe structure like the radial artery.
• Pressure transducers are applied to the skin overlying the artery
• It has same principle as palpation except substitution of doppler
as shown in the figure below.
probe instead of finger.
• Contact stress between the transducer and the skin reflect
• Doppler Shift
intraluminal pressure.
9 Change / shift in frequency of sound waves as blood flow.
• Disadvantages:
• This is useful in pediatric, obese or trauma patients.
9 Sensitivity to movement artifacts
• Some Doppler models can detect both systolic / diastolic pressure.
9 Frequent calibration
Figure: Tonometry is a method of continuous (beat-to-beat) arterial BP
determination. The sensors must be positioned directly over the artery.
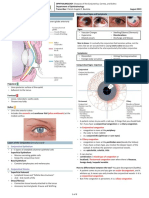
3. Effect of BP Cuff Width on BP Readings
Figure: A Doppler probe secured over the radial artery will sense red • The measurement of the cuff’s bladder should be at least halfway
blood cell movement as long as the BP cuff is below systolic pressure. around the desired extremity.
• The width of the bladder cuff should be 20-50% greater than the
2.3 Auscultation diameter of the extremity.
• Inflation of BP cuff in between systolic and diastolic pressure will • Narrower cuff – may overestimate the systolic pressure.
cause collapse of underlying artery. • Wider cuff – may underestimate the systolic pressure.
• Korotkoff sounds • The error with a cuff 20% too wide is not as significant as the error
9 Produced by a turbulent flow with a cuff 20% too narrow.
9 Audible thru stethoscope • Refer to the figure on the next page:
• Auscultatory gap 9 A – narrowest bladder cuff may produce overestimation of
9 Absence of Korotkoff sounds the systolic pressure.
9 May be encountered among hypertensive patients 9 B – ideal bladder cuff and will produce accurate results.
9 C – shows a wider bladder cuff that will produce
underestimation of the systolic pressure.
Monitoring of the Anesthetized Patient | 3 of 4
• Train of four (TOF)
9 The most common pattern used to evaluate residual blockade.
9 It has four stimuli at 2 hertz frequency.
9 The TOF ratio (T4/T1) should be above 0.9 (90%) in order to
rule out residual muscle weakness.
• Potential adverse effects of residual neuromuscular blockade in
the immediate postoperative period.
a. Need for tracheal reintubation
b. Impaired oxygenation and ventilation (erroneously attributed to
opioids)
c. Impaired pulmonary function (reduced forced vital capacity and
peak expiratory flow rate)
d. Increased risk of aspiration and pneumonia
e. Pharyngeal dysfunction
f. Delayed discharge from the Post Anesthesia Care Unit (PACU)
Figure: Blood pressure cuff width influences the pressure readings.
Three cuffs, all inflated to the same pressure, are shown. The narrowest
cuff (A) will require more pressure, and the widest cuff (C) less pressure, to
occlude the brachial artery for determination of systolic pressure.
(A) Narrowest – Overestimation
(B) Ideal – Accurate
(C) Widest – Underestimation
4. Central Venous Pressure (CVP)
• Essentially equivalent to right atrial pressures
• Serve as a reflection of right ventricular preload.
• Reflects the:
9 Amount of blood returning to the heart
9 Ability of the heart to pump the blood into the arterial system
Figure: Peripheral Nerve Stimulator attached to anesthetized
patient under neuromuscular block.
5. Pulmonary Artery Monitoring
• A flow-directed device described as a balloon flotation-
pulmonary artery catheter.
VIII. SAMPLEX
• It is a major advance in hemodynamic monitoring, and it has There are only 3 questions on my samplex regarding this topic. LOL.
become an important tool in the quantitative assessment of Still a lot of possible questions. Study well!
cardiopulmonary function.
1. Which of the following monitors is under the principle of Oscillometry?
A. Capnogram C. Electrocardiogram
6. Transesophageal Echocardiography B. Pulse oximeter D. Blood pressure monitoring
• Accurate estimates of left ventricular preload.
2. Which of the following monitors is under the principle of Beer-
• Estimates intra-cardiac filling and contractility.
Lamberts Law?
• Estimates ejection fraction.
A. Capnogram C. Electrocardiogram
B. Pulse oximeter D. Blood pressure monitoring
VI. MONITORING NEUROLOGIC FUNCTION 3. In monitoring thermoregulation during general anesthesia, which of the
1. Bispectral Monitoring (BIS) following location is best to place probe to access body core temp?
A. Oral C. Distal esophagus
• The BIS monitor determines the depth of general anesthesia. B. Rectal D. Tympanic membrane
• It has a sensor which is placed on the patient’s forehead to pick up
electrical signals from the cerebral cortex and displays it in the 📌 No proofreading. Use at your own risk.
digital signal converter. Use Samplex questions only as your guide.
