Professional Documents
Culture Documents
Chlorhexidine For Prevention of Alveolar Osteitis: A Randomised Clinical Trial
Uploaded by
JulieOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chlorhexidine For Prevention of Alveolar Osteitis: A Randomised Clinical Trial
Uploaded by
JulieCopyright:
Available Formats
Original Article
http://dx.doi.org/10.1590/1678-7757-2017-0245
Chlorhexidine for prevention of
alveolar osteitis: a randomised
clinical trial
Abstract
Diego HALABI1 Objective: To determine the effectiveness of chlorhexidine 0.12%
Jose ESCOBAR2 mouthwash (CHX) after tooth extraction for the prevention of alveolar osteitis
(AO). Material and methods: We conducted a double-blind randomised
Cyntia ALVARADO1
clinical trial stratified by risk factors. We enrolled a cohort of 822 patients
Nicolette MARTINEZ1
who underwent dental extractions, and were considered to be at risk of
Carlos MUÑOZ1 developing AO (previous surgical site infection, traumatic extraction, and
tobacco smoking). After extraction, patients were randomly allocated for
CHX group or placebo group, matched by risk factors. The primary outcome
was clinical diagnosis of AO: increasing postoperative pain for 4 d within and
around the socket, and total or partial breakdown of the blood clot in the
socket with or without bone exposure. Results: Follow-up was completed
by 744 participants (372 chlorhexidine and 372 placebo). We detected no
significant differences between the two groups at baseline. After completed
follow-up, risk factors were equally distributed between the two groups.
Overall incidence of OA was 4.97%, in which 27 participants treated with
placebo (7.26%) and 10 participants treated with CHX (2.69%) developed
AO. CHX reduced the incidence of AO by 63% [Absolute Risk Reduction:
4.57 (95% CI 1.5-7.7), Number Needed to Treat: 21.88 (95% CI 13.0-69.3),
Fisher’s exact test: p=0.006]. No adverse effects were reported. Conclusion:
The use of chlorhexidine 0.12% mouthwash after tooth extraction is safe and
effective in reducing the incidence of AO in high-risk patients.
Keywords: Preventive dentistry. Oral surgery. Tooth extraction.
Chlorhexidine. Clinical trial. Alveolar osteitis.
Submitted: June 21, 2017
Modification: September 8, 2017
Accept: September 27, 2017
Corresponding address: 1
Universidad Austral de Chile, Facultad de Medicina, Escuela de Odontologia, Valdivia, Chile.
Diego Halabi 2
Servicio de Salud Valdivia, Valdivia, Chile.
Universidad Austral de Chile, Facultad de Medicina,
Escuela de Odontologia, Valdivia, Chile.
Phone: +56 63 2293928
e-mail: diego.halabi@uach.cl
J Appl Oral Sci. 1/7 2018;26:e20170245
Chlorhexidine for prevention of alveolar osteitis: a randomised clinical trial
Introduction was approved by the Research Ethics Committee of
the Public Health Service of Valdivia. The trial was
Patients who undergo dental extractions are at registered as ISRCTN14646628.
risk of developing post-operative complications, and
Population
the most common is the alveolar osteitis (AO)12. Our
We recruited patients registered to receive dental
group8 recently reported an incidence of 6.4% of AO,
care from a list of random numbers generated
and we determined by a logistic regression model that
by computer, from April 2013 to December 2015.
previous surgical site infection, tobacco smoking and
Inclusion criteria were adults of 18 years or older
traumatic extraction are risk factors for developing AO.
with clinical indications for tooth extraction, and who
These risk factors explain why there were changes in
presented at least one of the following risk factors
prevalence ranging from 3.9% up to 29.6% for the
for developing AO: tobacco smoker (consumption
third molar10,23.
of ≥5 cigarettes 24 h before extraction), previous
With a risk model that predicts the development
surgical site infection (clinical diagnosis of chronic
of AO, it is possible to implement preventive health
periodontitis, acute periodontal conditions, apical
care to those individuals at high risk. Thus, clinicians
periodontitis, pericoronitis, fungal infections, or dental
can help their patients to avoid the severe pain caused
pulp gangrene) and/or traumatic extraction (lifting
by this complication17, which traditionally receives
a flap, use of elevators for >4 min, and/or rotary
symptomatic treatment of uncertain effectiveness16.
instruments).
Hence, clinicians can reduce health care costs and
Exclusion criteria were patients requiring extraction
provide comfort for patients9.
in the operating theater, residents of rural areas who
It has been proposed that chlorhexidine 0.12%
manifested difficulty in returning for follow-up, patients
mouthwash can be used after extraction for the
allergic to chlorhexidine, patients under antimicrobial
prevention of AO10,13,18. Chlorhexidine is the most
therapy, antibiotic prophylaxis, or antibiotics therapy
widely used antiseptic in dentistry because its
after extraction.
broad-spectrum antibacterial effectiveness is well
Dental extractions were performed by dental
established2, so it can be implemented as a simple
surgery team from the emergency department of
and inexpensively public health policy.
the clinic, in accordance with standard procedures as
However, the clinical trials that support chlorhexidine
defined by the National Health Service14.
0.12% mouthwash are inconclusive, showing
methodological weaknesses and having a high risk of
Interventions
bias5,9,24. Therefore, the need to conduct randomized
After surgery, patients were allocated to the
clinical trials of better quality and including risk factors
treatment group or the placebo group. Treatment
is imperative.
consisted of a mouthwash with 15 ml chlorhexidine
Here, we conducted a double-blind randomised
0.12% (Oralgene® Mouthwash 0.12%, Maver, Chile)
clinical trial stratified by risk factors to determine the
for 30 s, twice a day for 7 d, starting 24 h after
effectiveness of CHX after tooth extraction for the
extraction. The placebo was sterile water, with the
prevention of AO.
same indications for use. Both chlorhexidine and
placebo were stored in similar brown plastic bottles,
and instructions were given orally and in writing to
Material and methods each participant.
To guarantee that in both groups (treatment
Trial design and placebo) the risk of alveolar osteitis was similar
We conducted a randomized, double-blind, parallel- and comparable, the assignment was performed by
group, stratified by risk factors, placebo-controlled, randomization, stratified by risk factors, and 7 groups
clinical trial in two public community dental clinics in were formed with the following possible combinations:
Valdivia, Chile (population 154,559). All participants smoker; previous infection; traumatic extraction;
agreed to participate by signing an informed consent smoker + previous infection; smoker + traumatic
form, according to the recommendations of the extraction; previous infection + traumatic extraction;
Declaration of Helsinki. The protocol of this study smoker + previous infection + traumatic extraction.
J Appl Oral Sci. 2/7 2018;26:e20170245
HALABI D, ESCOBAR J, ALVARADO C, MARTINEZ N, MUÑOZ C
To avoid the risk of having more patients in a group,
we stored black envelopes in a box containing a paper
with the letter C for chlorhexidine or P for placebo (half
of each). The envelopes were chosen for each patient Statistics
after the extraction and transported to another room We performed the statistical analysis by DH using
(without opening them); they were read only by one R 3.3.1 (R Foundation for Statistical Computing,
of the authors, who then distributed the chlorhexidine Vienna, Austria). We used the Fisher’s exact test to
or placebo accordingly. For each patient who was detect significant differences in the incidence of AO
assigned to a group, the subsequent patient who between CHX and placebo groups, and also to analyse
arrived with the same risk factors was matched to gender, tooth location, patient smoking, previous
the opposite group, and the respective envelope was infection and traumatic extraction variables. We used
discarded (to ensure homogeneity of groups). unpaired t-test was to detect significant differences in
age between CHX and placebo groups. We determined
Outcome measures the incidence of AO for both groups and calculated
We recorded age (years), gender (male or the Number Needed to Treat (NNT). For all tests,
female), tooth location (mandibular or maxillary), statistical differences were determined to be significant
diagnosis or previous surgical site infection (yes or at p<0.05.
no, as described), smoking (smoker or non-smoker,
as described) and traumatic extraction (yes or no, as
described) before tooth extraction for each patient.
Results
The primary outcome was positive diagnosis of AO
one week after tooth extraction. Positive diagnosis of
From April 2013 to December 2015, we recruited
AO was identified by the authors in patients with the
822 participants. Out of these, 744 met inclusion
following characteristics: 1) increasing postoperative
criteria and completed the follow-up. They were
pain intensity for 4 d within and around the socket
allocated into two groups of 372 for treatment of
and 2) total or partial breakdown of the blood clot in
chlorhexidine 0.12% or placebo. Figure 1 shows the
the socket with or without bone exposure.
flow diagram of participants.
At the same time, we assessed hypersensitivity
As seen in Table 1, we included 381 female
to chlorhexidine (contact dermatitis, pruritus, vesicle
participants and 363 males at baseline. The mean age
formation, urticaria, dyspnea, or anaphylactic shock),
was 43.43 years (SD 14.99). Comparison of baseline
dysgeusia (alteration of taste perception, bitter taste
data between the group treated with chlorhexidine
or burning) or pigmentation (staining of teeth and/or
0.12% and the one treated with placebo did not show
tongue) as potentially adverse events.
statistically significant differences for age [t(degrees of
We treated patients who developed alveolar
freedom)=0.917 (742), p=0.359], gender (p=0.463),
osteitis and other complications in accordance with
location of the extracted tooth (p=0.238), previous
the available clinical protocols of the Chilean Health
infection in surgical site (p=0.999), tobacco smoke
Ministry14.
(p=0.999) or traumatic extraction (p=0.999).
Once all participants completed the follow-up, we
Sample size
observed that the risk factors were equally distributed
We estimated sample size using data published
between the two groups, without statistically
previously by Halabi, et al.8 (2012), expecting an
significant differences (see details in Table 2).
incidence reduction of two-thirds. The PA expected
We diagnosed 37 cases of AO, with an overall
incidence of disease (AO) in the placebo group was
prevalence of 4.97%. In the group treated with
6.14%, while the PB expected incidence of disease
chlorhexidine 0.12% mouthwash we diagnosed 10
(AO) in the CHX group was 2.05%. Additionally, k
participants (2.69%) with AO, while in the placebo
groups ratio of sample sizes between groups was 1:1.
group they were 27 (7.26%) (p=0.006, statistical
The power of the study was set at 80% (β=0.20),
power=0.821). CHX reduced the incidence of AO by
with α=0.05 as the significance level. Based on these
63% [Absolute Risk Reduction: 4.57 (CI95% 1.5-7.7),
parameters, we applied the following equation19:
Number Needed to Treat: 21.88 (CI95% 13.0-69.3)].