• BIS values varies from 0 to 100 Good luck!
9 0 means ‘deep sleep’
9 100 means ‘awake’
• Ideal value range to safely perform surgery is between 40-60.
VII. MONITORING NEUROMUSCULAR BLOCKADE
1. Peripheral Nerve Stimulator
• A recommendation for standards of monitoring during anesthesia
and recovery” studied by the Association of Anesthetists of Great
Britain and Ireland (AAGBI) requires that “a peripheral nerve
stimulator must be utilize whenever neuromuscular blocking
drugs are administered.”
• This device delivers an electrical stimulus to a peripheral nerve,
most commonly the ulnar nerve.
• The expected outcome is twitching of the innervated thumb and
the presence or absence of muscle weakness is evaluated by
decreasing muscle twitching with repetitive nerve stimulus.
Monitoring of the Anesthetized Patient | 4 of 4
You might also like
- Monitoring During AnaesthesiaDocument17 pagesMonitoring During AnaesthesiaSummaiyya FazalNo ratings yet
- Monitoring Intra OperatifDocument21 pagesMonitoring Intra OperatifAlaa Ulil HaqiyahNo ratings yet
- Anes DLR Feb 26 2023Document11 pagesAnes DLR Feb 26 2023Benjune RoseladaNo ratings yet
- Monitoring Intra Operatif: Mindi Widayani NRP 122.022.1115 FK UPN "Veteran" JakartaDocument21 pagesMonitoring Intra Operatif: Mindi Widayani NRP 122.022.1115 FK UPN "Veteran" Jakartaputri wulandariNo ratings yet
- Anesthesia MonitoringDocument14 pagesAnesthesia MonitoringIga Bagus Suastika100% (3)
- 6 - Monitoring During Anaesthesia (Updated)Document15 pages6 - Monitoring During Anaesthesia (Updated)ضبيان فرحانNo ratings yet
- Anesthesia 3Document24 pagesAnesthesia 3PM Basiloy - AloNo ratings yet
- 7 - Capnography ProcedureDocument2 pages7 - Capnography ProcedurejasminemuammilNo ratings yet
- Case 8Document6 pagesCase 8ReddyNo ratings yet
- Recommendations For Standards of Monitoring During Anaesthesia and Recovery 2021Document14 pagesRecommendations For Standards of Monitoring During Anaesthesia and Recovery 2021Ahmad Fairuz Abdul ShokriNo ratings yet
- Intervensi Tumor CerebriDocument5 pagesIntervensi Tumor CerebriASIH DEVINo ratings yet
- RLE - Reviewer-SuctioningDocument16 pagesRLE - Reviewer-SuctioningVinzii DrtNo ratings yet
- Standards For Basic Anesthetic MonitoringDocument3 pagesStandards For Basic Anesthetic MonitoringMuhammad AsyrafNo ratings yet
- Anesthesia MonitoringDocument69 pagesAnesthesia MonitoringCzar SyNo ratings yet
- Perioperative MonitoringDocument25 pagesPerioperative MonitoringHanif SumonNo ratings yet
- Transoperative 812217287Document27 pagesTransoperative 812217287Pepe PeñaNo ratings yet
- Respiratory Term 2Document13 pagesRespiratory Term 2Abegail QuintoNo ratings yet
- Impact of Continuous Non-Invasive Blood Pressure Monitoring On Hemodynamic Fluctuation During General Anesthesia: A Randomized Controlled StudyDocument9 pagesImpact of Continuous Non-Invasive Blood Pressure Monitoring On Hemodynamic Fluctuation During General Anesthesia: A Randomized Controlled StudyShovie Thalia MirandaNo ratings yet
- Dr. AftabDocument87 pagesDr. Aftabalhada azofit almaNo ratings yet
- Monitoring in Icu and AneshtesiologyDocument19 pagesMonitoring in Icu and AneshtesiologySuvini GunasekaraNo ratings yet
- Week 7Document12 pagesWeek 7MARIKA BALONDONo ratings yet
- 13 - Partial Brain Tissue Oxygenation MonitoringDocument2 pages13 - Partial Brain Tissue Oxygenation MonitoringjasminemuammilNo ratings yet
- General Anaesthesia OverviewDocument21 pagesGeneral Anaesthesia OverviewAndri SaputraNo ratings yet