J Appl Oral Sci. 3/7 2018;26:e20170245
Chlorhexidine for prevention of alveolar osteitis: a randomised clinical trial
Figure 1- CONSORT flow diagram of patients included in the final analysis
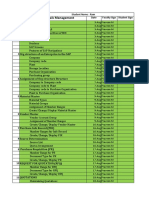
Table 1- Baseline data of participants, mean age (SD), and frequency (%) of gender, location of the tooth extracted, previous surgical site
infection, tobacco smoke and traumatic extraction
Chlorhexidine Placebo Total P value
(n=372) (n=372) (n=744)
Age (years ± SD) 43.93±15.15 42.92±14.84 43.43±14.99 0.396
Gender [n (%)]
Female 185 (48.6%) 196 (51.4%) 381 (100%) 0.463
Male 187 (51.5%) 176 (48.5%) 363 (100%)
Tooth location [n (%)]
Mandibular 158 (47.5%) 175 (52.5%) 333 (100%) 0.238
Maxillary 214 (52.1%) 197 (47.9%) 411 (100%)
Previous surgical site infection [n (%)]
Yes 339 (50%) 339 (50%) 678 (100%) 0.999
No 33 (50%) 33 (50%) 66 (100%)
Smoking [n (%)]
Smoker 152 (49.8%) 153 (50.2%) 305 (100%) 0.999
Non-smoker 220 (50.1%) 219 (49.9%) 439 (100%)
Traumatic extraction [n (%)]
Yes 51 (50%) 51 (50%) 102 (100%) 0.999
No 321 (50%) 321 (50%) 642 (100%)
See more details in Table 3. 0.12% mouthwash to reduce the prevalence of
No patient had hypersensitivity to chlorhexidine, postextraction AO, and we contrasted it with a placebo-
dysgeusia or tooth pigmentation. controlled group. We presented new findings in which
chlorhexidine treatment reduces the incidence of AO by
63% in high-risk patients, with strong statistical power.
Subgroup analysis showed no difference in the
Discussion
incidence of AO and location of the extracted tooth.
Mandibular teeth developed the same rate of AO as
We conducted a randomised, controlled trial to
that of the maxillary teeth, and anterior teeth showed
assess the effectiveness of postoperative chlorhexidine
J Appl Oral Sci. 4/7 2018;26:e20170245
HALABI D, ESCOBAR J, ALVARADO C, MARTINEZ N, MUÑOZ C
a similar prevalence to posterior teeth. These findings of AO after extraction of impacted mandibular third
are consistent with our previous observations 8. molars (RR 0.62; 95% CI, 0.40 to 0.96). In contrast,
Therefore, our results can be extrapolated to any Delilbasi, et al.7 (2002) found that 0.2% chlorhexidine
patient who requires an extraction, regardless of the had no statistically significant effect in reducing the
location of the tooth. prevalence of AO after mandibular third molar removal
AO incidence in this study was quite similar to that (RR 0.88; 95% CI, 0.45 to 1.72). However, these
which we reported previously: 4.97% versus 6.4%8. studies have a high risk of bias6,9,24.
We suspect that the incidence might have been higher Our study has several strengths compared to those
in the placebo group on this occasion (incidence was reported in the literature. To minimize selection bias,
7.26%), since the study sample consisted of patients we randomly included only the patients who had the
with an increased risk of developing alveolar osteitis. risk factors that we reported previously8. Thus, the
However, we can explain this because the placebo preventive effect was studied in a group known to
effect can work as an effective treatment, especially have a high risk of developing AO, and not in persons
in conditions associated with pain .
15,22
who have not had chances to develop AO, regardless
Our results have some similarities with those of receiving treatment or not.
reported in the literature with similar interventions. We assigned participants to each group randomly,
Ragno and Szutnik 18
(1991) reported a statistically blindly and matched by risk factors. Thus, both groups
significant reduction of 50% in the prevalence of AO had similar distribution in the risk of developing AO,
after the extraction of mandibular third molars [risk and the results cannot be taken by a simple imbalance
ratio (RR) 0.5; 95% confidence interval (CI), 0.27 to in the risk to develop AO in any of the groups.
0.93]. Larsen13 (1991) studied the AO preventive effect Additionally, we did not observe losses regarding
of chlorhexidine 0.12% mouthwash after mandibular follow-up or treatment withdrawals, minimising
third molar removal and observed a reduction in the attrition bias risk. This was because we designed a
prevalence of 60% (RR 0.4; 95% CI, 0.21 to 0.75). protocol of four phone calls encouraging the patient
Hermesch, et al. 10
(1998) reported that chlorhexidine to attend the clinical control, and our local community
0.12% mouthwash reduced to 38% the prevalence clinics allow to “retain” patients.
Studies that we compared previously used a model
Table 2- Frequency of patients by matched risk factors for
alveolar osteitis, distributed by treatment group of impacted mandibular third molars. We consider
that this model does not differ from ours, in which we
Risk factor Chlorhexidine Placebo Total
(n=372) (n=372) (n=744) included the extraction of any tooth in the mouth. The
S 24 24 48 only difference is that in the extraction of impacted
PI 191 190 381 third molars, the risk factor “traumatic extraction” is
TE 3 3 6 exacerbated, which explains why the prevalence of AO
S+PI 106 107 213 in these studies is higher. In addition, we controlled
S+TE 6 6 12 the tooth location, which gives us the advantage that
PI+TE 26 26 52 our results can be extrapolated to a wider population,
S+PI+TE 16 16 32 and not be limited to only those procedures with a
Total 372 372 744 high level of tissue damage (i.e. mandibular third
molar extraction).
S: Tobacco smoke
PI: Previous infection in surgical site Nonetheless, this study has some weaknesses.