- Icu 2Document9 pagesIcu 2GemilleDaphneAndradaNo ratings yet
- GUIDELINES FOR THE USE OF PULSE OXIMETRY IN MONITORING COVID-19 PATIENTS IN HBIC - EnglishDocument3 pagesGUIDELINES FOR THE USE OF PULSE OXIMETRY IN MONITORING COVID-19 PATIENTS IN HBIC - EnglishThanh NamNo ratings yet
- Acute Compartment Syndrome in Orthopedics: Cause, Diagnosis, and ManagementDocument16 pagesAcute Compartment Syndrome in Orthopedics: Cause, Diagnosis, and ManagementAbdullah AzzamNo ratings yet
- Mini Project-1Document16 pagesMini Project-1S ThivinNo ratings yet
- Your Big IdeaDocument12 pagesYour Big Ideaapi-380169571No ratings yet
- Ambulatory Blood Pressure MonitoringDocument5 pagesAmbulatory Blood Pressure Monitoringابو عبد الرحمنNo ratings yet
- $RFIIM3JDocument4 pages$RFIIM3JMichaelNo ratings yet
- Conns Syndrome Gonzales NickaDocument10 pagesConns Syndrome Gonzales Nickamafeehney feehilyNo ratings yet
- Pulmonary EmbolismDocument2 pagesPulmonary EmbolismAnjana BasilNo ratings yet
- Nursing Care Plan AnemiaDocument3 pagesNursing Care Plan AnemiaNat B. AntipoloNo ratings yet
- Prepration of Patient For General AnasthesiaDocument63 pagesPrepration of Patient For General Anasthesiashiree21No ratings yet
- Monitoring in AnesthesiaDocument7 pagesMonitoring in AnesthesiaAhmed zanon -أحمد ظنونNo ratings yet
- Article MapeoDocument5 pagesArticle Mapeoapi-654112138No ratings yet
- 3 Using Pulse OximeterDocument2 pages3 Using Pulse OximeterAbdallah AlasalNo ratings yet
- Coronary AtherosclerosisDocument3 pagesCoronary AtherosclerosisGwyn Oona Florence ForroNo ratings yet
- Brain Death AANDocument2 pagesBrain Death AANFabián Esteban Maturana Barra100% (1)
- Prado, Catherine BSN IIB (Activity 1 Case Scenario)Document52 pagesPrado, Catherine BSN IIB (Activity 1 Case Scenario)Catherine PradoNo ratings yet
- (ANES) Sat 05 Pharmacology of Inhalational Anesthetics (A2021)Document3 pages(ANES) Sat 05 Pharmacology of Inhalational Anesthetics (A2021)Ricky Justin NgoNo ratings yet
- Local AnesthesiaDocument25 pagesLocal Anesthesiaapi-19916399No ratings yet
- Drug Study PediaDocument18 pagesDrug Study PediaCyx17No ratings yet
- Increased ICPDocument22 pagesIncreased ICPCHARLOTTE DU PREEZNo ratings yet
- BSN2 2 CMCA RLE Using A Pulse OximeterDocument2 pagesBSN2 2 CMCA RLE Using A Pulse OximeterJane RicadNo ratings yet
- Evidence Based Nursing (Ebn)Document29 pagesEvidence Based Nursing (Ebn)UmmNo ratings yet
- Basic Anesthetic Monitoring 2011Document3 pagesBasic Anesthetic Monitoring 2011egomezgrasNo ratings yet
- Verazon, Bsn3a-Myastenia NCPDocument5 pagesVerazon, Bsn3a-Myastenia NCPJaylord VerazonNo ratings yet
- Or - Postoperative PhaseDocument10 pagesOr - Postoperative Phase11 - JEMELYN LOTERTENo ratings yet
- A B C D E: Advanced Trauma Life Support - AtlsDocument2 pagesA B C D E: Advanced Trauma Life Support - AtlsAnnsha VeimernNo ratings yet
- Invasive and Non Invasive MonitorDocument22 pagesInvasive and Non Invasive Monitorbagya priyaNo ratings yet
- Increased ICP by MoumitaDocument58 pagesIncreased ICP by Moumitatalktotrisha23No ratings yet
- HPN & CHF: RLE #1 Alabe, Aquino, Aquino, Binwag, Tolentino, RosalesDocument10 pagesHPN & CHF: RLE #1 Alabe, Aquino, Aquino, Binwag, Tolentino, RosalesApril Mae Magos LabradorNo ratings yet
- Edwards Hemodynamic Monitoring For COVID Critically Ill PatientsDocument3 pagesEdwards Hemodynamic Monitoring For COVID Critically Ill PatientsblanquishemNo ratings yet
- Sepsis Emergency-Avepa 2020 1. Systemic Inflammation (Sirs)Document3 pagesSepsis Emergency-Avepa 2020 1. Systemic Inflammation (Sirs)Yaiza Garcia CasadoNo ratings yet
- Sedation For Icu Patients PresentationDocument8 pagesSedation For Icu Patients Presentationapi-736869233No ratings yet
- Barana JointDocument36 pagesBarana Jointmadara ëNo ratings yet
- Survey of Postop .... 2012j.bjane.2012.06.011Document8 pagesSurvey of Postop .... 2012j.bjane.2012.06.011Zinar PehlivanNo ratings yet
- NCPDocument6 pagesNCPLevyanne GsanchezNo ratings yet
- (GYNE) 2018 April Midterms Ratio (Pucca)Document31 pages(GYNE) 2018 April Midterms Ratio (Pucca)NoreenNo ratings yet
- Clinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzDocument31 pagesClinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzNoreenNo ratings yet
- (Gyne) Family Planning (Dra Ona - Dra Castro) Updated Version (2022)Document14 pages(Gyne) Family Planning (Dra Ona - Dra Castro) Updated Version (2022)NoreenNo ratings yet
- (Anes) 5 - Local Anesthetics (Dra. Bonoan-Chan) ?Document5 pages(Anes) 5 - Local Anesthetics (Dra. Bonoan-Chan) ?NoreenNo ratings yet
- (Cardio B) 1 - Acute Rheumatic Fever and Rheumatic Heart Disease (Dr. Antolin, 2019)Document4 pages(Cardio B) 1 - Acute Rheumatic Fever and Rheumatic Heart Disease (Dr. Antolin, 2019)NoreenNo ratings yet
- (IM A) (Hema) IDA and Hypoproliferative Anemias-Dr. Perez 2 (Kim Villanueva)Document5 pages(IM A) (Hema) IDA and Hypoproliferative Anemias-Dr. Perez 2 (Kim Villanueva)NoreenNo ratings yet
- (Anes) 1 - Preanesthetic Evaluation (Dra. Luna-Gomez) ?Document5 pages(Anes) 1 - Preanesthetic Evaluation (Dra. Luna-Gomez) ?NoreenNo ratings yet
- (IM A) (Com Dse) Typhoid Fever (Strawberry)Document4 pages(IM A) (Com Dse) Typhoid Fever (Strawberry)NoreenNo ratings yet
- (IM A) (Com Dse) Typhoid Fever-Dr. Salandanan, Dr. Tan (Trisha Oberio, Kristine Navarro, Aisle Paler)Document4 pages(IM A) (Com Dse) Typhoid Fever-Dr. Salandanan, Dr. Tan (Trisha Oberio, Kristine Navarro, Aisle Paler)NoreenNo ratings yet
- Case 9 Section EDocument12 pagesCase 9 Section ENoreenNo ratings yet
- Clinical Therapeutics: Case 1Document17 pagesClinical Therapeutics: Case 1NoreenNo ratings yet
- (IM A) (Com Dse) Rabies-Dr. Coronel (Vision)Document7 pages(IM A) (Com Dse) Rabies-Dr. Coronel (Vision)Noreen100% (1)
- (MED) 3.05 Approach To Edema, Chest Pain, & Palpitations - AzaresDocument18 pages(MED) 3.05 Approach To Edema, Chest Pain, & Palpitations - AzaresNoreenNo ratings yet
- (Ophtha) 7 - Diseases of The Conjunctiva, Cornea, and Sclera (2019)Document8 pages(Ophtha) 7 - Diseases of The Conjunctiva, Cornea, and Sclera (2019)NoreenNo ratings yet
- Cardiology: Normal and Abnormal Myocardial Function: LendldeornmanDocument2 pagesCardiology: Normal and Abnormal Myocardial Function: LendldeornmanNoreenNo ratings yet
- (Pedia 3A) NEPHRO COMPILED PDFDocument40 pages(Pedia 3A) NEPHRO COMPILED PDFNoreenNo ratings yet
- (Pedia 3A) Immunology-Dr. de Jesus (Pinky Square)Document6 pages(Pedia 3A) Immunology-Dr. de Jesus (Pinky Square)NoreenNo ratings yet
- (MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)Document11 pages(MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)NoreenNo ratings yet
- Hypovolemic Shock & DIC (Bernabe)Document4 pagesHypovolemic Shock & DIC (Bernabe)NoreenNo ratings yet
- Hilot Wellness Massage Reviewer PDFDocument3 pagesHilot Wellness Massage Reviewer PDFPaul AndaNo ratings yet
- Krok 5Document53 pagesKrok 5Wolf WolforNo ratings yet
- Syncope: Mrs Shagufta IshtiaqDocument39 pagesSyncope: Mrs Shagufta IshtiaqZahid Ahmed KhanNo ratings yet