TE: Traumatic extraction Firstly, it is difficult to ensure that patients have
Table 3- Incidence of alveolar osteitis in patients treated with chlorhexidine 0.12% mouthwash or placebo
AO Health Total ARR (95% CI) NNT P value
(95% CI)
Chlorhexidine 10 362 372 4.57% 21.88 0.006*
Placebo 27 345 372 (1.5 – 7.7) (13.0 – 69.3)
Total 37 437 744
AO: Alveolar Osteitis; ARR: Absolute Risk Reduction; NNT: Number Needed to Treat; CI: Confidence interval; *: p<0.05; power=0.822
(Fisher’s exact test)
J Appl Oral Sci. 5/7 2018;26:e20170245
Chlorhexidine for prevention of alveolar osteitis: a randomised clinical trial
followed the full treatment, because they administered References
themselves in their homes. To reduce the risk of poor
treatment procedure, we phoned the patients once a 1-Amler MH. The time sequence of tissue regeneration in human
extraction wounds. Oral Surg Oral Med Oral Pathol. 1969;27(3):309-18.
day for the first 4 d to remind them to use the rinse.
2-Balbuena L, Stambaugh KI, Ramirez SG, Yeager C. Effects of topical
Additionally, we required them to bring the bottles oral antiseptic rinses on bacterial counts of saliva in healthy human
of mouthwash to the dental control, to ensure that subjects. Otolaryngol Head Neck Surg. 1998;118(5):625-9.
3-Berchier CE, Slot DE, Van der Weijden GA. The efficacy of 0.12%
it was fully used. If this had not been the case, the
chlorhexidine mouthrinse compared with 0.2% on plaque accumulation
patient would have been discarded from the follow-up. and periodontal parameters: a systematic review. J Clin Periodontol.
We used sterile water as placebo, which could have 2010;37(9):829-39.
4-Bonesvoll P. Oral pharmacology of chlorhexidine. J Clin Periodontol.
been a risk if the patient recognized it as such, but
1977;4(5):49-65.
in the reinforcement phone calls, we did not detect 5-Caso A, Hung L-K, Beirne OR. Prevention of alveolar osteitis with
this situation in any patient. Secondly, the operational chlorhexidine: a meta-analytic review. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 2005;99(2):155-9.
definition of smokers was changed in relation to our
6-Daly B, Sharif MO, Newton T, Jones K, Worthington HV. Local
previous study8 (i.e. consumption of ≥5 cigarettes 24 h interventions for the management of alveolar osteitis (dry socket).
after extraction, to consumption of ≥5 cigarettes 24 h Cochrane Database Syst Rev. 2012;12:CD006968.
7-Delilbasi C, Saracoglu U, Keskin A. Effects of 0.2% chlorhexidine
before extraction). To include the patient as a smoker
gluconate and amoxicillin plus clavulanic acid on the prevention of
we had to know if they smoked previously. alveolar osteitis following mandibular third molar extractions. Oral Surg
It has been proposed that intra-alveolar application Oral Med Oral Pathol Oral Radiol Endod. 2002;94(3):301-4.
8-Halabí D, Escobar J, Muñoz C, Uribe S. Logistic regression analysis of
of chlorhexidine 0.2% gel may be an effective
risk factors for the development of alveolar osteitis. J Oral Maxillofac
treatment to prevent AO11,20,21. However, the evidence Surg. 2012;70(5):1040-4.
supporting this preventive therapy has the same 9-Hedström L, Sjögren P. Effect estimates and methodological quality
of randomized controlled trials about prevention of alveolar osteitis
inconsistencies and weaknesses as the studies
following tooth extraction: a systematic review. Oral Surg Oral Med
of chlorhexidine 0.12% mouthwash6. There is no Oral Pathol Oral Radiol Endod. 2007;103(1):8-15.
biological plausibility that this form of treatment can 10-Hermesch CB, Hilton TJ, Biesbrock AR, Baker RA, Cain-Hamlin
be more effective, because a concentration of 0.2% J, McClanahan SF, et al. Perioperative use of 0.12% chlorhexidine
gluconate for the prevention of alveolar osteitis: efficacy and risk
shows no additional antibacterial benefits than the
factor analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
concentration of 0.12%3, and the substantivity of the 1998;85(4):381-7.
chlorhexidine mouthwash is sufficient to maintain its 11-Hita-Iglesias P, Torres-Lagares D, Flores-Ruiz R, Magallanes-Abad N,
Basallote-Gonzalez M, Gutierrez-Perez JL. Effectiveness of chlorhexidine
effect for 12 h4. There is no evidence that chlorhexidine
gel versus chlorhexidine rinse in reducing alveolar osteitis in mandibular
may have a negative effect on haemostasis, and the third molar surgery. J Oral Maxillofac Surg. 2008;66(3):441-5.
mode of use as a mouthwash does not interfere with 12-Jaafar N, Nor GM. The prevalence of post-extraction complications
in an outpatient dental clinic in Kuala Lumpur Malaysia - a retrospective
clot formation, since our application protocol begins 24
survey. Singapore Dent J. 2000;23(1):24-8.
h after the extraction, when the clot has already been 13-Larsen PE. The effect of a chlorhexidine rinse on the incidence of
stabilized and begins to be replaced with granulation alveolar osteitis following the surgical removal of impacted mandibular
third molars. J Oral Maxillofac Surg. 1991;49(9):932-7.
tissue .