- Summarized ACLS ScriptDocument7 pagesSummarized ACLS Scriptnc.angel.niceNo ratings yet
- Penyakit Jantung Kongenital - TikaDocument43 pagesPenyakit Jantung Kongenital - Tikatika martikaNo ratings yet
- Implanted Cardioverter Defibrillator (Icd) Identification - : Wallet CardDocument1 pageImplanted Cardioverter Defibrillator (Icd) Identification - : Wallet CardΑλεξης ΝεοφυτουNo ratings yet
- Blood Sugar Blood Pressure Log 12012017Document2 pagesBlood Sugar Blood Pressure Log 12012017Mahbub RahmanNo ratings yet
- Hipertension Arterial (Hta) : ¿Qué Es La Hipertensión Arterial Según La Organización Mundial de La Salud (OMS) ?Document4 pagesHipertension Arterial (Hta) : ¿Qué Es La Hipertensión Arterial Según La Organización Mundial de La Salud (OMS) ?CésarÑañezNo ratings yet
- Physician's Report Form LIC03-012Document2 pagesPhysician's Report Form LIC03-012hnevkarNo ratings yet
- Automated External DefibrillatorDocument4 pagesAutomated External Defibrillatormelek saadiNo ratings yet
- Mitral ValveDocument48 pagesMitral Valvestoicea_katalinNo ratings yet
- Osce Notes - Myocardial InfarctionDocument10 pagesOsce Notes - Myocardial InfarctionmmmalcampoNo ratings yet
- Fisiologia Do Sistema Cardiovascular II e III - TextoDocument6 pagesFisiologia Do Sistema Cardiovascular II e III - TextoDavidson De AraújoNo ratings yet
- Varicose VeinsDocument2 pagesVaricose VeinsroycNo ratings yet
- ECG Skill LabDocument37 pagesECG Skill LabNayyer Khan100% (1)
- Cerebral AutoregulationDocument5 pagesCerebral AutoregulationJana ThukuNo ratings yet
- Predictor Scale of Delayed Cerebral Ischemic in Aneurysmal Subarachnoid Hemorrhage Case Series: What A Radiologist Should KnowDocument5 pagesPredictor Scale of Delayed Cerebral Ischemic in Aneurysmal Subarachnoid Hemorrhage Case Series: What A Radiologist Should KnowPopy TheresiaNo ratings yet
- Comparative Circulatory SystemDocument15 pagesComparative Circulatory SystemSmartcool SoNo ratings yet
- Acute Coronary Syndrome: Diagnosis and Initial Management: Each YearDocument9 pagesAcute Coronary Syndrome: Diagnosis and Initial Management: Each YearGabriela Pacheco0% (1)
- Stroke: BackgroundDocument10 pagesStroke: Backgroundjhay-r reyesNo ratings yet
- Body Fluids and CirculatoinDocument34 pagesBody Fluids and CirculatoinPrasmita BeheraNo ratings yet
- Pathophysiology: Predisposing Factors Precipitating FactorsDocument3 pagesPathophysiology: Predisposing Factors Precipitating FactorsFc ßobby HechanovaNo ratings yet
- 10.1038@s41569 020 00451 XDocument16 pages10.1038@s41569 020 00451 XAldo González SalinasNo ratings yet
- Clinical and Angiographic Profile of Coronary Artery Disease in Young Women - A Tertiary Care Centre Study From North Eastern IndiaDocument13 pagesClinical and Angiographic Profile of Coronary Artery Disease in Young Women - A Tertiary Care Centre Study From North Eastern IndiaIJAR JOURNALNo ratings yet
- Cardiovasular SystemDocument5 pagesCardiovasular SystemAsher Eby VargeeseNo ratings yet
- DysrhythmiaDocument30 pagesDysrhythmiaJJ JirapathNo ratings yet
- 22 Ventricular Septal DefectDocument26 pages22 Ventricular Septal Defectdhiraj parmarNo ratings yet
- BVCCT-304 EchocardiographyDocument71 pagesBVCCT-304 EchocardiographyManisha khanNo ratings yet
- Coronary Artery DiseaseDocument20 pagesCoronary Artery DiseaseAli Aborges Jr.No ratings yet
- Stroke Hemoragik (DR - Dr. Syahrul, SPS (K) )Document25 pagesStroke Hemoragik (DR - Dr. Syahrul, SPS (K) )YogaNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (32)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)