1
14-Ministerio de Salud. Guía Clínica AUGE de Urgencia Odontológica
With the strengths and weaknesses of our study, Ambulatoria. 2011.
we conclude that the use of chlorhexidine 0.12% 15-Moore PA, Crout RJ, Jackson DL, Schneider LG, Graves RW, Bakos
L. Tramadol hydrochloride: analgesic efficacy compared with codeine,
mouthwash after tooth extraction is highly effective
aspirin with codeine, and placebo after dental extraction. J Clin
compared with placebo mouthwash in preventing AO in Pharmacol. 1998;38(6):554-60.
high-risk patients. Clinical trials evaluating preventive 16-Noroozi AR, Philbert RF. Modern concepts in understanding and
management of the “dry socket” syndrome: comprehensive review
effects should consider the risk factors in the study
of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
design to minimise risk of bias. 2009;107(1):30-5.
17-Oginni FO. Dry socket: a prospective study of prevalent risk factors
Acknowledgments in a Nigerian population. J Oral Maxillofac Surg. 2008;66(11):2290-5.
18-Ragno JR Jr, Szkutnik AJ. Evaluation of 0.12% chlorhexidine rinse
This clinical trial was self-funded by the authors.
on the prevention of alveolar osteitis. Oral Surg Oral Med Oral Pathol.
Austral University of Chile supported the fees of 1991;72(5):524-6.
registration and publication. 19-Shao J, Chow S-C, Wang H. Sample size calculations in clinical
research. 2. ed. New York: Chapman & Hall; 2003.
Conflict of interest
Authors declare no conflict of interest.
J Appl Oral Sci. 6/7 2018;26:e20170245
HALABI D, ESCOBAR J, ALVARADO C, MARTINEZ N, MUÑOZ C
20-Torres-Lagares D, Gutierrez-Perez JL, Infante-Cossio P, Garcia- 22-Turner JA, Deyo RA, Loeser JD, Von Korff M, Fordyce WE. The
Calderon M, Romero-Ruiz MM, Serrera-Figallo MA. Randomized, importance of placebo effects in pain treatment and research. JAMA.
double-blind study on effectiveness of intra-alveolar chlorhexidine gel 1994;271(20):1609-14.
in reducing the incidence of alveolar osteitis in mandibular third molar 23-Upadhyaya C, Humagain H. Prevalence of dry socket following
surgery. Int J Oral Maxillofac Surg. 2006;35(4):348-51. extraction of permanent teeth at Kathmandu University Teaching
21-Torres-Lagares D, Infante-Cossio P, Gutierrez-Perez JL, Romero-Ruiz Hospital (KUTH), Dhulikhel, Kavre, Nepal: a study. Kathmandu Univ
MM, Garcia-Calderon M, Serrera-Figallo MA. Intra-alveolar chlorhexidine Med J (KUMJ). 2010;8(29):18-24.
gel for the prevention of dry socket in mandibular third molar surgery. 24-Yengopal V, Mickenautsch S. Chlorhexidine for the prevention of
A pilot study. Med Oral Patol Oral Cir Bucal. 2006;11(2):E179-84. alveolar osteitis. Int J Oral Maxillofac Surg. 2012;41(10):1253-64.
J Appl Oral Sci. 7/7 2018;26:e20170245
You might also like
- Molar Incisor Hypomineralization: A Clinical Guide to Diagnosis and TreatmentFrom EverandMolar Incisor Hypomineralization: A Clinical Guide to Diagnosis and TreatmentKatrin BekesNo ratings yet
- Infection Control in the Dental Office: A Global PerspectiveFrom EverandInfection Control in the Dental Office: A Global PerspectiveLouis G. DePaolaNo ratings yet
- Ekso 1Document8 pagesEkso 1HASANUDDIN STNo ratings yet
- 19-109 Putri Amalia CSS Radiologi PDFDocument20 pages19-109 Putri Amalia CSS Radiologi PDFPutri AmaliaNo ratings yet
- Articulo 1Document7 pagesArticulo 1Adrian EspinosaNo ratings yet
- Journal Exo:BM 5Document5 pagesJournal Exo:BM 5asdfasdNo ratings yet
- Journal Exo:BM 5Document5 pagesJournal Exo:BM 5asdfasdNo ratings yet
- Translate BMDocument4 pagesTranslate BMnrlNo ratings yet
- Efficacy of Intra-Alveolar Chlorhexidine Gel in Reducing Frequency of Alveolar Osteitis in Mandibular Third Molar SurgeryDocument4 pagesEfficacy of Intra-Alveolar Chlorhexidine Gel in Reducing Frequency of Alveolar Osteitis in Mandibular Third Molar SurgeryCahyo AdyNo ratings yet
- Risk Factors of Oral Cancer-A Hospital Based Case Control StudyDocument6 pagesRisk Factors of Oral Cancer-A Hospital Based Case Control StudyDevica DR PutriNo ratings yet
- Recent Advancements in Management of Alveolar Osteitis (Dry Socket)Document5 pagesRecent Advancements in Management of Alveolar Osteitis (Dry Socket)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Prevencion de La Neummonia PostDocument9 pagesPrevencion de La Neummonia PostDiana SalinasNo ratings yet
- Medoral 21 E696Document7 pagesMedoral 21 E696andreeaNo ratings yet
- Health Effects From Exposure To Dental Diagnostic X-Ray: Environmental Health and ToxicologyDocument6 pagesHealth Effects From Exposure To Dental Diagnostic X-Ray: Environmental Health and ToxicologyhelmysiswantoNo ratings yet
- Journal of Cranio-Maxillo-Facial SurgeryDocument6 pagesJournal of Cranio-Maxillo-Facial SurgeryRahmatiaMozaikeNo ratings yet
- Management of Dry SocketDocument8 pagesManagement of Dry SockettasyaNo ratings yet
- Systemic Review of Dry Socked Aetiology Treatment and PreventionDocument4 pagesSystemic Review of Dry Socked Aetiology Treatment and PreventionAnnisa MardhatillahNo ratings yet
- Foreign Body Aspirations in Dental Clinics: A Narrative ReviewDocument14 pagesForeign Body Aspirations in Dental Clinics: A Narrative Reviewicha nursyamNo ratings yet
- Mauprivez 2016Document28 pagesMauprivez 2016Abel PelaezNo ratings yet
- Dreyer - Et - Al-2018-J Periodon ResDocument25 pagesDreyer - Et - Al-2018-J Periodon ResAFKs GamerNo ratings yet
- Single StepDocument6 pagesSingle StepDaniel Alejandro Flores Gutierrez.No ratings yet
- Clorexidina en CirugiaDocument4 pagesClorexidina en CirugiaLuch Carla FloresNo ratings yet
- 01art1 s2.0 S0020653922001678 MainDocument6 pages01art1 s2.0 S0020653922001678 Maindr.antonio.velasquezNo ratings yet
- The Effect of Resin Infiltration On Proximal Caries Lesions in Primary and Permanent Teeth. A Systematic Review and Meta-Analysis of Clinical TrialsDocument10 pagesThe Effect of Resin Infiltration On Proximal Caries Lesions in Primary and Permanent Teeth. A Systematic Review and Meta-Analysis of Clinical Trialsmae leeNo ratings yet
- Dento 1Document11 pagesDento 1Yeni PuspitasariNo ratings yet
- Recent Advances in Diagnostic Oral MedicineDocument6 pagesRecent Advances in Diagnostic Oral Medicinegayathrireddy varikutiNo ratings yet
- I0003-3219-89!3!359 White Spot Lesion AlignerDocument6 pagesI0003-3219-89!3!359 White Spot Lesion AlignerLima JúniorNo ratings yet
- Prevalence of Non-Carious Cervical Lesions in Dakar PrisonsDocument6 pagesPrevalence of Non-Carious Cervical Lesions in Dakar PrisonsDHONY MIFTAHUL HUDANo ratings yet
- Jcpe 13246Document17 pagesJcpe 13246Dr. Pragyan SwainNo ratings yet
- 1 s2.0 S1879729615001064 MainDocument4 pages1 s2.0 S1879729615001064 MainMarcelo DiasNo ratings yet
- Interventions For The Prevention of Dry Socket - An Evidence-Based UpdateDocument4 pagesInterventions For The Prevention of Dry Socket - An Evidence-Based Updateanees jamalNo ratings yet
- HipertensiDocument7 pagesHipertensiSyafara Santos AffadhaNo ratings yet
- Tooth Extraction Before Radiotherapy Is A Risk Factor For Developing Osteoradionecrosis ofDocument31 pagesTooth Extraction Before Radiotherapy Is A Risk Factor For Developing Osteoradionecrosis ofbichocorralNo ratings yet
- Tic Treatment of Teeth With Apical Period On Tit Is Single vs. Multi Visit TreatmentDocument6 pagesTic Treatment of Teeth With Apical Period On Tit Is Single vs. Multi Visit Treatmentgpv38No ratings yet
- Dry SocketDocument10 pagesDry Socketkanikak97No ratings yet
- Medi 100 E25304Document5 pagesMedi 100 E25304Nurul AidaNo ratings yet
- Efficacy of Warm Saline and Chlorhexidine Mouth Rinses in Prevention of Alveolar Osteitis After Third Molar Surgery: A Comparative StudyDocument5 pagesEfficacy of Warm Saline and Chlorhexidine Mouth Rinses in Prevention of Alveolar Osteitis After Third Molar Surgery: A Comparative StudyHusnul BasyarNo ratings yet
- Articulo 4Document11 pagesArticulo 4Alan SublimeNo ratings yet
- Corneal UlcerDocument6 pagesCorneal UlcerChanifah SitiNo ratings yet
- Alveolar Osteitis: Patients' Compliance To Post-Extraction Instructions Following Extraction of Molar TeethDocument5 pagesAlveolar Osteitis: Patients' Compliance To Post-Extraction Instructions Following Extraction of Molar TeethSweetz Viena ParamitaNo ratings yet
- Cleidocranial Dysplasia A Review of Clinical Radiological Genetic Implications and Guidelines ProposalDocument8 pagesCleidocranial Dysplasia A Review of Clinical Radiological Genetic Implications and Guidelines ProposalGina Alexandra Aldana PortelaNo ratings yet
- Polak Et Al-2015-Journal of Clinical Periodontology PDFDocument13 pagesPolak Et Al-2015-Journal of Clinical Periodontology PDFChristine HacheNo ratings yet
- Management of Post-Orthodontic White Spot Lesions: An Updated Systematic ReviewDocument6 pagesManagement of Post-Orthodontic White Spot Lesions: An Updated Systematic ReviewRiska Endah CahyaniNo ratings yet
- Comparative Efficacy of Chemiluminescence and ToluDocument7 pagesComparative Efficacy of Chemiluminescence and ToluAqila FadiaNo ratings yet
- Lapsus 1Document3 pagesLapsus 1Winda WidhyastutiNo ratings yet
- Effects of Honey in The Management of Alveolar Osteitis: A StudyDocument24 pagesEffects of Honey in The Management of Alveolar Osteitis: A Study123No ratings yet
- Medoral 18 E38Document7 pagesMedoral 18 E38Seena JoveinNo ratings yet
- Jurnal Kedokteran GigiDocument9 pagesJurnal Kedokteran GigiamrinagristaauliaNo ratings yet
- Kirim 1Document2 pagesKirim 1Rara Suci RhamadhanNo ratings yet
- Alamanos 2016Document12 pagesAlamanos 2016dana40018256No ratings yet
- Barbara Kirnbauer Norbert Jakse Astrid Truschnegg Ivana Dzidic Khaled Mukaddam Michael PayerDocument13 pagesBarbara Kirnbauer Norbert Jakse Astrid Truschnegg Ivana Dzidic Khaled Mukaddam Michael PayermpaivaecostaNo ratings yet
- China Risk FactorsDocument6 pagesChina Risk FactorsNoor MohammadNo ratings yet
- J Clinic Periodontology - 2015 - JepsenDocument6 pagesJ Clinic Periodontology - 2015 - JepsenJimmy SandovalNo ratings yet
- Medi 96 E5864Document6 pagesMedi 96 E5864mono1144No ratings yet
- 2018 JCP Rodrigo SEPA - PerimplantDocument11 pages2018 JCP Rodrigo SEPA - PerimplantAFKs GamerNo ratings yet
- Case-Control Study of Oral Disease Indexes in Individuals With Head and Neck Cancer After Antineoplastic TherapyDocument6 pagesCase-Control Study of Oral Disease Indexes in Individuals With Head and Neck Cancer After Antineoplastic TherapyGeorgia.annaNo ratings yet
- Recurrence Rates After Surgical Removal of Oral Leukoplakia-A Prospective Longitudinal Multi-Centre StudyDocument13 pagesRecurrence Rates After Surgical Removal of Oral Leukoplakia-A Prospective Longitudinal Multi-Centre StudyRafa LopezNo ratings yet
- 2 PDFDocument5 pages2 PDFPipin HeryantoNo ratings yet
- Diag 1 Current and Future Research in Diagnostic Criteria and Evaluation of Caries Detection MethodsDocument10 pagesDiag 1 Current and Future Research in Diagnostic Criteria and Evaluation of Caries Detection MethodsAbdulmajeed alluqmaniNo ratings yet
- Opthalmologi JurnalDocument11 pagesOpthalmologi JurnalShintaPuspitasariNo ratings yet
- Final - 2018 CA-1 Tutorial Textbook - Smartphone or Tablet-3Document342 pagesFinal - 2018 CA-1 Tutorial Textbook - Smartphone or Tablet-3Nick-Hugh Wisdom100% (1)
- Cusick ReferenceDrugCardDocument2 pagesCusick ReferenceDrugCardJulieNo ratings yet
- Anesthesia Resident Requirements PDFDocument21 pagesAnesthesia Resident Requirements PDFJulieNo ratings yet
- Pimp Questions-SmithDocument66 pagesPimp Questions-SmithJulie100% (2)
- Respiratory Therapy Pocket Reference: Ifnopt TriggerDocument2 pagesRespiratory Therapy Pocket Reference: Ifnopt TriggerJulieNo ratings yet
- UnderstandingAnesthesia1 1 2Document144 pagesUnderstandingAnesthesia1 1 2marina_shawkyNo ratings yet
- OMFS Rotation OverviewDocument12 pagesOMFS Rotation OverviewJulieNo ratings yet
- Upload 8Document2 pagesUpload 8cingyaNo ratings yet
- Wa0007 PDFDocument56 pagesWa0007 PDFfida amalinaNo ratings yet
- ML Adult OR Emergency ManualDocument30 pagesML Adult OR Emergency ManualJulieNo ratings yet
- Omsite 2004 PDFDocument196 pagesOmsite 2004 PDFJulieNo ratings yet
- PONV Prophylaxis Reference CardDocument1 pagePONV Prophylaxis Reference CardJulieNo ratings yet
- 2008 Oral and Maxillofacial Surgery Self Assessment Tool (OMSSAT)Document253 pages2008 Oral and Maxillofacial Surgery Self Assessment Tool (OMSSAT)Julie75% (4)
- OMSITE QuestionsDocument6 pagesOMSITE QuestionsJulieNo ratings yet
- 2007 Oral and Maxillofacial Surgery Self Assessment Tool (OMSSAT)Document220 pages2007 Oral and Maxillofacial Surgery Self Assessment Tool (OMSSAT)Julie100% (2)
- Omsite 2005 PDFDocument180 pagesOmsite 2005 PDFJulie100% (2)
- Cocero Anticoagulantes Orales Directos y Comorbilidades Marzo 2019Document8 pagesCocero Anticoagulantes Orales Directos y Comorbilidades Marzo 2019api-265532519No ratings yet
- 2009 Oral and Maxillofacial Surgery Self Assessment Tool (OMSSAT)Document272 pages2009 Oral and Maxillofacial Surgery Self Assessment Tool (OMSSAT)Julie100% (1)
- Omsite 2004 PDFDocument196 pagesOmsite 2004 PDFJulieNo ratings yet
- 2009 Oral and Maxillofacial Surgery Self Assessment Tool (OMSSAT)Document272 pages2009 Oral and Maxillofacial Surgery Self Assessment Tool (OMSSAT)Julie100% (1)
- Omfs TRST 4 PDFDocument201 pagesOmfs TRST 4 PDFgrizzlov100% (2)
- I0003 3006 64 2 80Document5 pagesI0003 3006 64 2 80angienayibeNo ratings yet
- Omssat2008 (1) (1) 1Document253 pagesOmssat2008 (1) (1) 1Ganga Hospital100% (2)
- Buccal Infiltration in MN Molars PDFDocument4 pagesBuccal Infiltration in MN Molars PDFJulieNo ratings yet
- Case Report: Hemorrhage After Dental Extractions PDFDocument9 pagesCase Report: Hemorrhage After Dental Extractions PDFJulieNo ratings yet
- Anaesthesia TMJ Pain Orthognathic Pathology Reconstruction PDFDocument220 pagesAnaesthesia TMJ Pain Orthognathic Pathology Reconstruction PDFAmit TyagiNo ratings yet
- Omfs TRST 4 PDFDocument201 pagesOmfs TRST 4 PDFgrizzlov100% (2)
- Articaine Vs Lido in Palatal TissueDocument7 pagesArticaine Vs Lido in Palatal TissueJulieNo ratings yet
- Does Pre-Emptive Administration of Ibuprofen Vs Acetaminophen Reduce Post-Op Pain?Document9 pagesDoes Pre-Emptive Administration of Ibuprofen Vs Acetaminophen Reduce Post-Op Pain?JulieNo ratings yet
- Does Grafting After Tooth Extraction Prevent Periodontal DiseaseDocument8 pagesDoes Grafting After Tooth Extraction Prevent Periodontal DiseaseJulieNo ratings yet
- California Evaluation Procedures For New Aftermarket Catalytic ConvertersDocument27 pagesCalifornia Evaluation Procedures For New Aftermarket Catalytic Convertersferio252No ratings yet
- Mechanical Seminar ListDocument9 pagesMechanical Seminar ListalokbdasNo ratings yet
- 20 5880100Document2 pages20 5880100'Theodora GeorgianaNo ratings yet
- Shangri La Hotels and Resorts SWOTDocument2 pagesShangri La Hotels and Resorts SWOTHadi Agustana100% (1)
- LSRetailDataDirector UserGuideDocument89 pagesLSRetailDataDirector UserGuideRock Lee60% (5)
- Online Dating GuideDocument101 pagesOnline Dating Guidewoodyallen78No ratings yet
- Chandler V MillerDocument2 pagesChandler V MillerJay Cezar100% (1)
- Safety and Quality of Health Care System in IndiaDocument18 pagesSafety and Quality of Health Care System in IndiaKNOWLEDGE FeedNo ratings yet
- Tribology Aspects in Angular Transmission Systems: Hypoid GearsDocument7 pagesTribology Aspects in Angular Transmission Systems: Hypoid GearspiruumainNo ratings yet
- Crestron Teams HardeningDocument20 pagesCrestron Teams HardeningmanishNo ratings yet
- Tech Note FormatDocument2 pagesTech Note FormatUgonna OhiriNo ratings yet
- Manual Flowpet 5GDocument56 pagesManual Flowpet 5GRahkmat DanizarNo ratings yet
- IBM OpenPages Admin Guide 7.0 PDFDocument822 pagesIBM OpenPages Admin Guide 7.0 PDFMba NaniNo ratings yet
- Format Transmittal - TemplateDocument1 pageFormat Transmittal - TemplateavriamandaNo ratings yet
- Kalokal Barangay Highway HillsDocument35 pagesKalokal Barangay Highway HillsDixie MirandaNo ratings yet
- Gliffy Public Diagram - ATM FlowchartDocument3 pagesGliffy Public Diagram - ATM Flowchartmy nNo ratings yet
- Supreme Court upholds return of unrepaired truckDocument35 pagesSupreme Court upholds return of unrepaired truckJeffreyReyesNo ratings yet
- Community Development and Umbrella BodiesDocument20 pagesCommunity Development and Umbrella Bodiesmoi5566No ratings yet
- App Cache 133069888033757953Document46 pagesApp Cache 133069888033757953akunkelasdNo ratings yet
- Ram SAP MM Class StatuscssDocument15 pagesRam SAP MM Class StatuscssAll rounderzNo ratings yet
- Navigating The Digital Age PDFDocument369 pagesNavigating The Digital Age PDFSteve GilsonNo ratings yet
- Problem Solving 5Document4 pagesProblem Solving 5Raphael Pizarro ArceoNo ratings yet
- SSRN Id983401Document43 pagesSSRN Id983401LeilaNo ratings yet
- Em8 1session2.2Document25 pagesEm8 1session2.2DreamCodmNo ratings yet
- COVID-19 Vaccination Appointment Details: Center Preferred Time SlotDocument1 pageCOVID-19 Vaccination Appointment Details: Center Preferred Time SlotRmillionsque FinserveNo ratings yet
- Presentation On Tutorial Question On Promissory EstoppelDocument13 pagesPresentation On Tutorial Question On Promissory EstoppelNaqeeb NexerNo ratings yet
- Inductive sensor technical specifications in 40 charactersDocument3 pagesInductive sensor technical specifications in 40 charactersBasarNo ratings yet
- Enclosure No. 6: Election Application PacketDocument8 pagesEnclosure No. 6: Election Application PacketLen LegaspiNo ratings yet
- Municipal Profile of Umingan, PangasinanDocument51 pagesMunicipal Profile of Umingan, PangasinanGina Lee Mingrajal Santos100% (1)
- Agreement: /ECE/324/Rev.2/Add.127 /ECE/TRANS/505/Rev.2/Add.127Document29 pagesAgreement: /ECE/324/Rev.2/Add.127 /ECE/TRANS/505/Rev.2/Add.127Mina RemonNo ratings yet